Abstract
Background
Laparoscopic adrenalectomy (LA) has become the standard technique for most indications. The aim of this study was to determine the predictive factors of intra- and postoperative complications in order to inform the orientation of patient to a surgeon with more experience in adrenal surgery.
Methods
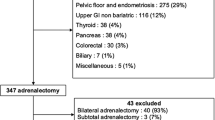
From January 1994 to December 2013, 520 consecutive patients benefited from LA at Huriez Hospital, Lille, France. Each complication was graded according to the Dindo–Clavien-grade scale. The predictive factors of complications were determined by logistic regression.
Results
Fifty-two surgeons under the supervision of 5 senior surgeons (individual experience >30 LA) participated. Postoperative complications with a grade of ≥2 occurred in 52 (10 %) patients (29 (5.6 %) medical, 19 (3.6 %) surgical, and 4 (0.8 %) mixed complications) leading to 12 (2.3 %) reoperations. There was no postoperative death. Intraoperative complication happened in 81 (15.6 %) patients responsible for conversion to open adrenalectomy (OA) [odds ratio (OR) 13.9, CI 95 % 4.74–40.77, p < 0.001]. History of upper mesocolic or retroperitoneal surgery was predictive of intraoperative complication (OR 2.02, 1.05–3.91, p = 0.036). Lesion diameter ≥45 mm was predictive of intraoperative complication (OR 1.94, 1.19–3.15, p = 0.008), conversion to OA (OR 7.46, 2.18–25.47, p = 0.001), and adrenal capsular breach (OR 4.416, 1.628–11.983, p = 0.004). Conversion to OA was the main predictive factor of postoperative complications (OR 5.42, 1.83–16.01, p = 0.002). Under adequate supervision, the surgeon’s individual experience and initial adrenal disease were not considered predictive of complications.
Conclusion
Lesion diameter over 45 mm is the determinant parameter for guidance of patients to surgeons with more extensive experience.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Since first description by Gagner et al. [1], laparoscopic adrenalectomy (LA) has become the standard technique for most indications compared to open adrenalectomy (OA) [2–4]. Several studies have described the outcomes of this technique and tried to point out risk factors of complications or conversion [5–7]. With the increasing diffusion of laparoscopy, many surgeons perform this procedure even if they have poor experience or came from a no-referral surgical department [8, 9]. The aim of the present study was to determine the predictive factors of intra- and postoperative complications.
Materials and methods
From January 1994 to December 2013, all patients who underwent laparoscopic adrenalectomy by lateral approach (LTA) at Huriez Hospital, Lille, France, were included. We created a retrospective database. Demographic and morphologic data, past abdominal or retroperitoneal surgery, thromboembolic risk factor, American Society of Anesthesiologists (ASA) score, morphologic and hormonal characteristics of adrenal tumor, intra- and postoperative parameters and outcomes, and histological diagnosis were analyzed.
All patients underwent a complete preoperative checkup including a complete endocrine evaluation associated with a morphologic evaluation by multidetector computed tomography (CT) or magnetic resonance imagery (MRI). If necessary functional imagery as [75se]cholesterol, [131I]metaiodobenzylguanidine scintigraphy or [18F]fluorodeoxyglucose positron emission tomography (FDG-PET) was performed. The only contraindication for LA was the suspicion of invasive malignancy.
Generally speaking, preoperative preparation was done by calcic inhibitors for pheochromocytoma, spironolactone, and potassium counterbalance for Conn’s syndrome and anticortisolic agents for Cushing’s syndrome.
A postoperative complication was defined as an unexpected or undesired postoperative course, each graded according to the Dindo–Clavien-grade scale [10]. For statistical analysis, we only considered postoperative complications with grade superior or equal to 2, and the type was further defined as medical or surgical. A surgical complication was defined as directly related to the surgical procedure, and a medical complication as depending on another factor. An intraoperative complication was defined as any medical or surgical undesirable event describe in the operative report.
