Abstract
Background
Although a large number of surgeons currently perform endoscopic hernia surgery using a total extraperitoneal (TEP) approach, reviews published to date are based mainly on trials that compare laparoscopic transabdominal preperitoneal (TAPP) repair with various types of open inguinal hernia repair.
Methods
A qualitative analysis of randomized trials comparing TEP with open mesh or sutured repair.
Results
In this review, 4,231 patients were included in 23 trials. In 10 of 15 trials, TEP repair was associated with longer surgery time than open repair. A shorter postoperative hospital stay after TEP repair than after open repair was reported in 6 of 11 trials. In 8 of 9 trials, the time until return to work was significantly shorter after TEP repair. Hospital costs were significantly higher for TEP than for open repair in all four trials that included an economic evaluation. Most trials (n = 14) reported no differences in subsequent recurrence rates between TEP and open repair.
Conclusions
The findings showed that endoscopic TEP repair is associated with longer surgery time, shorter postoperative hospital stay, earlier return to work, and recurrence rates similar to those for open inguinal hernia repair. The procedure involves greater expenses for hospitals, but appears to be cost effective from a societal perspective. The TEP technique is a serious option for mesh repair of primary hernias.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Inguinal hernia repair is one of the most common surgical procedures. In the United States alone, more than 700,000 of these procedures are performed each year, incurring approximately 3.5 billion dollars of hospital costs [1]. Optimizing surgical technique to improve short-term outcome and reduce the rate of recurrence is therefore of great value to health care.
Over the past 20 years, several hernia repair techniques have been introduced [2–4]. Reducing the rate of recurrence has been the main incentive for the development of these new techniques. The introduction of the Lichtenstein tension-free hernioplasty, which uses a mesh to reinforce the abdominal wall, has decreased recurrence rates greatly [5]. Another advantage of the Lichtenstein hernia repair is that it is a relatively straightforward and easy-to-learn procedure requiring minimal dissection that can be performed using local anesthesia. In addition, because the technique is tension free, it is associated with significantly less postoperative pain and discomfort than conventional open repair [6].
Since the introduction of laparoscopic inguinal hernia repair, most of the ongoing discussion has focused on the choice between open or endoscopic surgery. Endoscopic inguinal hernia repair is associated with shorter recovery periods, earlier return to daily activities and work, and fewer postoperative complications [7]. Some authors suggest that endoscopic repair of recurrent hernia is easier because it is performed in virgin tissue.
On the other hand, endoscopic hernia repair requires special skills to overcome limitations inherent to this type of surgery such as loss of depth perception, limited range of motion, and reduced tactile feedback. As a consequence, endoscopic hernia repair has a significant learning curve [8] and is associated with longer operating times [9]. Furthermore, some serious complications during laparoscopic transabdominal preperitoneal (TAPP) mesh repair have been reported [10–13], some even resulting in the death of a patient [11, 13]. Some authors propose that these complications may have been avoided if an endoscopic extraperitoneal approach had been used [11].
Neumayer et al. [14] compared a mixed design of total extraperitoneal (TEP) and laparoscopic TAPP repair with anterior open inguinal repair according to the Lichtenstein method. Randomized clinical trials comparing only TEP repair with open repair are scarce. Although many surgeons have now adopted the TEP repair, reviews and metaanalyses published to date are based primarily on comparisons between both laparoscopic and endoscopic repair with open inguinal hernia repair [15]. In light of this, a systematic review was performed to examine all published and nonpublished randomized controlled trials comparing TEP with open mesh and suture repair.
Materials and methods
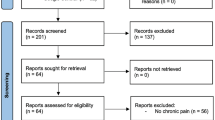
Randomized trials comparing TEP with open mesh or suture repair were included in this review. Studies that included both TEP and TAPP were not included. Relevant randomized controlled trials were identified through a systematic search of Pubmed, Medline, Embase, and Cochrane using the keywords “TEP” and “randomized controlled trial.” Studies published as abstracts and presented at scientific meetings also were included in the review to minimize bias.
A total of 23 randomized trials comparing TEP repair with open hernioplasty were identified. In some cases, different outcomes for the same trial were published in separate articles. Therefore, a total number of 29 publications had to be analyzed [16–44]. Of the 23 trials included in this review, 18 were reported as full articles and 5 as abstracts only. Most trials compared TEP with one method of open repair. In seven trials, TEP was compared with two or more open types of inguinal hernia repair (Table 1).
