Abstract
Background: Continuous ambulatory peritoneal dialysis (CAPD) is an effective form of treatment for patients with end-stage renal disease. Open insertion of peritoneal dialysis (PD) catheters is the standard surgical technique, but it is associated with a relatively high incidence of catheter outflow obstruction and dialysis leak. Omental wrapping is the most common cause of mechanical problems. The purpose of this study was to determine the efficacy of the laparoscopic omental fixation technique to prevent the obstruction caused by omental wrapping and also to compare this laparoscopic technique with open peritoneal dialysis catheter insertion with respect to postoperative discomfort, complication rates, and catheter survival. Methods: Between March 1998 and October 2001, 42 double-cuff, curled-end CAPD catheters were placed in 42 patients. The outcomes of the 21 patients in whom the PD catheters were placed laparoscopically with omental fixation technique were compared with those of the 21 patients in whom the catheters were placed with open surgical technique. Recorded data included patient demographics, catheter implantation method, early and late complications, catheter survival, and catheter outcome. Results: Early peritonitis episodes occurred in 8 of 21 patients (38.0%) in the open surgical group (OSG) versus 2 of 21 patients (9.5%) in the laparoscopic omental fixation group (LOFG) (p < 0.05); late peritonitis episodes occurred in 3 of 21 patients (14.2%) in the OSG versus 1 of 21 patients (4.7%) in the LOFG (p < 0.05). Early exit site infection occurred in 8 of 21 patients (38.0%) in the OSG versus 4 of 21 patients (19.0%) in the LOFG (p < 0.05), with many catheter-related problems in the conventional surgical group. There was no outflow obstruction in the LOFG. The conventional procedure was faster than the laparoscopic omental fixation technique. Analgesic requirements and hospital stay were less in the laparoscopic group. Laparoscopic surgery also enabled diagnosis of intraabdominal pathologies and treatment of the accompanying surgical problems during the same operation. Occult inguinal hernia was diagnosed in 2 patients, inguinal hernioplasty was performed in 4 patients, adhesiolysis was performed in 8 patients who had previous abdominal surgery, and liver biopsy was taken in 2 patients. Ovarian cystectomy was performed in another patient during laparoscopic CAPD catheter placement. Conclusion: The laparoscopic omental fixation technique (described by Öğünç and published in 1999) is a highly effective and successful method for preventing obstruction due to omental wrapping with a better catheter survival. Laparoscopic surgery also allows the diagnosis and treatment of the accompanying surgical pathologies during the same operation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Continuous ambulatory peritoneal dialysis (CAPD) is an effective therapy that has been widely used during the past 20 years in the management of patients with end-stage renal failure [19]. However, complications related to the peritoneal catheter, such as peritonitis, exit site infection, tunnel infection, pericatheter leakage, or mechanical dysfunction, and incorrect positioning of the catheter within the abdomen causing failure of fluid drainage remain troublesome [5, 8].
The ideal method of insertion of PD catheters remains debatable [11]. The most commonly used technique is an open surgical approach [18]. Less frequently, catheter insertions have been accomplished percutaneously by blind trocar or guidewire placement [5]. In recent years, laparoscopic surgery (LS) has found a wider use for peritoneal catheter placement with various techniques [1, 4, 9, 13]. Several authors have reported series of laparoscopic PD catheter placements with satisfactory success rates and acceptable morbidity [2, 5, 7, 9].
One of the most important aspects for success in CAPD is the presence of a functioning catheter, one that allows adequate drainage of dialysate solution [20]. A major and frustrating complication is mechanical outflow obstruction, which is reported to occur in up to 60% of patients [10]. PD catheter obstruction is frequently caused by omentum blocking the side holes of the catheter tubing [20]. The incidence of this complication has been reported to be 4–34.5% [5, 6]. The most common cause of catheter malfunction was omental wrapping in 183 of 578 (31.6%) patients receiving treatment for catheter placement with the open surgical technique in PD during a 12-year period [15]. To overcome this problem, Öğünç devised a laparoscopic technique consisting of omental fixation onto the parietal peritoneum during CAPD catheter placement [14]. The first results of 10 consecutive patients were published in 2001 [15]. Due to the satisfactory preliminary results of this technique, we routinely use this procedure, and this prospective study was peformed.