As the main operator was considered the surgeon who performed the entire procedure or led to an undesirable event resulting in a change of operator. For each surgeon, we classified adrenalectomies chronologically and made statistical analysis calculating the median of individual experience. We also divided this variable in two groups (junior surgeon ≤30 adrenalectomies, senior surgeon >30 adrenalectomies) using as cut-off the numbers with the largest difference in complication outcomes established due to a ROC curve.
Surgical procedure
LA was carried out by classical approach described by Gagner et al. [1], with the patient in flank position, using subcostal approach with 3 trocars for left adrenalectomy and 1 more trocar for liver retraction when facing a right adrenalectomy. When necessary, conversion to laparotomy was made by an ipsilateral subcostal incision. Nasogastric suction was used during the operation but was abandoned at the end of procedure. Patients received systematically prophylaxis for deep vein thrombosis, and antibiotic prophylaxis was administered only for Cushing’s syndrome. All patients operated for Cushing’s syndrome or having a bilateral adrenalectomy received hydrocortisone pre and postoperatively. Normal diet and mobilization were initiated on the first postoperative day.
Statistical analysis
Statistical analyses were performed with SPSS 20.0 for Mac OS X (SPSS Inc., Arlington, Virginia). Continuous variable was expressed as the mean ± SD (min–max). Categorical data were compared with the Chi-square analysis or Fisher’s exact test, as appropriate, and continuous data with the Mann–Whitney U test or Student t test. A bilateral p value <0.05 was considered statistically significant. Variables with a p value <0.2 in univariate analysis were considered for multivariate model using a downward stepwise linear or logistic regression analysis. We verified the calibration of the logistic regression models using the Hosmer–Lemeshow test. The area under the ROC curve was calculated from the empirical curve (connection of each point of the graph that corresponds to a specific threshold). Tumor size and individual experience threshold were calculated from binomial approximation.
Results
Population
From January 1994 to December 2013, 520 patients (220 male and 300 female) with a median age of 49.6 years (13–95) underwent a LA. Characteristics are summarized in Table 1. 235 patients (45.2 %) had a previous surgery including 149 (28.7 %) appendectomies and 60 (11.5 %) upper mesocolic and/or retroperitoneal surgeries (20 cholecystectomies, 17 nephrectomies, 8 adrenalectomies, 7 colorectal procedures, 7 bariatric procedures, 1 antireflux procedure).
Indications for surgery, presented in Table 1, included 137 (26.3 %) pheochromocytomas, 183 (35.2 %) Conn syndrome, 98 (18.8 %) Cushing’s syndrome, 41 (7.9 %) metastatic diseases, 49 (9.4 %) non-secreting tumors, 11(2.5 %) cysts, and 1 (0.2 %) virilizing tumor. Within those diseases, 37(7.1 %) were genetically determined including 9 Von Hippel–Lindau diseases (VHL), 3 type 1 neurofibromatosis (NF1), 8 Carney complexes, 8 type 2a multiple endocrine neoplasia (MEN2a), 5 MEN1, 2 succinate dehydrogenase complex subunit D gene mutations (SDHD), 1 Bourneville tuberous sclerosis, and 1 enzymatic blocks of 21-hydroxylase.
Histological examination showed inside the 91 Cushing’s syndrome by adenoma, 9 adrenocortical carcinomas (ACC), and 1 normal adrenal gland. Inside the 175 Conn’s syndrome by adenoma, there were 1 adrenocortical carcinoma and 1 pheochromocytoma. Inside the 42 metastasis, 3 no-functional adenomas, 1 cyst, and 1 necrosis of the gland were present. Inside the 49 non-secreting tumors, 19 no-functional adenomas, 17 adrenocortical carcinomas, 4 neurogenic tumors, 1 metastasis, 1 cyst, 1 lymphoma, and 1 Cushing’s adenoma were present. The rest of histological diagnoses are presented in Table 2. A total of 64 (12 %) lesions were malignant. All histological diagnoses are summarized in Table 2.
