Abstract
B-mode ultrasound is a safe noninvasive procedure that has been used to characterize aspects of the oropharyngeal swallow. The submental suprahyoid muscles are often investigated with ultrasound because of their contributions to hyolaryngeal elevation. There are several techniques for positioning the ultrasound transducer in the coronal plane, however, there is limited research on how reliability of measurement of the cross-sectional area (CSA) of the geniohyoid differs across transducer placement technique. This study examined three methods of transducer placement in the coronal plane by two examiners to determine the reliability of measurement of CSA of the geniohyoid muscle. Forty healthy adults participated in the study. Each participant’s geniohyoid muscles were imaged using B-mode ultrasound under three transducer placement conditions in the coronal plane by two examiners. Geniohyoid CSA was measured from each ultrasound image. A three-way mixed-methods ANOVA was used to determine whether there were significant differences in geniohyoid CSA among transducer position conditions, trials, and examiners. There were significant differences among the transducer placement conditions, indicating that each condition was measuring a different portion of the muscle. There were no significant differences among repeated trials nor between examiners within each method of transducer placement. All three conditions of transducer placement were reliable at measuring geniohyoid CSA across trials and examiners. This study emphasizes the need for consistency of placement, whichever method is selected. It also highlights the need for researchers to provide a precise description of methods for positioning the transducer so that placement is reproducible.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ultrasound has been used in both research and clinical settings to characterize various aspects of the oropharyngeal swallow [1,2,3,4,5,6]. Ultrasound is an imaging technique that uses high frequency sound waves and their echoes to create images of internal structures [7]. B-mode is a two-dimensional ultrasound image display composed of bright dots representing ultrasound echoes. The brightness of each dot is determined by the amplitude of the returned echo signal. These images allow for visualization and quantification of internal anatomy.
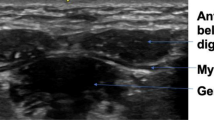
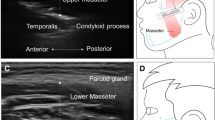
Many oropharyngeal structures have been imaged with B-mode ultrasound at rest and during swallowing. The tongue [8,9,10,11,12,13,14,15,16,17,18,19], masseter muscle [18, 20,21,22], hyoid [6, 23,24,25,26,27,28,29,30,31], pharynx [32], larynx [23, 26, 27, 30], and submental suprahyoid muscles [9, 12, 14, 17,18,19, 22, 25, 33,34,35,36,37,38,39,40,41,42,43,44,45,46] have been visualized with ultrasound in healthy children [47, 48] and adults [8, 10, 11, 13,14,15, 21,22,23,24,25,26,27, 29,30,31, 33, 36, 38,39,40, 42, 45, 46, 49] as well as in persons with neuromuscular disease or disorders [6, 12, 16, 17, 20, 23, 27, 44, 50], structural and functional differences after treatments to the head and neck [28, 32, 37, 51, 52], and aged individuals with sarcopenia [9, 18, 19, 26]. The submental suprahyoid muscles, specifically the anterior belly of the digastric [12, 14, 18, 38, 40, 43], the mylohyoid [12, 18, 38, 40], and geniohyoid muscles [9, 12, 14, 18, 22, 33,34,35,36,37, 39, 41, 42, 45, 46, 53], are often investigated because of their contributions to hyolaryngeal elevation and the potential for their dysfunction to predict dysphagia.
Positioning of the ultrasound transducer varies across studies depending upon the structures of interest. Measures of hyoid excursion and thyrohyoid approximation are typically imaged with the transducer in the sagittal plane [23, 25, 28,29,30,31]. The oral tongue, tongue base and submental suprahyoid muscles have been visualized with the ultrasound transducer oriented in both the sagittal [9, 18, 33,34,35, 39, 42] and coronal planes [9, 12, 14,15,16,17,18,19, 22, 25, 37, 38, 40, 41, 43,44,45,46].
To image the submental suprahyoid muscles in the sagittal plane, investigators typically use a convex transducer probe positioned midsagittally, keeping the acoustic shadows of the mental symphysis and hyoid bone in the field of vision [33,34,35, 39, 42]; a linear transducer may also be used [9].
When using the transducer in the coronal plane to image the submental suprahyoid muscles, investigators have utilized a number of methods for placement of a linear transducer probe. Common placements include positioning the probe perpendicular to the floor of mouth at one third the distance between the mandibular or mental symphysis and the parotid gland [9, 14, 22, 41, 43, 44], one third the distance between the mandibular symphysis and the hyoid bone [18, 19, 46, 53, 54], or one half the distance between the mandibular symphysis and the hyoid bone [12, 15, 16, 25, 40, 45]. Others have taken a more posterior view, placing the transducer probe close to the hyoid bone [33, 37]. Watkin et al. (2001) [55] used a scanning procedure consisting of a 10 s sweep in the coronal plane beginning at the mandibular symphysis and continuing to the hyoid bone. The midpoint of the geniohyoid muscle was used for analysis and determined as the middle frame within the total sweep sequence. Some researchers have forgone precision of placement in order to identify the optimal image for quantitative analysis [38, 56, 57].
Because ultrasound does not use ionizing radiation, it is a safe noninvasive procedure that may be used repeatedly to document changes in oropharyngeal musculature. Morphologic changes to the submental suprahyoid muscles have been monitored over time in response to interventions such as swallowing exercises, strengthening protocols, and aggressive nutritional management [12, 38, 40, 42, 44, 45]. Given the serial nature of longitudinal assessment, it is important that transducer placement be reliable and consistent across study evaluations when used to document changes to the muscle over time.
