Abstract
Introduction
Anastomotic complications after esophagectomy are relatively frequent. The off-label use of self-expanding covered metal stents has been shown to be an effective initial treatment for leaks, but there is a paucity of literature regarding their use in cervical esophagogastric anastomoses. We reviewed our outcomes with anastomotic stenting after esophagectomy with cervical esophagogastric reconstruction.
Methods
All stents placed across cervical anastomoses following esophagectomy from 2004 to 2014 were retrospectively reviewed. Indications for surgery and stent placement were collected. For patients with serial stents, each stent event was evaluated separately and as part of its series. Success was defined as resolution of indicated anastomotic problem for at least 90 days. Complications were defined as development of stent-related problems.
Results
Twenty-three patients had a total of 63 stents placed (16 % prophylactic, 38 % leak, 46 % stricture). Sixty percent of patients had successful resolution of their initial anastomotic problem; 67 % required more than one stent. Strictures and leaks healed in 27 and 70 % of patients, respectively, at a median of 55.5 days. Stent-related complications occurred in 78 % of patients. Complications (per stent event) included 62 % migration, 11 % clinically significant tissue overgrowth, 8 % minor erosion (ulcers), and 8 % major erosion. Stents placed for stricture were more likely to result in complications, especially migration (76.7 vs. 48.5 %, p = 0.02). Preoperative chemoradiation was a significant risk factor for erosion (22.5 vs. 4.3 %, p = 0.05), but not for overall complications. Patients with major erosions had longer stent duration compared to those without (92 vs. 36 days, p = 0.14).
Discussion
Although stents are effective at controlling post-esophagectomy anastomotic leaks, they are not effective for treating strictures. Stents have high complication rates, but most are minor. Chemoradiation is a risk factor for stent erosion. Caution should be used when stent duration exceeds 2–3 months due to the risk of erosion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Anastomotic complications after esophagectomy are relatively frequent and are challenging to manage. The most common anastomotic problems after esophagectomy are leaks (3–25 %) and strictures (5–46 %) [1, 2]. In this relatively high risk, chronically ill group of patients, more minimally invasive approaches are now being used to treat complications as they arise. Submucosal injection of fibrin glue, clipping, endoscopic vacuum therapy, endoscopic insertion of transluminal drains, and other injectable have been used with varying success [3]. Over the past decade, the use of covered self-expanding metal esophageal stents has grown in popularity as a primary treatment of anastomotic leaks after esophagectomy (Fig. 1). Several studies have shown that stents can heal or control esophageal and foregut anastomotic leaks in 60–100 % of patients [1, 4–6]. In comparison, very little data exist on the use of esophageal stents to treat anastomotic strictures despite this being a growing trend. The few studies that do exist are mainly on bariatric foregut patients, and they show stricture resolution rates to be low at 12.5–33 % [5, 7]. The aim of this study was to review the role of covered metal stents after esophagectomy with cervical esophagogastric reconstruction.
Materials and methods
Patients
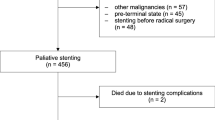
All patients who had a removable stent placed across a cervical anastomosis following esophagectomy with posterior gastric pull-up reconstruction at a single institution from April 2004 through April 2014 were retrospectively reviewed under an institutional review board (IRB)-approved protocol. Indications for surgery and stent placement were recorded. Patient demographics (age, gender, presence of preoperative chemoradiation therapy) and stent information (diameter, brand, use of stent fixation, stent duration) were collected. Stent complications were categorized as clinically significant tissue overgrowth, migration, and erosion. For patients with serial stents, each stent placement, or “stent event,” was evaluated first separately and then as part of its series per patient. Patients were allowed to take a liquid/mechanical soft diet with stents in place. Patients were followed at least every 3 months for 2 years and then annually per routine protocol.
Definitions
Leaks and strictures were diagnosed by endoscopic evaluation prompted by clinical suspicion (Fig. 2). Leaks were graded on a scale from 1 to 4 according to the classification set forth by Lerut et al. [8] (Table 1). Stents were categorized as “prophylactic” if they were placed in “at-risk” anastomosis as determined by attending surgeon within 24 h of anastomosis creation. Clinically significant tissue overgrowth was defined as hypertrophic granulation tissue caused by the stent that either created dysphagia or made stent removal difficult (Fig. 3). Minor erosion was defined as an ulceration under the stent separate from the anastomotic problem. Major erosion was defined as stent erosion into surrounding structures. Migration was defined as symptomatic proximal movement (into the cricopharyngeal area) or distal movement such that the anastomosis was found on endoscopy to be uncovered/exposed. Success was defined as clinical resolution of indicated anastomotic problem durable for at least 90 days after endoscopic resolution. A “stent event” was defined as placement of a new stent.