Intraoperative outcomes
A total of 520 patients underwent LA, 227 on the right side, 253 on left side including 1 cyst fenestration, 40 bilateral, and 13 robot-assisted operations. A bilateral adrenalectomy was performed for 22 Cushing’s syndromes by hyperplasia, 13 bilateral pheochromocytomas, 2 Conn syndromes by hyperplasia, 2 bilateral non-secreting tumors, and 1 bilateral metastasis, and 19 were genetically determined. The details of all procedures are summarized in Table 3.
The mean operative time for right, left, robotic, and bilateral adrenalectomy was, respectively, 141.3 ± 62.1 (58–380), 136.7 ± 61.6 (50–365), 176.3 ± 93.3 (min–max), and 235.7 ± 65.7 (104–390) min. In multivariate analysis, length of surgery was positively correlated to the lesion diameter (r = 0.303, p < 0.001) and to robotic adrenalectomy (r = 0.058, p = 0.013).
An additional procedure was carried out for 32 patients (6.2 %) including 3 cholecystectomies, 2 nephrectomies (1 renal adenocarcinoma and 1 hemostatic nephrectomy), and 1 partial nephrectomy for a local recurrence of an adenocarcinoma, 1 caudal pancreatectomy for an associated endocrine tumor in a MEN1 syndrome, 2 hepatic wedge resections (1 for a metastasis of a medullary thyroid carcinoma and 1 for a suspicion of metastasis), 2 partial gastric resections (1 for adherences with a pheochromocytoma and 1 for a gastric diverticulum), 3 resections of paraganglioma (1 laryngeal, 1 interaortocaval and 1 juxta-adrenal), 2 thoracic drainages, 1 resection of an interaortocaval tumor, 1 colostomy closing, 4 umbilical hernia repairs, 3 samples for research, and 7 other minor procedures. Univariate analysis showed that an additional procedure was associated with a risk of conversion to open surgery (OR 3.958, 1.248–12.550, p = 0.034).
Eighty-one (15.6 %) intraoperative complications (summarized in Table 4) occurred, leading to 21 conversions to OA (4 %). Among these 21 patients, 8 presented bleeding (3 vena cava injuries, 2 renal vein injuries, 1 adrenal vein injury and 2 unspecified bleedings), 12 technical constraints (5 due to the tumor volume and 7 to tumor adherences or difficulties in dissection), and 1 respiratory intolerance of the pneumoperitoneum. Others intraoperative incidents, summarized in Table 4, especially included 19 bleedings due to 6 splenic decapsulations treated by an application of TachoSil®, 12 vein injuries, 1 splenic artery injury, 19 adrenal capsular breaches, and 14 pneumothorax, which only 2 required transthoracic drainage. Univariate and multivariate analyses showed that a history of upper mesocolic or retroperitoneal surgery (OR 2.02, 1.05 to 3.91, p = 0.036) and lesion diameter (area under the ROC curve 0.589, p = 0.011) of ≥ 45 mm (OR 1.94, 1.19–3.15, p = 0.008, Se 51 %, Sp 66 %) were associated with a risk of intraoperative complication (Fig. 1). Lesion diameter (area under the ROC curve 0.695, p = 0.004) of ≥45 mm (OR 4.416, 1.628–11.983, p = 0.004, Se 68 %, Sp 64 %) was also associated with a risk of adrenal capsular breach (Fig. 2).
The mean operative bleeding was 82.5 ml (0–5250), 7 patients (1.3 %) were transfused during the procedure, of which 4 underwent a conversion to OA. Blood transfusion was associated with a risk of conversion to OA both in univariate (OR 38.902, 8.069–187.564, p < 0.001) as in multivariate analyses (OR 12.63, 2.13–74.98, p < 0.001).