Many researchers who used ultrasound for various swallow-related investigations provided information concerning inter- or intra-rater reliability on a subset of their data in their publications [10, 14, 15, 17, 22, 28, 29, 31, 37, 41, 45, 49, 55]. Such ratings are important to establish the reliability of the investigators in the execution of their protocols. However, determining reliability was not the focus of their work; rather the impact of their intervention or the conditions of the oropharyngeal swallow they investigated were the outcomes of interest. There is a body of research that focuses specifically on assessing the reliability of ultrasound; much of this work has primarily assessed hyoid displacement and thyrohyoid approximation with the transducer in the sagittal plane. Macrae, Doeltgen and Huckabee (2012) [24] assessed the inter and intrarater reliability of three examiners in their assessment of hyoid bone rest and maximal displacement in healthy participants. Their intraclass correlation coefficient (ICC) was high for inter-rater agreement at 0.86 for rest measures and 0.86 for maximal displacement. Intra-rater reliability was higher at 0.95 for rest and 0.98 for maximal displacement. In their study of reliability of measuring hyoid bone displacement during swallowing in persons with dysphagia, Chen, Hsiao, Wang Fu, and Wang (2017) [58] determined the interrater ICC between two examiners as 0.892; the intrarater ICC of the two examiners was 0.996 and 0.959. Winiker and colleagues (2021, 2022) [56, 57] assessed the reliability of a pocket-sized ultrasound system in the assessment of swallowing in healthy subjects and persons with dysphagia. They found poor inter- and intrarater reliability (ICC = 0.34 and ICC = 0.38 respectively) with the pocket-sized system for real-time online assessment of hyoid displacement in healthy subjects; interrater reliability was better for those with dysphagia (ICC = 0.55) and increased when offline measurement of hyoid displacement was performed (interrater ICC = 0.83; intrarater ICC = 0.83). Andrade et al. (2022) [59] performed a systematic review and meta-analysis of reliability in ultrasound measurement of hyoid displacement. They calculated an interrater reliability of 0.858 and intrarater reliability of 0.968; there was also significant heterogeneity for intrarater reliability.
Reliability of measurement of thyrohyoid approximation in the sagittal plane has also been examined in the literature. Winiker and colleagues (2021, 2022) [56, 57] calculated poor to moderate inter- and intrarater reliability (ICC = 0.32 and ICC = 0.38 respectively) for a pocket-sized ultrasound system for online assessment of thyrohyoid approximation in healthy subjects and moderate interrater reliability (ICC = 0.56) for those with dysphagia. Reliability increased with secondary offline measurement of thyrohyoid approximation in persons with dysphagia (interrater ICC = 0.83; intrarater ICC = 0.83). Huang, Hsieh, Chang, Chen, and Wang (2009) [23] evaluated the reliability of ultrasonographic examination of thyrohyoid approximation in healthy persons and patients post-stroke with or without dysphagia. Intrarater ICC values from two sonographers were 0.974 and 0.989, respectively. Their interrater ICC value was 0.983.
Few studies have assessed the reliability of measurement of oropharyngeal structures in the coronal plane. In their reliability assessment of a pocket-sized ultrasound unit, Winiker and colleagues (2021, 2022) [56, 57] measured cross-sectional area (CSA) of the submental suprahyoid muscles at rest in the coronal plane, positioning the scanner until the largest and clearest boundaries for the left and the right anterior belly of the digastric muscles and the geniohyoid muscles were visualized. Real-time online interrater reliability was moderate to good for measurement of the geniohyoid muscle CSA in healthy subjects (ICC = 0.49) and persons with dysphagia (ICC = 0.60). Online intrarater reliability was good for healthy subjects (ICC = 0.71). Reliability improved greatly for persons with dysphagia when their images were analyzed off-line (interrater ICC = 0.99; intrarater ICC = 0.98). Perry, Winkelman and Huckabee [25] (2016) compared variability in measurement of the submental suprahyoid muscles at rest using hand-held and fixed positioning of the ultrasound transducer in the coronal plane approximately halfway between the mental symphysis and the hyoid bone in healthy adults. Multiple trials were collected with both techniques across three testing sessions. For test–retest reliability, there were no significant main effects of trial or session, and there was no difference in CSA of the geniohyoid muscle across transducer placement techniques. However, they found significant differences in across-session variability, with larger measurements in the third (final) session when the fixed transducer was used.
Overall, the reliability of ultrasound for measurement of oropharyngeal swallow structures and events appears good to excellent; however, there is less evidence of reliability of measurement of submental suprahyoid muscles in the coronal plane. Given the number of options for placement of the ultrasound transducer probe in the coronal plane, and the need for consistency of placement of the transducer across trials and evaluation sessions when using ultrasound to document change of submental suprahyoid muscles in response to swallowing interventions, further assessment of reliability is warranted. The purpose of this study, therefore, is to examine three conditions of transducer probe placement in the coronal plane by two examiners over multiple trials to determine the reliability of measurement of CSA of the geniohyoid muscle. It is hypothesized that the examiners will not differ significantly in their measures of CSA of the geniohyoid muscle across multiple trials and within probe placement conditions, but that CSA of the geniohyoid muscle will differ depending upon the transducer probe placement condition.
Methods and Materials
This study was undertaken with the understanding and written consent of each subject according to the ethical principles of the World Medical Association Declaration of Helsinki (version 2002) and approved by the Institutional Review Board of the University of Wisconsin Milwaukee. It was an experimental mixed group design investigating three methods of transducer probe placement in the coronal plane and their impact on measures of the geniohyoid muscle with B-mode ultrasound in forty healthy adults. The design included three factors with two within-subjects factors (probe placement condition and trial) and one between-subjects factor (examiner). All training in the study protocol and measurement of the outcome measures was performed in the Swallow Physiology Laboratory on the Kenwood Campus of the University of Wisconsin Milwaukee.
Participants
Forty (40) healthy adults (29 women, 11 men) aged 20 to 59 were recruited for this study through flyers displayed in private and public spaces at the University of Wisconsin Milwaukee and surrounding community. Participants considered themselves in general good health and were not experiencing symptoms of upper respiratory infection during their involvement in the study. None had been treated for cancer of the head and neck or had current or a history of neurologic disease or stroke. No participant had surgery to the mouth, throat, or neck other than tooth extractions.