Stent details
The removable stents used were Polyflex esophageal stents (Boston Scientific, Natick, MA, USA) of different diameters (16, 18, and 21 mm) and lengths (9, 12, and 15 cm); fully covered Alimaxx and Endomaxx esophageal stents (Merit Medical Endotek, South Jordan, UT, USA) of different diameters (18, 20, and 22 mm) and lengths (7, 10, and 12 cm); and Wallflex esophageal stents (Boston Scientific, Natick, MA, USA) of different diameters (18 and 23 mm) and different lengths (10.3 and 10.5 cm). Appropriate stent sizes were chosen based on the conduit anatomy. Stents were routinely removed or exchanged at 3–6 week intervals (although earlier intervention was necessary in some cases due to complications such as migration). Ten of 63 stent placements had clips applied (4) or endoscopic sutures (6) placed in an effort to prevent stent migration. Three advanced foregut surgeons at our institution performed all stent placements and removals.
Statistical analysis
Comparisons were made using paired Student’s t test.
Results
Twenty-three patients had a total of 63 stents placed with an average 2.7 separate stent events per patient (67 % of patients required more than one stent placement event). Indication for surgery was esophageal malignancy in 22/23 patients with 13/23 patients receiving preoperative chemoradiotherapy. Mean age was 64.3 years, and 21/23 patients were male. Median follow-up was 839 days (16–4159).
The indication for initial stent placement was: prophylaxis (35 %), leak (35 %), and stricture (30 %). Of the eight patients with initial prophylactic stents, 2 developed leaks identified during routine stent removal; both were successfully treated with subsequent stent replacement. Five of the patients with prophylactic stent placements developed strictures. None of the patients with prophylactic stents developed a major erosion. Considering all stent events, and accounting for these clinical changes, the overall distribution of indications for stent placement was: prophylaxis (16 %), leak (38 %), and stricture (46 %). Median single stent duration was 25.5 days (IQR = 13–39.8), and median overall stent duration per patient was 62 days (IQR = 40–74.5). Stent brands included 13/63 Alimaxx, 22/63 Wallflex 6/63 Polyflex, and 8/63 Endomaxx.
Efficacy
Excluding stents placed for prophylaxis, 60 % of patients had successful resolution of their initial primary anastomotic problem. Of the 11 patients who had stents placed for strictures, healing was achieved in 27 % of patients at a median of 42 days (IQR = 32–67). Of the 10 patients stented for leaks, healing was noted in 70 % at a median of 59 days (IQR = 50.5–66) (Table 2). The distribution of leak grades is shown in Fig. 4. Leak resolution with stents by grade was: 3/4 Grade 1, 1/3 Grade 2, and 3/3 Grade 3.
Morbidity
Overall, stent-related complications occurred in 78 % of patients. Nearly all stents placed across a cervical esophagogastric anastomosis had at least one minor problem, with the average number of complications per stent event being 0.9. Complications (per stent event) included 11 % clinically significant tissue overgrowth, 62 % migration, and 16 % erosions (8 % minor, 8 % major) (see Fig. 5). Overall, 17 % of patients experienced a major erosive event. Compared to stents placed for leaks, stents placed for stricture were more likely to result in complications (80 vs. 60 %, p = 0.09), especially migration (76.7 vs. 48.5 %, p = 0.02) (see Table 3). Two of five major erosions were in patients who had stents placed for stricture without initial leak. Preoperative chemoradiation was found to be a significant risk factor for erosive events (22.5 vs. 4.3 %, p = 0.05) although not for overall complications (Table 4).
Migration did not appear to be affected by stent diameter (60% ≥ 20 vs. 64 % < 20 mm, p = 0.73) or stent fixation (50.0 % migration when stents were fixed vs. 64.2 % migration when not, p = 0.40). Larger stent diameter did not appear to affect erosion rates (20 % ≥ 20 vs. 10.7 % < 20 mm, p = 0.32). No valid trends in complications were found when comparing specific stent brands.
There were 4 deaths in the series. Two patients developed tracheoesophageal fistulas and subsequently elected to pursue hospice care. One patient died of non-stent-related complications before resolution of leak. One died of metastatic disease before stent removal. No patient died during stent placement or removal.
The median number of days to heal a leak or stricture was 55.5 days, whereas the median number or stent days leading to a major erosion was 92 days (p = 0.14) (Table 5). In stents that did not experience erosive events, median stent duration was 36 days.
