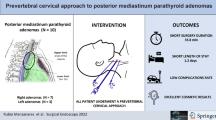
Abstract
Background
Parathyroid gland mediastinal ectopia is an unusual but challenging condition in surgical management of hyperparathyroidism. Posterior mediastinum parathyroid ectopia is rare, and glands need to be removed either with a broad open cervical or thoracic approach. In recent years, several minimally invasive approaches to mediastinal parathyroid glands have been described, but for posterior mediastinum adenomas, proposed techniques are transthoracic.
Methods
The aim of this paper is to describe, to our best knowledge for the first time, a standardized pure endoscopic cervical technique to approach posterior mediastinal parathyroid adenomas which we have used in three patients.
Results
The technique was applied in three patients which excellent surgical, postoperative, and cosmetic results.
Conclusions
Endoscopic prevertebral approach is a feasible, sure and inexpensive standardized pure endoscopic cervical approach to posterior mediastinal parathyroid adenomas, which may result in a less aggressive surgical option when compared with thoracic approaches.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Parathyroid gland mediastinal ectopia is an unusual but challenging condition in surgical management of hyperparathyroidism. Posterior mediastinal parathyroid glands are believed to result from inferoposterior migration of the superior parathyroid glands and can be a rare cause of ectopic parathyroid tissue [1].
The mediastinum is bounded superiorly by the thoracic inlet and inferiorly by the diaphragm. For clinical purposes, the mediastinum has traditionally been divided into the anterior (or anterosuperior), middle, and posterior compartments. There are no fascial planes between these divisions, and they are in continuity with each other. Thus, tumors can exist in more than one compartment. The anterior mediastinum lies between the sternum and the pericardium. It contains the thymus, lymph nodes, and loose connective tissue. The middle mediastinum contains the heart, the proximal great vessels, phrenic nerves, trachea, and main bronchi. The posterior mediastinum lies posterior to the pericardium and anterior to the thoracic vertebrae. It contains the esophagus, descending thoracic aorta, azygos vein, thoracic duct, and autonomic ganglia [2].
Most of posterior mediastinum parathyroid ectopia can be removed either with an open cervical or thoracic approach. However, a large incision and an extensive dissection are usually required. This occurs especially in obese patients or in cases with previous neck surgery.
In recent years, several minimally invasive approaches to mediastinal parathyroid gland have been described [3–22]. Cervical endoscopic or video-assisted approaches refer to anterior mediastinum adenomas. When focusing in posterior mediastinum adenomas, proposed techniques are always transthoracic, with a minimal open incision or by minimally invasive video-assisted thoracoscopy. Robotic assistance has also been referred in recent publications [23–26].
Cervical approach is a more familial surgical field for Endocrine General Surgeons. Its endoscopic performance may result in a less aggressive surgical option when compared with thoracic approaches due to the lack of pleural incisions. Besides, cervical approach carries out an easier patient management for anesthesiologists, as selective bronchial intubation is not needed.
The aim of this paper is to describe a feasible, sure and inexpensive standardized pure endoscopic cervical approach to posterior mediastinal parathyroid adenomas.
Materials and methods
Patients
Three consecutive patients were operated. Institutional protocols were strictly followed and patients gave explicit informed consent both for surgery and endoscopic approach. All patients were female, with age of 49, 56, and 69 years. Biochemical diagnosis of primary hyperparathyroidism was established, and surgery was indicated in two patients according to the ASBMR Guidelines for the Management of Asymptomatic Primary Hyperparathyroidism [27] (New Guidelines were not yet published at the moment of surgery). These two younger patients (cases 2 and 3) were morbidly obese, whit BMI of 45 and 56 kg/m2 respectively.
The older patient (case 1), had underwent a previous total thyroidectomy for multinodular goiter and total parathyroidectomy without auto-transplantation for secondary hyperparathyroidism, attended at other institution. This patient presented a recurrent hyperparathyroidism whit surgical indication.
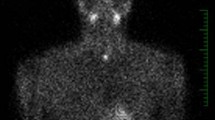
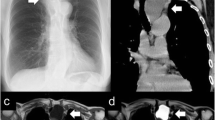
Neck ultrasonography and Tc-99 m-MIBI dual-phase scintigraphy with SPECT/CT imaging were performed in all three patients, demonstrating in all cases a single gland disease on the right side of posterior mediastinum, at Th3-Th4 vertebral level (Fig. 1).
Surgical technique
The surgical intervention is performed under general anesthesia and tracheal intubation. Antibiotic and antithrombotic prophylaxis was used in all patients.