Because of heterogeneity between studies (Table 1), it was not possible to pool the data. The divergences in trial designs were too great, and not all data needed to perform a quantitative statistical analysis were available. Therefore, we performed only a qualitative analysis. The current review focuses on operating time, hospital stay, return to work, major complications, recurrence rates, and costs of TEP, as compared with suture repair. Statistical significance was defined as a p value less than 0.05.
Results
The 23 trials analyzed in the current review included a total of 4,231 patients. The follow-up periods ranged from 0 to 48 months.
Operating time
Data on the duration of surgery were compared in 15 of the trials. The TEP repair required significantly more time than the open methods of inguinal hernia repair in 10 of the trials. One trial reported a shorter operating time for TEP repair than for Lichtenstein hernioplasty. For three trials, no significant differences were found. Bilgin et al. [19] mentioned operating times, but did not state whether the differences observed were statistically significant (Table 2).
Hospital stay
In-hospital stay was mentioned in available data on 11 trials. Significant differences in favor of TEP repair were found in six trials. Heikkinen et al. [16] found a longer hospital stay after TEP repair than after Lichtenstein tension-free hernioplasty (6.25 vs 4.75 h; p < 0.001). In two trials, no differences between groups were found, and in one study, p values were omitted (Table 3).
Major complications
Only one major complication, a bowel obstruction, was reported among the patients undergoing TEP repair within the framework of a randomized trial [17]. Among the patients undergoing open surgery, no major complications occurred during or after the surgical procedure.
Return to work
In nine trials, return to work was compared between TEP and open repair. In eight of these trials, TEP repair was associated with significantly fewer workdays lost than open repair (Table 4).
Recurrence rates
Recurrence rates were reported in 15 trials. Liem et al. [41] reported a significantly lower rate of recurrence after TEP than after various methods of open mesh and open nonmesh repair (p = 0.006). In the remaining 14 trials, no significant differences were found (Table 5).
Costs
An economic evaluation was performed in only four trials [16, 17, 36, 40]. In the trial by Heikkinen et al. [16], hospital costs were significantly higher for TEP endoscopic repair than for Lichtenstein repair ($1239 vs $782; p < 0.001). Total costs, defined as direct and indirect costs caused by absence from work, were however higher with open repair ($3,912 vs $4,661 for TEP vs Lichtenstein, respectively; p = 0.02). The cost-effectiveness analysis by Andersson et al. [17] showed similar results, namely, higher direct costs for TEP than for Lichtenstein repair ($2,085 vs $1,480; p < 0.001), but no difference in total costs, including costs of sick leave ($4,408 vs $4,757; p = 0.21). In the study by Liem [40], TEP repair was found to involve higher hospital costs: Dfl 2,417.24 ($1,309.13) vs Dfl 1,384.91 ($750.05). However, societal costs were lower for endoscopic repair, resulting in total costs that were only Dfl 251.50 ($136.21) higher for TEP repair. Fleming et al. [36] reported nearly 40% higher costs for TEP repair than for Shouldice, mainly caused by the high costs of laparoscopic equipment and disposables.
Discussion
Laparoscopic hernia surgery has been criticized because of its complexity, high costs, risk of major complications, and need for general anesthesia. The majority of randomized trials compare a laparoscopic TAPP repair with open methods of inguinal hernia repair. As a consequence, systematic reviews and metaanalyses published to date have been based primarily on a comparison between TAPP and open groin hernia repair. Because most surgeons have now adapted the endoscopic extraperitoneal approach, a review of all trials comparing TEP with open mesh and nonmesh repair was performed.
Most of the randomized trials in the current review reported longer surgery time for TEP than for open repair. Possible reasons for these prolonged operative times are the intricacy of the procedure and the need for general anesthesia.
A major drawback of the laparoscopic approach for inguinal hernia repair is the risk of major complications. The TEP procedure for hernia repair is performed within the preperitoneal space. The peritoneal space is avoided, presumably leading to a considerable reduction in the risk of major vascular complications, intestinal obstructions, and perforations.
In the current review, only one major complication was reported among the patients undergoing TEP hernia repair [17]. This patient experienced a small bowel obstruction 3 days after surgery. A loop of the small intestine had herniated through a peritoneal tear. These peritoneal defects occur in approximately 10% to 47% of endoscopic hernia repairs [38, 45, 46]. However, herniation occurs rarely and can be prevented by closing the peritoneal defect, for example, through the use of endoscopic stapling or pretied suture loop ligation [46].
