Abstract
Background
Social and racial disparities have been identified as factors contributing to differences in access to care and oncologic outcomes in patients with colorectal cancer. The aim of this study was to investigate national disparities in minimally invasive surgery (MIS), both laparoscopic and robotic, across different racial, socioeconomic and geographic populations of patients with rectal cancer.
Methods
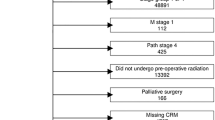
We utilized the American College of Surgeons National Cancer Database to identify patients with rectal cancer from 2004 to 2011 who had undergone definitive surgical procedures through either an open, laparoscopic or robotic approach. Inclusion criteria included only one malignancy and no adjuvant therapy. Multivariate analysis was performed to investigate differences in age, gender, race, income, education, insurance coverage, geographic setting and hospital type in relation to the surgical approach.
Results
A total of 8633 patients were identified. The initial surgical approach included 46.5 % open (4016), 50.9 % laparoscopic (4393) and 2.6 % robotic (224). In evaluating type of insurance coverage, patients with private insurance were most likely to undergo laparoscopic surgery [OR (odds ratio) 1.637, 95 % CI 1.178–2.275], although there was a less statistically significant association with robotic surgery (OR 2.167, 95 % CI 0.663–7.087). Patients who had incomes greater than $46,000 and received treatment at an academic center were more likely to undergo MIS (either laparoscopic or robotic). Race, education and geographic setting were not statistically significant characteristics for surgical approach in patients with rectal cancer.
Conclusions
Minimally invasive approaches for rectal cancer comprise approximately 53 % of surgical procedures in patients not treated with adjuvant therapy. Robotics is associated with patients who have higher incomes and private insurance and undergo surgery in academic centers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The application of minimally invasive surgery (MIS) for the treatment of colorectal cancer has increased in the last decade [1, 2]. Minimally invasive approaches include both laparoscopy and robotics. When compared to open surgery, several studies have shown equivalent oncologic results of laparoscopic surgery [3–6]. Laparoscopy also offers several short-term benefits, including shorter hospital length of stay, lower estimated blood loss and decreased postoperative pain [7]. Compared to laparoscopic surgery, the postoperative benefits and oncologic outcomes of robotic surgery in colorectal cancer have been less established, in part because of less experience and adoption of robotic surgery in this disease process [8–10]. In contrast, robotic surgery has been better established in its application to malignancies and other benign disease processes in urology and gynecology [11–13].
Although the role of robotics in colorectal surgery is not yet clearly defined, the use of robotic surgery in colorectal cancer has grown nationally [14]. With this trend, not only will the oncologic outcomes of robotic compared to both laparoscopic and open approaches be of significant interest [15], but also the evaluation of patient access to robotic surgery and the identification of associated disparities are important. Socioeconomic and racial disparities have already been reported in laparoscopic surgery for colorectal cancer [16]. Further in urologic oncology, similar disparities have characterized in minimally invasive radical prostatectomy, including both laparoscopic and robotic approaches [17]. In this study, we analyzed national disparities with respect to race, socioeconomic status and geographic location for patients with rectal cancer with respect to the robotic surgical approach as compared to open and laparoscopic surgery.
Methods
The American College of Surgeons (ACS) National Cancer Database (NCDB) captures approximately 70 % of the country’s cancer cases through its participating hospitals. Since 2004, surgical approach has been recorded and includes the open, laparoscopic, laparoscopic converted to open, robotic and robotic converted to open approaches. For the purposes of this study, we identified patients with rectal cancer treated with surgery from 2004 to 2011. Inclusion criteria included patients with only one rectal malignancy who did not receive any chemotherapy or radiation treatment. Although chemoradiation plays a role in the treatment of certain rectal tumors, studies have characterized a diverse set of disparities regarding access to these treatments [18–20]. Therefore, to focus our analysis on surgical approach and its associated disparities, we excluded patients who received any chemotherapy or radiation.
