Abstract
Objective
To determine by meta-analysis, whether D2 lymphadenectomy at laparoscopic-assisted distal gastrectomy (LADG) is as effective as that during open distal gastrectomy (ODG) for patients with advanced gastric cancer (AGC).
Data sources and review methods
All clinical trials that compared laparoscopic with open D2 lymphadenectomy for AGC published in English from January 1995 to June 2013 were identified in PubMed, Embase, Web of Science, and Cochrane library searches. A modified scale was used to assess the quality of the literature. We analyzed the number of harvested lymph nodes (HLNs), body mass index (BMI), tumor size, serosa invasion status, and positive lymph node rate. Meta-analyses were performed using weighted mean differences (WMD) for continuous variables, and risk differences (RD) or odds ratios (OR) for dichotomous variables.
Results
No eligible randomized trials were identified, but eight non-randomized trials were analyzed. In the pooled data of 677 patients who underwent LADG and 687 ODG, there were no significant differences the number of HLN (WMD: −0.98, 95 % confidence interval, CI −3.21 to 1.26), BMI (WMD: −1.20, 95 % CI −2.64 to 0.24), tumor size (WMD: −0.30, 95 % CI −0.65 to 0.05), serosa invasion status (RD: 0.04, 95 % CI −0.03 to 0.11), and positive lymph node rate (OR: 0.66, 95 % CI −0.44 to 1.01) between the groups.
Conclusion
Our findings suggest that for patients with comparable BMI and tumor status, surgical technique did not significantly influence the number of HLNs, suggesting that D2 lymphadenectomy performed laparoscopically is as effective as an open procedure in AGC.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Dissection of the lymph nodes adjacent to the stomach and celiac axis (D2 lymphadenectomy) has been an essential component of the surgical treatment of resectable advanced gastric cancer (AGC) in East Asia for some time, and is now increasingly accepted as the standard of care in Western countries [1]. The extent and quality of lymph node dissection is critical: in laparoscopic-assisted distal gastrectomy (LADG) for AGC, this can be measured by the number of harvested lymph nodes (HLNs) and the incidence of non-compliance (the identification of nodal tissue at a node station that should have been resected) [2–4]. The number of HLNs is frequently used as an outcome measure in studies of LADG, but it remains unclear how the number of HLNs yielded by D2 lymphadenectomy during LADG compares with the number yielded during open distal gastrectomy (ODG).
Several non-randomized controlled trials (NRCTs) have been undertaken to compare D2 lymphadenectomy during LADG with D2 lymphadenectomy during ODG for the treatment of AGC [5–12]. We undertook a systematic review and meta-analysis of data from these NRCTs. As well as the number of HLNs, we also systematically and objectively compared the body mass index (BMI), tumor size, serosa invasion status, and positive lymph node rate of patients who underwent LADG with those who underwent ODG. The latter four parameters are considered to have contributed to selection bias in these NRCTs. We proposed null hypotheses that the number of HLNs would not be significantly different in patients undergoing laparoscopic or open surgery, and that the absence of significant differences in the other parameters would indicate that there was no selection bias in the recruitment to the NRCTs. If there were significant differences, it would suggest that it could not be convincingly established that the quality of D2 lymphadenectomy undertaken during LADG was equivalent to that undertaken during ODG in patients with AGC.