Data Collection Procedures
B-Mode Ultrasound
Ultrasound images of the submental suprahyoid musculature were recorded in the coronal plane. Each participant’s submental suprahyoid musculature was imaged using B-mode ultrasound with three transducer placement conditions in the coronal plane by two examiners. The order of transducer placement condition and examiner were randomized to avoid an order effect of either condition or examiner. Three trials were recorded under each of the three transducer placement conditions followed by a 15-min rest period. After the rest period, the subject was again recorded with each of the methods in a randomized order by the second examiner. As a result, subjects provided a total of 18 samples from which measurements of the geniohyoid were made.
Participants were seated in a comfortable upright position with their head in a relaxed neutral head posture, and asked to keep the tongue on the floor of the mouth in a natural rest position. The following transducer placement conditions in the coronal plane were used for each subject:
-
1.
Condition 1: Probe placed at the measured half-way distance between mental symphysis and hyoid bone [12, 15, 16, 25, 40, 45] (Fig. 1): Each examiner independently palpated the position of the hyoid bone at rest and measured the total distance from the hyoid bone to the mental symphysis in mm. This distance was divided in half, and a mark corresponding to that distance was made with a black non-toxic removable pen on the participant’s skin to aid in repeatable transducer placement across the three trials for the condition.
This condition was selected as a compromise among methods that position the probe perpendicular to the floor of mouth at a proportion of total distance between the mandibular/mental symphysis and the hyoid bone.
-
2.
Condition 2: Probe placed 2 cm anterior to the hyoid bone [adapted from 33, 37]: Each examiner independently palpated the position of the hyoid bone at rest and made a mark 2 cm anterior to the hyoid bone using a red non-toxic removable pen on the participant’s skin to aid in repeatable transducer placement across the three trials for the condition.
This condition was selected to assess the geniohyoid in a more posterior position while defining a specific place to set the transducer, that is 2 cm anterior to the hyoid bone, to enhance reliability of repeated placement.
-
3.
Condition 3: Probe sweep anterior to posterior from mental symphysis to hyoid bone [55]: The transducer probe was placed at the mental symphysis in the coronal plane until the bright hyperechoic rim of the bone was imaged (Fig. 2a). The examiner then swept the transducer posteriorly toward the hyoid bone at a constant rate for approximately 10 s following the beat of a metronome until the acoustic shadow of the hyoid bone was imaged (Fig. 2b).
This condition was selected because it was a novel scan technique in the ultrasound and swallowing literature; it was of interest to see whether the researchers could be reliable in using this technique.
The markings identifying the locations for Conditions 1 and 2 were removed after scanning by the first examiner. After the 15-min rest period, the second examiner independently reassessed the appropriate position for Conditions 1 and 2 and continued with their scanning.
Pressure on the skin was avoided by the use of a generous amount of contact gel applied to the transducer head and the participant’s skin. Ultrasound data were acquired with the Mindray Z6 Ultrasound System ultrasound machine ((Shenzhen Mindray Biomedical Electronics Co., LTD., Shenzhen, China) using a 40 mm linear transducer with a range of 6 to 14 MHz. Imaging began with the unit’s default settings for musculoskeletal examination, which were frequency of 8.5 MHz, depth of 3.7 cm, and gain of 50 dB. Settings were then selected to optimize the image for each participant. Frequency was maintained at 8.5 MHz for all participants except one; depth varied between 2.8 cm and 4.6 cm, with the majority of participants imaged at 3.7 cm. Gain was manipulated most often, ranging from 39 to 60 dB, with most participants remaining at the default gain setting of 50 dB. All data were recorded using the features of the Mindray Z6 machine and exported for off-line analysis.
Ultrasound Data Reduction Procedures
Still frames containing the B-mode images for Conditions 1 and 2 were saved as bit-mapped images (BMP file format) and sweep videos from Condition 3 were saved in AVI format. AVS Video Converter 9.1 (Online Media Technologies, Ltd., UK) was used to select the frame halfway between the hyperechoic rim of the mental symphysis and the first appearance of the acoustic shadow cast by the hyoid bone. This frame was saved as a BMP still image. Still frames from each participant’s evaluations were stored for analysis on a Dell PC (OptiPlex 7440).
The stored BMP files were analyzed with ImageJ v.1.51w, a public domain Java image processing program (https://imagej.net/ij/index.html). Cross-sectional area (CSA) of the geniohyoid muscles was measured on each ultrasound image. Cross-sectional area was chosen as the dependent variable because previous work assessing reliability of oropharyngeal structures in the coronal plane [25, 56, 57] used muscle CSA. In addition, the investigators intended to apply the procedures used in this study to future work in which change in muscle morphology will be monitored in response to oropharyngeal exercises that target the submental suprahyoid muscles. Since it is not known in what dimensions such exercises will change muscle morphology, for example, muscle thickness, muscle breadth, or both, cross-sectional area is a suitable metric as it captures morphologic change in all dimensions.
The bilateral geniohyoid muscles were measured as a single muscular unit due to lack of distinction between the left and right muscles. The scale of each image was set by ImageJ using the depth indicator in cm on the ultrasound image. The margins of the geniohyoid were identified by the brighter hyperechoic reflection of the fascia surrounding the muscle. The circumference of the geniohyoid was then outlined within the fascia using the freehand drawing tool in ImageJ, and the area of each region was calculated in cm2. Figure 3 provides an example image with the bilateral geniohyoid outlined.
Each examiner measured geniohyoid CSA on all images acquired during their assessments. In addition, inter- and intrajudge reliability were assessed using intraclass correlation for 10% of the images chosen at random. The ICC for interjudge reliability was 0.97 and for intrajudge reliability was 0.98.