Regarding conversion to OA, in addition to blood transfusion and additional procedure, right side (OR 2.685, 0.065–6.769, p = 0.042), intraoperative complication rate (OR 16.402, 6.15–43.77, p < 0.001) and lesion diameter (area under the ROC curve 0.73, p < 0.001) of ≥45 mm (OR 7.8, 2.58–23.54, p < 0.001, Se 76.2 %, Sp 69 %) were statistically associated with univariate analysis (Fig. 3). In multivariate analysis, blood transfusion, lesion diameter ≥45 mm (OR 7.46, 2.18–25.47, p = 0.001), and intraoperative incident rate (OR 13.9, 4.74–40.77, p < 0.001) were significant predictive factors of conversion to OA.
Drainage was routinely used in our experience, 330 patients (63.3 %) benefited from it, which was associated with a risk of surgical complication only in univariate analysis (OR 4.02, 1.18–13.72, p = 0.015).
Postoperative outcomes
There was no postoperative death. We reported 100 complications in 82 patients (15.6 %). Sixty-four complications, less or equal to grade 2, happened in 52 (10 %) patients. Only 13 patients (2.5 %) had complication ≥grade 3. There was no significant difference between the complication rates in right, left, bilateral or robot-assisted adrenalectomy.
Twelve patients (2.3 %) underwent a reoperation due to complications. Five patients benefited from a thoracic drainage for 4 pneumothoraces and 1 reactional pleural effusion secondary to an infected wound hematoma which was drained at the same time. Six hemoperitoneums of which 3 were due to splenic injury leading to 2 urgent splenectomies. and 1 radioembolization of the splenic artery. The latter was complicate by an acute renal failure and respiratory distress syndrome with no need of reanimation. The 3 other hemoperitoneums were due to bleeding in the space of adrenalectomy and required an reoperation through a subcostal incision. One patient required an open reoperation for an ischemic colitis that did not require a colonic resection but was complicated by acute pancreatitis Balthazar E and acute respiratory distress syndrome.
One patient required reanimation and hyperbaric therapy following an air embolism. The postoperative outcomes are summarized in Table 5, and the details of all complications ≥grade 2 in Table 6.
Regarding overall complications, univariate analysis showed that blood transfusion (OR 12.917, 2.81–59.42, p = 0.002), conversion to open surgery (OR 7.953, 3.17–19.94, p < 0.001), intraoperative incidents (OR 2.47, 1.28–4.75, p = 0.009), and lesion diameter (p = 0.028) were associated with a risk of overall complication. In multivariate logistic regression analyses, blood transfusion (OR 6.391, 1.13–36.16, p = 0.036) and conversion to open surgery (OR 5.42, 1.83–16.01, p = 0.002) were independent predictive factors.
In univariate analysis, blood transfusion, conversion to open surgery and lesion diameter were also associated with a risk of medical complication. In multivariate analysis, blood transfusion (OR 15.2, 3.16–73.05, p = 0.001) and BMI (OR 1.07, 1.02–1.13, p = 0.009) were predictive of medical complication.
Conversion to open surgery (OR 5.94, 1.82–19.38, p = 0.011), surgical drain (OR 4.02, 1.18–13.72, p = 0.015) and intraoperative incidents (OR 3.4, 1.58–9.09, p = 0.004) were predictive of surgical complications in univariate analysis. In multivariate logistic regression, intraoperative incident (OR 3.13, 1.23–7.92, p = 0.016) was the only significantly predictive factor.
Median length of hospital stay (LOS) was 4.4 days. In multivariate logistic regression, LOS was shorter when the preoperative diagnosis was neither Cushing’s syndrome or pheochromocytoma (p = 0.039), but was higher in patients with ASA score ≥3 (p = 0.032) and with a thromboembolic risk factor (p = 0.013). Further, the increase of LOS was linked to age (r = 0.116, p = 0.003) and to lesion diameter (r = 0.026, p = 0.003).
Impact of experience
The interventions were performed by 52 different surgeons under the supervision of 5 senior surgeons (experience >30 procedures). The average number of interventions by a surgeon was 10 (min = 1, max = 104).
