Abstract
Background
Although the internal hernias have been a huge topic in the field of bariatric surgery, there were a few reports in gastric cancer. The purpose of this study was to analyze the incidence, clinical features, and prevention of internal hernia after gastrectomy for gastric cancer.
Methods
Twelve patients who underwent surgical treatment for internal hernia in our hospital after gastrectomy were analyzed. Features, including incidence, symptoms, and signs, were investigated in detail.
Results
The operative procedures for preceding gastrectomies were open distal gastrectomy in three patients, open total gastrectomy in three patients, laparoscopic-assisted distal gastrectomy in two patients, and laparoscopic total gastrectomy in four patients. The most frequent sites of internal hernias were jejunojejunostomy mesenteric defects (five patients) and Petersen’s defect (five patients), mesenterium of transverse colon (one patient), and esophagus hiatus (one patient). There was no significant difference between open and laparoscopic preceding gastrectomies. After closure of the mesenteric defect was introduced, no further internal hernias occurred. On CT examination, the whirl sign was present in ten patients on 3D images.
Conclusions
The present data suggest the importance of early recognition and treatment of internal hernia, as well as its prevention by closure of mesenteric defects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A laparoscopic-assisted gastrectomy (LAG) has the advantages of less invasiveness and better cosmetic outcomes. Moreover, several prospective, randomized, controlled trials have concluded that the long-term, disease-free survival of patients who undergo LAG is similar to that of patients who undergo conventional open surgery [1].
Use of the Roux-en-Y reconstruction has been gradually increasing in recent years, most likely to avoid anastomotic leakage and reflux inflammation of the remnant stomach. As a result, the incidence of Roux-en-Y reconstruction methods has increased in laparoscopic distal and total gastrectomy. However, artificial apertures are created iatrogenically during Roux-en-Y reconstruction [2, 3].
Although the internal hernias have been a huge topic in the field of bariatric surgery, there were a few reports in gastric cancer. An internal hernia is defined as a “defect of unusual size within a body cavity, into which intestines may intrude and become incarcerated or strangulated.” Internal hernia is a known complication of laparoscopic Roux-en-Y gastric bypass (LRYGBP), with a reported incidence of 0.2–6.2 %. It has been suggested that the postoperative loss of mesenteric fat and reduced adhesion formation resulting from the laparoscopic approach promote internal hernia development. Studies of complications after gastric Roux-en-Y bypass surgery for obesity have reported a significantly higher incidence of internal hernia after laparoscopic surgery than after open surgery [4–6].
Symptoms vary from nonspecific intermittent abdominal pain of chronic duration to acute abdominal pain associated with nausea, vomiting, and obstipation typical of a small-bowel obstruction. Delay in intervention may result in intestinal gangrene with the need for resection of variable lengths of small intestine, with resultant morbidity and possible mortality [7, 8].
There are only a few reports of internal hernia associated with Roux-en-Y reconstruction after laparoscopic gastrectomy for gastric cancer, especially laparoscopic treatment. The purpose of this study was to analyze the incidence, clinical features, and prevention of internal hernia after gastrectomy for gastric cancer.
Patients and methods
From January 2006 to March 2011, 428 patients underwent gastrectomy for gastric cancer with Roux-en-Y reconstruction at Tokushima University Hospital. They included 295 males and 133 females, aged 37–91 (median 72 years). A total of 250 patients underwent open procedures, whereas 178 patients underwent laparoscopic procedures. The mean follow-up period after gastrectomy is 51.0 months. In our institution, the indications for laparoscopic gastrectomy included T1a(M), T1b(SM), and T2(MP) without lymph node metastasis.
Roux-en-Y procedures
In patients with Roux-en-Y reconstruction, the jejunum was brought up in an antecolic route, although the retrocolic route was occasionally used. In open total gastrectomy, esophagojejunal anastomosis was performed by circular stapler. In laparoscopic-assisted total gastrectomy, anastomosis was initially performed by circular stapler, whereas recently, anastomosis was performed by the overlap method. In distal gastrectomy, anastomosis was performed by the side-to-side method. The jejunojejunostomy was performed by side-to-side methods. In this study, there were 418 patients with antecolic route and ten patients with retrocolic route.
Internal hernia
This study included the 12 patients who underwent surgical treatment for internal hernia in our hospital after gastrectomy for gastric cancer. All patients underwent computed tomography before the emergency operation for internal hernia.
Statistical analyses
The results are expressed as mean ± standard deviation. Statistical significance was set at p < 0.05. Analyses were performed with the Stat Mate III statistical package (Atms Inc., Tokyo, Japan).
