Abstract
Background
The Carolinas comfort scale (CCS) is an ideal tool for assessing patients’ quality-of-life post hernia repair, but its use has been barely investigated preoperatively. The aim was to quantify preoperative symptoms and assess their relevance in predicting postoperative clinical outcomes following totally extraperitoneal (TEP) inguinal hernia repair.
Methods
The CCS was modified for preoperative use (modified or MCCS) by omitting mesh sensation questioning. Data collection was prospective over a 16 months period. (M)CCS questionnaires were completed preoperatively and at 2 then 6 weeks post repair. Intraoperative findings were also recorded. One hundred and four consecutive patients consented for TEP repair were included using a fibrin glue mesh fixation technique.
Results
All three questionnaires were completed by 88 patients (84.6 %). Preoperative MCCS scores did not differ with age, obesity, the presence of bilateral or recurrent inguinal herniae or hernia type. Higher MCCS grouping [OR 4.3 (95 % CI 1.5–12.6)] and the presence of bilateral herniae [OR 8.5 (1.2–61.8)] were predictors of persisting discomfort at 6 weeks, with lower scores on MCCS [OR 16.4 (3.9–67.6), obesity (OR 9.9 91.6–63.2)] and recurrent hernia repair [OR 11.4 (1.4–91.0)] predicting increased discomfort at 2 weeks versus preoperatively. MCCS scores were inversely correlated with the size of a direct defect (r −0.42, p = 0.011) but did not differ with the intraoperative finding of an incidental femoral and/or obturator hernia. Female sex was strongly associated with recognition of a synchronous incidental hernia (5 vs 57 %, p = 0.001).
Conclusions
Pre- and post-operative scoring of hernia specific symptoms should be considered as part of routine surgical practice, to counsel patients on their expectations of pain and discomfort post repair and to select those who might be more appropriate for a watchful waiting approach. Females with inguinal hernia warrant complete assessment of their groin hernial orifices intraoperatively due to a high rate of synchronous incidental hernia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Inguinal hernia is one of the commonest pathologies presenting to general surgeons, and repair of this condition is a major burden on health care budgets. With the advent of modern mesh repair techniques demonstrating low recurrence and complication rates, postoperative outcomes in terms of symptoms and quality-of-life (QoL) during recovery have become a key focus of the modern hernia literature. The Carolinas comfort scale (CCS) is a validated Likert-type questionnaire developed specifically for mesh hernia repair that discriminates well between satisfied and unsatisfied patients, has demonstrated utility in detecting recurrence, and is an ideal means of addressing QoL and comfort post hernia repair [1–3].
Laparoscopic repair of inguinal hernia has lower reported rates of acute and chronic postoperative groin discomfort than open approaches, with a quicker return to work, and is recommended by guidelines for repair of recurrent and bilateral herniae [4]. It also adds the advantage of being able to visualise all the hernial orifices in the region with a single minimally invasive approach. Arguments against laparoscopic repair include an increased cost of disposables the need for general anaesthesia, a steeper learning curve and a higher but overall negligible rate of major visceral and vascular complications [4–6]. Thus uptake of laparoscopic repair techniques has not been universal and a policy of selective use is recommended by published guidelines [4].
Watchful waiting has been suggested as part of management algorithms for asymptomatic and minimally symptomatic hernia [4, 7], as the absolute rate of incarceration per year is low, coupled with a finite morbidity of repair, especially in terms of chronic groin discomfort. Furthermore, the total cost to the health system may be higher with early repair [7].
If a selective approach to offering laparoscopic repair is to be followed by surgeons, then selection of suitable patients must consider the advantages of improved QoL and minimised discomfort leading to an early return to work. Likewise the minimally symptomatic hernia that is appropriate for a watchful waiting approach requires definition. Despite this, the preoperative assessment of symptoms and QoL, although a key focus postsurgery in the recent literature, is infrequently reported and quantified. Preoperative pain and the relationship to postoperative outcomes has been investigated by a number of studies, although broader measures such as activity and QoL impairment measures have been infrequently investigated [8].