For statistical analysis of surgeon’s experience we excluded bilateral adrenalectomies, which were usually practiced by senior surgeons (p = 0.007 in multivariate analysis).
When individual experience was estimated by its median, greater surgeon’s experience was associated with a risk of intraoperative incident (32.72 ± 30.97 in the group of intraoperative complications and 24.95 ± 27.46 in the group of non-intraoperative complications, p = 0.048) in univariate analysis but not in multivariate logistic regression. ASA score ≥3 (p = 0.033) and the lesion diameter (r = 0.155, p < 0.001) also appeared significantly related to a higher experience in multivariate analysis.
When individual surgeon’s experience was divided in 2 groups, adrenalectomy made by junior surgeons was linked to a lower risk of intraoperative complication and conversion to open surgery. In multivariate logistic regression it was only related to a lower risk of intraoperative complication (OR 0.465, 0.28–0.78, p = 0.004).
The experience of the unit allowed a decrease in LOS (r = −0.107, p < 0.001), mean operative time (r = −0.144, p < 0.001) and capsular breach (p = 0.025) but did not change overall intra- and postoperative complications and conversion to open surgery.
Discussion
In this monocentric series of 520 consecutive patients operated for adrenal lesion, independently of diagnosis, laparoscopic adrenalectomy by transabdominal lateral approach seems to be safe with a very low rate of mortality.
In our experience, we only realized adrenalectomy by lateral transabdominal approach. The retroperitoneoscopic approach could be preferred in two cases: for bilateral lesions in order not to have to return the patient between the two procedures and for patients with past abdominal surgery [11–13]. Limitations of this approach are mainly represented by high BMI and lesion diameter over 6 cm. In this study, 40 bilateral adrenalectomies have been performed. There were no differences in rate of intraoperative incidents, surgical or medical complications and LOS. Multivariate analysis showed that a history of upper mesocolic or retroperitoneal surgery increased the risk of intraoperative incident as well as the risk of conversion and surgical complications. These results confirm what has already been described in medical literature [14]. There may be a place for the retroperitoneoscopic approach in this last case, but there is no clear evidence of superiority of one approach over the other [3, 15–17].
Robotic-assisted adrenalectomy can be performed safely and effectively with operative time and conversion rates similar to laparoscopic adrenalectomy and better ergonomics for the surgeon [18, 19]. Our study showed similar outcomes between LA and robotic-assisted adrenalectomy except for operative time, but it concerned only 13 patients representing the beginning of our experience and should be reassessed in future.
Complication rate is around 10 % in literature, major medical complications are mainly represented by respiratory disease and major surgical complication by bleeding [3–5, 7, 20]. In our study, overall postoperative morbidity ≥grade 2 of Dindo–Clavien scale rate was 10 % leading to 12 (2.3 %) reoperations but no death.
Postoperative medical complications were mainly represented by respiratory complications and various infections; BMI and intraoperative blood transfusion were both predictive factors. We insist on the importance of a fast track management to accelerate recovery. The general condition of patients influences the occurrence of postoperative outcomes [4, 21]. In our study, age, an ASA score ≥3 and a history of thromboembolic incident increased the LOS.
Postoperative surgical complications are less frequent than medical complications. Bleeding was the most frequent postoperative surgical complication causing half of the reoperations. We described 8 patients with a pancreatic complication, all were left-side adrenalectomies, 6 were ≥grade 2 of Dindo–Clavien scale including half fistula and half pancreatitis. On these 6 complications, only 1 was serious, requiring support in reanimation. Postoperative pancreatic complications are classically described but rarely found in literature [22]. In our experience they represented 11.5 % of patients with a complication ≥grade 2 of Dindo–Clavien-grade scale. Only one patient developed a renal infarction. In our surgical technique, we pay special attention to identify renal artery and vein, especially on the left side, in order to avoid this complication. Surgical drainage was frequently applied in our study (n = 330, 63.3 %) but associated with a risk of surgical complication in univariate analysis. This attitude should be given up in future in accordance with the current trend [5, 23]. In multivariate logistic regression, intraoperative incident was the only significantly predictive factor of surgical complication.
