Abstract
Introduction
The success of laparoscopic surgery is due to the less surgical trauma, including less operative pain, complications and better cosmetics. Objective of our study was to compare in two blind randomized groups of patients, the surgical outcome of total extra-peritoneal (TEP) inguinal hernia repair using either single-port or conventional surgical technique. We will report our interim results in the first group of 50 patients.
Materials and methods
Our study is a prospective, randomized, controlled clinical trial conducted from August 2011 to June 2013. Fifty patients aged between 21 and 80 years undergoing surgery for unilateral inguinal hernia were randomised into two groups: conventional laparoscopic TEP inguinal hernia repair versus single-port TEP repair. Clinical data on patient demographics, surgical technique and findings, postoperative complications and pain scores were collected. Primary endpoint is the postoperative pain while secondary endpoints are recurrence, chronic pain, postoperative hospital stay and complications.
Results
Out of the 50 patients, 26 underwent single-port hernia TEP repair and 24 had conventional 3-port TEP hernia repair after randomization. Mean operative time was 51.7 (±13.4) min in the multiport group and 59.3 (±14.9) min in the single-port group, respectively (P = 0.064). Mean hospital stay was 19.7 (±4.8) h in the conventional group and 22.1 (±4.5) h in the single-port group (P = 0.079). No statistically significant differences were observed between the two groups for postoperative complications, and no recurrence reported at 11 months follow-up. There was no significant difference in the pain scores (visual analog scale) between the two groups at regular intervals post surgery.
Discussion
The outcomes after laparoscopic TEP inguinal hernia repair with a single-port device are comparable to the standard three-port technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The success of laparoscopic surgery can be attributable to its reduced surgical trauma, including less postoperative pain, complications and better cosmetics. Endo-laparoscopic inguinal hernia repair has evolved during the past decade with the addition of “reduced port surgery” concept to accomplish the aforementioned characteristics. The totally extra-peritoneal (TEP) approach for laparoscopic inguinal hernia repair was first described in 1993 [1]. It is 15 years later in 2008 that we hear about the first case of laparoendoscopic single-site surgery (LESS) for TEP inguinal hernia repair [2]. Safety and efficacy of LESS-TEP inguinal hernia repair have been assessed in a few prospective studies [3–5], but only a single-randomized controlled clinical trial comparing LESS-TEP with conventional TEP (CTEP) inguinal hernia repair has been published up to now [6].
The primary objective of our study was to determine if laparoscopic TEP inguinal hernia repair using a mesh carried out with a single-port (LESS-TEP), compared to conventional 3 ports (CTEP), results in a significant difference in the postoperative pain in two blind randomized groups of patients. Secondary objectives were to assess any significant difference between two groups of patients in recurrence rate, postoperative pain, hospital stay and complications. Here, we report our interim results in the first group of 50 patients.
Materials and methods
Our study is a prospective, randomised, controlled clinical trial commenced August 2011 in our institution with National University of Singapore’s Domain Specific Review Board (DSRB) approval (2011/00092). Patient recruitment completed. This paper is intended as an interim report on our findings from the first 50 subjects.
We included patients with age 21–80 years with a clinical diagnosis of an inguinal hernia under ASA (American society of anesthesiologists) physical status classification I or II with a body mass index (BMI) less than 30 kg/m2. Patients with bleeding disorders, incarcerated, obstructed, strangulated, recurrent or bilateral inguinal hernia were excluded. Patients who had previous lower abdominal surgery on the same side of the hernia or patients with previous lower segment cesarean section (LSCS) were also excluded from the study.
Patients were prospectively recruited from our outpatient clinics. All patients had indications for laparoscopic inguinal hernia repair and agreed to participate after having received both verbal and written information regarding the trial. Each patient was randomly assigned to one of the two study arms using the closed envelope method, with one arm receiving LESS-TEP while the other receiving CTEP inguinal hernia repair. All subjects and postoperative assessors were blinded to the procedure performed.