Methods
Search strategy
Studies were identified by searches of PubMed, EMBASE, Web of Science, and the Cochrane Library for relevant articles published between January 1995 and June 2013. The search strategy was as follows:
PubMed
(“Stomach Neoplasms”[Mesh] AND “surgery”[Subheading]) AND “laparoscopy”[mesh] AND ((“1995/01/01”[PDAT]: “2013/06/30”[PDAT]) AND “humans”[MeSH Terms] AND English(lang)
Embase
‘Stomach’/exp and ‘neoplasm’/exp and ‘laparoscopic surgery’/exp and [humans]/lim and [english]/lim and [embase]/lim and [1-1-1995]/sd not [30-6-2013]/sd
Web of Science
(TS = (gastric cancer AND surgery AND laparoscopy)) AND Language = (English)
Databases = SCI-EXPANDED, CPCI-S, CCR-EXPANDED, IC Timespan = 1995-2013
Cochrane Library
#1 [Stomach Neoplasms] explode all trees and with qualifiers: [Surgery—SU]
#2 [Laparoscopy] explode all trees
#3 #1 and #2 (from 1995 to 2013)
Inclusion and exclusion criteria
We included clinical trials that: (1) made a comparison between LADG with D2 lymphadenectomy and ODG with D2 lymphadenectomy for the treatment of AGC from 1995 to 2013; (2) recorded the majority of the following: number of HLNs, BMI, tumor size, serosa invasion status, and the positive lymph node rate; (3) were written in English; and (4) involved a previously unreported patient group. We excluded trials that: (1) did not use ODG as a concurrent control; (2) provided insufficient data or were duplicate publications.
Definitions
We included studies in which D2 lymphadenectomy was performed according to the lymph node classification of the Japanese Gastric Cancer Association (guideline version 3) [13], which state that lymph node numbers 1, 3, 4sb, 4d, 5, 6, 7, 8a, 9, 11p, and 12a should be dissected. Advanced gastric cancer was defined as invading the muscularis propria of the stomach wall or beyond [14].
Quality of literature
For the purposes of this review, we used a modified scale method to assess the quality of literature according to a previously established scoring system, the methodological index for non-randomized studies (MINORS) [15]. The modifications included: (1) six of the 12 items were not considered: four were not related to the validity of the data (statement of the study aim, evaluation of endpoints, and adequacy of statistical methods) and two were better suited to assess the validity of long-term outcomes (adequate follow-up period and follow-up loss <5 %); (2) the item “prospective calculation of sample size” was modified to assess the proficiency of the surgical teams and the power given by the actual number of LADG cases; and (3) the item “important data being presented” was included in the modified MINORS scale (Table 1).
Data extraction
Two researchers independently extracted data from each study. The extracted information comprised: study features, data needed for quality assessment, and the patients’ clinical pathological parameters (including HLN, BMI, tumor size, tumor stage, and number of positive lymph nodes). If the study provided medians and ranges instead of means and standard deviations (SDs), we estimated the means and SDs using the technique described by Hozo and colleagues (Table 2) [16].
Statistical analysis
Meta-analysis was performed using weighted mean differences (WMDs) for continuous variables and odds ratios (ORs) or risk differences (RDs) for dichotomous variables. The latter were used if there were no events in either the intervention or control arms of the study [17]. Between-study heterogeneity was assessed by performing χ 2 tests (assessing the P value), and by calculating the I 2 statistic. If the P value was less than 0.05 and I 2 exceeded 50 %, we considered heterogeneity to be substantial. In these circumstances, random-effect models were used instead of fixed-effect models. Ninety-five percent confidence intervals (CIs) are reported. All reported P values are two sided, and values <0.05 are considered statistically significant. Statistical analyses were performed using Stata Version 11 (Stata Corp, College Station, Tex., USA).
Results
Studies selected
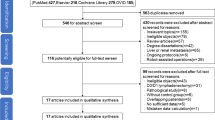
The search strategy retrieved 1,359 reports in English. After the titles and abstracts had been reviewed, 29 reports were included for full-text review (six randomized controlled trials and 23 NRCTs). Of these, 19 were excluded because tumor stage or control data were unavailable. Ten reports were finally selected for quality assessment. A flow chart of the search strategies is illustrated in Fig. 1.
Quality assessment
The quality assessment of the NRCTs is shown in Table 3. The studies by Huscher et al. and Cui et al. were excluded because their score was <10 points.
Outcomes
Number of HLNs
Two of the eight studies reported that there were statistically significant differences between the number of HLNs in the LADG and ODG groups, but in the pooled data, there was no significant difference between the groups (WMD: −0.98, 95 %CI −3.21 to 1.26; Fig. 2A)
A Meta-analysis of the number of harvested lymph nodes in LADG versus ODG. B Meta-analysis of body mass index in LADG versus ODG. C Meta-analysis of tumor size in LADG versus ODG. D Meta-analysis of serosa invasion rate in LADG versus ODG. E Meta-analysis of rate of positive lymph nodes in LADG versus ODG
BMI
Only one of three studies found that BMI was significantly lower in the LADG group than the ODG group. In the pooled data, there was no statistically significant difference (WMD: −1.20, 95 % CI −2.64 to 0.24; Fig. 2B).