Statistical Analysis
Means and standard deviations for CSA of the geniohyoid muscle were reported for each condition by examiner. Inferential statistics included a mixed-methods Three-Way ANOVA for two within-subjects factors (condition and trial) and one between-subjects factor (examiner) using the General Linear Model (GLM) in SPSS (SPSS Statistical software version 28.0, IBM, Armonk, NY) to determine whether there were significant changes in geniohyoid CSA as a function of examiner, transducer placement condition, and trial. In the event of a significant ANOVA, potential three-way and two-way interactions were to be interpreted first, followed by the main effects of trial, examiner, and transducer placement condition. Apriori paired comparisons between examiners or placement conditions using the Bonferroni adjustment were planned to determine whether geniohyoid muscle CSA differed as a result of these factors.
Results
Forty healthy adults participated in this study that investigated the use of B-mode ultrasound to measure CSA of the geniohyoid muscle under three transducer placement conditions by two examiners. Facial hair was not an exclusion criterion for this study; two men were enrolled in the study who had closely trimmed facial hair in the submental area. There were no issues with image acquisition for these participants. One subject could not be recorded under Condition 2 by either examiner because the short length between her mental symphysis and hyoid bone yielded no difference in the probe position for Conditions 1 and 2. Therefore, of 720 possible samples (40 subjects by two examiners by three transducer placement conditions by three trials per condition), 714 ultrasound images were available for analysis.
Means and standard deviations for geniohyoid muscle CSA are summarized by transducer placement condition and examiner in Table 1. All three trials were used in calculating the mean.
To determine whether geniohyoid muscle CSA differed significantly as a result of transducer placement condition, trial, or examiner, a mixed-methods Three-Way ANOVA was performed using the General Linear Model procedure in SPSS v.28.0. There were no significant three-way (condition by trial by examiner) or two-way (condition by trial, condition by examiner, trial by examiner) interactions; therefore, the main effects were interpreted independently.
The main effect of examiner was not significant (F(1,76) = 0.013, p = 0.908, η2 = 0.000), indicating that the two examiners did not differ in their measurement of geniohyoid muscle CSA. The main effect of trial also was not significant (Wilks’ Lambda = 0.993, F(2,75) = 0.258, p = 0.773, η2 = 0.007), indicating that measurement of geniohyoid muscle CSA did not differ across repeated trials.
The main effect of transducer placement condition was significant (Wilks’ Lambda = 0.328, F(2,75) = 76.753, p = 0.000, η2 = 0.672), indicating that geniohyoid muscle CSA differed significantly depending upon placement of the transducer. Mean and standard deviation of geniohyoid muscle CSA by transducer placement condition, pooled across trial and examiner, are summarized in Table 2. Pairwise comparisons using the paired t-test with Bonferroni adjustment revealed significant differences in mean CSA among all three transducer placements. Table 3 presents the mean difference, standard error of the difference and significance level after Bonferroni adjustment for each of the paired comparisons.
Discussion
A major benefit of using ultrasound to assess parameters of the oropharyngeal swallow is that it is noninvasive and can be used repeatedly without exposing the participant to the risks or discomfort associated with other imaging procedures such as videofluoroscopy or flexible endoscopy. Ultrasound has been used to measure changes in the submental suprahyoid muscles in response to strengthening or progressive resistance protocols [12, 38, 40, 42, 45]. Given the options for positioning the ultrasound transducer in the coronal plane reported in the literature, for example one third the distance between the mental symphysis and parotid gland [9, 14, 22, 41, 43, 44], one half the distance between the mental symphysis and the hyoid bone [12, 15, 16, 25, 40, 45], or positioning until the best image is available [38, 56, 57], it is essential that transducer placement be consistent and reliable when documenting change in submental suprahyoid muscle morphology over time. The purpose of this study was to examine three conditions of transducer probe placement in the coronal plane by two examiners over multiple trials to determine the reliability of measurement of CSA of the geniohyoid muscle.
There were no significant differences among the three repeated trials nor between examiners within each method of ultrasound transducer placement. These results indicate that examiners could independently and reliably place the transducer in the same place repeatedly over three trials in each of the three transducer placement conditions.
There were significant differences among the transducer placement conditions, indicating that different sections of the geniohyoid were being imaged depending upon transducer location. In reviewing geniohyoid mean CSA in Table 2, the geniohyoid CSA becomes larger as the muscle progresses posteriorly from the mental symphysis to the hyoid bone, increasing from 1.27 cm2 to 1.80 cm2. It also appears that the midpoint of the 10 s transducer sweep on average fell as a point along the geniohyoid between one half the distance of the mental symphysis and 2 cm before the hyoid bone, rather than at the measured halfway point. Regardless of transducer probe position technique, all three conditions of transducer placement were reliable at measuring CSA of the geniohyoid muscle across trials and examiners.
The results of this study are similar to those of Perry et al. (2016) [25], who found no significant main effects of trial or session, and no difference in CSA of the geniohyoid muscle between hand-held and fixed transducer positioning in their comparative study in healthy adults. It is likely that they found no differences in transducer positioning condition since the transducer was being held in the same position halfway between the mental symphysis and the hyoid bone in each condition whether it was hand-held or fixed in place.
The significant differences in geniohyoid CSA depending upon position of the transducer probe observed in this study emphasize the vital need for consistency of probe placement, whatever method is selected, especially when working longitudinally to document change in muscle morphology in the coronal plane. Researchers may incorrectly attribute significant differences observed longitudinally in geniohyoid CSA to an intervention or change in disease status when these could actually be an artifact of inconsistent placement of the transducer probe across evaluations. Study results also highlight the need for researchers and clinicians to provide a precise description of methods for positioning the transducer so that placement is reproducible across assessments and examiners. Researchers must be careful to establish techniques for consistent placement of the transducer probe and specify these procedures in their protocols in order to support replication of their work.