The aim of this study was to demonstrate the utility of completing a quantitative pre-operative assessment using a modified hernia specific CCS questionnaire (modified or MCCS) in terms of audit of surgical outcomes, and whether such a preoperative evaluation can be predictive of postoperative discomfort, or of hernia anatomy, to help in guiding clinical decision making and management algorithms.
Materials and methods
The study was of a prospective cohort design including a total of 104 consecutive TEP inguinal hernia repairs over a 16 months period from November 2011 to March 2013. The study was conducted in accordance with good clinical practice guidelines and with consent for data collection. All repairs were performed under the care of a single surgeon and using a standardised technique of pre-formed anatomical prosthesis (ParietexTM Anatomical Mesh 15 × 10 cm, TECT 1510 ADP2, Covidien, Mansfield, MA, USA) placement with fibrin glue fixation in all patients (TISSEAL [Fibrin Sealant], Baxter, Deerfield, IL, USA) and Endoloop closure of the sac of medial defects as previously described [9, 10]. Any incidentally found femoral or obturator hernias were covered by the mesh, or where large occluded by a pre-formed mesh plug (Perfix Plug® small, Bard Davol Inc., Warwick, RI, USA). Intraoperative assessment of the hernia anatomy was described as per the EHS classification guidelines [11].
The CCS was modified for pre-operative use (MCCS) by omitting the questions related to mesh sensation in each of the 8 domains, resulting in a maximum score of 75. Total scores for each respondent were then converted to a percentage of the applicable maximum. A slight modification was made by adding the symptom of sneezing to item five of the original CCS score, as in the author’s experience this was a frequently reported aggravator. A simple VAS score was also collected simultaneously with the questionnaire on each occasion (Table 1).
Data were collected during clinical consultation pre-, and at 2 and 6 weeks postoperatively. All scores were converted to a percentage of the maximum possible score. A priori selection and recording of patient characteristics of age, the presence of bilateral or recurrent herniae, BMI > 30, a disturbed pre-peritoneal plane (by previous TEP, radical prostatectomy, appendectomy or other relevant lower abdominal surgery) was based on previously reported and suspected factors influencing reported symptoms or suggesting a technically difficult repair. To facilitate further analysis and create clinically meaningful severity groupings, the CCS and MCCS scores were stratified according to symptom groups, namely Very Satisfied (<5 %), Satisfied (<30 %), Somewhat satisfied and Unsatisfied, consistent with the author’s previously published study [9].
Baseline MCCS scores were analysed by logistic regression and the change in preoperative, 2 and 6 weeks percentages by repeated measures ANOVA, with the above covariates. To investigate the predictive ability and clinical utility of the preoperative MCCS, these symptom cohorts were examined in terms of the following clinically relevant questions:
Postoperative outcomes by multivariate logistic regression, specifically:
-
(a)
6 week outcomes, in terms of being either very satisfied or not.
-
(b)
2 week outcomes, in terms of reporting increased discomfort from preoperative levels.
Hernia anatomy, in terms of
-
(a)
The presence of an occult femoral or obturator hernia at operation, and.
-
(b)
EHS classification of the hernia anatomy found at operation.
Analysis was performed by SPSS software v21 (SPSS Inc, Chicago, Il). Non-parametric tests where available were used for non-normally distributed data, p was set at 0.05 and two-tailed.
Results
Of the 104 consecutive patients who were assessed preoperatively, 102 completed the initial 2 weeks postoperative CCS and 88 (84.6 %) at the second (6 week) follow-up visit.
The baseline characteristics were compared across these sample populations to determine whether those who failed to provide a full set of scores differed from the remaining cohort (Table 2). There was a significant difference in terms of age, with those who failed to provide a full postoperative symptom assessment being younger, but otherwise the patient cohorts were similar.
Pre-operative scores ranged from 0 to 85.3 %, with a median of 17.3 % (mean 23.9 %), 2 weeks scores ranged from 0 to 69.4 %, with a median of 4 % (mean 8.3 %), and 6 weeks scores ranged from 0 to 37.4 %, with a median 0 % (mean 2.4 %). The breakdown of patients by symptom severity grouping, at each time point, is found in Table 3.
