Abstract
Background
This study aimed to evaluate the development and outcomes of laparoscopic antireflux surgery in Germany using a nationwide representative survey.
Methods
A written questionnaire including 34 detailed questions and 288 structured items about diagnostic and therapeutic approaches, number of procedures, complications, and mortality was sent to 546 randomly selected German surgeons (33% of the registered general surgeons) at the end of 2000.
Results
The response rate was 72%, and a total of 2,540 antireflux procedures were reported. According to the survey, 81% of all procedures were performed laparoscopically, and 0.1% were performed thoracoscopically. As reported, 65% were total fundoplications, 31% were partial fundoplications, and 4% were other procedures. Of the surgeons who had experience with laparoscopic antireflux techniques (29%), 71% preferred a 5-trocar technique, and 91% used the Harmonic Scalpel for dissection. There were significant technical variations among the surgical procedures (e.g., use and size of the bougie, length of the wrap, additional gastropexy, fixation of the wrap). The overall complication rate for laparoscopic fundoplication was 7.7% (5.7% surgical and 2% nonsurgical complications), including rates of 0.6% for esophageal perforations and 0.6% for splenic lesions. The conversion rate was 2.9%; the reoperation rate was 1.6%; and the overall hospital mortality rate was 0.13%. The authors observed a striking learning curve difference in complication rates between hospitals performing fewer than 10 laparoscopic antireflux techniques annually and those performing more than 10 fundoplications per year (14% vs 5.1%, p < 0.001). Long-term dysphagia and interventions occasioned by dysphagia occurred significantly more often after total fundoplications than after partial fundoplications (6.6% vs 2.4%; p < 0.001). Similar findings were reported for Nissen versus floppy Nissen procedures. The overall failure rate, however, was similar for both groups (Nissen 8.7%; partial 9%, difference not significant).
Conclusions
Until now, no unique laparoscopic antireflux technique has been accepted, and a number of different antireflux procedures with numerous modifications have been reported. The morbidity and mortality rates reported in this article compare very well with those in the literature, and 1-year-follow-up results are promising.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
As in most Western countries, gastroesophageal reflux disease (GERD) is endemic in Germany, and minimally invasive surgery has become more and more important as a treatment option for this disease. Despite initial criticism, standardized laparoscopic procedures have been developed for most abdominal diseases requiring surgery, and special training schemes to keep complication rates low are available [21]. Laparoscopic antireflux procedures are widely accepted, and early results are reported by many surgeons. These results are published primarily by centers with high case numbers and good results, whereas the actual complication rates might be rather underestimated.
Because large randomized studies are not available, it appears necessary to evaluate large patient numbers retrospectively. This evaluation will be helpful for both patient information and quality control. The use of an anonymous questionnaire contributed to an honest report of negative results that otherwise would not be available for scientific evaluation.
We describe the results of an anonymous representative poll among German surgeons. These results describe the “German experience” with a nonselected patient population and allow us to survey their approach to the treatment of GERD.
Materials and methods
Selection of surgeons
On the basis of address information for all German surgical departments, including private practitioners [4], a random selection of every third institution (n = 546) was asked to answer our survey. Departments and private practitioners obviously not trained in the treatment of GERD (e.g., orthopedic surgeons and vascular surgeons) were excluded before the survey.
Questionnaire
A total of 34 detailed questions required answers concerning 288 structured items. The questions asked for the actual use of diagnostic and therapeutic procedures and the exact number of procedures, as well as treatment-related early morbidity, hospital mortality, and 1-year follow-up data. To increase the validity of the answers, the questions were very detailed and exact. We were especially interested in evaluating the assumed large variation of surgical procedures performed.
The figures were classified by the responders as “counted” or “estimated.” For the evaluation of complication, conversion, and mortality rates, and outcome, only “counted” data were considered. The data shown in the tables represent morbidity and mortality rates (%) for the different study groups.
Statistical analysis
Complications and outcome data were counted and presented as mean percentage rates referring to the corresponding total study population. For comparison of nonquantitative data, the χ2-test was used. Parametric data were tested using one-way analysis of variance (ANOVA) (SigmaStat for Windows 2.03; SPSS Inc., Chicago, USA). Data are presented as mean, median, and range of the different parameters for each responding hospital. Differences were considered as statistically significant at a p value less than 0.05.