Surgical Methodology (CTEP): 1 cm of infra-umbilical transverse skin incision made and deepened down bluntly up to the anterior fascial layer. About 1.5 cm or one middle finger breadth size vertical incision made in the anterior fascial layer, and muscle was retracted laterally to expose the pre-peritoneal space. Conventional 10 mm laparoscopic port was used to insufflate CO2. Olympus ENDOEYE (USA) 10 mm laparoscope was inserted through the 10 mm port, and dissection of the pre-peritoneal space was carried out up to the Retzius’ space. Standard 5 mm port was inserted in the midline about three finger breaths from the pubis under vision. Another 5 mm port inserted in between the camera port and the 5 mm port. Lateral dissection carried out up to the Bogros’ space laterally. Myopectineal orifices dissected to identify the hernia defects. Hernia sac dissected off from the cord structures, and contents reduced into the peritoneal cavity. In some patients where the sac is excessive, it was divided and ligated with pre-made non-absorbable surgical loop. Standard 10 × 15 cm polypropylene mesh was used to cover the myopectineal orifices in all cases. The mesh was secured with absorbable tackers (AbsorbaTack™ 5 mm, COVIDIEN, USA). The rectus sheath was repaired with absorbable sutures, and subcutaneous absorbable sutures were used to close the skin.
Surgical Methodology (LESS-TEP): The surgical technique was similar as for CTEP method except a single-port device (TriPort+™, Olympus, USA) was used through the infra-umbilical incision. Olympus ENDOEYE (USA) 5 mm laparoscope was used. In both groups, three skin plasters were placed over the abdomen after skin closure.
The main surgeon for all surgeries remained the same. But all other authors also performed CTEP and LESS-TEP randomly, supervised by the main surgeon. A standard analgesia regime was used for all patients postoperatively up to 5 days. The demographic information, intra-operative findings, operative time and length of postoperative hospital stay of all patients were recorded in a data collection template. The European Hernia Society (EHS) groin hernia classification was used to record the intra-operative findings of type and size of hernia defects [7]. Visual Analog Scale (VAS) for pain during the postoperative period at 6 and 24 h or at discharge was recorded by a nurse. Patients were followed up 1, 4 weeks, 3 and 6 months intervals and assessed for any postoperative complications and VAS.
The primary endpoint of this non-inferiority study is the 24-h postoperation pain score. From our retrospective review of the laparoscopic inguinal hernia repair cases, it is found that the mean pain score of single-port laparoscopic inguinal hernia repair was 0.55 units less than that of conventional laparoscopic hernia repair with standard deviation 1.8 units. The non-inferiority can be declared only if the mean pain score of single-port laparoscopic hernia repair is not 0.4 units more than that of conventional laparoscopic hernia repair. A trial size of 90 subjects in total, 50 per group will be sufficient to test the non-inferiority based on the assumptions which are described before, using one-sided 2 sample t test with 80 % power and 5 % significant level. The total accrual target would thus be 100, 50 per group, after considering the withdrawer, defaults and lost to follow-up.
Statistical analysis was done using IBM SPSS Statistics Desktop version 22.0.0. Fisher’s exact test or χ 2 test was used where applicable for analysis of categorical variables. T Test was used for analysis of continuous variables. P value less than 0.05 was considered as statistically significant.
Results
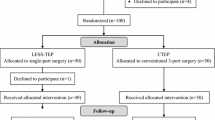
Twenty-four subjects were randomized to CTEP, and twenty-six randomized to LESS-TEP. Fifty-four subjects were assessed for eligibility, and four of them declined to participate. From the 50 subjects randomized, no subjects were lost to follow-up (Fig. 1). All patients were males. The patient demographic information study showed no significant difference between the two groups (Table 1). Most common comorbidities were hypertension and hyperlipidemia. Three subjects in the CTEP group had previous open inguinal hernia repair on the opposite side. One subject from each group was on Aspirin for ischemic heart disease. One subject in the CTEP group had a permanent pacemaker, and bipolar diathermy has to be used intra-operatively.
