Abstract
Background
Endoscopic adrenalectomy is currently performed using multiple ports placed either transabdominally or retroperitoneally. We report our initial experience with single-incision retroperitoneoscopic adrenalectomy (SIRA).
Methods
A prospective database of patients undergoing adrenalectomy from December 2013 through March 2016 was analyzed. We adopted conventional retroperitoneoscopic adrenalectomy (CORA) in December 2013 and transitioned to SIRA in March 2015. SIRA was performed using three trocars placed through a single 2-cm incision below the 12th rib. Clinical characteristics and outcomes were compared between patients undergoing SIRA and CORA.
Results
One hundred and five adrenalectomies were performed in 102 patients: 34 laparoscopic transperitoneal, 24 CORA, 37 SIRA and 7 open. The SIRA and CORA groups were similar with respect to clinical characteristics (SIRA vs. CORA: mean BMI 27.0 vs. 28.8 kg/m2, maximum BMI 38.9 vs. 44.3 kg/m2; mean nodule size 3.2 vs. 3.2 cm, maximum nodule size 8.0 vs. 6.0 cm). One patient undergoing SIRA required placement of an additional 5-mm port because of extensive adhesions. No patients who underwent SIRA or CORA required conversion to open adrenalectomy. There were no deaths, and blood loss remained <10 mL for all cases. Operative length was similar between SIRA and CORA (105 vs. 92 min, P = 0.26). In multivariable linear regression analysis, nodule size > 5 cm (effect = 1.75, P < 0.001) and pheochromocytoma (effect = 1.30, P = 0.05) were significant predictors of increased operative length for SIRA. BMI and laterality (right vs. left) did not affect operative length. Rates of postoperative temporary abdominal wall relaxation, length of stay and postoperative pain medication use were similar between the two groups.
Conclusions
SIRA is safe and feasible to implement as a refinement of CORA and may be applied to technically challenging cases involving obese patients or large nodules. The use of three ports allows for two-handed dissection, which may shorten the learning curve for many surgeons.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Endoscopic adrenalectomy is considered the standard of care for resection of benign adrenal masses [1, 2]. This can be performed through a transperitoneal or retroperitoneal approach. Although the most common technique in the USA remains laparoscopic transperitoneal adrenalectomy, the retroperitoneoscopic approach has gained much popularity over the past decade [3, 4]. A recent prospective, randomized study reported shorter operative length, less blood loss, reduced postoperative pain and faster recovery for the retroperitoneal versus the transperitoneal approach [5].
Currently, conventional retroperitoneoscopic adrenalectomy (CORA) is most commonly performed using three individual ports placed through three separate incisions [6]. Single-access retroperitoneoscopic adrenalectomy (SARA) was first described in 2009 as a refinement to CORA that enabled adrenalectomy to be performed through a single incision [7, 8]. In the original technique described, SARA required single-handed dissection performed through two 5-mm ports. This may be technically challenging and has not been widely adopted.
In the current study, we report our modified technique of single-incision retroperitoneoscopic adrenalectomy (SIRA). Our aim was to demonstrate the safety and feasibility of SIRA and to evaluate its performance against the well-established CORA technique.
Methods
Patients and study design
Following institutional review board approval, we evaluated a prospectively maintained database of patients undergoing adrenalectomy at University of California, Los Angeles Medical Center (UCLA), from December 2013 to March 2016. At UCLA, CORA was adopted in December 2013 and subsequently transitioned to SIRA in March 2015. Exclusion criteria for both CORA and SIRA included nodule size >8 cm and suspicion for malignancy based on imaging characteristics. Patients not eligible for surgery with CORA or SIRA underwent laparoscopic transperitoneal adrenalectomy if the nodule was >8 cm but appeared benign on imaging or open adrenalectomy if there was a high suspicion for malignancy.