We described 82 intraoperative incidents happening in 81 patients (15.6 %) leading to 21 open surgery conversion (4 %). An important part of our study is the differentiation between an intraoperative incident, which could lead to conversion but not necessarily, and postoperative complications, which condition the postoperative outcome. In most studies [3, 4, 17], intraoperative incidents described are the only ones responsible for conversion to open surgery. Furthermore we considered capsular breach as an intraoperative incident too. These 2 reasons could explain why our rate is higher than the one found in medical literature. Bleeding was the main intraoperative incident responsible for a quarter of conversions to OA, a wound of the vena cava to the right and the renal vein to the left represented a real dangerous situation. Intraoperative pneumothorax occurred 14 times, which represented 17.3 % of intraoperative incidents; their management was easy by placing a transdiaphragmatic suction drain externalized by a trocar incision. But, within 12 postoperative reoperations, 4 (33.3 %) patients underwent a thoracic drainage for pneumothorax. First exposure of adrenal gland by section of phrenicosplenic ligament or triangular ligament of the liver must be performed carefully in order not to damage the diaphragm.
Nineteen (3.7 %) breaches of the tumor capsule happened in these patients, independently of the diagnosis. Lesion diameter over 45 mm was predictive of capsular breach. Limit the risk of breach of the tumor capsule is essential in cases of malignant lesions, especially ACC [24]. Laparoscopic resection in case of adrenocortical carcinoma can be safely proposed in expert centers but is still controversial [5, 25–27]. A stringent preoperative patient selection, a meticulous operative technique and early deliberate conversion to laparotomy could contribute to limit that risk.
The lesion diameter appeared as a very important predictive parameter of outcome. Superior to 45 mm, it was associated with a risk of intraoperative incident, capsular breach, conversion to open surgery, and it was correlated to an increase of LOS and duration of surgery. Lesion diameter over 5–6 cm has been reported as independent predictive factors for conversion, but associated with similar postoperative morbidity [6, 27–29]. Numerous studies reported the feasibility of laparoscopic adrenalectomy with lesion diameter over 10 cm [3, 5, 30, 31]. Our study confirms past described results and adjusts the critical size to a lower level. Patients with a lesion larger than 45 mm should be managed in an expert center.
Impact of initial adrenal disease on intra- and postoperative complications is still feared. We performed 137 adrenalectomy for pheochromocytoma in this study, rates of intra- and postoperative complications were similar as in others indications. Laparoscopic adrenalectomy for pheochromocytoma in an expert center is no longer a risk situation [3, 32].
Under adequate supervision by a senior surgoen, being a junior surgeon was not predictive of more intra- and postoperative complications or conversion to laparotomy. Paradoxically, the increase in experience was predictive in multivariate analysis of intraoperative complication. It could be explained by the fact that, the more experience a surgeon has, the more difficult LA he performs; lesion diameter in the group of senior surgeons was significantly higher. As it has been shown for some other procedures [33, 34], in a expert unit, standard LA, with lesion diameter smaller than 45 mm without major history of abdominal surgery could be executed by a junior surgeon without increasing the risk of overall complications. In the twenty-first century, in a high-volume unit and during their teaching, residents and junior surgeons face more interventions by laparoscopy than laparotomy. Different population-based retrospective cohort analysis from the USA [21, 35, 36] have shown contradictive results about influence of an individual surgeon’s experience on postoperative outcomes. But these studies included both LA and OA, all type of surgeons without regard of their activity, the number of adrenalectomies performed by year, and database from state discharge data.