There was no significant difference in preoperative MCCS scores on linear regression by the a priori factors of age, sex, obesity, the presence of bilateral or recurrent inguinal herniae, a disturbed tissue plane from previous surgery, or by the EHS hernia anatomy classification found at repair.
On repeated measures ANOVA, there was a clear improvement in the subsequent self reported symptoms of patients undergoing TEP inguinal hernia repair as measured by pre- and post-operative (M)CCS scores at both the 2 and 6 weeks mark (p < 0.001).
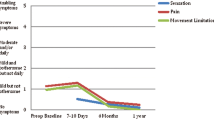
There was a significant correlation between preoperative MCCS scores and the reported discomfort postoperatively. However, and as expected, the minimally symptomatic MCCS group demonstrated significantly increased scores at 2 weeks before improving at 6 weeks post surgery (Fig. 1). The a priori selected factors of age, the presence of bilateral or recurrent herniae, a disturbed pre-peritoneal plane and obesity once again did not have a statistically significant influence on sequential scores on multivariate analysis, neither did the hernia defect by size, nor type.
On individual patient basis, 21 % reported increased symptoms at 2 weeks compared to preoperative levels, reducing to just two cases (3.8 % of complete respondents) at 6 weeks.
Predicting hernia anatomy
Hernia anatomy as found intraoperatively and defined by the EHS classification [11] was compared to preoperative symptoms. Reported discomfort did not differ preoperatively between patients with direct and/or indirect hernia of any size, whether unilateral or bilateral (Mann–Whitney U test). However, preoperative symptoms were significantly and negatively correlated with increasing size of a direct inguinal hernia when present (Pearson R − 0.42, p = 0.011, Fig. 2B). A positive correlation was also noted with indirect defects, particularly bilateral defects, but this was not statistically significant (Fig. 2A).
Overall, 9 % were found to have an occult femoral, obturator or Gimbernat’s hernia at TEP repair. MCCS scores did not significantly differ preoperatively between these patients and those without an occult hernia found at surgery, but as has been previously reported [12] female sex was a strong predictor of finding a synchronous occult hernia (present in 5.2 % males vs 57.1 % females, p = 0.001, Chi square test). Post operative symptoms did not significantly differ after the reduction with or without plug occlusion (in a single case) of these clinically occult herniae where present at both 2 weeks (p = 0.661, Mann–Whitney U test) and 6 weeks (p = 0.736).
Predicting the likelihood of increased discomfort at 2 weeks postoperatively
Patients who reported increased symptoms at 2 weeks, compared to baseline preoperatively, were compared to those who reported improved symptoms by multivariate logistic regression. The minimally symptomatic group by preoperative MCCS (‘Very Satisfied’ patients) had an OR of 16.2 (95 % CI 3.9–67.6) of increased discomfort at 2 weeks follow-up. Obesity [OR 9.9 (1.6–63.2)] and recurrent hernia [OR 11.4 (1.4–91.0)] were also significant predictors of increased discomfort in this early postoperative period.
Predicting the likelihood of a less than satisfied outcome at 6 weeks
Patients who were very satisfied, or not, at 6 weeks post surgery were compared by multivariate logistic regression. The degree of discomfort preoperatively on MCCS was a significant predictor of the presence of persisting symptoms at 6 weeks, with each increment from very satisfied to unsatisfied associated with an OR of 4.3 (95 % CI 1.5–12.6). Undergoing bilateral hernia repair was also predictive of persisting discomfort [OR 8.5 (1.2–61.8)] at the 6 weeks follow-up visit.
Discussion
Preoperative symptom severity as measured by the modified CCS is a significant predictor of reported postoperative symptoms, and is inversely correlated with the size of a direct defect when present. To our knowledge this is the first report of a hernia specific CCS-based questionnaire used in the preoperative and early postoperative setting for inguinal hernia repair, although a CCS-based scale has been reported in the assessment of ventral hernia repair techniques [13] and a similar but non-specific questionnaire has been used preoperatively in the investigation of post-herniorrhaphy pain risk factors [8].
