Abstract
Background
Chronic pain is a common complication arising after conventional open herniorrhaphy and to a lesser extent postlaparoscopic inguinal hernia repairs as groin incision is avoided. Although published studies support elimination of mesh fixation during endoscopic procedures, the vast majority of surgeons will still recommend it by fear of encountering increased recurrence rates, if omitted. Regrettably, penetrating staple or tack fixation devices are the preferred methods to secure the mesh and cannot be applied at the level of the triangles of ‘doom’ and ‘pain’ where hernia tends to reoccur the most. This ongoing prospective cohort study aimed to confirm the safety and advantages of fibrin glue, as a substitute to staple mesh fixation during totally extraperitoneal (TEP) inguinal hernia repair.
Methods
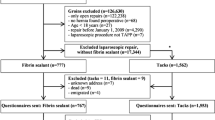
Over a 10-year period, 703 patients underwent 1000 elective TEP inguinal hernia repairs. Mesh fixation was achieved using exclusively fibrin sealant. Patients were reviewed at 2, 6 weeks and thereafter on an ad hoc basis if judged necessary until complete resolution of their symptoms. Quality of life (QoL) was assessed in a subgroup of 320 patients using the Carolina Comfort Scale (CCS).
Results
No conversion to open surgery was observed. There were three cases of major morbidities and no mortality. Three months after surgery, only seven patients (1 %) experienced chronic groin or testicular discomfort and none of them required prescription painkillers. When using the CCS, at 2 weeks 93.1 % of the patients were either satisfied or very satisfied with their outcome. This satisfaction index increased up to 99.2 % at 6 weeks post surgery. Finally, only eight hernia recurrences (1.1 %) were reported, of which five occurred during the first month of the study.
Conclusion
Fibrin glue mesh fixation of inguinal hernia during TEP repair is extremely safe and reliable, with a very high satisfaction index for the patients and limited risk of developing chronic pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Inguinal hernia repair is probably the most commonly performed procedure in general surgery worldwide, and since the turn of the twenty-first century, minimally invasive techniques such as transabdominal preperitoneal (TAPP) and totally extraperitoneal (TEP) approaches have been gaining ground to the point where many surgeons would now consider them as the preferred methods for surgical treatment of inguinal hernias. Recognized advantages over the ‘gold standard’ open Lichtenstein repair procedure include the ability to diagnose and repair associated occult, femoral, and obturator hernias, quicker recovery and faster return to normal physical activities, reduction in postoperative pain, decreased risk of developing chronic groin pain, and improved cosmetic appearances [1–3].
Also the incidence of chronic groin pain is reduced by half in patients treated laparoscopically, a significant number of them will still experience inadequate outcome with an estimated risk of 6 % (range 1–16 %) [4]. It is recognized that the use of anchoring devices such as staples or tacks, commonly employed to secure prosthetic mesh to the groin, increase this risk, and in serious cases staples removal may be necessary [5]. Unfortunately, mechanical fixation offers a false sense of security, as the mesh cannot be anchored inferiorly at the level of the triangles of doom and pain that correspond to the area where hernia recurrence tends to occur the most [6]. Several recent published studies have also recommended nonfixation of the mesh in order to minimize the incidence of nerve or vascular injury from the tacks, while at the same time maintaining comparable hernia recurrence rate [7]. This may provide an acceptable option in selected cases, especially in the presence of small inguinal hernias, but we must then accept the associated risk of early mesh displacement, folding from postoperative extraperitoneal seroma or hematoma formation, or mesh shrinkage that could not only cause hernia recurrence but also cause chronic pain [8].
To address this problem, alternative techniques have recently emerged including fibrin sealant as an adhesive for mesh fixation and resulting in less reported postoperative pain [9]. This was corroborated by a personal study showing that fibrin glue was safe and reliable, with a very limited risk of developing postoperative chronic groin pain [10]. The aim of this ongoing prospective cohort study was to validate our initial findings with a significantly larger group of patients, but also and mainly to assess postoperative satisfaction levels and quality of life (QoL) using a comprehensive scoring system specifically designed for hernia repairs.
Materials and methods
Data from 703 patients undergoing elective TEP inguinal hernia repair were prospectively collected over a 10-year period, between February 2005 and February 2015.