Results
Responding surgeons
By the end of 2001, 71.8% (n = 392) of all the questionnaires had been returned, with 228 respondents answering that they do not perform antireflux surgery. Detailed data suitable for statistical evaluation were available from 120 hospitals. These institutions submitted detailed “counted” data regarding mortality and morbidity. The responses from 44 hospitals included only short answers regarding diagnostic and therapeutic strategies for GERD (Table 1).
Surgical procedures, hospital size, type of institution, and number of surgeons
The 392 hospitals included in our study performed 620,448 operations in 1999. These included 2,540 antireflux procedures were performed in 164 hospitals (Table 1). The hospitals performing laparoscopic antireflux surgery usually are larger (84 ± 33 vs 58 ± 27 beds) and perform significantly more operations per year (2190 ± 1085 vs 1146 ± 686; p < 0.001). In 1999, 92% of the university hospitals (23/25) and 75% of the academic hospitals (60/80) were performing antireflux surgery, but only 34% (81/237) of the community and private nonacademic hospitals and none of the private practitioners were doing so (Table 1).
Surgery was performed laparoscopically in 2,053 cases (80.8%) in 113 hospitals (mean, 18.5 procedures per center and year; median, 7; range, 0–320), and using the open approach in 485 cases (19.1%) in 124 hospitals (mean, 3 procedures per center annually; median: 7; range: 0–20). One hospital performed two thoracoscopic antireflux procedures.
The surgical procedures chosen were reported for 1,909 cases. These procedures included 1,289 total fundoplications (65%) (49% using modified Nissen- Rosetti, 9% using Nissen–Rosetti, 35% using floppy Nissen, 3% using Nissen, and 4% using other modifications), 620 partial fundoplications (31%) (83% using posterior partial Toupet fundoplications, 13% using anterior hemifundoplications [AHFP], 0.8% using posterior partial Guarner fundoplications, 0.2% using Hill procedures, and 2.4% using other modifications), 81 other techniques (4%) (e.g., Lig. teres plasty, Vicryl-mesh, Lortat-Jacob procedure) (Fig. 1).
In 2000, 113 (29%) of the 392 responding hospitals had experience using laparoscopic surgery for GERD. Of these, 53% began to use this approach between 1998 and 2000, 34% between 1995 and 1997, and 13% before 1994. In addition, 18% of the hospitals actually not performing any antireflux surgery planned to start laparoscopic antireflux surgery in the near future. In 1999, 69 (61%) of the hospitals performing laparoscopic antireflux surgery had performed fewer than 11 laparoscopic fundoplications; 14 (12%) reported 11 to 20 laparoscopic fundoplications; and 11 (10%) performed up to 50 procedures, 9% more than 50 fundoplications. There was an average of 2.1 surgeons per hospital performing laparoscopic fundoplications. As reported, 34% of the centers had only 1 qualified surgeon performing laparoscopic antireflux surgery; 56% had 2 or 3, qualified surgeons; and 10% had 4 or 5 qualified surgeons. The individual experience per surgeon was 9.7 laparoscopic antireflux procedures in 1999 (university hospitals, 8.1; nonuniversity hospitals, 10.4).
Preoperative diagnostic procedures
Preoperative upper gastrointestinal (GI) endoscopy was considered to be mandatory by all surgeons, and barium swallow by 61%. Esophageal function tests (manometry and 24-h pH study) were always used by 60%. Other tests such as the 24-h gastric pH study, photo-optic bilirubin assessment, and gastric emptying scintigraphy were used only optionally (Table 2).
Of all hospitals performing antireflux surgery, 25% performed endoscopies (23 university hospitals [70%] and 97 others [19%]), and 16% performed esophageal functional studies including manometry and pH studies (university hospitals, 57%; others, 7%) in their own departments.
Standard procedure
In the survey, 111 hospitals reported whether a standard antireflux procedure existed in their department or not. Whereas 85% reported an existing standard procedure, 15% did not have a standard procedure. The major reason for the choice of the standard procedure was “convincing own results” (67%), followed by “better standardization” and convincing reports in the literature (53%). Of all the hospitals, 26% mentioned that their procedure of choice would correspond to “expert opinion.” Only 20% considered their procedures as “the one with fewer complications,” and only 19% considered their choice to be “technically easier.” As their method of choice, 64% chose a 360° procedure (Nissen, 16%; Nissen-Rosetti, 27%; Floppy-Nissen, 21%). Partial fundoplications were standard in 10% of the hospitals (Toupet, 5%; AHFP, 5%). Both 360° fundoplication and a Toupet-procedure were reported as standard procedures by 9%. Other procedures such as Ligamentum teres plasty, implantation of a prolene mesh, and esophagofundopexy according to Lortat-Jacob were specified by 3%.