Patients offered MIS but then converted to open were analyzed in their respective minimally invasive group, either laparoscopic or robotic, since our primary goal was to determine disparities in access to minimally invasive surgery and not to analyze the factors associated with conversion rates to open. Surgical procedures included partial resection, total proctectomy, proctocolectomy and pelvic exenteration. Analysis of type of surgery was excluded as the decision to convert a minimally invasive procedure to an open procedure may have influenced the final surgery type that was performed.
Patients with either adenocarcinoma or neuroendocrine tumors of the rectum were included. For adenocarcinoma, the following ICD-O-3 codes were used: 8140–8148, 8200, 8260–8263 and 8480–8496. For neuroendocrine tumors, the ICD-O-3 codes included 8150–8155 and 8240–8248. In addition to cancer histology, other pathologic factors included tumor size, grade and clinical stage. Demographic factors included patient age, gender, race, income, education, insurance status, facility type and location. Recognizing that insurance is related to age such that patients over 65 qualify for Medicare, we stratified insurance type by age < 65 and age ≥ 65 in a separate analysis to account for this factor.
Patient characteristics are reported using the mean, median and standard deviation for continuous variables, and using frequencies and relative frequencies for categorical variables. Comparisons were made between procedures using the Kruskal–Wallis and Chi-square tests for continuous and categorical variables, respectively. Multinomial general linear models were used to identify a set of patient characteristics that are significantly associated with a given surgical approach. The variables included in the model were obtained using the backward selection method (α = 0.05). Baseline category odds ratios (ORs) were obtained from the fitted model and represent the odds of having a robotic or laparoscopic procedure as compared to an open surgery for a change in the given patient characteristic. These models determined which demographic and oncologic variables were independently associated with each of type of surgical approach. All analyses were conducted in SAS v9.4 (Cary, NC, USA) at a significance level of 0.05.
Results
A total of 8633 patients were identified between 2004 and 2011 with rectal cancer who had undergone surgery without receiving chemotherapy or radiation. Over half of these patients (53.5 %) underwent minimally invasive procedures (50.9 % laparoscopic and 2.6 % robotic). Patient oncologic variables are shown in Table 1. The majority of patients were at either clinical stage I or II across each group of surgical approach, which was expected given the exclusion of chemoradiation. Differences with respect to tumor size and tumor grade are shown. The majority of patients undergoing the robotic approach had adenocarcinoma, whereas neuroendocrine tumors were more represented in the laparoscopic and open groups.
Table 2 shows the differences among demographic variables for each group of surgical approach. These included age, gender, race, income, education, insurance status, urban versus rural location, distance from home residence to hospital and facility type. Comparison of patient comorbidity status quantified by the NCDB using the Charlson–Deyo comorbidity score is also shown.
Table 3 shows the multivariate analysis of both the demographic variables and oncologic characteristics as predictors of surgical approach with respect to MIS compared to open. Compared to open surgery, oncologic factors associated with increased odds ratios (ORs) for robotic surgery included tumor size <5 cm. Clinical stage, comorbidity score and tumor grade were not significant predictive factors for robotic surgery as compared to open surgery. Similar results were found for the laparoscopic approach versus open. In addition, patients with neuroendocrine tumors were more likely to undergo laparoscopic surgery.
Statistically significant demographic variables predictive of MIS included treatment at an academic center and income over $46,000. Privately insured patients were also more likely to undergo laparoscopic surgery than open surgery as compared to uninsured patients. Having private insurance was also associated with an increased likelihood of undergoing robotic surgery, though the confidence interval was not statistically significant.
We also conducted a multivariate analysis of variables predictive of robotic surgery compared to laparoscopic surgery, as shown in Table 4. In this analysis, income greater than $46,000 was associated with a statistically significant increase in robotic surgery compared to laparoscopic surgery. Treatment at an academic center or a comprehensive cancer center was also strongly associated with the robotic approach. Similar to the comparison with open surgery, insurance status was a statistically significant factor in determining a robotic versus laparoscopic approach.