The intra-operative findings, namely laterality of hernia, type and defect size of hernia, presence and grading of adhesions, type of sac contents showed no significant differences between the two groups (Table 2). The peritoneal sac was divided and ligated in 4 (16.7 %) subjects in the CTEP group and 9 (34.6 %) subjects in the LESS-TEP group (P = 0.196). Peritoneal defects were found in 4 (16.7 %) and 1 (3.8 %) subjects consecutively in the CTEP and LESS-TEP groups (P = 0.181), and all defects were repaired with pre-made surgical loops. Conversion to open technique or use of additional ports was not required in both groups.
The mean operative time, length of hospital stay after surgery and postoperative complication rates between the two groups showed no statistically significant difference (Table 3). The most common complications were postoperative seroma and hematoma formation. In the LESS-TEP group, two subjects developed scrotal hematoma which was noticed during the discharge and they were symptomatic at subsequent follow-ups. Both hematomas were aspirated under sterile conditions with local anesthesia about 3 weeks after surgery and the patients recovered uneventfully: 4 (16.7 %) patients in the CTEP group and 2 (7.7 %) patients in the LESS-TEP group developed seromas which were noticed at discharge and also at 1-week follow-up. All seromas were managed conservatively, and all patients recovered uneventfully during the follow-up period. One subject in the CTEP group had port site superficial wound infection which was conservatively managed. Complications, such as injury to cord structures and iliac vessels, acute urinary retention, mesh infection, recurrence of hernia, ischemic orchitis and chronic pain, were not observed in any of the subjects during a follow-up period of 11 months. VAS for pain during the postoperative period and during the follow-up period showed no statistically significant difference between the two groups (Table 4). In the CTEP group, patients had no pain at the 3-month follow-up and in both groups; patients had no pain at 6-month follow-up.
Discussion
Laparoscopic approach for inguinal hernia repair has become the acceptable treatment for groin hernia repairs in the recent past due to its reduced postoperative pain and low recurrence rates [8, 9]. There are few laparoscopic approaches to inguinal hernia repair [8]. Trans-abdominal pre-peritoneal (TAPP) approach was initially gaining popularity and it was comparable to the TEP approach [10], but due to significantly reduced postoperative pain [11] and slightly reduced risk of port site hernia and visceral injuries [10], the TEP approach has become more acceptable. The safety and feasibility of the laparoscopic TEP approach have been repeatedly assessed over the years since 1993 when Ferzli et al. [12] published his series of 101 patients [8, 9, 13]. The concept of “reduced port surgery” has added a new look to the laparoscopic approach in many sub-specialities. LESS approach is feasible and has been used safely for appendectomy [14, 15], cholecystectomy [16–18] and even for colectomy [19] with its obvious proven benefit of cosmetics and debatable effects on postoperative pain compared to the conventional laparoscopic approaches.
In an era where minimal surgical trauma is gaining concern, Lau et al. [20] in 2002 describes his needlescopic approach for groin hernia repair with its better postoperative pain compared to CTEP approach. In 2010, we described our institutional experience in LESS-TAPP approach for groin hernia repair with comparable outcomes to the conventional TAPP approach [21]. In an attempt for reduced port surgery, Kwon et al. [22] did TEP inguinal hernia repair in 24 patients without the supra-pubic port and demonstrated advantages in postoperative pain, urinary retention, operating time, postoperative hospital stay and cosmetic effect over the CTEP technique.
In 2010, Agrawal et al. [23] described his experience in using the TriPort™ system in LESS-TEP technique to be safe and feasible and managed to perform the procedure with a median incision length of 30 mm. We used the same TriPort™ system in all our patients who underwent LESS-TEP with a standard 1-cm infra-umbilical transverse incision.