More generally, the experience of our unit appeared more important than individual surgeon’s experience with a decrease of LOS, mean operative time thanks to a standardization of the surgical technique and reduction of capsular breach thanks to a stringent preoperative patient selection. Bergamini et al. [8] found that LA outside expert centers (<3 LA per year) was associated with a higher rate of intraoperative complication and conversion. We insist on the importance of a unit’s experience [37, 38]. Saunders et al. [9] found that surgeons who in average only operated one or two adrenalectomies a year performed 50 % of all adrenalectomies. Good practice for a surgical procedure can only be learned in an expert center.
Conclusion
Our monocentric series, including more than 500 patients has confirmed that LA is safe with a very low rate of mortality. Under adequate supervision and with a careful patient selection, individual surgeon’s experience and the initial adrenal disease did not appear to be major predictive factors of complications. The lesion diameter appeared as the main predictive parameter of complication and which, in our opinion, must guide patients to a surgeon with extensive experience in adrenal surgery.
References
Gagner M, Lacroix A, Bolté E (1992) Laparoscopic adrenalectomy in Cushing’s syndrome and pheochromocytoma. N Engl J Med 327:1033
Brunt LM et al (1996) Laparoscopic adrenalectomy compared to open adrenalectomy for benign adrenal neoplasms. J Am Coll Surg 183:1–10
Assalia A, Gagner M (2004) Laparoscopic adrenalectomy. Br J Surg 91:1259–1274
Bickenbach KA, Strong VE (2012) Laparoscopic transabdominal lateral adrenalectomy. J Surg Oncol 106:611–618
Gaujoux S et al (2011) Risk factors for conversion and complications after unilateral laparoscopic adrenalectomy. Br J Surg 98:1392–1399
Shen ZJ et al (2007) Predictive factors for open conversion of laparoscopic adrenalectomy: a 13-year review of 456 cases. J Endourol Endourol Soc 21:1333–1337
Gupta PK et al (2011) Outcomes after laparoscopic adrenalectomy. Surg Endosc 25:784–794
Bergamini C, Martellucci J, Tozzi F, Valeri A (2011) Complications in laparoscopic adrenalectomy: the value of experience. Surg Endosc 25:3845–3851
Saunders BD et al (2003) Who performs endocrine operations in the United States? Surgery 134:924–931 (discussion 931)
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Mercan S, Seven R, Ozarmagan S, Tezelman S (1995) Endoscopic retroperitoneal adrenalectomy. Surgery 118:1071–1075 (discussion 1075–1076)
Walz MK et al (2006) Posterior retroperitoneoscopic adrenalectomy—results of 560 procedures in 520 patients. Surgery 140:943–948 (discussion 948–950)
Zhang X et al (2007) Technique of anatomical retroperitoneoscopic adrenalectomy with report of 800 cases. J Urol 177:1254–1257
Seifman BD, Dunn RL, Wolf JS (2003) Transperitoneal laparoscopy into the previously operated abdomen: effect on operative time, length of stay and complications. J Urol 169:36–40
Berber E et al (2009) Comparison of laparoscopic transabdominal lateral versus posterior retroperitoneal adrenalectomy. Surgery 146:621–625 (discussion 625–626)
Rubinstein M et al (2005) Prospective, randomized comparison of transperitoneal versus retroperitoneal laparoscopic adrenalectomy. J Urol 174:442–445 (discussion 445)
Nigri G et al (2013) Meta-analysis of trials comparing laparoscopic transperitoneal and retroperitoneal adrenalectomy. Surgery 153:111–119
Brandao LF et al (2014) Robotic versus laparoscopic adrenalectomy: a systematic review and meta-analysis. Eur Urol 65:1154–1161
Taskin HE, Berber E (2013) Robotic adrenalectomy. Cancer J Sudbury Mass 19:162–166