Operative technique
SIRA was performed with the patient in prone position on non-compressive bolsters to allow the abdominal contents to fall forward and expand the retroperitoneal working space [9] (Fig. 1). The retroperitoneal space was entered by direct cutdown through a 2-cm skin incision made just below the inferior border of the 12th rib. A mini-GelPOINT device (Applied Medical) equipped with three 5 mm ports was placed through the single incision. The retroperitoneal space was insufflated up to 30 mm Hg. A 5 mm 30° camera and two additional instruments, a blunt dissector and a LigaSure device, were inserted through the GelPOINT device. Gerota’s fascia was entered bluntly, and the superior pole of the kidney was identified. The medial dissection was then performed to ligate the adrenal vein with the LigaSure device. For right-sided adrenalectomy, the medial border of the IVC was dissected to identify the insertion of the adrenal vein. For left-sided adrenalectomy, the inferior phrenic vein was used as a landmark to identify the adrenal vein. Caution must be taken to securely and safely ligate the adrenal vein, especially on the right side, with consideration for use of hemoclips in certain cases. The adrenal gland was then circumferentially dissected with a rim of periadrenal fat. The specimen was removed in an Endocatch bag and morcellated when necessary.
Single-incision retroperitoneoscopic adrenalectomy (SIRA) technique. A Patient is placed in a prone position. B A single 2-cm incision is made lateral to paraspinal muscle and just below the 12th rib and a direct cut down incision is made to enter the retroperitoneum. C The mini-GelPOINT device equipped with 3 individual 5-mm ports is placed through the incision. D The 2-cm incision is closed with subcuticular suture. E Depiction of the left-sided retroperitoneal anatomy of the operative field. F Depiction of the right-sided retroperitoneal anatomy of the operative field
CORA was performed using two 5 mm ports and one 10-mm port placed through three separate incisions as previously described [6]. Once retroperitoneal access was achieved, the rest of the operation was performed in similar fashion to the SIRA technique described above.
Predictors and outcome variables
We compared the patient characteristics and operative outcomes of all patients undergoing SIRA and CORA during the study period. Clinical characteristics included age, gender, BMI, nodule size, laterality and indication for adrenalectomy. Operative outcomes included length of operation, estimated blood loss, length of stay, the use of oral and intravenous postoperative narcotic pain medication and the rate of abdominal wall relaxation. Abdominal wall relaxation is defined as a subjective sensation of weakening of the ipsilateral abdominal wall associated with a physical finding of abdominal wall bulging. This is different from abdominal wall hernia in that no actual fascial defect is present. Patients were examined at their initial postoperative visit for abdominal wall relaxation and asked whether they subjectively felt any abdominal wall bulging following surgery. All patients with abdominal wall relaxation had follow-up at 1–2 months following surgery to determine whether it had resolved.
Statistical analysis
Patient demographic data and operative outcomes were reported as means ± standard deviations or medians ± interquartile ranges for continuous variables, and frequencies and percentages for categorical variables. Student t test or Wilcoxon rank-sum was used to compare continuous variables, and the Chi-square test was used to compare categorical variables. Univariate and multivariable linear regressions were performed to evaluate the association between clinical characteristics and operative length. Specifically, the outcome variable operative length was log-transformed (natural logarithm) in the linear regression. The effect of a predictor variable was calculated as e β, where β is the regression coefficient estimated from the linear regression model. This effect can be used to approximate the ratio of operative length associated with one unit increase in that predictor. Multivariable regression analyses included adjustments for patient age and BMI, nodule size and indication for surgery (including the presence of pheochromocytoma). Nodule size was analyzed as a continuous variable and a dichotomous variable using size cutoffs of 3, 4 and 5. P values of less than 0.05 were defined as statistically significant.
Results
Patient characteristics
During the study period, 105 adrenalectomies were performed in 102 patients. Of these, 24 patients underwent CORA, 37 patients underwent SIRA, 34 patients underwent laparoscopic transperitoneal adrenalectomy and 7 patients underwent open adrenalectomy. The mean age of the study cohort was 54.5 ± 13.7 years, and 54.1% of the patients were female. The mean BMI was 27 ± 5.6 kg/m2 (range 16.1–38.9 kg/m2). The indications for adrenalectomy were aldosteronoma (43%), pheochromocytoma (24%), non-functional adenoma (24%), hypercortisolism (6%) and metastatic disease (3%). There was no difference in baseline patient characteristics between the SIRA and CORA groups (Table 1).