In this study, we carried out a prospective analysis of all CAPD catheters inserted by both open and laparoscopic surgical techniques and compared complication rates and catheter survival.
Materials and methods
Between March 1998 and October 2001, 42 double-cuff, curled-end CAPD catheters were placed in 42 patients. The outcomes of the 21 patients in whom the PD catheters were placed laparoscopically with omental fixation technique (Öğünç technique) were compared with those of 21 patients in whom the catheters were placed with open surgical technique. Recorded data included patient demographics, catheter implantation method, operating time, postoperative analgesic requirement, duration of hospitalization, early and late complications, catheter survival, and catheter outcome.
Local anesthesia was preferred for catheter placement in open surgical technique (conventional technique), although all patients were considered fit enough for general anesthetic.
The Curl Cath catheter with two felt cuffs (Sherwood Davis & Geck, Quinton, Canada) was used for all patients. All patients received 1 g of Cefazolin sodium intravenously prior to surgery as a prophylaxis. Catheters were implanted in the operating room by senior surgical residents under the supervision of one attending surgeon (G. Ögünç) in the conventional group. Under local anesthesia (1.0% lidocaine–HCl) and 0.5% bupivacaine–HCl mixed in equal volumes), a 5 or 6-cm vertical incision was made through the skin, the subcutaneous tissue, and the anterior rectus sheath. The rectus muscle fibers were dissected bluntly down to the posterior rectus sheath. A purse string suture (3–0 vicryl) was placed through the posterior rectus sheath, transversalis fascia, and the peritoneum. A 5-mm incision to the peritoneal cavity was made with a scalpel. The catheter was threaded on a stiffening stylet and introduced deeply into the true pelvis, and the purse string suture was closed snugly around the tube. The cuff was placed between the posterior rectus sheath and rectus fibers, and then the fascia was sewn tightly with 0 prolene sutures. The catheter was grasped with a hemostat and pulled through the exit site incision, which had been determined 1 day prior to surgery and depended on the size and shape of the abdomen and patient’s preference. The wound was closed with 4–0 silk sutures.
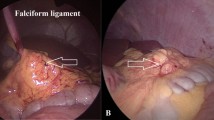
All patients in the laparoscopic omental fixation group (LOFG) were considered suitable for general anesthetic and gave informed consent. In 11 of 21 patients who had previous abdominal surgery, PD catheter was inserted laparoscopically. One day prior to surgery, the belt line of the patients was identified in the vertical position, with respect to pants and belt as usually worn. Depending on the size and shape of the abdomen, and taking into account the patient’s preference, the tunnel was marked with the aid of a stencil in such a way that the exit hole was created at least 2 cm above or below the belt line, as in the conventional group. In this way, the catheter would not be subjected to excessive motion with the patient’s activities, and there would not be pressure on the tunnel with the patient bending forward. Catheters were implanted by G. Öğünç under general endotracheal anesthesia in the laparoscopic group. A nasogastric tube was inserted. The surgeon stood on the right side of the patient. A subumbilical transverse incision 1 to 1.5 cm long was made through the skin, the subcutaneous tissue, and the anterior rectus sheath. The rectus muscle fibers were dissected bluntly down to the posterior rectus sheath. A 10-mm trocar with a grip was inserted and fixed; the grip is a cylindrical instrument that has applications in endoscopic surgery procedures for fixation of the trocar and can be used with the trocar to gain initial access to the abdominal cavity with an open cutdown technique instead of a Hasson trocar. A pneumoperitoneum was established via this trocar, inflating to a pressure of 10 mmHg. The initial exploratory laparoscopy was conducted with a 30° video laparoscope. Two 5-mm lateral rectus sheath ports were placed under direct vision, with one used for the exit site (Fig. 1). The operating table was tilted approximately 30° for a Trendelenburg position. Lateral inferior edges of the omentum were grasped and fixed onto the parietal peritoneum of the lateral abdominal wall at two points with a 3–0 prolene suture at the level of the umbilicus. If the omentum was large or bulky, another fixation suture was applied between the middle inferior edge of the omentum and the falciform ligament (Figs. 2 and 3). The catheter was threaded onto a stiffening stylet and introduced through the umbilical trocar deep into the true pelvis. The cuff was placed between the posterior rectus sheath and rectus fibers, and then the fascia was sewn tightly with 0 prolene sutures. The catheter was grasped with a hemostat and pulled through the 5-mm trocar site. The operation was completed by closing the other port sites with 4–0 silk sutures. Adhesiolysis was performed in 8 patients who had had previous abdominal surgery (Fig. 4) and liver biopsy was taken in 2 patients (Fig. 5); ovarian cystectomy was performed in another patient (Fig. 6) during laparoscopic CAPD catheter placement. Inguinal hernioplasties were performed by means of the transabdominal preperitoneal (TAPP) approach using prolene mesh graft with tacker fixation in 1 patient. A curved prostesis (3D max Mesh Bard Comp., U.S.A) was used by means of TAPP without fixation in 3 patients (Fig. 7). Bilateral hernioplasties were performed in 1 patient. Catheler patency was verified by a rapid in-and-out exchange before the patient was sent to the ward and observed in one of two groups. PD in the supine position was initiated using small volumes within 24 h after catheter implantation. The patient started CAPD 14 days postoperatively, in the open surgical group (OSG) and 7 days postoperatively in the laparoscopic omental fixation group (LOFG). Complications were classified as early (up to 4 weeks after the operation date) or late (more than 4 weeks postoperation).