Discussion
Anastomotic complications (leaks and strictures) following esophagectomy are challenging issues that plague both physician and patient. Leaks result in longer hospital stays, worse long-term outcomes, and decreased survival in already frail post-esophagectomy cancer patients [9]. Until relatively recently, re-operative surgery and conservative management were the only options for treatment, but were often associated with poor outcomes (40–100 % mortality in re-operative surgery and up to 40 % morbidity and mortality for conservative management) [4, 10]. Off-label use of esophageal stenting for anastomosis-related problems is emerging in the literature as a potentially less invasive, highly effective alternative therapy for anastomotic problems.
Rajan and colleagues recently reported their results on the safety of stenting leaks after esophageal surgery [4]. In 32 patients with stented leaks, primarily following esophagectomy, the mortality rate was 4 %, which is low compared to the reported 35–70 % mortality rate in all patients with leaks after esophagectomy. Similarly, Schweigert et al. reviewed their 10-year experience with post-esophagectomy intrathoracic anastomotic leaks and found a 24 % mortality rate in 29 patients who had leaks amenable to endoscopic stenting which was lower than their 33 % leak-associated mortality with standard surgical treatment [9]. Nguyen et al. reported 18 post-esophagectomy patients with mostly intrathoracic leaks, comparing stenting and draining with traditional management. They found stents to be effective at controlling leaks in 100 % patients [6]. Subsequently, the Cleveland Clinic published their data on 18 patients with leaks, strictures, and fistulas after mainly bariatric foregut surgery, and found an 85 % eventual resolution of anastomotic leaks and 1 of 3 strictures resolved with stenting [5]. Along these same lines, Dr. Saar and colleagues at the Mayo Clinic reported their results on stents for treating leaks and strictures after mainly bariatric foregut surgery and found only 12.5 % (2/16) resolution of strictures treated with stents and healing of leaks in 40 % (2/5) of the patients [7]. Hoeppner et al. reviewed 35 patients with esophagogastric or esophagojejunal anastomotic leaks and found stents to be associated with a 70 % healing rate. Healing rates were significantly better for intrathoracic anastomoses [1].
Despite these data, there is a paucity of literature addressing the utility of stenting across cervical esophagogastric anastomoses following esophagectomy. Our study aimed to look at this subgroup of patients. Despite showing that a majority of anastomotic problems will heal with stenting, we identified a high rate of problems. Most of the complications (90 %) are bothersome, such as stent migration, tissue overgrowth, and small erosions, and are not serious. However, with almost an 80 % stent-related complication rate, even these minor problems are quite burdensome to patients and clinicians alike.
Most importantly, we have identified a > 10 % major erosive complication rate in our patient population demonstrated by the development of tracheoesophageal fistulas and erosions into the cervical vertebrae and other major surrounding structures. Two of these patients with tracheoesophageal fistulas elected to forego further treatment, influenced by their original heavy cancer burden (advanced stage III adenocarcinoma) and exhaustion at the thought of another major surgery. While there are reports of sudden death due to exsanguination from vascular erosive events [4], luckily, we did not experience that particular complication in our population likely due to the small sample size. Our data suggest that preoperative chemoradiation (4 vs. 22 %, p = 0.02) and longer stent duration (36 days vs. 92 days, p = 0.14) may to be risk factors for erosive events.
Our experience with stenting for cervical anastomotic strictures has been disappointing. Theoretically, stenting would provide a gentler, more continuous dilation allowing for scar remodeling and healing with fewer interventions than required with serial dilations. However, nearly as many patients with stented strictures developed major erosive complications as healed. While this study was not designed to compare dilation with stenting, any potential benefit of stenting for cervical anastomotic strictures seems to be largely outweighed by the development of new problems (migration, overgrowth, and erosions).
Stenting across a cervical anastomosis is technically challenging largely dependent upon the length of the remnant esophagus. Although the data were not collected specifically in this study, most of our cervical anastomoses reside 2–4 cm distal to the cricopharyngeus muscle. This leaves considerably less real estate to anchor the stent than the general guideline of 5 cm. This is likely the main contributor to the considerable migration problem reported in our series, which at 62 % is much higher than the 8.5–47 % rate reported for other locations [1, 4, 7]. Some have suggested that delaying oral nutrition may decrease migration rates [4]. This seems to make intuitive sense, especially in cervical stents, but we routinely allow patients to have clear liquids and a mechanical soft diet shortly after stent placement in accordance with manufacturer recommendations to avoid stent cracking (personal communication). This issue needs further study before definitive conclusions can be drawn. Larger stent diameter (up to 28 mm) has also been suggested to decrease migration [4]. While we did not find a difference in migration rates between stent diameters, we did not use any stents of a similar magnitude. Theoretically, larger diameter stents could lead to more erosions in the cervical area although we did not identify a difference in erosion rates based on stent diameter greater than or <20 mm. Various fixation methods have been proposed as another method to mitigate stent migration; however, this was not an effective strategy in our study (50.0 % migration when fixed vs. 64.2 % migration when not fixed, p = 0.40), despite our initial enthusiasm in the laboratory setting [11]. Migration rates were also significantly higher in stents placed for stricture than for leaks. This may be due to stent dislodgement as the stricture’s scar softens and the lumen widens.