The MCCS scale used in this study could predict which patient was likely to report persisting symptoms at 6 weeks post surgery, and who was likely to report increased discomfort from baseline in the acute postoperative period at 2 weeks. Pain and discomfort is a subjective experience, varied by multiple factors relating to an inherent susceptibility of the patient, the stimulus, and the expression and interpretation of the response. This analysis of a hernia specific perioperative symptom scoring system with a consistent repair technique performed under the care of a single surgeon, suggests that these inherent patient factors are indeed key to the reported discomfort post repair, and that a risk of postoperative discomfort can be assessed preoperatively. This finding is clinically relevant in counselling and consenting patients on their expectations of QoL and discomfort post repair, and in selecting patients suitable for a watchful waiting approach. This may also be of relevance in guiding both the clinician and patient regarding the significance of unexpectedly persisting discomfort in the late postoperative period. Although the aim of this study was not to investigate chronic pain or discomfort (being defined as that persisting over a 3 months period), it has been reported that early postoperative as well as local preoperative pain is a risk factor for chronic pain [14, 15]. Our findings are consistent with those of Aasvang et al. [8] who identified that preoperative activity impairment as measured by the 13 point activity assessment scale, coupled with reported local pain and response to a noxious heat stimulus, were significant preoperative risk factors that predicted post-herniorraphy pain .
Additionally, this study identified a clear inverse correlation of preoperative MCCS scores with hernia anatomy, in terms of the size of a direct defect where present. Furthermore, given that indirect inguinal herniae may be up to ten times more likely to obstruct than direct herniae according to consensus guidelines [4], preoperative symptom scoring could lend support to deciding upon watchful waiting in patients with direct defects. The explanation for this phenomenon may be indirect, related to confounders such as increased age, or a direct relationship between laxity of the abdominal wall and Hasselbach’s triangle, and the degree of stimulation of pain receptors and thus discomfort.
Femoral, inguinal and obturator hernia commonly coexist, with in-common local biomechanical and systemic risk factors. As has been previously reported in the literature [12] and recommended by international guidelines [4], laparoscopic repair of female patients with inguinal herniae should be considered due to a high rate of associated femoral herniae. Although preoperative symptoms did not differ in the presence of such additional hernia, our study reinforces this view with 57 % of females undergoing repair in this series having otherwise clinically occult femoral and/or obturator herniae.
The 16 % drop out rate at 6 weeks follow-up is a concern in this study, even though we attempted to contact these missing patients for telephone assessment to ensure consistent reporting methodology and a consistent effect of observer and expectation bias in data collection. Patients lost to followup tended to be of younger age, which previous studies suggest is a risk factor for greater post-operative pain. This bias could be considered being counteracted by the author’s experience that satisfied patients are more likely to be those that decline to attend a second follow-up visit. Some reporting bias may also have been introduced, as the data was not collected in an anonymous blinded fashion. However, the operative technique and data collection as mentioned above was consistent across the study population. This standardised TEP repair technique has been previously reported in detail [9, 10]. The low overall rate of symptoms at 6 weeks postsurgery in this study compares favourably with the reported literature, especially as measured using a sensitive tool such as the CCS, highlighting the minimal postoperative discomfort of TEP repair.
Conclusion
Quantitative preoperative as well as postoperative assessment should be strongly considered by surgeons when consenting patients for hernia repair. Both the modified and standard CCS are ideal tools for this purpose. Preoperative symptoms are correlated to both early and late postoperative discomfort and hernia anatomy. Quantifying discomfort preoperatively as an addition to routine clinical examination can provide clinically useful data to guide both surgeon and patient in the consent process. Obese patients, or those with recurrent or bilateral herniae are at increased risk for early postoperative discomfort. Preoperative symptoms were not predictive of an incidental femoral and/or obturator hernia. However as has been previously reported, females with inguinal herniae should undergo a laparoscopic repair technique due to the high incidence of these synchronous herniae in this population, for which a TEP approach is ideal.