Proponents of laparosopic inguinal hernia repair often refer to the shorter hospital stay and the earlier return to daily activities and work associated with this approach. Obviously, hospital stay and return to work are very important outcome measures given that many patients who undergo inguinal hernia repair are of working age. The majority of trials in the current review showed earlier hospital discharge and quicker return to work after TEP than after open hernia repair. In a systematic review by the Hernia Trialist Collaboration [47], which included mainly trials comparing TAPP with open procedures, no significant difference in length of hospital stay was observed between groups (p = 0.50). However, return to normal daily activities was found to be earlier after minimally invasive surgery (p < 0.001).
The economic benefits to society of reduced absence from work are clearly indicated by the differences in direct and total costs. Whereas in-hospital costs are significantly higher for TEP than for open hernia repair, no differences exist in total costs, including costs associated with workdays lost. Although endoscopic TEP hernia repair is more expensive for hospitals, it appears to be cost effective for society as a whole. However, long-term recurrence rates and morbidity have not been included in the economic evaluations performed to date.
In a recent metaanalysis of randomized trials comparing open and laparoscopic inguinal hernia repair [7], a trend toward an increase in the relative probability of short-term hernia recurrence after laparoscopic repair was detected. However, this trend was found only for TAPP compared with open hernia repair and not for trials comparing TEP with open hernia repair. None of the differences observed were statistically significant.
In the current analysis of 23 trials comparing TEP repair with open mesh and sutured repairs, only one trial reported a significant difference in the number of recurrences [41]. Among 994 patients undergoing inguinal hernia repair, a lower recurrence rate after TEP than after open repair using various techniques was observed (21/507 vs 43/487; p = 0.006). None of the other trials showed any significant differences in recurrence rates between the different techniques. A possible reason for this is that these trials were not adequately powered to detect significant variances of this magnitude. Future large trials may show up such differences, which are not apparent in most of the studies analyzed in the current review.
Neumayer et al. [14] compared both the TAPP and TEP repair techniques with the open Lichtenstein method and concluded that the open technique is superior to the laparoscopic technique for mesh repair of primary hernias. Endoscopic TEP repair tends to be superior to TAPP repair, because of less morbidity as well as lower recurrence rates and complications [48, 49].
Endoscopic TEP repair seems to be associated with longer surgery time, shorter hospital stay, and earlier return to work than open inguinal hernia repair. (Table 6) Although TEP is associated with higher hospital costs, it does not seem to produce an increase in total expenses, including costs of sick leave. Recurrence rates after TEP repair seem to be comparable with, if not better than, rates after open methods of repair.
References
Rutkow IM, Robbins AW (1993) Demographic, classificatory, and socioeconomic aspects of hernia repair in the United States. Surg Clin North Am 73: 413–426
Lichtenstein IL, Shulman AG, Amid PK, Montllor MM (1989) The tension-free hernioplasty. Am J Surg 157: 188–193
Welsh DRJ, Alexander MAJ (1993) The Shouldice repair. Surg Clin North Am 73: 451–469
Stoppa RE, Warlaumount CK (1995) The preperitoneal approach and prosthetic repair of groin hernias. In: Nyhus LM, Coldon RE (eds) Hernia. 4th ed. JB Lippincott, Philadelphia pp 118–210
EU Hernia Trialists Collaboration (2000) Mesh compared with nonmesh methods of open groin hernia repair: systematic review of randomized controlled trials. Br J Surg 87: 854–859
Scott NW, McCormack K, Graham P, Go PM, Ross SJ, Grant AM (2002) Open mesh versus nonmesh for repair of femoral and inguinal hernia. Cochrane Database Syst Rev 4 CD002197