Henry JF, Sebag F, Iacobone M, Hubbard J, Maweja S (2002) Lessons learned from 274 laparoscopic adrenalectomies. Ann Chir 127:512–519
Park HS, Roman SA, Sosa JA (2009) Outcomes from 3144 adrenalectomies in the United States: which matters more, surgeon volume or specialty? Arch Surg Chic Ill 1960(144):1060–1067
Cougard P, Peix JL, Peschaud F, Goudet P (2001) Acute pancreatitis after bilateral laparoscopic adrenalectomy in patients with ectopic ACTH syndrome. Ann Chir 126:336–338
Gurusamy KS, Samraj K, Mullerat P, Davidson BR (2007) Routine abdominal drainage for uncomplicated laparoscopic cholecystectomy. Cochrane Database Syst Rev. doi:10.1002/14651858.CD006004.pub3
Icard P et al (2001) Adrenocortical carcinomas: surgical trends and results of a 253-patient series from the French Association of Endocrine Surgeons study group. World J Surg 25:891–897
Donatini G et al (2014) Long-term survival after adrenalectomy for stage I/II adrenocortical carcinoma (ACC): a retrospective comparative cohort study of laparoscopic versus open approach. Ann Surg Oncol 21:284–291
Brix D et al (2010) Laparoscopic versus open adrenalectomy for adrenocortical carcinoma: surgical and oncologic outcome in 152 patients. Eur Urol 58:609–615
Porpiglia F et al (2010) Retrospective evaluation of the outcome of open versus laparoscopic adrenalectomy for stage I and II adrenocortical cancer. Eur Urol 57:873–878
Walz MK et al (2005) Endoscopic treatment of large primary adrenal tumours. Br J Surg 92:719–723
Parnaby CN et al (2008) The role of laparoscopic adrenalectomy for adrenal tumours of 6 cm or greater. Surg Endosc 22:617–621
Gagner M, Pomp A, Heniford BT, Pharand D, Lacroix A (1997) Laparoscopic adrenalectomy: lessons learned from 100 consecutive procedures. Ann. Surg. 226:238–246 (discussion 246–247)
Lezoche E et al (2008) Perioperative results of 214 laparoscopic adrenalectomies by anterior transperitoneal approach. Surg Endosc 22:522–526
Shen WT, Grogan R, Vriens M, Clark OH, Duh Q-Y (2010) One hundred two patients with pheochromocytoma treated at a single institution since the introduction of laparoscopic adrenalectomy. Arch Surg Chic Ill 1960(145):893–897
Donkervoort SC, Dijksman LM, Versluis PG, Clous EA, Vahl AC (2014) Surgeon’s volume is not associated with complication outcome after laparoscopic cholecystectomy. Dig Dis Sci 59:39–45
Yamamoto M et al (2013) Evaluating the learning curve associated with laparoscopic left hemicolectomy for colon cancer. Am Surg 79:366–371
Stavrakis AI, Ituarte PHG, Ko CY, Yeh MW (2007) Surgeon volume as a predictor of outcomes in inpatient and outpatient endocrine surgery. Surgery 142:887–899 (discussion 887–899)
Turrentine FE et al (2007) Adrenalectomy in Veterans Affairs and selected university medical centers: results of the patient safety in surgery study. J Am Coll Surg 204:1273–1283
Begg CB, Cramer LD, Hoskins WJ, Brennan MF (1998) Impact of hospital volume on operative mortality for major cancer surgery. JAMA 280:1747–1751
Birkmeyer JD, Skinner JS, Wennberg DE (2002) Will volume-based referral strategies reduce costs or just save lives? Health Aff Proj Hope 21:234–241
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Thibaut Coste, Robert Caiazzo, Fanelly Torres, Marie Christine Vanthygem, Bruno Carnaille, and François Pattou have no conflicts of interest or financial ties to disclose.
Additional information
An erratum to this article is available at http://dx.doi.org/10.1007/s00464-017-5437-9.
Rights and permissions
About this article
Cite this article
Coste, T., Caiazzo, R., Torres, F. et al. Laparoscopic adrenalectomy by transabdominal lateral approach: 20 years of experience. Surg Endosc 31, 2743–2751 (2017). https://doi.org/10.1007/s00464-016-4830-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-4830-0