There was a striking difference regarding the choice of standard procedure between university and nonuniversity hospitals, with 22% of the universities performing partial fundoplications (AHFP in 17%; Toupet in 6%) as the standard procedure. On the other hand, only partial fundoplications were performed in 10% of the nonuniversity hospitals (AHFP in 3%; Toupet in 7%, difference not significant). According to the findings, 55% of the surgeons made their surgical decision according to the results of preoperative diagnostic findings, with 41% choosing a partial fundoplication in cases with esophageal motility dysfunction, 9% choosing a Nissen procedure, 3% choosing a gastropexy, and 4% not performing antireflux surgery for these patients or referring them to specialized centers. These questions were not answered by 41% of the surgeons, who had no experience in this field.
Open operation: primary choice and conversion
Laparoscopic surgery was the standard approach in 113 (69%) of the 164 hospitals, with 31% performing open surgery for GERD. In cases of recurrent disease, 46% chose laparoscopic surgery, whereas 49% used the open approach for these cases, and 4% chose the transthoracic approach (open, 2%; thoracoscopically, 2%), with 1% of the surgeons using the thoracoscopic or open abdominal approach. Almost half of the surgeons (49%) saw no indication for a primarily open approach and started every antireflux procedure laparoscopically. As a reason for a primary open approach, 32% defined prior abdominal operations. Further reasons included refundoplications (32%), giant hiatal hernias (8%), aged patients (4%), and others (12%).
The overall conversion rate was 2.9% (mean per center annually, 7%; median, 0; range, 0–100)%). Figure 2 shows the reasons for conversion to open surgery. The most common causes were bleeding (41.7%) and technical problems (16.7%). Other reasons were adhesions (16.7%), esophageal perforations (8.3%), injuries to the spleen (8.3%), and injuries to the stomach wall (2.8%).
General technical aspects
Standard access
For laparoscopic fundoplication, 71% of all surgeons routinely used five trocars in 2000; 26% used four trocars; and 3% performed the procedures using a six- or three-trocar technique. For creation of the pneumoperitoneum, 69% used the Veress needle, and 31% used the open (Hassan) technique. The overwhelming majority (91%) routinely used the Harmonic Scalpel for dissection, with 5% using the electric scissors, and another 4% using the hook cautery.
Dissection of the crura and hiatoplasty, and intraoperative endoscopy
In 2000, dissection of the crura together with esophageal mobilization was mandatory in 31% of the hospitals. Another 44% performed this technique in selected cases, and 11% never used it (Table 3). A bougie was always used by 46%, used selectively by 15% and never used by 24% of the hospitals.
The great majority of the hospitals (94%) performed a posterior hiatoplasty, whereas 6% performed an anterior hiatoplasty. Intraoperative routine endoscopy was always performed by 6% and selectively used by 22% of the surgeons.
Technical details of the wrap (360° fundoplication, AHFP, Toupet)
With regard to the wrap construction, numerous technical variations in the antireflux procedures were observed (Table 4). Of the 120 hospitals (12.5%) that sent a completed questionnaire, 15 reported that they did not use a 360° procedure at all. Another 96 hospitals sent detailed information regarding the details of the 360° fundoplication used in their institution. The wrap length varied from 2 to 9 cm (2–3 cm, 53%; 3.5–6 cm, 39%; 6.5–9 cm, 8%), The number of sutures varied from 2 to 8 (2–3, 63%; 4, 25%; 5–8, 12%). In 81% of the hospitals, the wrap was fixed to the esophagus, with 16% also fixing the wrap to the crura. As reported, 73% of the surgeons used a bougie for calibration (small bougie [8–15 mm], 66%; large bougie [>15 mm], 34%), and 27% did not use any bougie.
Similarly, we observed interhospital differences regarding the techniques used for partial fundoplications. Of 45 hospitals that sent detailed information regarding their Toupet procedure, 52% (62/120) reported that they did not use this procedure at all. The desired extension of their posterior partial fundoplication varied between 180° and 270° (180°, 8%; 180–270°, 55%; 270°, 37%). According to the survey, 15% of the hospitals used sutures between the wrap and both crura (university hospitals, 44%; nonuniversity hospitals, 8%), and another 15% used stitches only to the left. Still another 70% used stitches only to the right crus. No use was made of AHFP by 81% (97/120), and 13% of the hospitals performing this procedure did not include the esophagus in their fixation. In addition to the wrap fixation to the right crus, 27% of the surgeons also used sutures between the wrap and the anterior commissure, and 18% also used stitches to the left crus. An additional fundopexy was performed by 20% of the surgeons.