Surgical procedure
All the repairs were performed under the care of a single surgeon experienced in this procedure. The repair technique used in this study has been described previously [11]. Patients were asked to empty their bladder prior to entering the theater. A urinary catheter was only used on rare occasions in male patients with current medical history of symptomatic benign prostatic hypertrophy (BPH). A single dose of 1 g intravenous cephalothin antibiotic was administered preoperatively. Sequential calf compressors and subcutaneous 20 mg enoxaparin were routinely used for deep venous thrombosis prophylaxis. CO2 insufflation pressure was set at 8 mmHg. Key points of this procedure included: lateral incision of the arcuate line if the lower edge of the posterior rectus sheath was extending too caudally in order to improve endoscopic view and create sufficient space for future mesh placement, generous exposure of the psoas muscle inferiorly along with the genitofemoral and the lateral femoral cutaneous nerves, as well as the femoral canal and obturator foramen to exclude any associated hernia formation (Fig. 1A, B). In the presence of a moderate (M2)- or large (M3)-size medial (direct) hernia as per the European Hernia Society (EHS) classification [12], the weakened transversalis fascia (TF) was plicated with a pretied loop of 2/0 Polydioxanone (PDS) (Endoloop® Ligature, Ethicon Endo-Surgery, Cincinnati, OH) (Fig. 1C) in order to reduce the incidence of postoperative seroma formation [13].
A Endoscopic view of a left femoral hernia (o) in a female patient, left round ligament (RL); B endoscopic view of a right obturator (o) and Gimbernat’s (←) hernias in a male patient, external iliac vein (EIV), vas deferens (VD), and spermatic vessels (SV); C Endoloop of PDS secured at the base of the inverted transversalis fascia (TF) after reduction in a direct right inguinal hernia, right epigastric vessels (EV); D final endoscopic view of bilateral Parietex meshes overlapping medially in the retropubic space and midline, following fibrin sealant fixation
A preshaped nonabsorbable large-size polypropylene mesh (Bard 3D® Max, Davol, Cranston, UK) was initially used at the beginning of this study. This prosthesis was progressively replaced by an anatomical preshaped polyester mesh with a lateral slit (Parietex™ Anatomical Mesh 15 × 10 cm, TECT 1510ADP2, Covidien, Mansfield, MA), due to its softness, the fact that it is hydrophilic and can be adequately secured around the spermatic cord structures in men, offering a generous prosthetic overlap laterally to further prevent recurrence.
Fibrin sealant (Tisseel, Baxter, Deerfield, IL, USA) containing fibrinogen and thrombin was used for mesh fixation of unilateral or bilateral hernia (1–2 ml of fibrinogen and 1–2 ml of thrombin with a final volume of 2–4 ml). The glue was mainly applied on the inferior border of the mesh at the level of the triangles of ‘doom’ and ‘pain’ (Fig. 1D). Since May 2008, fibrin sealant has been applied using a disposable spraying applicator device (DuploSpray MIS, Baxter, Deerfield, IL, USA) that has significantly decreased the amount of time necessary to achieve adequate mesh fixation due to accelerated fibrin polymerization process.
Patient follow-up and evaluation of patient satisfaction
Patients were reviewed at 2 and 6 weeks following surgery. If deemed necessary, subsequent visits were also organized. Postoperative satisfaction index and QoL were assessed in a subset of patients able to read in English and complete the questionnaire using a comprehensive scoring system [Carolinas Comfort Scale (CCS)] specifically designed for hernia repairs and measuring severity of pain, mesh sensation, and movement limitations in eight different categories, resulting in a maximum score of 115 [14]. Total scores for each respondent were converted to a percentage of the applicable maximum. A slight modification was made by adding the symptom of sneezing to item 5 of the original CCS score, as in the author’s experience this was a frequently reported aggravator [15]. The CCS was categorized into ‘very satisfied’ (≤0.05), ‘satisfied’ (>0.05 to ≤0.03), ‘neutral’ (>0.3 to ≤0.6), and ‘unsatisfied’ (>0.6) as previously reported [10]. Mann–Whitney U test or Kruskal–Wallis test was used to analyze the continuous CCS scores at 2 and 6 weeks to compare between type of surgery (unilateral or bilateral), type of hernia, sex, and age (≤50 or >50 years). All collected data with identifying information were stored in a secured database.