Statistical analysis
The outcomes of the 21 patients in whom PD catheters were placed laparoscopically were compared with those of 21 patients in whom the catheters were placed with open surgical technique. Data were compared using the chi-square for nominal variables and the t-test for continuous variables. The Kaplan–Meier survival curves were compared by Breslow–Gehan–Wilcoxon test.
Results
Patient characteristics are summarized in Table 1. There were no statistically significant differences between the two study groups in patient gender and cause of end-stage renal disease; however, the LOFG patients were older and more obese. There was no requirement of conversion to the conventional method in the LOFG. The duration of the operation was significantly longer in the LOFG (p < 0.05) (Table 1). Lengthy surgery was necessitated for adhesiolysis (in eight patients who had had previous abdominal surgery) and for the treatment of intraabdominal surgical pathologies—inguinal hernioplasty (for patients, one of which had a bilateral inguinal hernia), liver biopsy (four patients), and ovarian cystectomy (one patient) in the LOFG. The duration of hospital stay was significantly longer in the OSG (p < 0.05) (Table 1). Postoperative pain was mild to moderate and controlled with oral and parenteral analgesics in the OSG. Parenteral analgesic requirement, was usually two to four doses after the procedure. Parenteral analgesics were not necessary in LOFG, except in one patient who received hernioplasty with prolene mesh graft using tacker fixation.
Catheter failure was defined as persistent peritonitis, exit site infection, persistent dialysate leak, and treatment failure requiring catheter removal.
The frequency and type of complications among the two study groups are shown in Table 2. Early peritonitis episodes occurred within 4 weeks of catheter placement in 2 of 21 patients (9.5%) in the LOFG versus 8 of 21 patients (38.1%) in the OSG (p < 0.05). Early exit site infection occurred in 4 of 21 patients (19.0%) in the LOFG versus 8 of 21 patients (38.%) in the OSG (p < 0.05). Early peritonitis in one of the two peritonitis episodes in the LOFG was associated with exit site infection in the early period. Early peritonitis in four of the eight peritonitis episodes in the OSG was associated with exit site infection in the early period. Early mechanical dysfunction occurred in 5 of 21 patients (23.8%) in the OSG. Peritoneal catheter obstruction due to omental wrapping was diagnosed in 4 patients by laparoscopy. An additional cause of obstruction was omental wrapping and fibrin clotting inside the catheter, which was diagnosed in 1 patient by laparoscopy. All who suffered mechanical dysfunction were rescued laparoscopically. There were no mechanical problems in the early and late periods in the LOFG. There was no pericatheter leakage in the early period in both groups. Late peritonitis episodes occurred in 1 of 21 patients (4.8%) in the LOFG versus 3 of 21 patients (14.3%) in the OSG (p < 0.05). A late peritonitis episode in the LOFG was associated with exit site infection in 1 patient. Late exit site infection occured in 1 of 21 patients (4.8%) in the LOFG versus 2 of 21 patients (9.5%) in the OSG. Only one (4.8%) pericatheter leakage occurred in the late period in the LOFG. There was no response spontaneously with delay in the start of PD. One (4.8%) tunnel infection occurred in the late period in the LOFG.