The use of headsets and other devices to fix ultrasound transducers in place have been reported in the literature for a number of years, with the goal to achieve greater reliability and consistency of transducer placement [25, 60,61,62]. Perry et al. (2016) [25] used a transducer stabilizer fixed to a bite block in their comparative study. For geniohyoid CSA, although there were no significant differences between the fixed and hand-held conditions, they found differences in across-session variability, with larger measurements in the third (final) session when the fixed transducer was used. The authors reported that their participants experienced more discomfort with the transducer stabilizer, and may have made postural adjustments to accommodate for the discomfort that could have affected submental suprahyoid muscle contraction. Additional research focusing on reliability of measurement across trials, examiners, and evaluation points is needed to determine the benefits of headsets or other devices to hold the ultrasound transducer in a fixed position.
As with most areas of dysphagia, there is considerable interest in translating procedures from the lab to the clinic. In order to translate the use of ultrasound into clinical practice, reliability and validity testing as well as development of normative data are essential [1]. Winiker and colleagues tested the reliability and validity of a pocket-sized ultrasound unit intended for use in clinical practice in a series of studies [30, 56, 57]. They concluded that the device they tested was not yet sufficient for online data acquisition in the clinical environment, in particular because of poor interrater reliability. Indeed, a recent consensus study initiated by the International Ultrasound (US) Working Group in 2020 [63] identified and prioritized fifteen items necessary to translate the use of ultrasound into speech-language pathology practice for the purpose of laryngeal and swallowing assessment. The highest ranked priority related to the theme of reliability, including test–retest reliability and inter- and intrarater reliability. The current study contributes to the call for additional literature establishing the reliability of ultrasound to assess and document the oropharyngeal swallow.
Videofluoroscopy and endoscopy are the gold standards for assessing the oropharyngeal swallow, however not all clinicians or researchers have access to these imaging techniques. Ultrasound may become another tool in the dysphagia toolbox if it proves valid and reliable. Research such as documented in the current study is one step in moving toward the practical aspects of ultrasound by establishing that investigators are highly reliable in imaging the submental suprahyoid musculature. In addition, ultrasound may fill needs in the dysphagia toolbox that may not be met by fluoroscopy or endoscopy. Fluoroscopy uses ionizing radiation to produce its image, therefore limiting its use as a tool for repeated documentation of swallowing function. Endoscopy uses an endoscope passed through the nares which causes discomfort in many subjects. There are a number of interventions or exercises available for treating dysphagia; however, considerable research is needed to determine optimal frequency, timing and type of exercises. Ultrasound can be used to document changes in muscle mass on a weekly basis or even more often because it is noninvasive and can be used repeatedly without exposing the participant to the risks or discomfort associated with other imaging procedures. It may be used to monitor changes in muscle morphology and help guide the clinician as to when videofluoroscopy or endoscopy should be recommended to examine potential changes in oropharyngeal swallowing function in response to exercises. Ultrasound therefore is a tool that can supplement the imaging gold standards of fluoroscopy and endoscopy.
Although the results of this study provide important information on the reliability of ultrasound with the transducer in the coronal plane, there are some limitations. The participants in this study were in good general health and aged 20 through 59. Although this cohort provides normative data for persons under the age of 60, most clients with dysphagia tend to be older [64]. Normative data need to be collected in an older population of persons in good health in order to provide needed comparative data.
Another limitation is that the extent of training for the researchers was not well documented. The investigators began their work in this area organically, discovering informally what structures could be visualized and how changing transducer probe orientation, angle and position influenced the ultrasound image. The researchers consulted with experienced colleagues with questions concerning scanning technique and determining optimal settings as well as options for measuring images online and offline. The International US Working Group ranked training protocols and competencies as the fifth highest priority [63], so the training of future researchers in our group will be documented more carefully.
This study is an important initial step in the process of establishing ultrasound as a research and ultimately a clinical tool in the documentation and assessment of the oropharyngeal swallow in patient populations. The results of this study suggest several areas for future research. As mentioned previously, this study should be replicated with an older cohort of generally healthy persons in order to establish the reliability of imaging the geniohyoid with ultrasound in the coronal plane as well as to contribute normative data against which older persons with dysphagia may be compared. It will also be important to determine whether the submental suprahyoid muscles can be imaged reliably with ultrasound in persons with tissue changes such as those that occur with spinal muscle atrophy [17], Duchenne muscular dystrophy [65], or radiation-induced damage after radiotherapy for cancer of the head and neck [66]. It is likely these tissue changes will affect the morphology of the submental suprahyoid muscles; therefore, it is necessary to establish the reliability of imaging these muscles and those of other populations with tissue changes with ultrasound in the coronal plane.
The authors intend to continue their research as proposed in the Discussion; this study is an essential step in establishing the reliability of investigators in using ultrasound to image the submental suprahyoid muscles.
Summary and Conclusions
The reliability of B-mode ultrasound for measuring cross-sectional area of the geniohyoid muscle in the coronal plane was assessed by two examiners using three methods of transducer probe placement. There were no significant differences among repeated trials nor between examiners within each method of ultrasound transducer placement, indicating that examiners can independently and reliably place the transducer in the same place repeatedly over multiple trials in each transducer placement condition. There were significant differences among the transducer placement conditions, indicating that each condition was measuring a different portion of the geniohyoid muscle. Regardless of position technique however, all three conditions of transducer placement were reliable at measuring cross-sectional area of the geniohyoid muscle across trials and examiners. This study emphasizes the need for consistency of placement, whatever method is selected, across evaluation points when ultrasound is being used to document change in muscle morphology in the coronal plane over time. It also highlights the need for researchers to provide a precise description of methods for positioning the transducer so that placement is reproducible. This study contributes to the call for additional literature establishing the reliability of ultrasound to assess and document the oropharyngeal swallow.
Data Availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Allen JE, Clunie GM, Winiker K. Ultrasound: an emerging modality for the dysphagia assessment toolkit? Curr Opin Otolaryngol Head Neck Surg. 2021;29(3):213–8. https://doi.org/10.1097/MOO.0000000000000708.