Operative outcomes
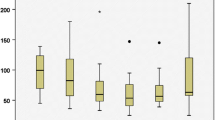
Operative outcomes including length of operation and estimated blood loss were similar between the SIRA and CORA groups (Table 2). The median operative length was 105 min for SIRA and 92 min for CORA (P = 0.26). Blood loss remained <10 mL for patients in both groups, and no patient required a blood transfusion. Length of stay was also similar, with most patients requiring only an overnight observation (SIRA vs. CORA: 1.1 ± 0.7 vs. 1.4 ± 1.1 days). Temporary abdominal wall relaxation occurred in 10.8% (N = 4) of SIRA patients and 12.5% (N = 3) of CORA patients, and all patients reported resolution of abdominal wall relaxation within 2 months of surgery. The use of postoperative pain medication was also similar between the two groups, with 58% of SIRA patients and 65% of CORA patients requiring intravenous pain medication in the first 24 h following surgery.
Conversion from SIRA to CORA was necessary in 1 patient who had a 3.5 cm left-sided pheochromocytoma due to extensive adhesions from prior abdominal surgery (including trauma laparotomy and gastric bypass). An additional 5 mm port was placed laterally to aid the dissection. No conversion to open adrenalectomy was necessary for either the SIRA or CORA group.
Predictors of operative length for SIRA
Clinical characteristics of patients undergoing SIRA were analyzed to identify predictors of operative length (Tables 3, 4). In multivariable regression, nodule size and pheochromocytoma were independent predictors of longer operative length. Nodule size > 5 cm was associated with a 75% increase in operative length (effect = 1.75, P < 0.01), and the presence of pheochromocytoma was associated with a 30% increase in operative length (effect = 1.30, P = 0.05). Older age was associated with shorter operative length, with effect of 0.93 for each 10 year increase in patient age. BMI and laterality had no impact on the operative length using the SIRA approach.
A trend toward shorter operative length was noted as we gained more experience with the SIRA technique. The average operative length for the first three quarters of SIRA cases (N = 28) was 121 ± 48 min, compared with 93 ± 18 min for the last quarter of cases (P = 0.09). There was no difference in clinical characteristics including the mean nodule size (3.4 vs. 3.1 cm, P = 0.87) and the presence of pheochromocytoma (25 vs. 22%, P = 0.86) during these two time periods.
Discussion
Laparoscopic adrenalectomy performed through either a transperitoneal or retroperitoneal approach has improved patient outcomes compared to open adrenalectomy for appropriately selected patients. Single-incision adrenalectomy remains to be widely adopted, likely due to the increased technical difficulty of this technique. To our knowledge, this is the first reported North American series of single-incision retroperitoneoscopic adrenalectomy. In our experience, SIRA was safe and feasible, and resulted in similar patient outcomes to CORA. The benefits of SIRA include the improved cosmesis and potentially decreased incisional pain.
Previous studies have reported that single-access retroperitoneal adrenalectomy can be safely performed for appropriately selected patients by surgeons experienced in adrenal surgery [8, 10–13]. Waltz et al. [8] demonstrated the safety of SARA in patients with small nodules and a “minimal amount of periadrenal fatty tissue” (no specific nodule size or BMI cutoff was mentioned). Shi et al. [14] reported a series of 19 patients with nodule size up to 4 cm who underwent SARA with similar perioperative outcomes compared to case-matched CORA controls. A more recent study by Wang et al. described 51 obese patients with BMI > 30 kg/m2 and nodule size up to 4 cm who safely underwent SARA [13].