Dialysis effluent cultures resulted in Staphylococcus aureus (two patients in the LOFG and nine patients in the OSG), Streptococcus spp (one patient in the OSG), Proteus spp (one patient in the OSG), and no growth (one patient in the LOFG). Exit site infection cultures resulted in S. epidermidis (five patients in the LOFG and eight patients in the OSG) and S. aureus (one patient in each group).
Surgical revision was necessitated in 3 patients in the LOFG. Pericatheter dialysate leak occurred in 1 of 21 patients in the LOFG. The catheter was replaced because it did not interrupt CAPD. In 1 patient, the catheter was replaced due to chronic tunnel infection. In another patient in the LOFG, the cause was chronic exit site infection.
In eight patients (38%) in the OSG, additional surgery was required to remedy problematic catheters. Five patients who had mechanical outflow obstruction were rescued laparoscopically. In two patients, catheters were removed due to relapse or resistant peritonitis. In patient, in the OSG, the cause of revision was chronic exit site infection.
Thirty-two PD catheters (18 LOFG, 14 OSG) were in use at last follow-up, with the remainder having been removed because of successful transplantation (1 LOFG, 1 OSG), persistent dialysate leak (1 LOFG), exit site infection (1 LOFG), patient’s choice to stop PD (1 OSG), relapsing or resistant peritonitis (3 OSG), and treatment failure (2 OSG, resistant fluid overload).
Figure 8 depicts survival free of catheter failure among the two study groups. Laparoscopically placed catheters with omental fixation technique resulted in better survival (90.5% at 12 months and 38.1% at 24 months) than those placed with open surgical technique (71.4% at 12 months and 23.8% at 24 months), with p = 0.019 and 0.023, respectively.
Discussion
PD is widely used for the treatment of patients with end-stage renel failure. However, complications related to the PD catheter have diminished its success.
The ideal method for the insertion of CAPD catheters remains the subject of debate. The most commonly used technique is open surgical approach by minilaparotomy [3]. Others have used a “blind” approach or a peritoneoscopic technique and laparoscopic technique. Both early and late complications have limited catheter survival with incorrect positioning and surgical trauma, which may also expose the patient to tenderness around the incision, postoperative pain, and potential development of an incisional hernia as well as bad cosmesis in open surgical technique. Open surgery can also lead to adhesion formation and subsequent restrictions in fluid distribution in the peritoneal cavity [3, 16]. Advantages of this procedure are that can be easily performed under local anesthesia by surgical residents, shorter operation time, and simpler material requirements. Blind guidewire methods have not gained widespread acceptance because lack of direct visual implantation carries a high risk of visceral injury [12]. Laparoscopic implantation of CAPD catheters has expanded in recent years largely because of the introduction of the laparoscopic technique, which allows direct visualization of the peritoneal cavity and presumably leads to better positioning of the catheter [2, 5]. Some authors prefer adhesiolysis if it is indicated during laparoscopic catheter placement [9]. Other advantages of laparoscopic catheter placement procedures are immediate testing for overall peritoneal catheter function under direct vision, smaller wounds with less tissue disturbance, diminished postoperative pain, quick recovery to social and professional activities, early resumption of PD, short hospital stay, improved cosmesis with minor scarring, low infection rate, and better functional survival [2, 7]. Disadvantages include the need for general anesthetic, the long duration of the operative procedure, adverse physiologic effects of CO2 pneumoperitoneum, and the cost of equipment and instrumentation (the equipment was available in our hospital and we used reusable laparoscopic surgical instruments). Skilled surgeons and teams are also required for basic laparoscopic procedures such as cholecystectomy [6, 9]. Wright et al. [19] suggested that the laparoscopic insertion technique is not superior to the conventional method, but laparoscopic surgery was only used for catheter insertion in their randomized prospective study.