Additional gastropexy
Whereas 7% of the surgeons always completed the fundoplication with an additional gastropexy, 39% did so in selected cases. The most frequently performed gastropexy was a fundophrenicopexy (63%), and 18% performed an anterior corpopexy by suturing the stomach to the abdominal wall.
Complications, mortality, and reoperations
The overall complication rate after laparoscopic fundoplication was 7.7% (mean per center, 10.5%; median, 0%; range, 0–100%). The rate was 5.7% for surgical complications (mean per center, 8.9%; median, 0%; range, 0–100%) and 2% for general complications (mean per center, 1.7%; median, 0%, range, 0–40%) (Table 5).
The most frequent surgical complications were lesions of the pleura and wound healing problems (respectively, 1.9% and 0.8% of the evaluated cases). Major complications such as esophageal perforations and lesions of the stomach wall were reported, respectively, in 0.6% and 0.5% of all cases. Furthermore, there were 0.4% intra- and postoperatively diagnosed bleeding complications, 0.6% involving injuries of the spleen and 0.1% involving other intraabdominal septic complications.
We were furthermore interested in evaluating whether a relationship between complication rates and the average experience of the hospital, expressed by the number of surgical procedures performed per year, would be detectable: Significant experience-related differences were found for hospitals performing up to 10 fundoplications per year (14%), as compared with hospitals performing more than 10 procedures per year (5.1%; p < 0.001). No further significant differences were found between hospitals performing more than 20, 30, or 40 fundoplications per year. Despite these findings, lesions of the pleura occurred most often in more experienced departments, with 27 of the 31 reported lesions occurring in hospitals performing more than 25 fundoplications per year (p < 0.01).
The overall reoperation rate after laparoscopic fundoplication was 1.6%, including a relaparotomy rate of 1.1% and a relaparoscopy rate of 0.5%.
Hospital mortality was reported to be 0.1%, which resulted from a pulmonary embolism after floppy Nissen fundoplication in one case and a nonspecified surgical complication after Toupet fundoplication in another case. Both lethal complications occurred in experienced university hospitals that performed more than 35 fundoplications per year. The mean postoperative hospital stay after laparoscopic fundoplication was 6.5 ± 2.4 days.
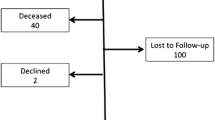
Technique-related outcome
Counted data suitable for outcome evaluation after antireflux procedures were available from 56 hospitals with a total of 2,059 cases. The minimum follow-up period for these patients was 1 year. In the survey, 46 hospitals reported follow-up results for patients who underwent surgery in 1999 and had follow-up data until the end of 2000. A total of 10 hospitals reported their cumulative results since initiation of laparoscopic antireflux surgery (median, 1995), with a minimum follow-up of 1 year.
Short-term dysphagia during the first month after surgery occurred in 39.1% of all the patients (median per center, 19.4; range, 0–100 %), with no differences between 360° and partial fundoplications (Table 6). Dysphagia lasting 4 to 12 weeks occurred significantly more often after 360° fundoplications (8.2% vs 2.5%, respectively). Approximately 4.5% of all patients reported dysphagia that lasted longer than 12 weeks. Again, a significant difference between 360° fundoplications and partial fundoplications was observed (6.6% vs 2.4%; p < 0.001). Even among the various 360° procedures, significant differences were observed (Table 6): Patients with short floppy Nissen had a long-term dysphagia rate of 3.6%, as compared with 6.6% after the original Nissen/Nissen–Rosetti procedure (p = 0.10). No significant differences were observed with regard to dysphagia in comparisons of Nissen and Nissen–Rosetti, use and size of the bougie, and hiatoplasty technique using the choices “never,” “always,” “selected cases.” Of the patients who underwent 360° fundoplication, 2.6% required intervention (dilation) because of dysphagia, which was not necessary after partial fundoplication (p < 0.001).
The overall failure rate was 9.3%, which included 3.8% symptomatic and 5.5% asymptomatic recurrences. There was no difference between partial and 360° fundoplications in terms of recurrence rates. Nonetheless, recurrent disease was significantly reduced with short floppy Nissen (2.3%), as compared with the original Nissen/Nissen–Rosetti procedure (13.5%; p < 0.001).