Lastly, recognizing that patients who qualify for Medicare are typically aged 65 years or older, we analyzed insurance status for patients in this older age group. As shown in Table 5, patients aged 65 and older comprised 3951 patients (46.8 % of the entire group). The majority of these patients have Medicare (83.0 %). In this subgroup of patients, insurance status was not significantly associated with surgical approach (p = 0.243). In contrast, in the subgroup of patients younger than 65, insurance status was significantly associated with surgical approach (p < 0.001).
Discussion
Robotic surgery has been increasingly utilized in the field of urology for both benign and malignant disease [11, 21]. Disparities have been identified in urologic oncology and studied in regard to their impact on patient outcomes [12, 17]. For example, racial disparities have been recognized among certain minorities undergoing prostate surgery such that African Americans were less likely to have minimally invasive radical prostatectomies compared to Caucasians [12, 17]. One study showed that African Americans were 22 % less likely to have minimally invasive radical prostatectomy compared to Caucasian patients, although this gap was improving in more recent years [17]. Other studies have reported differences for minorities in access to MIS in a more general sense [22, 23]. Differences between rates of MIS and open procedures have also been identified with regard to income, education levels and insurance status [24–26].
In comparison with urologic oncology where robotic surgery has been largely adopted, the use of robotics has only recently spread into colorectal surgery [14]. Presently, laparoscopic surgery and open surgery are the most utilized surgical approaches, which were also confirmed by this study with 50.9 % of surgeries performed laparoscopically and 46.5 % performed open. The relative novelty of robotics in colorectal surgery makes it difficult to estimate its rate of nationwide application. Analysis of the NCDB is limited to 2004 and 2011 when the American College of Surgeons first began collecting data on surgical approach. Whereas the oncologic outcomes of laparoscopic colorectal surgery have been found to be equivalent to open surgery [3, 6], similar studies have not yet been performed in robotic surgery. Short-term results of robotic surgery have been proposed to be equivalent to laparoscopic or open approaches, though long-term results have not matured [27, 28]. The ACS has not yet released the validated survival data on patients treated after 2006, which would be of particular interest when comparing the long-term oncologic outcomes of rectal cancer patients stratified by surgical approach. Innovative studies are being performed to determine the long-term oncologic benefits of robotic surgery in rectal cancer [29–31].
Disparities between the open and laparoscopic approach in colorectal cancer have been extensively studied. Studies have suggested that racial disparities exist in the treatment of colorectal diseases [16, 32]. Racial disparities in access to chemotherapy have been described [18, 19]. In order to focus on disparities among surgical approach, we excluded patients who received any form of chemotherapy. However, consistent with a recent study utilizing the Nationwide Inpatient Sample (NIS) database showing that race was not a significant variable contributing to disparities between open and laparoscopic surgery for colorectal diseases [16], the multivariate analysis of this study also did not show race to be a significant predictor of surgical approach.
Insurance status has also been shown to have disparate effects on treatments, whereby patients with private insurance or Medicare had higher rates of laparoscopic surgery [33]. Similarly, higher levels of income have been shown to be associated with laparoscopic surgery [16, 32, 33], and we have shown here that this trend continues with robotic surgery. However, we recognize that many of the large nationwide datasets which have been used to examine economic disparities on surgical approach are somewhat limited in the stratification of income levels. The NCDB uses a maximum income level cutoff of over $46,000, while the NIS uses $39,000. Another similarity between laparoscopic and robotic surgery identified during our analysis was that robotic surgery was significantly associated with treatment at academic centers, which is a parallel finding of other studies with regard to the laparoscopic approach [16, 34]. This phenomenon may be related to higher case volumes at teaching hospitals, as well as the presence of general surgery training programs or MIS fellowships and other fellowships which emphasize robotic training. As robotic surgery has the potential to continue to grow in its applications and practicing general surgeons and trainees acquire more experience with robotics, the characterization of disparities with respect to access to robotics may become increasingly relevant.