The technique of LESS-TEP started with Cugura et al. [2] in 2008 and up to now, the advantage of this technique over the CTEP is still debatable. We encountered four studies [3–6] where the comparison of CTEP and LESS-TEP techniques has been made. Our study population characteristics are comparable to the study population in the randomised clinical trial conducted by Tsai et al. [6]. And, they reported a longer operative time and a minor benefit of reduction of immediate postoperative pain in the LESS-TEP group [6]. In our study, we did not observe any statistically significant difference in any of the above outcomes. Kim et al. [4] also reported no significant difference in the operative time between the LESS-TEP and CTEP groups in his study. In a comparison study between CTEP and LESS-TEP, Cugura et al. [3] concluded that both techniques are comparable and LESS-TEP is a safe and a feasible technique with a short learning curve. Tai et al. [5] in their study state that inguinal hernia repair via the LESS-TEP technique is as safe as the CTEP technique. However, they believe that the LESS-TEP technique is not an efficacious surgical alternative to the CTEP technique for inguinal hernia likely due to the significantly shorter mean operative time in the CTEP series [5]. In our study, as well as all four studies mentioned above [3–6] had no conversions to open technique and no additional ports were used in the LESS-TEP group. In our interim analysis of the first 50 patients of our randomized controlled clinical trial, we did not observe any significant differences in the postoperative hospital stay, complications and pain scores between the LESS-TEP and CTEP groups in our study, and all other parameters studied were comparable between the two groups with no statistically significant differences with a follow-up period of 11 months.
In conclusion, we observe that the outcomes after laparoscopic TEP inguinal hernia repair with a single-port device is not superior to the conventional three-port technique, except for the obvious effect on cosmesis due to the number of scars. We believe that long-term follow-up data are required for further validation of advantages of the LESS-TEP technique over the CTEP technique.
References
McKernan JB, Laws HL (1993) Laparoscopic repair of inguinal hernias using a totally extraperitoneal prosthetic approach. Surg Endosc 7:26–28
Cugura JF, Kirac I, Kulis T, Jankovic J, Beslin MB (2008) First case of single incision laparoscopic surgery for totally extraperitoneal inguinal hernia repair. Acta Clin Croat 47:249–252
Cugura JF, Kirac I, Kulis T, Sremac M, Ledinsky M, Beslin MB (2012) Comparison of single incision laparoscopic totally extraperitoneal and laparoscopic totally extraperitoneal inguinal hernia repair: initial experience. J Endourol 26:63–66
Kim JH, Lee YS, Kim JJ, Park SM (2013) Single port laparoscopic totally extraperitoneal hernioplasty: a comparative study of short-term outcome with conventional laparoscopic totally extraperitoneal hernioplasty. World J Surg 37:746–751
Tai HC, Lin CD, Chung SD, Chueh SC, Tsai YC, Yang SS (2011) A comparative study of standard versus laparoendoscopic single-site surgery (LESS) totally extraperitoneal (TEP) inguinal hernia repair. Surg Endosc 25:2879–2883
Tsai YC, Ho CH, Tai HC, Chung SD, Chueh SC (2013) Laparoendoscopic single-site versus conventional laparoscopic total extraperitoneal hernia repair: a prospective randomized clinical trial. Surg Endosc 27:4684–4692
Miserez M, Alexandre JH, Campanelli G, Corcione F, Cuccurullo D, Pascual MH, Hoeferlin A, Kingsnorth AN, Mandala V, Palot JP, Schumpelick V, Simmermacher RK, Stoppa R, Flament JB (2007) The European hernia society groin hernia classification: simple and easy to remember. Hernia 11:113–116