Step 1: Team disposition and patient placement
The surgeon is located at the head of the patient on the right side and the assistant stands on the left. The scrub and instruments table is placed on the right side of the surgeon. Monitors are placed in front of surgeon at the left side of the patient, at patient’s abdomen level (Fig. 2).
The patient is placed in a position of slight hyperextension of the neck, and the head is slightly rotated to the opposite side of intervention (Fig. 3).
Step 2: Creating the working space
A 11-mm incision is made at midway between sternal knot and mastoid. Electro-cautery and shears dissection is performed to open a plane between carotid sheet and prethyroidal muscles and esophagus. Once the anterior aspect of cervical spine is reached, blunt digital dissection is used to extend retro-esophageal dissection (Fig. 4).
Step 3: Trocar placement
Three trocars are placed on anterior sternocleidomastoid muscle relief. At this point, two 5-mm trocars, or a 2.8 mm and a 5 mm trocar, are placed under digital control in the space between carotid sheet an prethyroidal muscles, 3–4 cm up (port 1, left hand) and down (port 2, right hand) previous incision, to slightly reach the previously dissected virtual space. Then, a 11-mm trocar (port 1, optics and extraction) is putted on place reaching the same space (Fig. 5). At this point, a 15 mmHg CO2 pneumomediastinum is slowly established (3 l/min).
Step 4: Mediastinal dissection
A 5 mm in diameter, 0º and 20 cm in length fiberoptic endoscope is introduced through port 1, a 2.8 or 5 mm atraumatic grasper trough port 2 and a Ligasure® dolphin tip 5 mm diameter and 20-cm-length instrument (Covidien, Covidien plc 20, Lower Hatch Street Dublin 2, Ireland) through port 3.
Using both instruments, blunt dissection is performed to extend the dissection deeper on the thorax, using as references the esophagus on the left side and carotid artery in the first centimeters on the right side and, later, the subclavian artery and brachiocephalic trunk on the anterolateral aspect of the surgical field. The dissection is progressed on this way till parathyroid adenoma relief is visualized (Fig. 6).
In the first case, we used as port 1 a 2.8-mm trocar and grasper, but we changed later to 5-mm instruments due to the fact that they allow an easier and quicker handling of the gland. The rationale for the selection of the energy device includes a thin tip bipolar instrument which enhances the dissection and warrants surrounding tissue protection during sealing, avoiding risks related to unnoticed contacts of the external aspect of the active branch of ultrasonic sealing devices in a small virtual space.
Step 5: Gland dissection
The gland is mobilized by means of blunt dissection (Fig. 7). Vascular attachments are easily identified, sealed, and cut. So the gland is get free in the mediastinum.
Step 6: Gland removal
At this point, the fiberoptic endoscope is changed to port 2 or 3 and the grasper is pulled through port 1. Using gentle traction, the gland is brought to the 11-mm incision and easily removed (Fig. 8), lightly extending the incision if necessary.
Step 7: Closure
Drainages are not used. Reabsorbable sutures are placed to close the gap between sternocleidomastoid and prethyroidal muscles at 11-mm incision. Subcuticular sutures and sterile strips are used to close skin wounds (Figs. 9, 10).
Results
No intraoperative adverse events occurred, neither related to pneumomediastinum, not due to the surgical technique. Mean operative time was 32 ± 7 min. Blood loss was virtually null.
Calcium levels at 20 h from surgery were normalized in all three cases. Two patients were discharged next day after surgery, with a slight lower cervical cutaneous emphysema as the only complaint. The remaining patient (reoperation for secondary hyperparathyroidism) was derived to Nephrologist.
Histology confirmed the preoperative diagnosis, with parathyroid adenomas weighing 2.6, 2.9, and 3.7 g, respectively. Posterior revisions confirmed a satisfactory evolution and the cure of the disease.
Discussion
Endoscopic parathyroid surgery has not reached a wide spread among endocrine surgeons [1]. Modern selective open approaches to hyperparathyroidism have diminished surgical aggressiveness and, for many surgeons, endoscopic accesses represent an unnecessarily accomplished approach.
Nevertheless, there is a group of patients who can clearly obtain benefits from an endoscopic approach.
Mediastinal parathyroid adenomas are uncommon and can usually be removed by an open cervical approach [2]. However, great incisions and extensive dissection are frequently required for gland identification and removal as gland allocation may be deep. Sternotomy and thoracotomy have been used likewise to remove these glands when a deeper localization or higher gland weigh was found [3–6].