There are limitations to our study as well, which are similar to those inherent to the datasets used in many studies on surgical disparities. One of the potential limitations of the NCDB database is that surgeries in which the approach was not specified by the operating surgeon may be grouped with the open procedures. This represents a potential for minimally invasive procedures not being properly encoded in their respective groups. Human error is intrinsic to any large database, and we therefore performed a comparison of robotic surgery to laparoscopic surgery to offset this potential limitation. The individual patient preference or bias for a given surgical approach is not captured by the NCDB. The particular decision-making process for a given patient is complex and dependent on several intangible factors, which have been shown to influence treatment [35, 36]. On the physician side, surgeon experience with MIS in rectal cancer is not captured by the NCDB. Surgeon experience with laparoscopy has been shown to affect outcome in patients with colorectal cancer such that surgeons practicing at high volume centers had lower rates of mortality [37, 38]. The same finding may be the case with robotic surgery since major academic centers have increased case-load volumes, which likely contributes to our finding that the robotic approach is more likely in academics. The NCDB does not record information regarding elective versus emergency surgery, whereby the latter would be considered a relative contraindication to performing either form of MIS [39]. Prior patient surgeries are not accounted for in the NCDB. Previous abdominal incisions and the increased presence of intra-abdominal adhesions may likely influence the decision-making process on surgical approach. Lastly, patient comorbidities or performance status may influence surgical approach. The NCDB uses the Charlson–Deyo score to estimate patient comorbidity. While there was a statistically significant difference in the comorbidity score across each group (Table 2), clinically these differences are small. Furthermore, comorbidity score was not an independent predictor of surgical approach on multivariate analysis.
In summary, we analyzed a large nationwide database known to capture 70 % of the cancer cases through its participating hospitals. The NCDB offers a multitude of demographic and oncologic factors relevant to the investigation of disparities among the different surgical approaches for rectal cancer. As more experience and widespread application of robotics matures nationwide, new data will become available regarding both the potential benefits and disadvantages of robotics in the treatment of rectal cancer. Recognition of demographic and oncologic disparities in surgical approach for rectal cancer is therefore of relevant importance. Consistent with other studies, we found that MIS is associated with insurance status, patient income and treating facility. Unique to the existing literature, we found that robotic surgery compared to laparoscopic surgery as the initial surgical approach offered to patients is influenced by patient income and the treating facility.
References
Kemp JA, Finlayson SR (2008) Nationwide trends in laparoscopic colectomy from 2000 to 2004. Surg Endosc 22(5):1181–1187
Biondi A, Grosso G, Mistretta A, Marventano S, Toscano C, Drago F, Gangi S, Basile F (2013) Laparoscopic vs. open approach for colorectal cancer: evolution over time of minimal invasive surgery. BMC Surg 13(Suppl 2):S12
Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ (2010) Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg 97(11):1638–1645
Fabozzi M, Allieta R, Contul RB, Grivon M, Millo P, Lale-Murix E, Nardi M Jr (2010) Comparison of short- and medium-term results between laparoscopically assisted and totally laparoscopic right hemicolectomy: a case–control study. Surg Endosc 24(9):2085–2091