Hsiao MY, Wu CH, Wang TG. Emerging role of ultrasound in dysphagia assessment and intervention: a narrative review. Front Rehabilit Sci. 2021;2: 708102. https://doi.org/10.3389/fresc.2021.708102.
Miura Y, Tamai N, Kitamura A, Yoshida M, Takahashi T, Mugita Y, Tobita I, Arita M, Urai T, Dai M, Noguchi H, Matsumoto M, Mukai K, Nakagami G, Ota E, Sugama J, Sanada H. Diagnostic accuracy of ultrasound examination in detecting aspiration and pharyngeal residue in patients with dysphagia: a systematic review and meta-analysis. Japan J Nurs Sci. 2021;18(2): e12396. https://doi.org/10.1111/jjns.12396.
Magalhães DDD, Bandeira JF, Pernambuco L. Quantitative approach to analyze hyoid bone movement during swallowing by ultrasound: an integrative review. Abordagem quantitativa por ultrassonografia para análise do movimento do osso hioide durante a deglutição: revisão integrativa. CoDAS. 2023;35(4):e20220002. https://doi.org/10.1590/2317-1782/20232022002pt.
Maeda K, Nagasaka M, Nagano A, Nagami S, Hashimoto K, Kamiya M, Masuda Y, Ozaki K, Kawamura K. Ultrasonography for eating and swallowing assessment: a narrative review of integrated insights for noninvasive clinical practice. Nutrients. 2023;15(16):3560. https://doi.org/10.3390/nu15163560.
Potente P, Buoite Stella A, Vidotto M, Passerini M, Furlanis G, Naccarato M, Manganotti P. Application of ultrasonography in neurogenic dysphagia: a systematic review. Dysphagia. 2023;38(1):65–75. https://doi.org/10.1007/s00455-022-10459-9.
McKinnis LN. Fundamentals of musculoskeletal imaging. 4th ed. Philadelphia: F.A. Davis Company; 2014.
Li C, Li J, Zhang C, Cao X, Li N, Song D, Yu T. Application of B+M-mode ultrasonography in assessing deglutitive tongue movements in healthy adults. Med Sci Monit. 2015;21:1648–55. https://doi.org/10.12659/MSM.893591.
Ogawa N, Mori T, Fujishima I, Wakabayashi H, Itoda M, Kunieda K, Shigematsu T, Nishioka S, Tohara H, Yamada M, Ogawa S. Ultrasonography to measure swallowing muscle mass and quality in older patients with sarcopenic dysphagia. J Am Med Dir Assoc. 2018;19(6):516–22. https://doi.org/10.1016/j.jamda.2017.11.007.
Chantaramanee A, Tohara H, Nakagawa K, Hara K, Nakane A, Yamaguchi K, Yoshimi K, Junichi F, Minakuchi S. Association between echo intensity of the tongue and its thickness and function in elderly subjects. J Oral Rehabil. 2019;46(7):634–9. https://doi.org/10.1111/joor.12788.
Ohkubo M, Scobbie JM. Tongue shape dynamics in swallowing using sagittal ultrasound. Dysphagia. 2019;34(1):112–8. https://doi.org/10.1007/s00455-018-9921-8.
Jung YJ, Kim HJ, Choi JB, Park JS, Hwang NK. Effect of dysphagia rehabilitation using kinesiology taping on oropharyngeal muscle hypertrophy in post-stroke patients: a double blind randomized placebo-controlled trial. Healthcare (Basel, Switzerland). 2020;8(4):411. https://doi.org/10.3390/healthcare8040411.
Nienstedt JC, Müller F, Rösler A, Pflug C. Presbyphagia diagnostics using M-mode ultrasound: changes in the tongue movement pattern. Dysphagia. 2020;35(4):696–701. https://doi.org/10.1007/s00455-019-10076-z.
Yamaguchi K, Hara K, Nakagawa K, Yoshimi K, Ariya C, Nakane A, Furuya J, Tohara H. Ultrasonography shows age-related changes and related factors in the tongue and suprahyoid muscles. J Am Med Dir Assoc. 2021;22(4):766–72. https://doi.org/10.1016/j.jamda.2020.10.012.
Yamaguchi K, Nakagawa K, Yoshimi K, Ariya C, Nakane A, Okumura T, Tohara H. The cross-sectional area of the middle and base of the tongue is associated with swallowing-related muscle strength. Dysphagia. 2022;37(6):1723–31. https://doi.org/10.1007/s00455-022-10431-7.
Recasens BB, Guillen-Sola A, Llorens JMM, Corberó AB, Moreno MV, Claramunt AA, Escobar GG, Rubio MA. Ultrasonographic and manometric study of the tongue as biomarkers of dysphagia in patients with amyotrophic lateral sclerosis. Neurol Sci. 2023;44(3):931–9. https://doi.org/10.1007/s10072-022-06486-x.
van der Heul AMB, Nievelstein RAJ, van Eijk RPA, Asselman F, Erasmus CE, Cuppen I, Bittermann AJN, Gerrits E, van der Pol WL, van den Engel-Hoek L. Swallowing problems in spinal muscular atrophy types 2 and 3: a clinical, videofluoroscopic and ultrasound study. J Neuromuscul Dis. 2023;10(3):427–38. https://doi.org/10.3233/JND-221640.
Umay E, Akaltun MS, Uz C. Association between swallowing muscle mass and dysphagia in older adults: a case-control study. J Oral Rehabil. 2023;50(6):429–39. https://doi.org/10.1111/joor.13439.
Yamaguchi K, Nakagawa K, Yoshimi K, Ariya C, Nakane A, Ishii M, Hasegawa S, Tohara H. Associations of swallowing-related muscle quantity and quality with sarcopenic parameters. Eur Geriatr Med. 2023;14(1):195–201. https://doi.org/10.1007/s41999-023-00747-4.