Memon MA, Cooper NJ, Memon B, Memon MI, Abrams KR (2003) Metaanalysis of randomized clinical trials comparing open and laparoscopic inguinal hernia repair. Br J Surg 90: 1479–1492
Edwards CC 2nd, Bailey RW (2000) Laparoscopic hernia repair: the learning curve. Surg Laparosc Endosc Percutan Tech 10: 149–153
Medical Research Council Laparoscopic Groin Hernia Trial Group (2001) Cost-utility analysis of open versus laparoscopic groin hernia repair: results from a multicentre randomized clinical trial. Br J Surg 88: 653–661
Tsang S, Normad R, Karlin R (1994) Small bowel obstruction: a morbid complication after laparoscopic herniorraphy. Am Surg 60: 332–334
Darzi A, Paraskeva PA, Quereshi A, Menzies-Gow N, Guillou PJ, Monson JR (1994) Laparoscopic herniorraphy: initial experience in 126 patients. J Laparoendosc Surg 4: 179–183
Phillips EH, Arregui M, Carroll BJ, Corbitt J, Crafton WB, Fallas MJ, Filipi C, Fitzgibbons RJ, Franklin MJ, McKernan B, et al (1995) Incidence of complications following laparoscopic hernioplasty. Surg Endosc 9: 16–21
Kald A, Anderberg B, Smedh K, Karlsson M (1997) Transperitoneal or totally extraperitoneal approach in laparoscopic hernia repair: results of 491 consecutive herniorrhapies. Surg Laparosc Endosc 7: 86–89
Neumayer L, Giobbie-Hurder A, Jonasson O, Fitzgibbons R Jr, Dunlop D, Gibbs J, Reda D, Henderson W (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350: 1819–1827
Bittner R, Sauerland S, Schmedt CG (2005) Comparison of endoscopic techniques vs Shouldice and other open nonmesh techniques for inguinal hernia repair: a metaanalysis of randomized controlled trials. Surg Endosc 19: 605–615
Heikkinen TJ, Haukipuro K, Koivukangas P, Hulkko A (1998) A prospective randomized outcome and cost comparison of totally extraperitoneal endoscopic hernioplasty versus lichtenstein hernia operation among employed patients. Surg Laparosc Endosc 8: 338–344
Andersson B, Hallén M, Leveau P, Bergenfelz A, Westerdahl J (2003) Laparoscopic extraperitoneal inguinal hernia repair versus open mesh repair: a prospective randomized controlled trial. Surgery 133: 464–472
Merello J, Guerra GA, Madriz J, Guerra GG (1997) Laparoscopic TEP versus open Lichtenstein hernia repair: randomized trial. Surg Endosc 11: 545
Bilgin B, Özmen MM, Zülfikaroglu B, Cete M, Hengirmen S (1997) Totally extraperitoneal (TEP) hernia repair preperitoneal open repair (PPOR). Surg Endosc 11: 542
Lal P, Kajla RK, Chander J, Saha R, Ramteke VK (2003) Randomized controlled study of laparoscopic total extraperitoneal vs open Lichtenstein inguinal hernia repair. Surg Endosc 17: 850–856
Payne J, Izawa M, Glen P (1996) Laparoscopic or tension-free inguinal hernia repair? A cost benefit analysis of 200 prospective randomized patients. SAGES, Philadelphia
Colak T, Akca T, Kanik A, Aydin S (2003) Randomized clinical trial comparing laparoscopic totally extraperitoneal approach with open mesh repair in inguinal hernia. Surg Laparosc Endosc Percutan Tech 13: 191–195
Bostanci BE, Tetik C, Özer S, Özden A (1998) Posterior approaches in groin hernia repair: open or closed. Acta Chir Belg 98: 241–244
Champault G, Rizk N, Catheline JM, Riskalla H, Boutelier P (1996) Hernies de l’aine: traitment laparoscopique pré-péritoneal versus opération de Stoppa. Etude randomisée: 100 cas. J Chir 133: 274–280
Champault GG, Rizk N, Catheline JM, Turner R, Boutelier P (1997) Inguinal hernia repair: totally preperitoneal laparoscopic approach versus stoppa operation: randomized trial of 100 cases. Surg Laparosc Endosc 7: 445–450
Suter M, Martinet O (2002) Postoperative pulmonary dysfunction after bilateral inguinal hernia repair: a prospective randomized study comparing the Stoppa procedure with laparoscopic total extraperitoneal repair (TEP). Surg Laparosc Endosc Percutan Tech 12: 420–425
Suter M, Martinet O, Spertini F (2002) Reduced acute phase response after laparoscopic total extraperitoneal bilateral hernia repair compared to open repair with the Stoppa procedure. Surg Endosc 16: 1214–1219
Khoury N (1998) A randomized prospective controlled trial of laparoscopic extraperitoneal hernia repair and mesh-plug hernioplasty: a study of 315 cases. J Laparoendosc Adv Surg Tech 8: 367–372
Bringman S, Ramel S, Heikkinen TJ, Englund T, Westman B, Anderberg B (2003) Tension-free inguinal hernia repair: TEP versus mesh-plug versus Lichtenstein. Ann Surg 237: 142–147