Results
Between February 2005 and February 2015, 703 patients underwent 1000 consecutive inguinal hernia repairs using an endoscopic TEP approach. The majority of the patients were male (646 males and 57 females), and the median age for the overall patient cohort was 49 years (range 16–87) (Table 1). A total of 406 patients (57.8 %) had unilateral hernias, and 297 patients (42.2 %) had bilateral inguinal hernias. Of the 1000 consecutive inguinal hernia repairs, 737 hernias (73.7 %) were indirect (lateral), 88 (8.8 %) were direct (medial), and 154 (15.4 %) were mixed. In 14 cases (1.4 %), the type was unspecified, but all of them were recurrent hernias and 7 cases (0.7 %) of Sportsman’s hernias were also included. Associated pathologies are summarized in Table 1. A total of 41 patients had an associated patent processus vaginalis, which was divided and closed at the proximal end with an Endoloop of PDS during TEP repair. During surgery, 51 femoral and 16 obturator hernias were also identified, reduced, and simultaneously repaired with mesh. Over the course of the study, no intraoperative complications were observed and there was no conversion to open surgery, but a single case (0.1 %) had to be completed by transabdominal preperitoneal (TAPP) approach. A total of 443 Bard 3D® Max and 557 Parietex™ meshes were used.
Postoperative complications
Overall, 38 postoperative morbidities were recorded in 37 patients (5.3 %) and are summarized in Table 2. These included three patients (0.4 %) who encountered a major complication. The first one developed a rectus sheath hematoma 1 week after surgery and treated by ligation of his inferior epigastric artery. The second patient presented with an early postoperative preperitoneal hernia formation, as a result of a slipped pretied Endoloop of PDS that was initially used to close the peritoneal sac opening after TEP repair of an inguinoscrotal hernia. This patient was successfully treated laparoscopically and made a full recovery with no further complaint [16]. The last complication was a bladder injury that occurred in a 76-year-old female patient with a past medical history of hysterectomy and who underwent TEP repair of bilateral inguinal (recurrent right) and femoral hernias. At the time of the surgery, the surgeon was unaware that the patient had previously undergone over 30 years ago a ‘ventrofixation’ of her bladder onto the anterior abdominal wall.
Out of the remaining 34 patients who developed 35 minor complications, there was only one (0.14 %) who developed symptoms of chronic groin pain. The pain was mild, and the patient was able to go back to work with the help of minor analgesic taken on demand. At 6 months postoperative, he no longer experienced any pain or discomfort.
During the first visit (2 weeks), 57 male patients experienced intermittent testicular discomfort that was already present prior to surgery in five of them (52/641: 8.8 %). The pain was mainly mild in intensity, and 35 of them reported complete resolution of their symptoms at the subsequent visit (6 weeks). Only six patients (0.9 %) still complained of chronic testicular discomfort 3 months after surgery and are therefore included in Table 2. In all these cases, the pain level was low and intermittent. No one required any regular analgesic. One patient (0.14 %) developed mild paresthesia, and four others (0.6 %) experienced transitory numbness in the distribution of the lateral femoral cutaneous nerve of the thigh. This uncommon event might have happened due to overzealous lateral dissection toward the anterosuperior iliac spine during recurrent hernia repair and should be avoidable as the nerve is readily visible. We reported nine cases (1.3 %) of superficial wound infections, but the operating surgeon only confirmed six of them. Oral antibiotic was initiated by the GP in three patients, prior to the first postoperative visit.
Hernia repair defects
From 2008, when judged necessary plication of the attenuated TF with a pretied Endoloop of 2/0 PDS was performed in the presence of a direct hernia defect. This included a total of 151 direct hernias plicated in 126 patients and categorized into three subgroups following the EHS classification: 5 M1 (defect ≤1.5 cm), 91 M2 (defect >1.5 cm but <3 cm), and 55 M3 (defect ≥3 cm). At first visit, three patients with a M3 defect were found to have a very small palpable but not symptomatic groin seroma that was not visible on inspection alone. All seromas were no longer detectable at 6 weeks postsurgery. Only one female patient operated on for a very large defect and associated with a recurrent incisional hernia from previous lower midline postlaparotomy scar subsequently developed a symptomatic groin seroma that was treated conservatively [13]. One patient had an early hernia recurrence as a result of rupture of the Endoloop after closure of a M3 defect. In this case, a groin hematoma developed following restarting of clopidogrel only 2 days postsurgery.