In our current series, patients with BMI up to 40 kg/m2 and nodule size up to 8 cm safely underwent SIRA. SARA as described by Waltz et al. was performed using single-handed dissection through two 5 mm ports. Our modified technique using the mini-GelPOINT device equipped with three individual ports enabled two-handed dissection, a technique similar to most other laparoscopic procedures. Unlike the studies by Shi et al. and Wang et al., we routinely used insufflation pressure up to 30 mmHg, which is helpful in particular for obese patients. Careful positioning with large abdominal bolsters is also necessary for obese patients to create an adequate working space. In addition, dissection of the retroperitoneum relies mainly on known landmarks (paraspinous muscle, superior pole of the kidney, and IVC for right-sided nodules and inferior phrenic vein for left-sided nodules, respectively). The presence of significant retroperitoneal fat is not prohibitive as long as the locations of these key landmarks are kept in mind. These principles may allow surgeons experienced in SIRA to expand their criteria in regards to nodule size and patient body habitus.
Our findings suggest that early in the learning curve, the best candidates for SIRA are patients with smaller nodules (<5 cm) and for indications other than pheochromocytoma. Larger nodules are more difficult to manipulate with the limited degrees of freedom available when the two working ports are placed very close together (essentially working in parallel), as is the case in the SIRA technique. Our current indications for performing SIRA include nodule size smaller than 5 cm and BMI under 40 kg/m2. We perform laparoscopic transabdominal adrenalectomy in most patients with nodule size greater than 6 cm.
Pheochromocytomas deserve special consideration, as they are often larger, more vascularized, and have greater adhesions to the surrounding tissues than other adrenal nodules. Control of the adrenal vein is critical in these cases, especially on the right side where the adrenal vein is generally short and wide, and drains directly into the IVC Bleeding from the adrenal vein in these cases may cause major hemorrhage and require emergent conversion to laparotomy. Extreme caution should be taken and the use of hemoclips as an alternative to the LigaSure devise should be considered. Care must also be taken when performing SIRA to avoid undue pressure on the pheochromocytoma from the limited angle of dissection, which may risk rupturing the pheochromocytoma [15, 16]. An advantage of retroperitoneoscopic adrenalectomy is the use of high insufflation pressures, which decrease capsular bleeding during dissection of a pheochromocytoma [16]. We did note the presence of a learning curve, with operative length decreasing after about 25 cases.
In our current series, operative outcomes including length of operation and postoperative pain medication use were similar between CORA and SIRA. Previously SARA was reported to decrease the length of stay compared to CORA (2.4 ± 0.7 vs. 3.1 ± 1.2 days, P < 0.01) [8]. The median reported length of stay following SARA or CORA is as high as 5–6 days [13, 14]. In our series, the length of stay for the CORA group was already minimal at 1.4 ± 1.1 days. As a result, no significant difference was observed when compared to the SIRA group. The rate of postoperative narcotic pain medication use for SIRA was 76%, higher than the rate of 45% previously reported for SARA. This is likely explained by differences in nursing protocols, use of non-narcotic pain medications and individual patient factors including pain tolerance.
Advancements in technology and surgical equipment have sparked growing enthusiasm for minimally invasive surgery. Our current study demonstrated the safety and feasibility of SIRA as a refinement to CORA. SIRA can be performed in the majority of patients who are eligible for CORA, even in technically challenging cases involving obese patients or large nodules. The use of three ports enables two-handed dissection, which may shorten the learning curve for this technique.