Clinical Outcomes of Surgical Therapy Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350(20):2050–2059
van der Pas MH, Haglind E, Cuesta MA, Furst A, Lacy AM, Hop WC, Bonjer HJ (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14(3):210–218
Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, Heath RM, Brown JM (2007) Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol 25(21):3061–3068
Alasari S, Min BS (2012) Robotic colorectal surgery: a systematic review. ISRN Surg 2012:293894
Shussman N, Wexner SD (2014) Current status of laparoscopy for the treatment of rectal cancer. World J Gastroenterol 20(41):15125–15134
Anderson JE, Chang DC, Parsons JK, Talamini MA (2012) The first national examination of outcomes and trends in robotic surgery in the United States. J Am Coll Surg 215(1):107–114 (discussion 114–106)
Patel MN, Hemal AK (2014) Robot-assisted laparoscopic simple anatomic prostatectomy. Urol Clin N Am 41(4):485–492
Trinh QD, Schmitges J, Sun M, Sukumar S, Sammon J, Shariat SF, Jeldres C, Bianchi M, Tian Z, Perrotte P et al (2012) Improvement of racial disparities with respect to the utilization of minimally invasive radical prostatectomy in the United States. Cancer 118(7):1894–1900
Sinno AK, Fader AN (2014) Robotic-assisted surgery in gynecologic oncology. Fertil Steril 102(4):922–932
Halabi WJ, Kang CY, Jafari MD, Nguyen VQ, Carmichael JC, Mills S, Stamos MJ, Pigazzi A (2013) Robotic-assisted colorectal surgery in the United States: a nationwide analysis of trends and outcomes. World J Surg 37(12):2782–2790
Speicher PJ, Englum BR, Ganapathi AM, Nussbaum DP, Mantyh CR, Migaly J (2014) Robotic low anterior resection for rectal cancer: a national perspective on short-term oncologic outcomes. Ann Surg. doi:10.1097/SLA.0000000000001017
Alnasser M, Schneider EB, Gearhart SL, Wick EC, Fang SH, Haider AH, Efron JE (2014) National disparities in laparoscopic colorectal procedures for colon cancer. Surg Endosc 28(1):49–57
Trinh QD, Sun M, Sammon J, Bianchi M, Sukumar S, Ghani KR, Jeong W, Dabaja A, Shariat SF, Perrotte P et al (2012) Disparities in access to care at high-volume institutions for uro-oncologic procedures. Cancer 118(18):4421–4426
Ayanian JZ, Zaslavsky AM, Fuchs CS, Guadagnoli E, Creech CM, Cress RD, O’Connor LC, West DW, Allen ME, Wolf RE (2003) Use of adjuvant chemotherapy and radiation therapy for colorectal cancer in a population-based cohort. J Clin Oncol 21(7):1293–1300
Hao Y, Landrine H, Jemal A, Ward KC, Bayakly AR, Young JL Jr, Flanders WD, Ward EM (2011) Race, neighbourhood characteristics and disparities in chemotherapy for colorectal cancer. J Epidemiol Community Health 65(3):211–217
McGory ML, Zingmond DS, Sekeris E, Bastani R, Ko CY (2006) A patient’s race/ethnicity does not explain the underuse of appropriate adjuvant therapy in colorectal cancer. Dis Colon Rectum 49(3):319–329
Huang KH, Carter SC, Hu JC (2013) Does robotic prostatectomy meet its promise in the management of prostate cancer? Curr Urol Rep 14(3):184–191
Ricciardi R, Selker HP, Baxter NN, Marcello PW, Roberts PL, Virnig BA (2008) Disparate use of minimally invasive surgery in benign surgical conditions. Surg Endosc 22(9):1977–1986
Varela JE, Nguyen NT (2011) Disparities in access to basic laparoscopic surgery at U.S. academic medical centers. Surg Endosc 25(4):1209–1214
Ward EM, Fedewa SA, Cokkinides V, Virgo K (2010) The association of insurance and stage at diagnosis among patients aged 55 to 74 years in the national cancer database. Cancer J (Sudbury, MA) 16(6):614–621
Kane CJ, Lubeck DP, Knight SJ, Spitalny M, Downs TM, Grossfeld GD, Pasta DJ, Mehta SS, Carroll PR (2003) Impact of patient educational level on treatment for patients with prostate cancer: data from CaPSURE. Urology 62(6):1035–1039