Clinical profile of internal hernia after gastrectomy
Twelve patients underwent emergency surgery for internal hernia after gastrectomy for gastric cancer (Table 1). They included 11 men and 1 woman, with a median age of 72 (54–80) years. Concerning the gender ratio of internal hernia, the incidence in male is higher than female (3.7 vs. 0.7 %, p = 0.05). Eleven patients developed hernia within 5 years, but one patient developed an internal hernia after 5 years. The operative procedures for preceding gastrectomy were open distal gastrectomy in three patients, open total gastrectomy in three patients, laparoscopic-assisted distal gastrectomy in two, and laparoscopic total gastrectomy in four patients. The stages in the gastrectomy were I in seven, II in zero, III in two, and IV in three. The retrocolic route was used in one patient.
Body mass index (BMI) of patients
The mean BMI at the time of surgery for internal hernia is 18.5 ± 2.3 kg/m2. On the other hand, the mean BMI at the first gastrectomy is 20.3 ± 1.7 kg/m2.
Incidence of internal hernia
Six patients developed their internal hernia following open gastrectomy (2.4 %), whereas six patients occurred after laparoscopic gastrectomy (3.3 %). There was no significant difference between open and laparoscopic preceding gastrectomies. In retrocolic route, one patient (10 %) had an internal hernia. Compared with the antecolic route, the rate is higher (10 vs. 2.1 %, p = 0.013).
Sites and treatments of internal hernia
The sites of internal hernia were a jejunojejunostomy mesenteric defect (five patients) and Petersen’s defect (five patients). There was one herniation through the esophageal hiatus and one through the mesenteric defect of the transverse mesocolon after a retrocolic approach (Table 2). Bowel resection was performed in two patients (Petersen’s defect and a defect in the mesentery of the transverse colon) because of bowel necrosis. Patients with defects of the mesentery of the transverse colon particularly underwent massive bowel resection and developed short-bowel syndrome. All operations were performed as emergencies. There were no deaths in this series.
Symptoms and preoperative evaluation of internal hernia
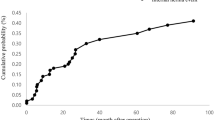
Abdominal pain is a cardinal symptom of internal hernia and was present in all patients. All patients were referred within 24 h of the onset of the symptoms. The next most common presentation was nausea and vomiting. Tachycardia and fever often were present (Table 3). On preoperative evaluation, inflammatory indicator (WBC and CRP) elevations were not often observed, but a high amylase level was frequently observed (nine patients). Acidosis was recognized in bowel resection cases. On preoperative CT examination, small intestinal dilation was observed in all cases, and biliopancreatic limb dilation was observed in seven patients. In our institution, 3D images can be easily constructed on every computer. The whirl sign was present in ten patients on 3D images (Fig. 1). Nine patients had ascites.
Preventive effect for internal hernia
After these cases of internal hernia, the mesenteric defect was closed by 4-0 absorbable thread during all open and laparoscopic procedures. No internal hernia was found after routine closure of the mesenteric defect was introduced.
Discussion
Use of the Roux-en-Y reconstruction has been gradually increasing in recent years, most likely to avoid anastomotic leakage and reflux inflammation of the remnant stomach. The reported incidence of internal hernia among this population rages widely, from 0.2 to 9 %. Increasing evidence suggests that technical factors related to construction of the Roux limb play an important role in determining susceptibility to this complication [9–15].
Studies of complications after gastric Roux-en-Y bypass surgery for obesity have reported a significantly higher incidence of internal hernia after laparoscopic surgery than after open surgery, which suggests reduction of intra-abdominal adhesions. In fact, laparoscopic gastrectomy is more of a risk factor for internal hernia than open surgery. In the present study, there was no significant difference between laparoscopic and open procedures. Therefore, the cause of the internal hernia is also associated with body weight loss. We speculate that significant weight loss may result in enlargement of mesenteric defects over time because of the loss of mesenteric fat, thus enhancing the development of internal hernia [16–19].
In whole patients, the ratio of male to female is 2.2. On the other hand, in large surveillance study in Japan, its rate is 2.5 [20]. Although the rate is similar, the incidence of internal hernia in male is higher than female (3.7 vs. 0.7 %, p = 0.05). In bariatric surgery, gender rate is higher in females [6]. It is very interesting and male is a risk factor for internal hernia.
The definition of the Petersen’s defect is the space between dorsum of the Roux limb and transverse mesocolon [1, 16]. The retrocolic approach create transverse mesocolon, jejunojejunostomy, and Petersen’s defects, whereas the antecolic approach create only two mesenteric defects: jejunojejunostomy and Petersen’s defect [21]. In this study, five patients had internal hernia due to Petersen’s defect. All patients underwent the antecolic route, so the orifice was made between the Roux limb and transverse colon.