Along last 20 years, diverse approaches have been proposed for mediastinal parathyroid gland adenomas, but cervical pure endoscopic approach has been rarely described [7] and details about a reproducible surgical technique for posterior mediastinum adenomas remain, to our best knowledge, undescribed.
Most of published papers focusing on this entity postulate open cervical or thoracoscopic approach, with a preferred use, in general, for the last one [10–16].
We had operated several anterior mediastinum parathyroid adenomas localized more than 6–7 cm from the sternal knot by means of endoscopic or video-assisted mediastinoscopy techniques. This previous experience encouraged us to adapt the endoscopic technique to posterior mediastinum.
The need for radioguided surgery and intraoperative parathyroid hormone monitoring has been advocated to assure good results with these minimally invasive approaches [17–21]. However, if preoperative localization is undoubted (Tc-99 m-MIBI dual-phase scintigraphy with SPECT/CT) and gland size is not very small, it may not be necessary.
Robotic techniques have been also postulated, and transthoracic approach is the preferred one. In spite of good results reported with these techniques, its use has not been widely spread, probably due to its more recent development, the lack of wide availability and its higher costs [23–26]. Besides, these techniques have the issue of longer operative times, usually larger than one and a half hour.
Possible limits for the described approach could be both small and very large adenomas. In our experience, most of superior parathyroid adenomas migrated to posterior planes of the neck and mediastinum have a considerable size. Besides, posterior mediastinum has an advantage when compared to anterior mediastinum, which is its virtually lack of fat tissue, even in obese patients, unlike anterior mediastinum, as we have seen in patients we have treated by means of both endoscopic anterior and posterior mediastinum approaches. If during surgery we were not able to find the adenoma, the guidance of an intraoperative oral endoscopic ultrasonography could be helpful. At this point, it is necessary to remark the relevance of a preoperative perfect knowledge of adenoma characteristics and location by means of Tc-99 m-MIBI dual-phase scintigraphy with SPECT/CT imaging.
However, may be that adenomas about 1 cm or less could be very hard to find. Probably, deep adenomas less than 1 cm may not be suitable for this approach, and radioguided VATS could be the best option. On the other hand, due to the narrow surgical field we can get, adenomas larger than 3–4 cm in transverse diameter probably could be very difficult to handle by means of the described approach, so perhaps VATS could be also the best option for these patients.
The cervical pure endoscopic approach proposed in this paper has shown, in our experience, a high feasibility and short surgical time, with excellent postoperative results regarding to patient comfort, length of stay and disease cure, offering besides a very reasonable proceeding costs.
References
Silverberg SJ, Shane E, Jacobs TP, Siris E, Bilezikian JP (1999) A 10-year prospective study of primary hyperthyroidism with or without parathyroid surgery. N Engl J Med 34:1249–1255
Kim JY, Hofstetter WL (2010) Tumors of the Mediastinum and Chest Wall. Surg Clin N Am 90:1019–1040
Assalia A, Inabnet WB (2004) Endoscopic parathyroidectomy. Otolaryngol Clin N Am 37:871–886
Nwariaku FE, Snyder WH, Burkey SH, Watumull L, Mathews D (2005) Inframanubrial parathyroid glands in patients with primary hyperparathyroidism: alternatives to sternotomy. World J Surg 29:491–494
Ogawa T, Tsuji E, Kanauchi H, Yamada K, Mimura Y, Kaminishi M (2007) Excision of postesophageal parathyroid adenoma in posterior mediastinum with intraoperative 99mTechnetium sestamibi scanning. Ann Thorac Surg 84:1754–1756
Nakai K, Fujii H, Maeno K, Nishida K, Kobayashi A, Shin J, Hara S, Nishi S (2014) A case of parathyroid adenoma adjacent to the thoracic spine in a hemodialysis patient. Clin Nephrol 81:52–57
Yun JS, Nam KH, Chung WY, Park CS (2008) Giant posterior mediastinal parathyroid adenoma. Thyroid 18:475–476