Systematic classification of indirect inguinal hernia according to the EHS was only introduced in June 2009. A total of 526 indirect hernia repair defects were reported as follows: 277 L1 (defect ≤1.5 cm), 177 L2 (defect >1.5 cm but <3 cm), and 72 L3 (defect ≥3 cm). In the larger (L3) indirect defects, the risk of developing clinically palpable seroma was not uncommon. In one case of very large right-sided inguinoscrotal hernia, we observed an early recurrence within few months due to a complete protrusion of the lateral aspect of the mesh through the defective posterior wall of the inguinal canal.
Patient satisfaction index
Postoperative satisfaction levels were assessed in 320 patients using the CCS comprehensive scoring system. At 2 weeks postoperative, 55 and 38.1 % of the patients reported being either ‘very satisfied’ or ‘satisfied’ with their treatment, respectively. This satisfaction level continued to improve at the second (6 weeks) visit with 86.5 and 12.7 % of patients’ satisfaction level, respectively (Table 3).
At 2 and 6 weeks postsurgery, patients that underwent bilateral surgery had higher CCS scores than patients that underwent unilateral surgery (p = 0.01 at 2 weeks and p = 0.02 at 6 weeks). While the CCS scores were higher in the bilateral group, the mean and median were at least in ‘satisfied’ range or better for both groups at 2 weeks. At 6 weeks, in the bilateral group, CCS scores were higher, and similarly, the mean and median scores were within the ‘very satisfied’ range (Table 4).
Patients 50 years or less were more likely to have higher CCS scores than patients greater than 50 years old, at 2 and 6 weeks postsurgery (p < 0.001 at both follow-ups). The means and medians in both age groups were at least in the ‘satisfied’ range at 2 weeks and at 6 weeks were in the ‘very satisfied’ range (Table 4).
Finally, eight hernia recurrences were reported in this series (1.1 %). Five of these occurred early in the study, all on the left side. One of the remaining three cases was diagnosed 6 years after his initial TEP repair, which was performed only 2 months after the start of this study. The last two cases occurred quite prematurely, one following mesh repair of a large right-sided inguinoscrotal hernia and the remaining one as a result of rupture of an Endoloop used to plicate the TF, secondary to the development of groin hematoma.
Discussion
With regard to primary unilateral inguinal hernia, defining whether the open tension-free Lichtenstein mesh repair is still to be considered, the ‘gold standard’ is a matter of debate with the recent explosion of novel quite appealing prosthetic materials and techniques in this field of surgery. At a more fundamental level, it seems that the divergence between supporters of the conventional ‘open’ versus ‘laparoscopic’ approaches will persist even though recent evidence suggests that minimally invasive techniques may offer better outcomes [1, 4].
The only agreed consensus is that laparoscopic or endoscopic approaches, such as TAPP and TEP, are more suitable for treatment of bilateral or recurrent inguinal hernia (after previous anterior approach) but only if performed by surgeons expert in those types of techniques [17]. Of importance, it also offers the possibility to concomitantly repair a contralateral occult inguinal hernia that may be present in >20 % of the cases [18] or an associated femoral hernia especially in female patients who carry a significantly higher risk [19, 20]. In our study, 42.2 % of the patient population was treated for bilateral inguinal hernias. This ratio seems relatively high when looking at larger case series quoting a proportion of around 30–35 %, as compared to unilateral repair [21, 22]. This discrepancy is easily explained by the fact that since 2011 we have been performing routine groin US of the contralateral side, in patients suitable for TEP repair with clinically unilateral inguinal hernia. If the US confirmed the presence of an associated ‘occult’ groin hernia, prophylactic repair was recommended [23]. When looking at postoperative morbidities, we only encountered three major complications (0.4 %) that required re-intervention. This incidence is significantly lower than previously reported series [21], and due to the fact that all our cases were performed under the care of one surgeon (Berney CR) with a vast experience in such technique. TEP or TAPP repairs of inguinal hernia are very challenging procedures to learn and master, with a long and steep learning curve. This should not be underestimated [24].