References
Smith CD, Weber CJ, Amerson JR (1999) Laparoscopic adrenalectomy: new gold standard. World J Surg 23:389–396
Winfield HN, Hamilton BD, Bravo EL, Novick AC (1998) Laparoscopic adrenalectomy: the preferred choice? A comparison to open adrenalectomy. J Urol 160:325–329
Conzo G, Tartaglia E, Gambardella C, Esposito D, Sciascia V, Mauriello C, Nunziata A, Siciliano G, Izzo G, Cavallo F, Thomas G, Musella M, Santini L (2016) Minimally invasive approach for adrenal lesions: systematic review of laparoscopic versus retroperitoneoscopic adrenalectomy and assessment of risk factors for complications. Int J Surg 28(Suppl 1):S118–S123
Chai YJ, Kwon H, Yu HW, Kim SJ, Choi JY, Lee KE, Youn YK (2014) Systematic review of surgical approaches for adrenal tumors: lateral transperitoneal versus posterior retroperitoneal and laparoscopic versus robotic adrenalectomy. Int J Endocrinol 2014:918346
Barczynski M, Konturek A, Nowak W (2014) Randomized clinical trial of posterior retroperitoneoscopic adrenalectomy versus lateral transperitoneal laparoscopic adrenalectomy with a 5-year follow-up. Ann Surg 260:740–747 discussion 747–748
Walz MK, Alesina PF, Wenger FA, Deligiannis A, Szuczik E, Petersenn S, Ommer A, Groeben H, Peitgen K, Janssen OE, Philipp T, Neumann HP, Schmid KW, Mann K (2006) Posterior retroperitoneoscopic adrenalectomy—results of 560 procedures in 520 patients. Surgery 140:943–948
Walz MK, Alesina PF (2009) Single access retroperitoneoscopic adrenalectomy (SARA)—one step beyond in endocrine surgery. Langenbecks Arch Surg 394:447–450
Walz MK, Groeben H, Alesina PF (2010) Single-access retroperitoneoscopic adrenalectomy (SARA) versus conventional retroperitoneoscopic adrenalectomy (CORA): a case-control study. World J Surg 34:1386–1390
Sho S, Gott DC, Yeh MW, Livhits MJ (2016) Right single-incision retroperitoneoscopic adrenalectomy using the mini gelpoint device. Video Endocrinol. doi:10.1089/ve.2016.0071
Branco AW, Kondo W, Stunitz LC, Neto SR, Nascimento CC, Filho AJ (2010) Adrenalectomy by retroperitoneal laparoendoscopic single site surgery. JSLS 14:571–575
Chung SD, Huang CY, Wang SM, Tai HC, Tsai YC, Chueh SC (2011) Laparoendoscopic single-site (LESS) retroperitoneal adrenalectomy using a homemade single-access platform and standard laparoscopic instruments. Surg Endosc 25:1251–1256
Lin VC, Tsai YC, Chung SD, Li TC, Ho CH, Jaw FS, Tai HC, Yu HJ (2012) A comparative study of multiport versus laparoendoscopic single-site adrenalectomy for benign adrenal tumors. Surg Endosc 26:1135–1139
Wang Y, He Y, Li BS, Wang CH, Chen Z, Lu ML, Wen ZQ, Chen X (2016) Laparoendoscopic single-site retroperitoneoscopic adrenalectomy versus conventional retroperitoneoscopic adrenalectomy in obese patients. J Endourol 30:306–311
T-p Shi, Zhang X, Ma X, H-z Li, Zhu J, B-j Wang, J-p Gao, Cai W, Dong J (2011) Laparoendoscopic single-site retroperitoneoscopic adrenalectomy: a matched-pair comparison with the gold standard. Surg Endosc 25:2117–2124
Toniato A, Boschin IM, Opocher G, Guolo A, Pelizzo M, Mantero F (2007) Is the laparoscopic adrenalectomy for pheochromocytoma the best treatment? Surgery 141:723–727
Dickson PV, Alex GC, Grubbs EG, Ayala-Ramirez M, Jimenez C, Evans DB, Lee JE, Perrier ND (2011) Posterior retroperitoneoscopic adrenalectomy is a safe and effective alternative to transabdominal laparoscopic adrenalectomy for pheochromocytoma. Surgery 150:452–458
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Drs. Sho, Yeh, Li and Livhits have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Sho, S., Yeh, M.W., Li, N. et al. Single-incision retroperitoneoscopic adrenalectomy: a North American experience. Surg Endosc 31, 3014–3019 (2017). https://doi.org/10.1007/s00464-016-5325-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5325-8