Wright DM, Kennedy A, Baxter JN, Fullarton GM, Fife LM, Sunderland GT, O’Dwyer PJ (1996) Early outcome after open versus extraperitoneal endoscopic tension-free hernioplasty: a randomized clinical trial. Surgery 119: 552–557
Wright DM, Hall MG, Paterson CR, O’Dwyer PJ (1999) A randomized comparison of driver reaction time after open and endoscopic tension-free inguinal hernia repair. Surg Endosc 13: 332–334
Simmermacher RK, Van Duyn EB, Clevers GJ, de Vries LS, van Vroonhoven TJMV (2000) Preperitoneal mesh in groin hernia surgery: a randomized trial emphasizing the surgical aspects of preperitoneal placement via a laparoscopic (TEP) or Grid-iron (Ugahary) approach. Hernia 4: 296–298
Nathanson L, Adib R (1996) Randomized trial of open and laparoscopic inguinal hernia repair. Surg Endosc 10: 192
Bessell JR, Baxter P, Riddell P, Watkin S, Maddern GJ (1996) A randomized controlled trial of laparoscopic hernia repair. Surg Endosc 10: 495–500
Decker D, Lindemann C, Springer W, Low A, Hirner A, von Ruecker A (1998) Endoscopic vs conventional hernia repair from an immunologic point of view. Surg Endosc 13: 335–339
Fleming WR, Elliott TB, Jones RM, Hardy KJ (2001) Randomized clinical trial comparing totally extraperitoneal inguinal hernia repair with the Shouldice technique. Br J Surg 88: 1183–1188
Champault G, Benoit J, Lauroy J, Rizk N, Boutelier P (1994) Hernies de l’aine de l’adulte: chirurgie laparoscopique vs opération de Shouldice: étude randomisée controlée: 181 patients: résultats préliminaires. Ann Chir 48: 1003–1008
Liem MS, van der Graaf Y, van Steensel CJ, Boelhouwer RU, Clevers GJ, Meijer WS, Stassen LP, Vente JP, Weidema WF, Schrijvers AJ, van Vroonhoven TJ (1997) Comparison of conventional anterior surgery and laparoscopic surgery for inguinal hernia repair. N Engl J Med 336: 1541–1547
Liem MS, van der Graaf Y, Zwart RC, Geurts I, van Vroonhoven TJ (1997) A randomized comparison of physical performance following laparoscopic and open inguinal hernia repair. Br J Surg 84: 64–67
Liem MSL, Halsema JAM, van der Graaf Y, Schrijvers AJ, van Vroonhoven TJ (1997) Cost effectiveness of extraperitoneal laparoscopic inguinal hernia repair: a randomized comparison with conventional herniorrhaphy. Ann Surg 6: 668–676
Liem MSL, van Duyn EB, van der Graaf Y, van Vroonhoven TJ (2003) Recurrences after conventional anterior and laparoscopic inguinal hernia repair: a randomized comparison. Ann Surg 237: 136–141
Champault G, Barrat C, Catheline JM, Rizk N (1998) Hernies de l’aine. Résultats à 4 ans de deux études prospectives randomisées comparant les opérations de Shouldice et de Stoppa à l’abord laparoscopique totalement pré-péritonéal (461 patients). Ann Chir 52: 132–136
Wright D, Paterson C, Scott N, Hair A, O’Dwyer PJ (2002) Five-year follow-up of patients undergoing laparoscopic or open groin hernia repair: a randomized controlled trial. Ann Surg 235: 333–337
Vatansev C, Belviranli M, Aksoy F, Tuncer S, Sahin M, Karahan O (2002) The effects of different hernia repair methods on postoperative pain medication and CRP levels. Surg Laparosc Endosc Percutan Tech 12: 243–246
Knook MTT, Weidema WF, Stassen LPS, van Steensel CJ (1999) Endoscopic total extraperitoneal repair of primary and recurrent inguinal hernias. Surg Endosc 13: 507–511
Lau H, Patil NG, Yuen WK, Lee F (2002) Management of peritoneal tear during endoscopic extraperitoneal inguinal hernioplasty. Surg Endosc 16: 1474–1477
Collaboration EH (2000) Laparoscopic compared with open methods of groin hernia repair: systematic review of randomized controlled trials. Br J Surg 87: 860–867
Leibl BJ, Jager C, Kraft B, Kraft K, Schwarz J, Ulrich M, Bittner R (2005) Laparoscopic hernia repair: TAPP or/and TEP? Langenbecks. Arch Surg 390: 77–82
The MRC Laparoscopic Groin Hernia Trial Group (1999) Laparoscopic versus open repair of groin hernia: a randomised comparison. Lancet 354: 185–190
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kuhry, E., van Veen, R.N., Langeveld, H.R. et al. Open or endoscopic total extraperitoneal inguinal hernia repair? A systematic review. Surg Endosc 21, 161–166 (2007). https://doi.org/10.1007/s00464-006-0167-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-006-0167-4