Van Den Engel-Hoek L, Lagarde M, Van Alfen N. Ultrasound of oral and masticatory muscles: why every neuromuscular swallow team should have an ultrasound machine. Clin Anat. 2017;30(2):183–93. https://doi.org/10.1002/ca.22818.
Park JS, Jung YJ, Kim MJ. Effects of neuromuscular electrical stimulation synchronized with chewing exercises on bite force and masseter muscle thickness in community-dwelling older adults in South Korea: a randomized controlled trial. Int J Environ Res Public Health. 2020;17(13):4902. https://doi.org/10.3390/ijerph17134902.
Yamaguchi K, Tohara H, Hara K, Chantaramanee A, Nakagawa K, Yoshimi K, Nakane A, Minakuchi S. Tongue thickness is associated with masticatory performance of perioral muscles: ultrasonographic study of perioral muscle characteristics in healthy young subjects. J Oral Rehabil. 2020;47(3):325–31. https://doi.org/10.1111/joor.12909.
Huang YL, Hsieh SF, Chang YC, Chen HC, Wang TG. Ultrasonographic evaluation of hyoid-larynx approximation in dysphagic stroke patients. Ultrasound Med Biol. 2009;35(7):1103–8. https://doi.org/10.1016/j.ultrasmedbio.2009.02.006.
Macrae PR, Doeltgen SH, Jones RD, Huckabee ML. Intra- and inter-rater reliability for analysis of hyoid displacement measured with sonography. J Clin Ultrasound. 2012;40(2):74–8. https://doi.org/10.1002/jcu.20874.
Perry SE, Winkelman CJ, Huckabee ML. Variability in ultrasound measurement of hyoid bone displacement and submental muscle size using 2 methods of data acquisition. Folia Phoniatr Logop. 2016;68(5):205–10. https://doi.org/10.1159/000473876.
Matsuo T, Matsuyama M, Nakatani K, Mori N. Evaluation of swallowing movement using ultrasonography. Radiol Phys Technol. 2020;13(1):62–8. https://doi.org/10.1007/s12194-019-00547-1.
Picelli A, Modenese A, Poletto E, Businaro V, Varalta V, Gandolfi M, Bonetti B, Smania N. May ultrasonography be considered a useful tool for bedside screening of dysphagia in patients with acute stroke? A cohort study. Minerva Med. 2021;112(3):354–8. https://doi.org/10.23736/S0026-4806.20.06571-4.
Costa BOID, Rodrigues DSB, Magalhães DDD, Santos AS, Santos RV, Azevedo EHM, Almeida AA, Pernambuco L. Quantitative ultrasound assessment of hyoid bone displacement during swallowing following thyroidectomy. Dysphagia. 2021;36(4):659–69. https://doi.org/10.1007/s00455-020-10180-5.
Kwong E, Ng KK, Leung MT, Zheng YP. Application of ultrasound biofeedback to the learning of the Mendelsohn Maneuver in non-dysphagic adults: a pilot study. Dysphagia. 2021;36(4):650–8. https://doi.org/10.1007/s00455-020-10179-y.
Winiker K, Burnip E, Gozdzikowska K, Guiu Hernandez E, Hammond R, Macrae P, Huckabee ML. Ultrasound: validity of a pocket-sized system in the assessment of swallowing. Dysphagia. 2021;36(6):1010–8. https://doi.org/10.1007/s00455-020-10232-w.
Peng CH, Pauloski BR. Ultrasonography as biofeedback to increase muscle activation during the Mendelsohn Maneuver in healthy adults. Dysphagia. 2023;38(4):1156–68. https://doi.org/10.1007/s00455-022-10542-1.
Ahn D, Lee GJ, Sohn JH. Ultrasonographic swallowing examination for early detection of neopharyngeal fistula after salvage total laryngectomy: a preliminary study. Head Neck. 2019;41(6):1804–8. https://doi.org/10.1002/hed.25617.
Yabunaka K, Konishi H, Nakagami G, Sanada H, Iizaka S, Sanada S, Ohue M. Ultrasonographic evaluation of geniohyoid muscle movement during swallowing: a study on healthy adults of various ages. Radiol Phys Technol. 2012;5(1):34–9. https://doi.org/10.1007/s12194-011-0132-3.
Shimizu S, Hanayama K, Metani H, Sugiyama T, Abe H, Seki S, Hiraoka T, Tsubahara A. Retest reliability of ultrasonic geniohyoid muscle measurement. Jpn J Compr Rehabilit Sci. 2016;7:55–60. https://doi.org/10.11336/jjcrs.7.55.
Shimizu S, Hanayama K, Nakato R, Sugiyama T, Tsubahara A. Ultrasonographic evaluation of geniohyoid muscle mass in perioperative patients. Kawasaki Med J. 2016;42:47–56. https://doi.org/10.11482/KMJ-E42(2)47.
Baba T, Goto T, Fujimoto K, Honda T, Yagi K, Nagao K, Ichikawa T. Age-related changes in geniohyoid muscle morphology predict reduced swallowing function. J Oral Health Biosci. 2017;30(1):18–25. https://doi.org/10.20738/johb.30.1_18.
Cheng DTH, Lee KYS, Ahuja AT, Tong MCF. Sonographic assessment of swallowing in irradiated nasopharyngeal carcinoma patients. Laryngoscope. 2018;128(11):2552–9. https://doi.org/10.1002/lary.27222.
Oh JC. Effect of the head extension swallowing exercise on suprahyoid muscle activity in elderly individuals. Exp Gerontol. 2018;110:133–8. https://doi.org/10.1016/j.exger.2018.06.004.
Mori T, Izumi S, Suzukamo Y, Okazaki T, Iketani S. Ultrasonography to detect age-related changes in swallowing muscles. Eur Geriatr Med. 2019;10(5):753–60. https://doi.org/10.1007/s41999-019-00223-y.