Internal hernias are known to be difficult to diagnose clinically. The only constant in patients with internal hernia is abdominal pain with a predilection for the upper abdomen, sometimes radiating to the back. Abdominal pain may be intermittent, because internal hernia may reduce spontaneously. A diagnosis of internal hernia should be considered in patients who present with recurring periumbilical, colicky abdominal pain, with or without nausea and vomiting. Tachycardia has been described in the literature as an important clinical predictor; in fact, most of the patients showed tachycardia in the present study [21–23]. The white blood cell count and CRP level are usually normal. Pancreatic enzymes have been reported to be good indicators of biliopancreatic limb obstruction
The retrocolic technique was a risk factor for intestinal obstruction. In the retrocolic group, internal hernias were the main cause of intestinal obstruction (86 %). In contrast, in the antecolic group, adhesions were the main cause of bowel obstruction, with a low incidence of internal hernia (34 %). In this study, massive bowel resection was performed in patients with the retrocolic technique [4].
With the increased availability of CT scanning, it has become a mainstay in the diagnosis of patients presenting with abdominal symptoms of questionable etiology. Several findings on CT scan pointed not only to the diagnosis of the internal hernia, but also to its location, and correlated well with intraoperative findings. The accuracy of CT scanning in the diagnosis of internal hernia has not been firmly established, but reports have suggested a sensitivity of approximately 60 % and a high specificity [14]. Important signs include the presence of mesenteric vessel engorgement (85 %) or crowding (92 %), displacement of the main mesenteric trunk outside the lateral margin of the aorta by more than the diameter of the aorta (85 %), and evidence of volvulus diagnosed by invasion of the position of the main mesenteric vessels (whirl sign) or an abnormal twisted appearance of the small bowel (38 %). Increased wall thickness and ascites were indicators of ischemic bowel. The most suggestive sign is an abnormal cluster of dilated small-bowel loops pressed along the periphery of the abdominal cavity with no overlying omental fat, causing central displacement of the colon and mesenteric vessels. In this series, 15 % of patients was suspected preoperatively of having internal hernia, mainly by identification of the whirl sign (whirling of the mesentery and mesenteric vessels) [17].
Historically only the jejunojejunostomy mesenteric defect is closed after LYGB for morbid obesity, but in this study, there were five cases with Petersen’s space between Roux ribs and transverse colon. Closure of the mesenteric defects (jejunojejunal defect and Petersen’s space) is recommended for these patients with an antecolic Roux-en-Y reconstruction, to minimize the incidence of internal hernia [9]. In a literature review, it was found that closure of all mesenteric defects, regardless of the technique used, decreased the rate of internal hernias. Possibly the greatest factor affecting the incidence of internal hernia after gastrectomy is closure of the mesenteric defects. Intuitively, an obliterated mesenteric defect should prevent internal hernias. Groups have recommended routine closure of all mesenteric defects, citing the decrease in the incidence of internal hernias after gastric bypass. In fact, after introducing closure of the mesenteric defect, there were no new cases of internal hernia [7].
To prevent the complications of bowel necrosis leading to sepsis, multiorgan failure, or death, we advocate early exploration of any unexplained abdominal pain in patients after gastrectomy, even in the presence of normal results on investigation.
Conclusions
Internal hernias are a specific cause of abdominal pain after gastrectomy with Roux-en-Y reconstruction for gastric cancer. The best course of management is certainly prevention by closure of mesenteric defects at the time of initial operation. In the diagnosis of internal hernia, CT is most useful. We strongly emphasize the importance of early recognition and treatment of internal hernia.