During laparoscopic inguinal hernia repair tacking the mesh to the anterior abdominal wall, pubic bone and Cooper’s ligament still remain the preferred method among surgeons, although this is associated with increased risk of vascular and nerve injuries, or chronic pubalgia [5, 25]. As a promising alternative, there is now good clinical evidence to support that fibrin sealant, which possesses similar tensile strength to staples [26], significantly decreases postoperative morbidity and incidence of chronic groin pain [9]. Its use for mesh fixation has also been recommended in the updated Guidelines of the International Endohernia Society (level 1B) [17]. In our series, only 1 % of our 703 patients reported chronic groin or testicular pain. These findings corroborate previously reported figures with an estimated risk of 6 % (range 1–16 %) [4]. At 2 weeks postsurgery, 52 out of the 641 (8.1 %) male patients who did not complain of preoperative testicular pain reported it as a de novo symptom. In most cases, a complete resolution of the pain was observed at the time of the second visit and only six patients complained of chronic mild intermittent testicular discomfort that lasted over 3 months, but not requiring any regular painkiller.
Of the 320 patients assessed for postoperative QoL using the CCS comprehensive scoring system, 55 and 38.1 % of them were either ‘very satisfied’ or ‘satisfied’ at their first visit. This satisfaction level improved even further at the second (6 weeks) visit with 86.5 and 12.7 % of patients’ satisfaction level, respectively. While the CCS scores were higher in patients 50 years or less compared to patients greater than 50, and higher in the bilateral surgery group compared to the unilateral surgery group at both 2 and 6 weeks, the average and median scores in each group and at both time points were at least in the ‘satisfied’ to ‘very satisfied’ range.
The vast majority of the patients (94.7 %) assessed for postsurgical satisfaction level (CSS) were treated using a very soft preshaped macroporous and hydrophilic polyester mesh (Parietex™) known to promote tissue ingrowth, alike fibrin sealant, therefore limiting prosthetic contraction when compared with polypropylene material [27]. It appears that the choice of the mesh combined with fibrin sealant fixation may in part explain such positive outcome. Albeit several recent series advocate no-mesh fixation motivated by similar short-term hernia recurrence rate and reduction in the overall cost of the procedure [7, 22], most surgeons still feel that there is a need for securing the prosthesis. Not only for large hernia defects, but also for smaller ones as there is always a potential risk of mesh dislocation or folding that may lead to hernia recurrence if not properly fixed, as previously discussed [28]. In their large 5203 TEP series, Tamme et al. [22] mentioned that staple fixation of the mesh was only used in exceptional cases involving a highly enlarged internal ring, meaning for large indirect hernias, or on inadequate extent of medial dissection because of previous surgery. Unfortunately, they did not say in how many of those cases a staple device was used. No mention either on the percentage of moderate to large indirect (L2 or L3) defects included in this study, which is crucial as the larger the defect the more critical the mesh fixation may become. Similarly, what about mesh fixation in the presence of larger direct (M2, or M3) inguinal defects? The recently updated Guidelines of the International Endohernia Society recommends mesh fixation for L3 or M3 defects [17].
There are two categories of mesh fixation, either using glue (fibrin sealant, synthetic cyanoacrylate) or mechanical (staples, tacks, sutures). Due to the fact that glue is noninvasive, another valuable advantage is that it can be applied safely on the lower aspect of the mesh at the level of the triangles of doom and pain. The direct long-term benefit is probably reduction in the risk of hernia recurrence as the inferomedial and inferolateral portion of the mesh remains adequately fixed [6]. The only way to confirm it is to design a prospective study with long-term (>5 years) follow-up, which would be extremely difficult to complete. Until then, only personal series may offer a partial answer. Alternative to fibrin glue is synthetic cyanoacrylate as recommended by others [29]. We personally favor human fibrin as it is completely biocompatible and nontoxic, is hemostatic as it mimics the final stages of the coagulation cascade, and promotes tissue ingrowth and wound healing, as it gets totally resorbed within 10–14 days. In comparison, cyanoacrylate produces an exothermic (polymerization occurs at around 45 °C) reaction when applied to the tissues, has no hemostatic or healing value, and may further prevent homogenous tissue ingrowth in the prosthesis as it never completely degrades.
Finally, five of the eight hernia recurrences that were reported in this series (1.1 %) occurred in the early phase of the study and attributed to the initial learning curve of our technique. The last two events happened quite prematurely, one following treatment of a very large right-sided inguinoscrotal hernia that the patient has had for over 15 years and in retrospect that should have been repaired with a significantly larger prosthesis. The remaining one was more material-related as the Endoloop used to plicate the weakened TF ruptured after the patient developed a postoperative groin hematoma from restarting his treatment of clopidogrel too prematurely. Since then, it has been common practice to apply a second pretied suture at the base of the inverted TF when the defect is too large (M3). Although our hernia recurrence rate was very low, this result should be taken with caution due to the difficulty to maintain adequate long-term follow-up.