Discussion
This study demonstrates the different procedures used for antireflux surgery in Germany. Although the introduction of laparoscopic cholecystectomy in Germany occurred very rapidly [19], the breakthrough for laparoscopic antireflux surgery did not develop before the end of the 1990s. Only 13% of the responding surgeons had started laparoscopic antireflux procedures by 1994. Since then, the number of hospitals offering laparoscopic surgery for GERD has increased dramatically. Of all the surgeons performing antireflux procedures, 34% started between 1995 and 1997, and 53% started between 1998 and 2000. In addition, an increasing number of patients undergoing surgery for GERD can be observed in Germany [14]. Similar findings are reported from other countries [20, 25, 27, 34].
Meanwhile, outpatient centers also have reported antireflux surgery, describing high case numbers and low morbidity and mortality rates [12]. Whereas most antireflux procedures in Germany were performed via laparotomy in 1995 [14], we observed 81% laparoscopic procedures in 1999. The experience of individual surgeons also increased during this period. One surgeon actually was performing an average of 10 laparoscopic antireflux procedures in 1999.
Most surgeons obviously follow an algorithm in preoperative diagnostic testing. Although preoperative endoscopy is mandatory for all surgeons, functional studies such as esophageal manometry, 24-h pH-monitoring, and barium swallow are mandatory only for 60%. However, in comparison with an previous nonrandomized study [14], this ratio has almost doubled. Modern methods of surgical education [21] and increasing numbers of consensus conferences [1–3, 10, 11, 13, 22] may have contributed to this development. Additional tests such as photo-optic bilirubin tests, 24-h gastric pH studies for assessing duodenoesophageal reflux, and gastric or esophageal emptying studies do not play a fundamental role in overall patient management in Germany. These findings are in agreement with the recommendations of the European Association for Endoscopic Surgery [10].
With case numbers increasing, an ongoing discussion regarding the procedure of choice with low rates of recurrent disease and few side effects has been initiated. The dangerous complications of Nissen fundoplication has resulted in various modifications of the original procedure, with exclusive or facultative use of partial wraps in a number of hospitals [17, 33–35]. This also was shown by the current study. Of the participating surgeons, 64% performed a 360° fundoplication as the standard procedure, whereas 10% chose a partial fundoplication as the standard operation. More than half of the surgeons, however, chose the different procedures in agreement with the results of preoperative functional tests. This so-called “tailored concept” is intended to minimize the risk of postoperative dysphagia through the use of a partial “weaker” wrap for patients with a weaker esophageal persistalsis. This concept is followed in a number of hospitals with promising results [17, 18, 33]. However, the randomized study addressing this issue by Rydberg et al. [24] failed to demonstrate any advantages of this concept.
An overall trend toward partial fundoplications has been described in another national report [34]. In 1995, 75% of all hospitals with a partial wrap as their standard procedure used the anterior hemifundoplication [14]. In 1999, only 45% of these hospitals still performed this procedure, most of them being university hospitals. The reasons for this development are beyond the scope of this study. Unfortunately, no randomized study exists that shows the advantage of one procedure over the others.
Considering the actual reported numbers of surgical procedures, it is surprising that more partial fundoplications were performed (31%) than would have been expected as a chosen standard procedure. As indicated by the case numbers, it appears that more experienced centers tend to perform increasing numbers of partial fundoplications. The observation that hospitals with lower case numbers mainly performed 360° fundoplications may be explained by different reasons. During the initial phase of laparoscopic surgery, most surgeons usually apply their experiences from open surgery. The decision to change a surgical procedure usually depends on increasing experience with the laparoscopic approach and on higher case numbers. During recent years, the authors have observed in laparoscopic training sessions that German surgeons are trained mainly in 360° fundoplications. It may well be that most surgical “trend setters” in Germany favor this method. However, a previous study [14] shows by comparison that the ratio of partial fundoplications has not changed in Germany.
The authors were surprised by the findings that more than 50% of the responding surgeons never dissect the crura, or do so only in selected cases, and that almost 25% of the surgeons perform a hiatoplasty only selectively. Similar results are reported from Italy [35]. Only 46% always use a bougie to calibrate the tightness of the hiatus. These findings are in contrast to the recommendations of the European Association for Endoscopic Surgery [10] and the European Study Group for Antireflux Surgery (ESGARS) [13]. As reported, 7% always combine the fundoplication with an additional gastropexy, and another 35% use gastropexy selectively. The use of gastropexy may help to avoid a paraesophageal recurrence, which is a worrisome complication reported in up to 7% after laparoscopic Nissen procedures (see review in [29]).