Fitzgibbons RJ Jr, Camps J, Cornet DA, Nguyen NX, Litke BS, Annibali R, Salerno GM (1995) Laparoscopic inguinal herniorrhaphy. Results of a multicenter trial. Ann Surg 221:3–13
Liem MS, van der Graaf Y, van Steensel CJ, Boelhouwer RU, Clevers GJ, Meijer WS, Stassen LP, Vente JP, Weidema WF, Schrijvers AJ, van Vroonhoven TJ (1997) Comparison of conventional anterior surgery and laparoscopic surgery for inguinal-hernia repair. N Engl J Med 336:1541–1547
McCormack K, Wake BL, Fraser C, Vale L, Perez J, Grant A (2005) Transabdominal pre-peritoneal (TAPP) versus totally extraperitoneal (TEP) laparoscopic techniques for inguinal hernia repair: a systematic review. Hernia 9:109–114
Krishna A, Misra MC, Bansal VK, Kumar S, Rajeshwari S, Chabra A (2012) Laparoscopic inguinal hernia repair: transabdominal preperitoneal (TAPP) versus totally extraperitoneal (TEP) approach: a prospective randomized controlled trial. Surg Endosc 26:639–649
Ferzli GS, Massaad A, Dysarz FA 3rd, Kopatsis A (1993) A study of 101 patients treated with extraperitoneal endoscopic laparoscopic herniorrhaphy. Am Surg 59:707–708
Kuhry E, van Veen RN, Langeveld HR, Steyerberg EW, Jeekel J, Bonjer HJ (2007) Open or endoscopic total extraperitoneal inguinal hernia repair? A systematic review. Surg Endosc 21:161–166
Rehman H, Rao AM, Ahmed I (2011) Single incision versus conventional multi-incision appendicectomy for suspected appendicitis. Cochrane Database Syst Rev 7(7):CD009022
Ding J, Xia Y, Zhang ZM, Liao GQ, Pan Y, Liu S, Zhang Y, Yan Z (2013) Single-incision versus conventional three-incision laparoscopic appendicectomy for appendicitis: a systematic review and meta-analysis. J Pediatr Surg 48:1088–1098
Markar SR, Karthikesalingam A, Thrumurthy S, Muirhead L, Kinross J, Paraskeva P (2012) Single-incision laparoscopic surgery (SILS) vs. conventional multiport cholecystectomy: systematic review and meta-analysis. Surg Endosc 26:1205–1213
Garg P, Thakur JD, Garg M, Menon GR (2012) Single-incision laparoscopic cholecystectomy vs. conventional laparoscopic cholecystectomy: a meta-analysis of randomized controlled trials. J Gastrointest Surg 16:1618–1628
Chang SK, Wang YL, Shen L, Iyer SG, Shaik AB, Lomanto D (2013) Interim report: a randomized controlled trial comparing postoperative pain in single-incision laparoscopic cholecystectomy and conventional laparoscopic cholecystectomy. Asian J Endosc Surg 6:14–20
Li P, Wang DR, Wang LH, Li YK, Chen J (2012) Single-incision laparoscopic surgery vs. multiport laparoscopic surgery for colectomy: a meta-analysis of eleven recent studies. Hepatogastroenterology 59:1345–1349
Lau H, Lee F (2002) A prospective comparative study of needlescopic and conventional endoscopic extraperitoneal inguinal hernioplasty. Surg Endosc 16:1737–1740
Goo TT, Goel R, Lawenko M, Lomanto D (2010) Laparoscopic transabdominal preperitoneal (TAPP) hernia repair via a single port. Surg Laparosc Endosc Percutan Tech 20:389–390
Kwon KH, Son BH, Han WK (2011) Laparoscopic totally extraperitoneal repair without suprapubic port: comparison with conventional totally extraperitoneal repair. J Korean Surg Soc 80:319–326
Agrawal S, Shaw A, Soon Y (2010) Single-port laparoscopic totally extraperitoneal inguinal hernia repair with the TriPort system: initial experience. Surg Endosc 24:952–956
Acknowledgments
Authors wished to acknowledge Drs Dino Halim Liem and Chiara Montana
Disclosure
Doctors Wijerathne Sujith, Agarwal Narendra, Ramzi Ahmad and Lomanto Davide have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wijerathne, S., Agarwal, N., Ramzy, A. et al. A prospective randomized controlled trial to compare single-port endo-laparoscopic surgery versus conventional TEP inguinal hernia repair. Surg Endosc 28, 3053–3058 (2014). https://doi.org/10.1007/s00464-014-3578-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3578-7