Conclusion
The end results of this 10-year continuing prospective cohort study confirm previous findings that mesh fixation with fibrin sealant during endoscopic TEP inguinal hernia repair is safe and reliable, with very high satisfaction index as verified by improved QoL, but also negligible risk of developing acute or chronic postoperative groin or testicular pain. To the majority of laparoscopic surgeons who are still routinely securing their mesh, it is now safe to say that fibrin sealant should be the preferred fixation method for groin hernias rather than any invasive mechanical device, such as staples or tacks.
References
Langeveld HR, van’t Riet M, Weidema WF, Stassen LP, Steyerberg EW, Lange J, Bonjer HJ, Jeekel J (2010) Total extraperitoneal inguinal hernia repair compared with Lichtenstein (the LEVEL-Trial): a randomized controlled trial. Ann Surg 251(5):819–824
Gong K, Zhang N, Lu Y, Zhu B, Zhang Z, Du D, Zhao X, Jiang H (2011) Comparison of the open tension-free mesh-plug, transabdominal preperitoneal (TAPP), and totally extraperitoneal (TEP) laparoscopic techniques for primary unilateral inguinal hernia repair: a prospective randomized controlled trial. Surg Endosc 25(1):234–239
Dulucq JL, Wintringer P, Mahajna A (2011) Occult hernias detected by laparoscopic totally extra-peritoneal inguinal hernia repair: a prospective study. Hernia 15(4):399–402
Aasvang E, Kehlet H (2005) Chronic postoperative pain: the case of inguinal herniorrhaphy. Br J Anaesth 95(1):69–76
Wong J, Anvari M (2001) Treatment of inguinodynia after laparoscopic herniorrhaphy: a combined laparoscopic and fluoroscopic approach to the removal of helical tackers. Surg Lap Endosc Percutan Tech 11(2):148–151
Lowham AS, Filipi CJ, Fitzgibbons RJ Jr, Stoppa R, Wantz GE, Felix EL, Crafton WB (1997) Mechanisms of hernia recurrence after preperitoneal mesh repair. Traditional and laparoscopic. Ann Surg 225(4):422–431
Teng YJ, Pan SM, Liu YL, Yang KH, Zhang YC, Tian JH, Han JX (2011) A meta-analysis of randomized controlled trials of fixation versus nonfixation of mesh in laparoscopic total extraperitoneal inguinal hernia repair. Surg Endosc 25(9):2849–2858
Amid PK (2004) Radiologic images of meshoma: a new phenomenon causing chronic pain after prosthetic repair of abdominal wall hernias. Arch Surg 139(12):1297–1298
Fortelny RH, Petter-Puchner AH, Glaser KS, Redl H (2012) Use of fibrin sealant (Tisseel/Tissucol) in hernia repair: a systematic review. Surg Endosc 26(7):1803–1812
Berney CR, Yeo AE (2013) Mesh fixation with fibrin sealant during endoscopic totally extraperitoneal inguinal hernia approach: a review of 640 repairs. Hernia 17(6):709–717
Putnis S, Berney CR (2012) Totally extraperitoneal repair of inguinal hernia: techniques and pitfalls of a challenging procedure. Langenbecks Arch Surg 397(8):1343–1351
Miserez M, Alexandre JH, Campanelli G, Corcione F, Cuccurullo D, Pascual MH, Hoeferlin A, Kingsnorth AN, Mandala V, Palot JP, Schumpelick V, Simmermacher RK, Stoppa R, Flament JB (2007) The European hernia society groin hernia classification: simple and easy to remember. Hernia 11(2):113–116
Berney CR (2012) The Endoloop technique for the primary closure of direct inguinal hernia defect during the endoscopic totally extraperitoneal approach. Hernia 16(3):301–305
Heniford BT, Walters AL, Lincourt AE, Novitsky YW, Hope WW, Kercher KW (2008) Comparison of generic versus specific quality-of-life scales for mesh hernia repairs. J Am Coll Surg 206(4):638–644
Knox RD, Berney CR (2015) A preoperative hernia symptom score predicts inguinal hernia anatomy and outcomes after TEP repair. Surg Endosc 29(2):481–486