Numerous differences in the technical details of wrap construction have been reported. It appears that especially during the Nissen procedure, no standards exist regarding the number of sutures, the length of the wrap, and the use and size of the bougie. With regard to to the so-called “Toupet” fundoplication, fewer then 40% of the surgeons try to get a real 270° wrap, and only 15% fix the wrap to both crurae as described for the original Toupet procedure [26]. The other reported techniques are modifications of the Toupet fundoplication or similar posterior 180° fundoplication according to Guarner [15]. As for anterior hemifundoplication, the reported technique of various hospitals is closer to the 120° Watson procedure [28] than to a real anterior 180° hemifundoplication.
The technical variations described in this report compare well with the evaluation of the procedure used by the surgeons. Fewer than one-fourth of the participants reported that their technique was in agreement with expert opinion. Even fewer surgeons considered their technique as technically less demanding or reported fewer complications. Two-thirds of the surgeons, however, were satisfied with their results.
Despite these wide technical variations, the reported rates for overall mortality (0.1%) and complications (7.7%), including esophageal perforation (0.6%) as most serious complication, compare well with those in the literature. Complication rates for laparoscopic fundoplication in other regional or national surveys [6, 14], multicenter studies [7, 23, 35], and reviews of the literature [29, 30] range between 3.5% and 15%, with mortality rates between 0% and 0.5%. Complication rates for partial (Toupet and AHFP) and 360° fundoplication also are comparable.
The high number of surgical complications after AHFP is not in agreement with the literature [16, 17, 32]. This again must be discussed in light of the reported low case numbers. Of the 11 complications during AHFP, including all major complications reported, 5 (1 esophageal perforation, 2 splenic lesions, 1 bleeding and 1 lesion of the stomach wall) occurred at one hospital with an overall complication rate of 83%. This is in agreement with the overall results showing that complication rates in less experienced centers (<10 fundoplications per year) are three times higher than the rates in experienced centers. Moreover, minor complications such as pleural lesions have been reported primarily from experienced centers. In these centers, rates up to 6.3% for intraoperative pleural lesions were reported [17]. A recent review reported pleural lesion rates lower than 2% [29], which also is in agreement with our findings (1.9%). This complication occurs mainly because of injury to the left pleural membrane during retroesophageal dissection, and usually does not require therapeutic intervention. A thoracic drain was placed in only 25% of all patients in the current survey. Others, however, have reported the general use of a thoracic drain after intraoperative pleural lesions [17]. It appears that more experienced surgeons perform a wider mobilization of the esophagus, which would explain the higher incidence of pleural lesions at these centers.
The reoperation rate reported for this study (1.6%) compares favorably with that in the literature [29, 35]. Nonetheless, the risk depends on the length of the follow-up period. The DeMeesters group recently reported a surprisingly high reoperation rate of 3% for trocar hernias after laparoscopic reflux operations [5].
The reported 1-year follow-up results showing an overall recurrence rate of 9.3% and a long-term dysphagia rate of 4.5% are promising. Nonetheless, notable differences with regard to the outcome of the various methods have been observed. With comparable recurrence rates, significantly more long-term dysphagia and dysphagia requiring reintervention were observed after Nissen fundoplications than after partial fundoplications. This is in agreement with the randomized study addressing this issue reported by Watson et al. [31]. Until now, long-term results had not been published. Similar but statistically nonsignificant differences between floppy Nissen [8, 9] and nonfloppy Nissen were reported. Regarding the use and size of the bougie as well as the type of a hiatoplasty, no significant differences in outcome were observed. The latter also is in agreement with another randomized study [31].
All these observations require further studies within the framework of quality assurance programs that have been established in various German states (e.g., for laparoscopic cholecystectomy or inguinal hernia repair). The current study shows significant variations in the different procedures used for antireflux surgery, which is an important finding that must be considered when the outcome and long-term results of different surgical centers are compared.
The reliability of self-reported data may be uncertain, and we cannot rule out the possibility that the nonresponders had results no worse than those described in this report. On the other hand, a number of institutions with low patient numbers and considerably high complication rates also reported their poor results, with complication rates as high as 100%. In addition, a completely anonymous data collection was warranted, and the majority of participating hospitals transmitted prospectively collected data within the framework of internal quality controls. We, therefore, are convinced that our study has high reliability.