Tumor size
Two of five studies demonstrated that the tumor size was statistically different between LADG and ODG, but there was no significant difference in the pooled data (WMD: −0.30, 95 % CI −0.65 to 0.05; Fig. 2C).
Serosa invasion status
In the pooled data, there was no significant difference in serosa invasion rate between the groups (RD: 0.04, 95 % CI −0.03 to 0.11; Fig. 2D).
Rate of positive lymph nodes
In the pooled data, there was no significant difference in the rate of positive lymph nodes between the groups (OR: 0.66, 95 % CI −0.44 to 1.01; Fig. 2E).
Discussion
Laparoscopic resection is a technique that offers important advantages (less blood loss, reduced postoperative pain, accelerated recovery, early return to normal bowel function, and reduced hospital stay) over open surgical procedures for patients with gastric cancer [20]. At the same time, some prospective randomized studies have shown that the survival rates of patients with early stage cancers in the middle or lower parts of the stomach undergoing either LADG or ODG were broadly comparable [21, 22]. This strongly suggests that LADG is an effective treatment for early gastric cancer.
The efficacy of LADG for the treatment of AGC is less clear. Because of the complexity of the laparoscopic technique, surgeons must focus on the quality of D2 lymphadenectomy during LADG, which is a fundamental aspect of oncological safety in the era of “D2 surgery” for AGC [2, 4]. In most clinical studies, the number of HLNs is widely accepted as the index of “quality” [2, 6, 18, 19, 21].
Our literature review identified 10 NRCTs that compared the efficacy of LADG with ODG for the treatment of AGC. We identified no randomized controlled studies. The modified MINORS scale method was used to assess the quality of these reports and eight of which scored no less than 10 were finally included in this study [15]. We focused on not only the number of HLNs but also the other clinicopathological parameters including BMI, tumor size, serosa invasion status, and positive lymph node rate. The latter four items were used to assess whether there had been selection bias in enrollment for the studies analyzed. Patients’ age and sex were not included in our meta-analysis as they were considered unlikely to influence the difficulty of lymph node dissection.
Our meta-analysis revealed that there were no significant differences in the number of HLNs, BMI, tumor size, and the rates of serosa invasion and positive lymph nodes between the groups. This suggests that the extent of obesity and tumor stage of enrolled patients, as well as the number of HLNs, was comparable between the groups and thus a conclusion can be drawn that the quality of D2 lymphadenectomy at LADG is equal to that at ODG for patients with AGC.
This is the first meta-analysis study to have focused on the number of HLNs from this perspective, which we considered to be not only an important predictor of oncological outcome after LADG, but also allowed a re-assessment of the quality of the non-randomized studies themselves. The findings of high-quality NRCTs might be as reliable as randomized controlled trials, particularly when pooled data are compared to evaluate the effectiveness of surgical procedures [23]. Nonetheless, our study has some limitations: no original data were obtained and no conclusions could be drawn about publication bias, as only eight studies were included. A high-quality randomized study is still necessary to allow firm conclusions to be drawn.