There are multiple potential limitations of this study. First, the sample size is small. With only 23 patients, the risk of committing a type II error is high when looking for differences between groups. Despite this, we were able to identify significance for a number of factors. Second, its retrospective nature limits comparisons between stenting and other therapies. For example, the study is not designed to compare stents to serial dilations. It is also not controlled to isolate the effects of the stents from other influences. Third, the prophylactic group is heterogeneous and due to the retrospective nature, we are unable to further stratify the specific “risk” of the anastomoses aside from labeling it “at risk.” Another potential bias in the study is the potential loss to follow-up as stent- and anastomotic-related complications can be difficult to track long term, especially in patients who go through multiple endoscopists. However, all patients with esophagectomies in our practice are cared for exclusively by three surgical endoscopists who perform all stent placements and follow-up visits for 5 years. In our experience, the incidence of further problems after clinical stability for 90 days is highly unusual.
Despite these limitations, we believe that our data should raise concerned awareness of the potential complications associated with covered stents in cervical anastomoses. Based on these results, we are now far more selective in stent placement. In general, we recommend limiting their use only to higher-grade leaks where the potential benefit mitigates the risk. We currently consider cervical strictures a contraindication to stent placement and recommend serial dilation. We are also much more vigilant about early removal (2–3 weeks) compared to our previous practice of 3–6 weeks.
Conclusion
Removable stents should be used with caution in cervical anastomoses following esophagectomy due to a high rate of minor complications and a >10 % risk of major erosion. Stenting is fairly effective at healing a majority of leaks, but not strictures. With only a 27 % success rate and 80 % complication rate, cervical strictures should be a contraindication to removable stent placement. Risk factors for erosive complications appear to be preoperative chemoradiation and longer stent duration. Regardless of indication, caution should be used when stent duration exceeds 2–3 months.
References
Hoeppner J et al (2014) Covered self-expanding stent treatment for anastomotic leakage: outcomes in esophagogastric and esophagojejunal anastomoses. Surg Endosc 28:1703–1711
Honkoop P et al (1996) Benign anastomotic strictures after transhiatal esophagectomy and cervical esophagogastrostomy: risk factors and management. J Thorac Cardiovasc Surg 6:1141–1148
Turkyilmaz A, Eroglu A, Aydin Y, Tekinbas C, Muharrem Erol M, Karaoglanoglu N (2009) The management of esophagogastric anastomotic leak after esophagectomy for esophageal carcinoma. Dis Esophagus 22(2):119–126
Rajan P et al (2014) Role of endoscopic stents and selective minimal access drainage in oesophageal leaks: feasibility and outcome. Surg Endosc 28:2368–2373
Yimcharoen P et al (2010) Endoscopic stent management of leaks and anastomotic strictures after foregut surgery. Surg Obes Relat Dis 7:628–636
Nguyen N et al (2011) Management of gastrointestinal leaks after minimally invasive esophagectomy: conventional treatments versus endoscopic stenting. J Gastrointest Surg 15:1952–1960
Puig C et al (2014) The role of endoscopic stents in the management of chronic anastomotic and staple line leaks and chronic strictures after bariatric surgery. Surg Obes Relat Dis 10:613–619
Lerut T et al (2002) Anastomotic complications after esophagectomy. Dig Surg 19:92–98
Schweigert M, et al. (2014) One decade of experience with endoscopic stenting for intrathoracic anastomotic leakage after esophagectomy: brilliant breakthrough or flash in the pan?. In: Presented at the annual scientific meeting and postgraduate course program, Southeastern Surgical Congress, Savannah, GA, February 22–25
Schweigert M, Solymosi N, Dubecz A, Stadlhuber RJ, Mus-chweck H, Ofner D, Stein HJ (2013) Endoscopic stent insertion for anastomotic leakage following oesophagectomy. Ann R Coll Surg Engl 95:43–47
Rieder E, Dunst CM, Martinec DV, Cassera MA, Swanstrom LL (2012) Endoscopic suture fixation of gastrointestinal stents: proof of biomechanical principles and early clinical experience. Endoscopy 44(12):1121–1126
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Speer, Dunst, Shada, and Swanstrom have no conflicts of interest or financial ties to disclose. Dr. Reavis is a consultant for Boston Scientific.
Rights and permissions
About this article
Cite this article
Speer, E., Dunst, C.M., Shada, A. et al. Covered stents in cervical anastomoses following esophagectomy. Surg Endosc 30, 3297–3303 (2016). https://doi.org/10.1007/s00464-015-4661-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4661-4