References
Miyagaki H, Takiguchi S, Kurokawa Y, Hirao M, Tamura S, Nishida T (2012) Recent trend internal occurrence after gastrectomy for gastric cancer. World J Surg 36:851–857
Hosoya Y, Lefor A, Ui T, Haruta H, Kurashina K, Saito S (2011) Internal hernia after laparoscopic gastric resection with antecolic Roux-en-Y reconstruction for gastric cancer. Surg Endosc 25:3400–3404
Comeau E, Gagner M, Inabnet WB, Herron DM, Quinn TM, Pomp A (2005) Symptomatic internal hernias after laparoscopic bariatric surgery. Surg Endosc 19:34–39
Onopchenko A (2005) Radiological diagnosis of internal hernia after Roux-en-Y gastric bypass. Obes Surg 15:606–611
Steele KE, Prokopowicz GP, Magnuson T, Lidor A, Schweitzer M (2008) Laparoscopic antecolic Roux-En-Y gastric bypass with closure of internal defects leads to fewer internal hernias than the retrocolic approach. Surg Endosc 22:2056–2061
Escalona A, Devaud N, Perez G, Crovari F, Boza C, Viviani P (2007) Antecolic versus retrocolic alimentary limb in laparoscopic Roux-en-Y gastric bypass: a comparative study. Surg Obes Relat Dis 3:423–427
Gunabushanam G, Shankar S, Czerniach D, Kelly JJ, Perugini RA (2009) Small-bowel obstruction after laparoscopic Roux-en-Y gastric bypass surgery. J Comput Assist Tomogr 33:369–375
Hwang RF, Swartz DE, Felix EL (2004) Causes of small bowel obstruction after laparoscopic gastric bypass. Surg Endosc 18:1631–1635
Coleman MH, Awad ZT, Pomp A, Gagner M (2006) Laparoscopic closure of the Petersen mesenteric defect. Obes Surg 16:770–772
Bauman RW, Pirrello JR (2009) Internal hernia at Petersen’s space after laparoscopic Roux-en-Y gastric bypass: 6.2 % incidence without closure. A single-surgeon series of 1047 cases. Surg Obes Relat Dis 5:565–570
Kumagai K, Hiki N, Nunobe S, Jiang X, Kubota T, Aikou S (2011) Different features of complications with Billroth-I and Roux-en-Y reconstruction after laparoscopy-assisted distal gastrectomy. J Gastrointest Surg 15:2145–2152
Garza E Jr, Kuhn J, Arnold D, Nicholson W, Reddy S, McCarty T (2004) Internal hernias after laparoscopic Roux-en-Y gastric bypass. Am J Surg 188:769–800
Higa KD, Ho T, Boone KB (2003) Internal hernias after laparoscopic Roux-en-Y gastric bypass: incidence, treatment and prevention. Obes Surg 13:350–354
Blachar A, Federle MP (2002) Gastrointestinal complications of laparoscopic Roux-en-Y gastric bypass surgery in patients who are morbidly obese: findings on radiography and CT. AJR Am J Roentgenol 179:1437–1442
Nguyen NT, Goldman C, Rosenquist CJ, Arango A, Cole CJ, Lee SJ (2001) Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg 234:279–291
Carmody B, DeMaria EJ, Jamal M, Johnson J, Carbonell A, Kellum J (2005) Internal hernia after laparoscopic Roux-en-Y gastric bypass. Surg Obes Dis 1:543–548
Cruz-Munoz N, Cabrera JC, Cuesta M, Hartnett S, Rojas R (2011) Closure of mesenteric defect can lead to decrease in internal hernias after Roux-en-Y gastric bypass. Surg Obes Relat Dis 7:176–180
Cho M, Pinto D, Carrodeguas L, Lascano C, Soto F, Whipple O (2006) Frequency and management of internal hernias after laparoscopic antecolic antegastric Roux-en-Y gastric bypass without division of the small bowel mesentery or closure of mesenteric defects: review of 1400 consecutive cases. Surg Obes Relat Dis 2:87–91
Koppman JS, Li C, Gandsas A (2008) Small bowel obstruction after laparoscopic Roux-en-Y gastric bypass: a review of 9527 patients. J Am Coll Surg 206:571–584
Ito Y, loka A, Tsukuma H, Ajiki W, Sugimoto T, Rachet B, Coleman MP (2009) Regional differences in population-based cancer survival between six prefectures in Japan. Cancer Sci 100:1306–1311
Felsher J, Brodsky J, Brody F (2003) Small bowel obstruction after laparoscopic Roux-en-Y gastric bypass. Surgery 134:501–505
Ahmed R, Miskovic D, Vijayaseelan T, O’Malley W, Hanna GB (2012) Root cause analysis of internal hernia and roux limb compression after laparoscopic Roux-en-Y gastric bypass using observation clinical human reliability assessment. Surg Obes Relat Dis 8:158–163
Higa KD, Boone KB, Ho T, Davies OG (2000) Laparoscopic Roux-en-Y gastric bypass for morbid obesity. Arch Surg 135:1029–1034
Disclosures
Drs. Kozo Yoshikawa, Mitsuo Shimada, Nobuhiro Kurita, Hirohiko Sato, Jun Higashijima, Hideya Kashihara have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yoshikawa, K., Shimada, M., Kurita, N. et al. Characteristics of internal hernia after gastrectomy with Roux-en-Y reconstruction for gastric cancer. Surg Endosc 28, 1774–1778 (2014). https://doi.org/10.1007/s00464-013-3384-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-3384-7