References
Songun I PH, Kranenbarg E MK et al. (2010) Surgical treatment of gastric cancer: 15-year follow-up results of the randomised nationwide Dutch D1D2 trial. Lancet Oncol 11(5):439–449
Miura S, Kodera Y, Fujiwara M et al (2004) Laparoscopy-assisted distal gastrectomy with systemic lymph node dissection: a critical reappraisal from the viewpoint of lymph node retrieval. J Am Coll Surg 198:933–938
Lee JH, Kim YW, Ryu KW et al (2007) A phase-II clinical trial of laparoscopy-assisted distal gastrectomy with d2 lymph node dissection for gastric cancer patients. Ann Surg Oncol 14:3148–3153
Ikeda O, Sakaguchi Y, Toh Y et al (2012) Evaluation of oncological adequacy of laparoscopic distal gastrectomy with special attention to lymph node dissection: a comparison with conventional open gastrectomy. Hepato-gastroenterol 59:627–632
Chun HT, Kim KH, Kim MC, Jung GJ (2012) Comparative Study of laparoscopy-assisted versus open subtotal gastrectomy for pT2 Gastric Cancer. Yonsei Med J 53:952–959
Du XH, Li R, Chen L, Shen D, Li SY, Guo Q (2009) Laparoscopy-assisted D2 radical distal gastrectomy for advanced gastric cancer: initial experience. Chin Med J (Engl) 122:1404–1407
Huang JL, Wei HB, Zheng ZH et al (2010) Laparoscopy-assisted D2 radical distal gastrectomy for advanced Gastric Cancer. Dig Surg 27:291–296
Hur H, Jeon HM, Kim W (2008) Laparoscopy-assisted distal gastrectomy with D2 lymphadenectomy for T2b advanced gastric cancers: three years’ experience. J Surg Oncol 98:515–519
Scatizzi M, Kroning KC, Lenzi E, Moraldi L, Cantafio S, Feroci F (2011) Laparoscopic versus open distal gastrectomy for locally advanced gastric cancer: a case-control study. Updates Surg 63:17–23
Shuang JB, Qi SB, Zheng JY et al (2011) A case-control study of laparoscopy-assisted and open distal gastrectomy for advanced gastric cancer. J Gastrointest Surg 15:57–62
Zhao Y, Yu P, Hao Y et al (2011) Comparison of outcomes for laparoscopically assisted and open radical distal gastrectomy with lymphadenectomy for advanced gastric cancer. Surg Endosc 25:2960–2966
Ziqiang W, Feng Q, Zhimin C et al (2006) Comparison of laparoscopically assisted and open radical distal gastrectomy with extended lymphadenectomy for gastric cancer management. Surg Endosc 20:1738–1743
(JGCA) JGCA (2011) Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer 14:101–112
Sobin L GMK, Wittekind C e. (2009) TNM classification of malignant tumours. 7th edn. Wiley & Blackwell
Slim K, Nini E, Forestier D, Kwiatkowski F (2003) Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg 73:712–716
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Sterne JAC (2008) Meta-analysis in Stata™[J]. Systematic reviews in health care: meta-analysis in context. Second edn. p 347–369
Huscher C, Mingoli A, Sgarzini G et al (2005) Value of extended lymphadenectomy in laparoscopic subtotal gastrectomy for advanced gastric cancer. J Am Coll Surg 200:314
Cui M, Xing JD, Yang W et al (2012) D2 dissection in laparoscopic and open gastrectomy for gastric cancer. World J Gastroenterol 18:833–839
Reyes CD, Weber KJ, Gagner M, Divino CM (2001) Laparoscopic vs open gastrectomy. A retrospective review. Surg Endosc 15:928–931
Huscher CG, Mingoli A, Sgarzini G et al (2005) Laparoscopic versus open subtotal gastrectomy for distal gastric cancer: five-year results of a randomized prospective trial. Ann Surg 241:232–237
Lee JH, Han HS, Lee JH (2005) A prospective randomized study comparing open vs laparoscopy-assisted distal gastrectomy in early gastric cancer. Surg Endosc 19:168–173
Abraham NS, Byrne CJ, Young JM et al (2010) Meta-analysis of well-designed nonrandomized comparative studies of surgical procedures is as good as randomized controlled trials. J Clin Epidemiol 63:238–245
Disclosures
Drs. Canrong Lu, Sixin Zhou, Zheng Peng and Lin Chen have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Canrong Lu and Sixin Zhou contributed equally to this work.
Rights and permissions
About this article
Cite this article
Lu, C., Zhou, S., Peng, Z. et al. Quality of D2 lymphadenectomy for advanced gastric cancer: is laparoscopic-assisted distal gastrectomy as effective as open distal gastrectomy?. Surg Endosc 29, 1537–1544 (2015). https://doi.org/10.1007/s00464-014-3838-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3838-6