A major and frustrating complication is mechanical outflow obstruction in CAPD. Mechanical obstruction usually results from malplacement at operation, omental wrapping, catheter migration out of the pelvis, or adhesions. These problems may cause it to malfunction immediately or several months after insertion [6, 8]. Catheter outflow failure follows open surgical and blind guidewire/trocar methods in 4–34.5% of placement [5], whereas laparoscopic placement techniques are complicated by flow dysfunction in 4.5–13% of patients [8]. Unfortunately, outflow obstruction is found in up to 60% of patients in some series [17]. Up to 20% of patient transfers to hemodialysis (HD) are directly related to catheter problems [16]. When omental wrapping occurs, a partial omentectomy is usually performed to resolve catheter obstruction through a minilaparotomy. [16]. Therapeutic laparoscopic omental resection can be performed in peritoneal dialysis patients [6]. All these rescue procedures cause additional stress of surgery for patients and inhibit immediate use of the catheter because the abdominal incision must first heal. This requires a secondary means of dialysis (HD), which involves additional cost, inconvenience, and the risks associated with HD catheters. Also, prophylactic omental resection can be performed at the time of catheter insertion. This significantly improves the life of the catheter in peritoneal dialysis patients [16]. In Öğünç’s technique, which consists of omental fixation onto the parietal peritoneum during laparoscopic CAPD catheter placement, omental wrapping was prevented. LS was used for the treatment of accompanying surgical pathologies, such as adhesions due to previous abdominal surgeries and inguinal hernias. Ovarian cyst excision and liver biopsies were performed during the same operation in this prospective study.
In our study, postoperative pain was mild and controlled with oral analgesics in the LOFG, and LS was also provided early in the begining of the PD.
The laparoscopic procedure took longer to perform than the conventional procedure. More time was required for the treatment of accompanying surgical pathologies and omentopexy (approximately 10 min was required for omentopexy) during the CAPD catheter placement in the laparoscopic group.
We reported a lower incidence of early infection after laparoscopic catheter placement. The explanation for the disparity in the rate of early peritonitis is unclear, but this is most likely related to a considerably higher incidence of exit site infection in the open surgical group.
LS was well tolerated in this series, and neither obesity nor previous surgery was a contraindication for the technique. The early and late complication rates in this series compare favorably with those of published series of both open and laparoscopic insertion [11, 18, 19].
In summary, the laparoscopic technique lowered the incidence of early peritonitis and exit site infection and also provided significantly higher long-term catheter survival rates compared to the open surgical technique. The laparoscopic omental fixation technique completely prevented mechanical outflow obstruction due to omental wrapping. In addition, the laparoscopic approach allowed adhesiolysis, diagnosis, and treatment of accompanying surgical pathologies during the same operation.
References
SR Ash (1990) ArticleTitleChronic peritoneal dialysis catheters: effects of catheter design, materials, and location. Semin Dialr 3 39–46
C Beyerlein-Bucher FW Albert (1991) ArticleTitleEndoscopic peritoneal dialysis catheter placement. Contrib Nephrol 89 28–30 Occurrence Handle1832630
JR Bulmaster SF Miller RK Linley Jr LM Jones (1985) ArticleTitleSurgical aspects of the Tenckhoff peritoneal dialysis catheter: a 7 year experience. Am J Surg 149 339–342 Occurrence Handle3156518
Z Cala (2000) ArticleTitleTrocar for laparoscopic placement of peritoneal dialysis catheter. Surg Endosc 14 308–309 Occurrence Handle10.1007/s004640000046 Occurrence Handle1:STN:280:DC%2BD3c3gtlGjsg%3D%3D Occurrence Handle10741456