Conclusion
This anonymous representative study allows for the estimation of overall risks in antireflux surgery, with special attention focused on the numerous techniques. It also includes the poor results of single institutions. This is important with regard to legal aspects. The study also allows the evaluation of diagnostic and technical trends as well as the estimation of their effects on complication rates. The overall complication and mortality rates are within the range reported in the literature. Data suggest that there is no place for the occasional laparoscopist in laparoscopic surgery for these advanced procedures. The best surgical technique for GERD, however, remains a subject of debate, and should be assessed with prospective randomized clinical studies.
References
Anonymus (2000) French-Belgian Consensus Conference on Adult Gastro-oesophageal Reflux Disease “Diagnosis and Treatment”: report of a meeting held in Paris, France on 21–22 January 1999. The jury of the consensus conference. Eur J Gastroenterol Hepatol 12: 129–137
Beck IT, (1997) Guidelines of the previous consensus conference and recent developments. Can J Gastroenterol 11(Suppl B): 21B–27B
Beck IT, Champion MC, Lemire S, Thomson AB, Anvari M, Armstrong D, Bailey RJ, Barkun AN, Boivin M, Bursey RF, Chaun H, Chiba N, Cockeram AW, Connon JJ, Da Costa LR, Faloon TR, Fedorak RN, Gillies RR, Goeree R, Hunt RH, Inculet RI, Klein A, Leddin DJ, Love JR, Worobetz LJ (1997) The Second Canadian Consensus Conference on the Management of Patients with Gastroesophageal Reflux Disease. Can J Gastroenterol 11(Suppl B): 7B–20B
Berufsverband der Deutschen Chirurgen (1998) Deutsche Chirurgie ‘98—Kliniken, Krankenhäuser, und Praxen in der Bundesrepublik Deutschland. Aktiv Druck und Verlag GmbH, Ebelsbach, Deutschland
Bowrey DJ, Blom D, Crookes PF, Bremner CG, Johansson LM, Lord RV, Hagen JA, DeMeeseter SR, DeMeester TR, Peters JH (2001) Risk factors and the prevalence of trocar-site herniation after laparoscopic fundoplication. Surg Endosc 15: 663–666
Champault G (1994) Réflux gastro-oesophagien—traitement par laparoscopie: 940 cas, expérience francaise. Ann Chir 48: 159–164
Cuschieri A, Hunter J, Wolfe B, Swanstrom LL , Hutson W (1993) Multicenter prospective evaluation of laparoscopic antireflux surgery: preliminary report. Surg Endosc 7: 505–510
DeMeester TR, Bonavina L, Albertucci M (1986) Nissen fundoplication for gastroesophageal reflux disease: evaluation of primary repair in 100 consecutive patients. Ann Surg 204: 9–20
Donahue PE, Larson GM, Stewardson RH, Bombeck CT (1977) Floppy Nissen fundoplication. Rev Surg 34: 223–224
EAES (1997) Laparoscopic antireflux surgery for gastroesophageal reflux disease (GERD): results of a consensus development conference. Held at the Fourth International Congress of the European Association for Endoscopic Surgery (EAES), Trondheim, Norway, 21–24 June, 1996. Surg Endosc 11: 413–426
Eypasch E, Thiel B, Sauerland S (2000) Laparoscopic fundoplication for gastroesophageal reflux disease. Langenbecks Arch Surg 385: 57–63
Finley CR, McKernan JB (2001) Laparoscopic antireflux surgery at an outpatient surgery center. Surg Endosc 15: 823–826
Fuchs KH, Feussner H, Bonavina L, Collard JM, Coosemans W (1997) Current status and trends in laparoscopic antireflux surgery: results of a consensus meeting. The European Study Group for Antireflux Surgery (ESGARS). Endoscopy 29: 298–308
Fuchs KH, Heimbucher J, Freys SM, Fein M, Thiede A (1998) Laparoskopische antirefluxchirurgie: erfahrungsbericht aus Deutschland. Zentralbl Chir 123: 1152–1156
Guarner V, Degollade JR, Tore NM (1975) A new antireflux procedure at the esophagogastric junction: experimental and clinical evaluation. Arch Surg 110: 101–106
Hüttl TP, Meyer G, Arck D, Lang R, Kousal K, Schildberg FW (1999): Die laparoskopische anteriore hemifundoplikatio: eine vorteilhafte alternative in der antirefluxchirurgie [Abstract]. Acta Chir Austriaca 153: 49