Winterich JA, Grzywacz JG, Quandt SA, Clark PE, Miller DP, Acuna J, Dignan MB, Arcury TA (2009) Men’s knowledge and beliefs about prostate cancer: education, race, and screening status. Ethn Dis 19(2):199–203
Kim CW, Kim CH, Baik SH (2014) Outcomes of robotic-assisted colorectal surgery compared with laparoscopic and open surgery: a systematic review. J Gastrointest Surg 18(4):816–830
Araujo SE, Seid VE, Klajner S (2014) Robotic surgery for rectal cancer: current immediate clinical and oncological outcomes. World J Gastroenterol 20(39):14359–14370
Gomez Ruiz M, Parra IM, Palazuelos CM, Martin JA, Fernandez CC, Diego JC, Fleitas MG (2015) Robotic-assisted laparoscopic transanal total mesorectal excision for rectal cancer: a prospective pilot study. Dis Colon Rectum 58(1):145–153
Al Asari S, Cho MS, Kim NK (2014) Safe anastomosis in laparoscopic and robotic low anterior resection for rectal cancer: a narrative review and outcomes study from an expert tertiary center. Euro J Surg Oncol. doi:10.1016/j.ejso.2014.10.060
Levic K, Donatsky AM, Bulut O, Rosenberg J (2014) A comparative study of single-port laparoscopic surgery versus robotic-assisted laparoscopic surgery for rectal cancer. Surg Innov. doi:10.1177/1553350614556367
Robinson CN, Balentine CJ, Sansgiry S, Berger DH (2012) Disparities in the use of minimally invasive surgery for colorectal disease. J Gastrointest Surg 16(5):897–903 (discussion 903–894)
Steele SR, Brown TA, Rush RM, Martin MJ (2008) Laparoscopic vs open colectomy for colon cancer: results from a large nationwide population-based analysis. J Gastrointest Surg 12(3):583–591
Kemp JA, Finlayson SR (2008) Outcomes of laparoscopic and open colectomy: a national population-based comparison. Surg Innov 15(4):277–283
Polite BN, Sing A, Sargent DJ, Grothey A, Berlin J, Kozloff M, Feng S (2012) Exploring racial differences in outcome and treatment for metastatic colorectal cancer: results from a large prospective observational cohort study (BRiTE). Cancer 118(4):1083–1090
Polite BN, Dignam JJ, Olopade OI (2005) Colorectal cancer and race: understanding the differences in outcomes between African Americans and whites. Med Clin N Am 89(4):771–793
Pitiakoudis M, Michailidis L, Zezos P, Kouklakis G, Simopoulos C (2011) Quality training in laparoscopic colorectal surgery: does it improve clinical outcome? Tech Coloproctol 15(Suppl 1):S17–S20
Harmon JW, Tang DG, Gordon TA, Bowman HM, Choti MA, Kaufman HS, Bender JS, Duncan MD, Magnuson TH, Lillemoe KD (1999) Hospital volume can serve as a surrogate for surgeon volume for achieving excellent outcomes in colorectal resection. Ann of Surg 230(3):404–411 (discussion 411–403)
Navez B, Navez J (2014) Laparoscopy in the acute abdomen. Best Pract Res Clin Gastroenterol 28(1):3–17
Acknowledgments
We thank the Commission on Cancer of the American College of Surgeons for access to the NCDB Participant User File.
Disclosures
Each of the authors has nothing to disclose. Drs. Emmanuel Gabriel, Pragatheeshwar Thirunavukarasu, Eisar Al-Sukhni, Kristopher Attwood and Steven J Nurkin have no conflict of interest of financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclaimer: The American College of Surgeons Committee on Cancer provided the Participant User File from the National Cancer Database, but has not reviewed or validated the results or conclusions of our study.
Rights and permissions
About this article
Cite this article
Gabriel, E., Thirunavukarasu, P., Al-Sukhni, E. et al. National disparities in minimally invasive surgery for rectal cancer. Surg Endosc 30, 1060–1067 (2016). https://doi.org/10.1007/s00464-015-4296-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4296-5