References
Heniford BT, Walters AL, Lincourt AE, Novitsky YW, Hope WW, Kercher KW (2008) Comparison of generic versus specific quality-of-life scales for mesh hernia repairs. J Am Coll Surg 206:638–644. doi:10.1016/j.jamcollsurg.2007.11.025
Belyansky I, Tsirline VB, Klima DA, Walters AL, Lincourt AE, Heniford TB (2011) Prospective, comparative study of postoperative quality of life in TEP, TAPP, and modified lichtenstein repairs. Ann Surg 254:709–715. doi:10.1097/SLA.0b013e3182359d07
Zaborszky A, Gyanti R, Barry JA, Saxby BK, Bhattacharya P, Hasan FA (2011) Measurement issues when assessing quality of life outcomes for different types of hernia mesh repair. Ann R Coll Surg Engl 93:281–285. doi:10.1308/003588411X13020150727480
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, Lange D, Fortelny R, Heikkinen T, Kingsnorth A, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Miserez M (2009) European hernia society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403. doi:10.1007/s10029-009-0529-7
Smart P, Castles L (2012) Quantifying the cost of laparoscopic inguinal hernia repair. ANZ J Surg 82:809–812. doi:10.1111/j.1445-2197.2012.06189.x
McCormack K, Scott NW, Go PM, Ross S, Grant AM, EU Hernia Trialists Collaboration (2003). Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev (1):CD001785. doi:10.1002/14651858.CD001785
Turaga K, Fitzgibbons RJ Jr, Puri V (2008) Inguinal hernias: should we repair? Surg Clin N. Am 88:127–138. doi:10.1016/j.suc.2007.11.004
Aasvang EK, Gmaehle E, Hansen JB, Gmaehle B, Forman JL, Schwarz J, Bittner R, Kehlet H (2010) Predictive risk factors for persistent postherniotomy pain. Anesthesiology 112:957–969. doi:10.1097/ALN.0b013e3181d31ff8
Berney CR, Yeo AET (2013) Mesh fixation with fibrin sealant during endoscopic totally extraperitoneal inguinal hernia approach: a review of 640 repairs. Hernia 17:709–717. doi:10.1007/s10029-012-1034-y
Putnis S, Berney CR (2012) Totally extraperitoneal repair of inguinal hernia: techniques and pitfalls of a challenging procedure. Langenbecks Arch Surg 397:1343–1351. doi:10.1007/s00423-012-0999-4
Miserez M, Alexandre JH, Campanelli G, Corcione F, Cuccurullo D, Pascual MH, Hoeferlin A, Kingsnorth AN, Mandala V, Palot JP, Schumpelick V, Simmermacher RKJ, Stoppa R, Flament JB (2007) The European hernia society groin hernia classification: simple and easy to remember. Hernia 11:113–116. doi:10.1007/s10029-007-0198-3
Putnis S, Wong A, Berney C (2011) Synchronous femoral hernias diagnosed during endoscopic inguinal hernia repair. Surg Endosc 25:3752–3754. doi:10.1007/s00464-011-1781-3
Colavita PD, Tsirline VB, Belyansky I, Walters AL, Lincourt AE, Sing RF, Heniford BT (2012) Prospective, long-term comparison of quality of life in laparoscopic versus open ventral hernia repair. Ann Surg 256:714–723. doi:10.1097/SLA.0b013e3182734130
Bansal VK, Misra MC, Babu D, Victor J, Kumar S, Sagar R, Rajeshwari S, Krishna A, Rewari V (2013) A prospective, randomized comparison of long-term outcomes: chronic groin pain and quality of life following totally extraperitoneal (TEP) and transabdominal preperitoneal (TAPP) laparoscopic inguinal hernia repair. Surg Endosc 27:2373–2382. doi:10.1007/s00464-013-2797-7
Dennis R, O’Riordan D (2007) Risk factors for chronic pain after inguinal hernia repair. Ann R Coll Surg Engl 89:218–220. doi:10.1308/003588407X178991
Disclosures
The authors Prof. Christophe R. Berney and Dr. Robert D. Knox have no conflicts of interest, nor corporate/commercial relationships to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Knox, R.D., Berney, C.R. A preoperative hernia symptom score predicts inguinal hernia anatomy and outcomes after TEP repair. Surg Endosc 29, 481–486 (2015). https://doi.org/10.1007/s00464-014-3692-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3692-6