Summary
Background
Primary hyperparathyroidism (HPT) is one of the most common endocrine disorders. The standard treatment is surgical removal via a cervical incision. In rare cases, abnormal parathyroid tissue may be present in the mediastinum and therefore inaccessible through the standard incision.
Case report
A 57-year-old female presented in our clinic with high ionized calcium and high parathyroid hormone levels. A technetium-99m sestamibi scan showed a focal mass in the superior mediastinum. A single-stage cervical exploration and video-assisted mediastinoscopic (VAM) removal of the intrathoracic ectopic parathyroid adenoma was performed.
Results
Our approach proved to be successful. There were no surgical complications and the patient was discharged on postoperative day 2.
Conclusion
We suggest that in the case of occult mediastinal hyperfunctioning parathyroid tissue, a VAM is a valuable extension of the standard explorative neck surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary hyperparathyroidism (HPT) is one of the most common endocrine disorders, and it is an important cause of hypercalcaemia. The frequency of the various parathyroid lesions underlying the hyperfunction is as follows: adenoma 85–95 %, primary hyperplasia 5–10 % [1]. The treatment of HPT is surgical removal. The standard approach is via a cervical incision.
Abnormal, hypersecreting parathyroid glands are found in ectopic locations in up to 15 to 20 % of patients. A small portion of these ectopic glands will be found in the mediastinum at a location that precludes removal through the traditional cervical incision [2]. Other approaches include traditional methods, such as thoracotomy, median sternotomy and manubriotomy. However, minimally invasive procedures, such as video-assisted thoracoscopy (VATS), the da Vinci robotic system and video-assisted mediastinoscopy (VAM), are becoming more popular. We describe the VAM approach combined with the standard exploration of the neck.
Case presentation
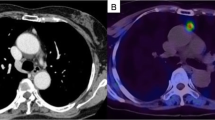
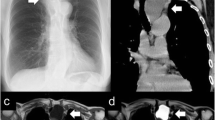
A 57-year-old female presented in our clinic with high ionized calcium (1.41 mmol/l) and high parathyroid hormone levels (85.1 ng/l). The patient underwent an ultrasound scan and a technetium-99m sestamibi scan for precise preoperative localization of the parathyroid lesion. The latter showed a focal mass in the left paratracheal area above the superior margin of the aortic arch (Fig. 1).
The operation was performed via Kocher’s incision. Careful revision of the parathyroid glands in their usual anatomical location with normal findings was followed by VAM revision of the left paratracheal area with the mass found inferiorly to the thymus. The mass was removed using blunt dissection and coagulation. A perioperative biopsy described the mass as a parathyroid tumour, which, together with a drop in the intact Parathyroid hormone (PTH) level (from 8.97 to 4.26 pmol/l) suggested a successful removal of the ectopic parathyroid lesion. The operative time was 65 minutes.
Histopathological report confirmed that the patient had a 10 × 6 × 4 mm adenoma of the parathyroid gland. On postoperative day 1, the ionized calcium (1.21 mmol/l) level returned to the normal range. On postoperative day 2, the Redon drainage tube was removed and the patient was discharged. There were no surgical complications.
Discussion
Primary hyperparathyroidism is one of the most common causes of hypercalcaemia. The standard treatment for HPT is surgical removal via a cervical incision. Abnormal, hypersecreting parathyroid glands are found in ectopic locations in up to 15 to 20 % of patients [2]. The presence of a mediastinal hyperfunctioning parathyroid gland is a rare condition that occurs in about 1 to 2 % of cases [3]. In these rare cases parathyroid tissue may not be accessible through the cervical incision; therefore, other surgical methods should be adopted. Sternotomy and thoracotomy remain the traditional surgical approaches for such cases. However, less invasive techniques are becoming more popular. Reports describing successful removal of hyperfunctioning parathyroid tissue by means of VATS [4], VAM [5] and the da Vinci robotic system [6] can be found. Both VATS and the da Vinci robotic system proved to be safe and effective, but require several keyhole incisions, single-lung ventilation and often chest drain insertion. The da Vinci robotic system is significantly more expensive in comparison to other methods. VAM is cost effective, offers short theatre time and short hospital stay. Another advantage of VAM is the ability to use a previous site of incision in cases of reoperation, which is beneficial from the cosmetic point of view.
We present our case of a successful single-stage cervical exploration and VAM removal of an intrathoracic ectopic parathyroid adenoma. We consider the use of technetium-99m sestamibi scan to be of paramount importance in localizing the hyperfunctioning parathyroid mass preoperatively, and suggest it should be used in preference to MR and CT imaging.
Conclusion
We suggest that VAM is a valuable extension of standard explorative neck surgery when operating on patients with mediastinal hyperfunctioning parathyroid tissue, particularly for cases in which imaging doesn’t show the localization of the adenoma and bilateral neck exploration gives negative results. This combined approach eliminates the necessity of reoperation and only requires a single incision, with obvious benefits to both patients and the healthcare provider.
References
Robbins SL, Kumar V, Cotran RS. Robbins and Cotran pathologic basis of disease. Philadelphia: Saunders Elsevier; 2010. p 1127.
Harvey A, Bohacek L, Neumann D, Mihaljevic T, Berber E. Robotic thoracoscopic mediastinal parathyroidectomy for persistent hyperparathyroidism: case report and review of the literature. Surg Laparosc Endosc Percutan Tech. 2011;21(1):e24–7.
Alesina PF, Moka D, Mahlstedt J, Walz MK. Thoracoscopic removal of mediastinal hyperfunctioning parathyroid glands: personal experience and review of the literature. World J Surg. 2008;32(2):224–31.
Amer K, Khan AZ, Rew D, Lagattolla N, Singh N. Video assisted thoracoscopic excision of mediastinal ectopic parathyroid adenomas: a UK regional experience. Ann Cardiothorac Surg. 2015;4(6):527–34.
Tcherveniakov P, Menon A, Milton R, Papagiannopoulos K, Lansdown M, Thorpe JA. Video-assisted mediastinoscopy (VAM) for surgical resection of ectopic parathyroid adenoma. J Cardiothorac Surg. 2007;2:41.
Ismail M, Maza S, Swierzy M, et al. Resection of ectopic mediastinal parathyroid glands with the da Vinci robotic system. Br J Surg. 2010;97(3):337–43.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
P. Libánský, D. Yershov, S. Adámek, J. Šimonek, M. Fialová, J. Kubinyi and R. Lischke state that there are no conflicts of interest.
Ethical standards
All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Rights and permissions
About this article
Cite this article
Libánský, P., Yershov, D., Adámek, S. et al. Video-assisted mediastinoscopic removal of ectopic parathyroid adenoma combined with standard cervical exploration. Eur Surg 48, 315–317 (2016). https://doi.org/10.1007/s10353-016-0413-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-016-0413-5