Moreno P, Francos JM, Shaha A, Bosch A, de Lama E, Rafecas A, Jaurrieta E (2007) Intercostal Video-Assisted Mediastinal Surgery through an intercostal window (IVAMS): a simpler approach to perform mediastinal parathyroidectomy. Surgery 142:410–413
Inabnet WB, Chu CA (2003) Transcervical endoscopic-assisted mediastinal parathyroidectomy with intraoperative parathyroid hormone monitoring. Surg Endosc 17:1678
Sukumar MS, Komanapalli CB, Cohen JI (2006) Minimally invasive management of the mediastinal parathyroid adenoma. Laryngoscope 116:482–487
Iacobone M, Mondi I, Viel G, Citton M, Tropea S, Frego M, Favia G (2010) The results of surgery for mediastinal parathyroid tumors: a comparative study of 63 patients. Langenbecks Arch Surg 395:947–953
Knight R, Ratzer ER, Fenoglio ME, Moore JT (1997) Thoracoscopic excision of mediastinal parathyroid adenomas: a report of two cases and review of the literature. Am Coll Surg 185:481–485
Lesser T, Bartel M (1999) Videothoracoscopic excision of mediastinal parathyroid adenoma. Eur J Surg 165:395–397
Randone B, Costi R, Scatton O, Fulla Y, Bertagna X, Soubrane O, Bonnichon P (2010) Thoracoscopic removal of mediastinal parathyroid glands: a critical appraisal of an emerging technique. Ann Surg 251:717–721
Kumar A, Kumar S, Aggarwal S, Kumar R, Tandon N (2002) Thoracoscopy: the preferred method for excision of mediastinal parathyroids. Surg Laparosc Endosc Percutan Tech 12:295–300
Iihara M, Suzuki R, Kawamata A (2012) Thoracoscopic removal of mediastinal parathyroid lesions: selection of surgical approach and pitfalls of preoperative and intraoperative localization. World J Surg 36:1327–1334
Wei B, Inabnet W, Lee JA, Sonett JR (2011) Optimizing the minimally invasive approach to mediastinal parathyroid adenomas. Ann Thorac Surg 92:1012–1017
Wild JL, Weigel T, Chen H (2006) The need for intraoperative parathyroid hormone monitoring during radioguided parathyroidectomy by video-assisted thoracoscopy (VATS). Clin Nucl Med 31:9–12
O’Herrin JK, Weigel T, Wilson M, Chen H (2002) Radioguided parathyroidectomy via VATS combined with intraoperative parathyroid hormone testing: the surgical approach of choice for patients with mediastinal parathyroid adenomas? J Bone Miner Res 17:1368–1371
Minamiya Y, Saito H, Ito M, Motoyama S, Katayose Y, Ogawa J (2009) Radio-guided thoracoscopic surgery with 99mTc-methoxy-isobutylisonitrile for treating an ectopic mediastinal parathyroid adenoma in an adolescent girl. Gen Thorac Cardiovasc Surg 57:657–659
Alesina PF, Moka D, Mahlstedt J, Walz MK (2008) Thoracoscopic removal of mediastinal hyperfunctioning parathyroid glands: personal experience and review of the literature. World J Surg 32:224–231
Lu HI, Chou FF, Chi SY, Huang SC (2015) Thoracoscopic removal of hypertrophic mediastinal parathyroid glands in recurrent secondary hyperparathyroidism. World J Surg 39:400–409
Profanter C, Schmid T, Prommegger R, Bale R, Sauper T, Bodner J (2004) Robot-assisted mediastinal parathyroidectomy. Surg Endosc 18(5):868–870
Brunaud L, Ayav A, Bresler L, Schjött B (2008) Da Vinci robot-assisted thoracoscopy for primary hyperparathyroidism: a new application in endocrine surgery. J Chir (Paris) 145:165–167
Harvey A, Bohacek L, Neumann D, Mihaljevic T, Berber E (2011) Robotic thoracoscopic mediastinal parathyroidectomy for persistent hyperparathyroidism: case report and review of the literature. Surg Laparosc Endosc Percutan Tech. doi:10.1097/SLE.0b013e31820607be
Karagkounis G, Uzun DD, Mason DP, Murthy SC, Berber E (2014) Robotic surgery for primary hyperparathyroidism. Surg Endosc 28:2702–2707
Bilezikian JP, Khan KA, Potts JT (2009) Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the third international workshop. J Clin Endocrinol Metab 94:335–339
Acknowledgments
The authors want to thank to Univadis (www.univadis.es) for his kind cession of use of base images for creating Fig. 4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. JM Martos-Martínez, C Sacristan Pérez, M Pérez-Andres, VM Duran-Muñoz-Cruzado, V Pino-Díaz, and FJ Padillo-Ruiz have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Martos-Martínez, J.M., Sacristán-Pérez, C., Pérez-Andrés, M. et al. Prevertebral cervical approach: a pure endoscopic surgical technique for posterior mediastinum parathyroid adenomas. Surg Endosc 31, 1930–1935 (2017). https://doi.org/10.1007/s00464-016-5197-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5197-y