JH Crabtree A Fishman (1999) ArticleTitleVideolaparoscopic implantation of long-term peritoneal dialysis catheters. Surg Endosc 13 186–190 Occurrence Handle10.1007/s004649900936 Occurrence Handle1:STN:280:DyaK1M7hslCqsA%3D%3D Occurrence Handle9918628
JH Crabtree A Fishman (1999) ArticleTitleLaparoscopic omentectomy for peritoneal dialysis catheter flow obstruction: a case report and review of the literature. Surg Laparosc Endosc Percutan Tech 9 228–233 Occurrence Handle10.1097/00019509-199906000-00018 Occurrence Handle1:STN:280:DC%2BD3c3mtFWmtg%3D%3D Occurrence Handle10804009
C Cruz MD Faber (1991) ArticleTitlePeritoneoscopic implantation of catheters for peritoneal dialysis: effect on functional survival and incidence of tunnel infection. Contrib Nephrol 89 35–39 Occurrence Handle1:STN:280:By6A2s7osVE%3D
MAV Garcia MAG Urena F Carnero EF Ruiz CR Rodriguez PA Perez-de-Lastra (1997) ArticleTitleOmental entrapping of the peritoneal dialysis catheter solved by a laparoscopic approach. Perit Dial Int 17 194–195 Occurrence Handle9159842
M Giannattasio P De Maio R La Rosa A Balestrazzi (1996) ArticleTitleVideolaparoscopy: a new alternative for implantation of peritoneal catheters in ESRD patients with previous abdominal surgeries. Perit Dial Int 16 96–97 Occurrence Handle1:STN:280:BymB3cvmsFw%3D Occurrence Handle8616188
CR Hughes DM Angotti RA Jubelirer (1994) ArticleTitleLaparoscopic repositioning of a continuous ambulatory peritoneal dialysis (CAPD) catheter. Surg Endosc 8 1108–1109 Occurrence Handle1:STN:280:ByqD1cvjtVE%3D Occurrence Handle7992186
TL Hwang MF Chen CH Wu MO Leu CC Huang (1995) ArticleTitleComparison of four techniques of catheter insertion in patients undergoing continuous ambulatory peritoneal dialysis. Eur J Surg 161 401–404 Occurrence Handle1:STN:280:BymD3M3mt1c%3D
JM Messana GA Block RD Swartz (2001) ArticleTitleInjury to the inferior epigastric artery complicating percutaneous peritoneal dialysis catheter insertion. Perit Dial Int 21 313–315 Occurrence Handle1:STN:280:DC%2BD38%2FisFOgug%3D%3D Occurrence Handle11475349
PHA Nijhuis JF Smulders JJ Jakimowicz (1996) ArticleTitleLaparoscopic introduction of a continuous ambulatory peritoneal dialysis (CAPD) catheter by a two-puncture technique. Surg Endosc 10 676–679 Occurrence Handle1:STN:280:BymB2s%2FitlM%3D
G Öğünç (1999) ArticleTitleA new laparoscopic technique for CAPD catheter placement. Perit Dial Int 19 493–494 Occurrence Handle11379868
G Öğünç (2001) ArticleTitleVideolaparoscopy with omentopexy: a new technique to allow placement of a catheter for continuous ambulatory peritoneal dialysis. Surg Today 31 942–944 Occurrence Handle10.1007/s005950170042 Occurrence Handle11759897
G Öğünç (2002) ArticleTitleMalfunctioning peritoneal dialysis catheter and accompanying surgical pathology repaired by laparoscopic surgery. Perit Dial Int Occurrence Handle12227386
GH Poole P Tervit (2000) ArticleTitleLaparoscopic Tenckhoff catheter insertion: a prospective study of a new technique. Aust N Z J Surg 70 371–373 Occurrence Handle10.1046/j.1440-1622.2000.01830.x Occurrence Handle1:STN:280:DC%2BD3c3ovFCitw%3D%3D Occurrence Handle10830603
RJ Robinson SB Leapman GM Wetherington RJ Hamburger NS Fineberg RS Filo (1984) ArticleTitleSurgical considerations of continuous ambulatory peritoneal dialysis. Surgery 96 723–729 Occurrence Handle6385317
MJ Wright K Bel’eed BF Johnson DW Eadington L Sellars MJ Farr (1999) ArticleTitleRandomized prospective comparison of laparoscopic and open peritoneal dialysis catheter insertion. Perit Dial Int 19 372–375 Occurrence Handle1:STN:280:DyaK1MvjsFKktQ%3D%3D Occurrence Handle10507820
T Yılmazlar M Yavuz H Ceylan (2001) ArticleTitleLaparoscopic management of malfunctioning peritoneal dialysis catheters. Surg Endosc 15 820–822 Occurrence Handle11443441
Acknowledgements
We thank the patients and Necati Sağıroğlu, Elif Gönül, Kemal Demir, Meral Sağıroğlu, Dönüş Güç, and Zeliha Özcan for their help with this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Öğünç, G., Tuncer, M., Öğünç, D. et al. Laparoscopic omental fixation technique versus open surgical placement of peritoneal dialysis catheters . Surg Endosc 17, 1749–1755 (2003). https://doi.org/10.1007/s00464-002-8586-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-002-8586-3