Berney CR (2012) Unusual clinical presentation of a preperitoneal hernia following endoscopic totally extraperitoneal inguinoscrotal hernia repair. Hernia 16(5):585–587
Bittner R, Montgomery MA, Arregui E, Bansal N, Bingener J, Bisgaard T, Buhck H, Dudai M, Ferzli GS, Fitzgibbons RJ, Fortelny RH, Grimes KL, Klinge U, Kockerling F, Kumar S, Kukleta J, Lomanto D, Misra MC, Morales-Conde S, Reinpold W, Rosenberg J, Singh K, Timoney M, Weyhe D, Chowbey P (2015) Update of guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal Hernia (International Endohernia Society). Surg Endosc 29(9):289–321
Griffin KJ, Harris S, Tang TY, Skelton N, Reed JB, Harris AM (2010) Incidence of contralateral occult inguina hernia found at the time of laparoscopic trans-abdominal pre-peritoneal (TAPP) repair. Hernia 14(4):345–349
Putnis S, Wong A, Berney C (2011) Synchronous femoral hernias diagnosed during endoscopic inguinal hernia repair. Surg Endosc 25(12):3752–3754
Old OJ, Kulkarni SR, Hardy TJ, Slim FJ, Emerson LG, Bulbulia RA, Whyman MR, Poskitt KR (2015) Incidental non-inguinals hernias in totally extra-peritoneal hernia repair. Ann R Coll Surg Engl 97(2):120–124
Köckerling F, Schug-Pass C, Adolf D, Keller T, Kuthe A (2015) Bilateral and unilateral total extraperitoneal inguinal hernia repair (TEP) have equivalent early outcomes: analysis of 9395 cases. World J Surg 39(8):1887–1894
Tamme C, Scheidbach H, Hampe C, Schneider C, Köckerling F (2003) Totally extraperitoneal endoscopic inguinal hernia repair (TEP). Surg Endosc 17(2):190–195
Bochkarev V, Ringley C, Vitamvas M, Oleynikov D (2007) Bilateral laparoscopic inguinal hernia repair in patients with occult contralateral inguinal defects. Surg Endosc 21(5):734–736
Berney CR (2012) Mastering the totally extraperitoneal technique is a prerequisite for successful inguinal hernia repair. ANZ J Surg 82(4):196–197
Olmi S, Erba L, Bertolini A, Scaini A, Croce E (2006) Fibrin glue for mesh fixation in laparoscopic transabdominal preperitoneal (TAPP) hernia repair: indications, technique, and outcomes. Surg Endosc 20(12):1846–1850
Katkhouda N, Mavor E, Friedlander MH, Mason RJ, Kiyabu M, Grant SW, Achanta K, Kirkman EL, Narayanan K, Essani R (2001) Use of fibrin sealant for prosthetic mesh fixation in laparoscopic extraperitoneal inguinal hernia repair. Ann Surg 233(1):18–25
Gonzalez R, Fugate K, McClusky D 3rd, Ritter EM, Lederman A, Dillehay D, Smith CD, Ramshaw BJ (2005) Relationship between tissue ingrowth and mesh contraction. World J Surg 29(8):1038–1043
Schwab R, Schumacher O, Junge K, Binnebosel M, Klinge U, Becker HP, Schumpelick V (2008) Biomechanical analyses of mesh fixation in TAPP and TEP hernia repair. Surg Endosc 22(3):731–738
Kukleta JF, Freytag C, Weber M (2012) Efficiency and safety of mesh fixation in laparoscopic inguinal hernia repair using n-butyl cyanoacrylate: long-term biocompatibility in over 1300 mesh fixations. Hernia 16(2):153–162
Acknowledgments
The authors did not receive any grant or sponsorship for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The authors Prof Christophe Berney and Joseph Descallar have no conflicts of interest nor corporate/commercial relationships to disclose.
Rights and permissions
About this article
Cite this article
Berney, C.R., Descallar, J. Review of 1000 fibrin glue mesh fixation during endoscopic totally extraperitoneal (TEP) inguinal hernia repair. Surg Endosc 30, 4544–4552 (2016). https://doi.org/10.1007/s00464-016-4791-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-4791-3