Kleimann E, Halbfass HJ (1999) Laparoskopische antirefluxchirurgie bei gastrooesophagealer refluxkrankheit: Ein 4-Jahres-Erfahrungsbericht. Chirurg 70: 456–463
Klingler PJ, Hinder RA, Smith SL, Branton SA, Floch NR, Seelig MH (1998) Laparoskopische antirefluxverfahren. Chirurg 69: 148–157
Krämling HJ, Hüttl TP, Heberer G (1999) Development of gallstone surgery in Germany. Surg Endosc 13: 909–913
McMahon RL, Mercer CD (2000) National trends in gastroesophageal reflux surgery. Can J Surg 43: 48–52
Meyer G, Hüttl TP (2001) Laparoscopic surgery in Europe: development and education. Surg Endosc 15: 229–231
Moss SF, Arnold R, Tytgat GN, Spechler SJ, Delle-Fave G, Rosin D, Jensen RT, Modlin IM (1998) Consensus Statement for Management of Gastroesophageal Reflux Disease: result of workshop meeting at Yale University School of Medicine, Department of Surgery, 16–17 November 1997. J Clin Gastroenterol 27: 6–12
Pessaux P, Arnaud JP, Ghavami B, Flament JB, Trebuchet G, Meyer C, Huten N, Champault G (2000) Laparoscopic antireflux surgery: comparative study of Nissen, Nissen–Rossetti, and Toupet fundoplication. Societe Francaise de Chirurgie Laparoscopique. Surg Endosc 14: 1024–1027
Rydberg L, Ruth M, Abrahamsson H, Lundell L (1999) Tailoring antireflux surgery: a randomized clinical trial. World J Surg 23: 612–618
Sandbu R, Haglund U, Arvidsson D, Hallgren T (2000) Antireflux surgery in Sweden, 1987–1997: a decade of change. Scand J Gastroenterol 35: 345–348
Toupet A, (1963) Technique d’oesophago-gastroplastie avec phréno-gastropexie appliquée dans la cure radicale des hernies hiatales et comme complément de l’operation de Heller dans les cardiospasmes. Acad Chir 89: 394–399
Viljakka M, Luostarinen M, Isolauri J (1997) Incidence of antireflux surgery in Finland 1988–1993. Influence of proton pump inhibitors and laparoscopic technique. Scand J Gastroenterol 32: 415–418
Watson A, Spychal RT, Brown MG, Peck N, Callander N (1995) Laparoscopic “physiological” antireflux procedure: preliminary results of a prospective symptomatic and objective study. Br J Surg 82: 651–656
Watson DI, de Beaux AC (2001) Complications of laparoscopic antireflux surgery. Surg Endosc 15: 344–352
Watson DI, Jamieson GG (1998) Antireflux surgery in the laparoscopic era. Br J Surg 85: 1173–1184
Watson DI, Jamieson GG, Devitt PG, Kennedy JA, Ellis T, Ackroyd R, Lafullarde T, Game PA (2001) A prospective randomized trial of laparoscopic Nissen fundoplication with anterior vs posterior hiatal repair. Arch Surg 136: 745–751
Watson DI, Jamieson GG, Pike GK, Davies N, Richardson M, Devitt PG (1999) Prospective randomized double-blind trial between laparoscopic Nissen fundoplication and anterior partial fundoplication. Br J Surg 86: 123–130
Wetscher GJ, Glaser K, Wieschemeyer T, Gadenstaetter M, Prommegger R, Profanter C (1997) Tailored antireflux surgery for gastroesophageal reflux disease: effectiveness and risk of postoperative dysphagia. World J Surg 21: 605–610
Windsor JA, Yellapu S (2000) Laparoscopic antireflux surgery in New Zealand: a trend towards partial fundoplication. Aust N Z J Surg 70: 184–187
Zaninotto G, Molena D, Ancona E (2000) A prospective multicenter study on laparoscopic treatment of gastroesophageal reflux disease in Italy: type of surgery, conversions, complications, and early results. Study Group for the Laparoscopic Treatment of Gastroesophageal Reflux Disease of the Italian Society of Endoscopic Surgery (SICE). Surg Endosc 14: 282–288
Acknowledgment
The authors thank all the participating surgeons and surgical departments that contributed to their study. This work is part of the medical thesis of Mr. Matthias Hohle at the Ludwig-Maximilians-University, Munich.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hüttl, T.P., Hohle, M., Wichmann, M.W. et al. Techniques and results of laparoscopic antireflux surgery in Germany. Surg Endosc 19, 1579–1587 (2005). https://doi.org/10.1007/s00464-005-0163-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-005-0163-0