Choi JB, Jung YJ, Park JS. Comparison of 2 types of therapeutic exercise: jaw opening exercise and head lift exercise for dysphagic stroke: a pilot study. Medicine. 2020;99(38): e22136. https://doi.org/10.1097/MD.0000000000022136.
Miura Y, Nakagami G, Tohara H, Ogawa N, Sanada H. The association between jaw-opening strength, geniohyoid muscle thickness and echo intensity measured by ultrasound. Med Ultrason. 2020;22(3):299–304. https://doi.org/10.11152/mu-2317.
Yano J, Yamamoto-Shimizu S, Yokoyama T, Kumakura I, Hanayama K, Tsubahara A. Effects of tongue-strengthening exercise on the geniohyoid muscle in young healthy adults. Dysphagia. 2020;35(1):110–6. https://doi.org/10.1007/s00455-019-10011-2.
Ogawa N, Wakabayashi H, Mori T, Fujishima I, Oshima F, Itoda M, Kunieda K, Shigematsu T, Nishioka S, Tohara H, Ohno T, Nomoto A, Shimizu A, Yamada M, Ogawa S. Digastric muscle mass and intensity in older patients with sarcopenic dysphagia by ultrasonography. Geriatr Gerontol Int. 2021;21(1):14–9. https://doi.org/10.1111/ggi.14079.
Wakabayashi H, Kishima M, Itoda M. Improvement of swallowing-related muscle mass assessed by ultrasonography in malnourished patient with Wallenberg syndrome: a case report. J Gen Family Med. 2021;22(6):341–3. https://doi.org/10.1002/jgf2.428.
Pauloski BR, Yahnke K. Using ultrasound to document the effects of expiratory muscle strength training (EMST) on the geniohyoid muscle. Dysphagia. 2022;37:788–99. https://doi.org/10.1007/s00455-021-10328-x.
Lu F, Okazaki T, Okuyama J, Izumi SI. Impacts of body positions on the geniohyoid muscle contraction and swallowing difficulty in healthy adults. Clin Exp Dent Res. 2023. https://doi.org/10.1002/cre2.760.
Geddes DT, Chadwick LM, Kent JC, Garbin CP, Hartmann PE. Ultrasound imaging of infant swallowing during breast-feeding. Dysphagia. 2010;25(3):183–91. https://doi.org/10.1007/s00455-009-9241-0.
Dharmarathna I, Miles A, Allen JE. Current approaches to instrumental assessment of swallowing in children. Curr Opin Otolaryngol Head Neck Surg. 2018;26(6):349–55. https://doi.org/10.1097/MOO.0000000000000492.
Nakamori M, Imamura E, Fukuta M, Tachiyama K, Kamimura T, Hayashi Y, Matsushima H, Ogawa K, Nishino M, Hirata A, Mizoue T, Wakabayashi S. Tongue thickness measured by ultrasonography is associated with tongue pressure in the Japanese elderly. PLoS ONE. 2020;15(8): e0230224. https://doi.org/10.1371/journal.pone.0230224.
Huckabee ML, Macrae P, Lamvik K. Expanding instrumental options for dysphagia diagnosis and research: ultrasound and manometry. Folia Phoniatr Logop. 2015;67(6):269–84. https://doi.org/10.1159/000444636.
Blyth KM, McCabe P, Madill C, Ballard KJ. Ultrasound in dysphagia rehabilitation: a novel approach following partial glossectomy. Disabil Rehabil. 2017;39(21):2215–27. https://doi.org/10.1080/09638288.2016.1219400.
Nachalon Y, Nativ-Zeltzer N, Evangelista LM, Dhar SI, Lin SJ, Shen SC, Belafsky PC. Cervical fibrosis as a predictor of dysphagia. Laryngoscope. 2021;131(3):548–52. https://doi.org/10.1002/lary.28880.
Takuro B, Takaharu G, Keiko F, Tsuyoshi H, Kazutomo Y, Kan N, Tetsuo I. Age-related changes in geniohyoid muscle morphology predict reduced swallowing function. J Oral Health Biosci. 2017;30(1):18–25. https://doi.org/10.20738/johb.30.1_18.
Feng X, Cartwright MS, Walker FO, Bargoil JH, Hu Y, Butler SG. Ultrasonographic evaluation of geniohyoid muscle and hyoid bone during swallowing in young adults. Laryngoscope. 2015;125:1886–91. https://doi.org/10.1002/lary.25224.
Watkin KL, Diouf I, Gallagher TM, Logemann JA, Rademaker AW, Ettema SL. Ultrasonic quantification of geniohyoid cross-sectional area and tissue composition: a preliminary study of age and radiation effects. Head Neck. 2001;23(6):467–74. https://doi.org/10.1002/hed.1061.
Winiker K, Burnip E, Gozdzikowska K, Hernandez EG, Hammond R, Macrae P, Thomas P, Huckabee ML. Ultrasound: reliability of a pocket-sized system in the assessment of swallowing. J Speech Lang Hear Res. 2021;64(8):2928–40. https://doi.org/10.1044/2021_JSLHR-21-00026.
Winiker K, Hammond R, Thomas P, Dimmock A, Huckabee ML. Swallowing assessment in patients with dysphagia: validity and reliability of a pocket-sized ultrasound system. Int J Lang Commun Disord. 2022;57(3):539–51. https://doi.org/10.1111/1460-6984.12703.
Chen YC, Hsiao MY, Wang YC, Fu CP, Wang TG. Reliability of ultrasonography in evaluating hyoid bone movement. J Med Ultrasound. 2017;25(2):90–5. https://doi.org/10.1016/j.jmu.2017.01.002.
Andrade RA, do Sales Coriolano, M. D. G. W., de Souza, E. L. H., da Silva, J. H. C., da Cunha, M. D., Pernambuco, L., Ribeiro, V. V., & da Silva, H. J. Reliability of ultrasound examination of hyoid bone displacement amplitude: a systematic review and meta-analysis. Dysphagia. 2022;37(6):1375–85. https://doi.org/10.1007/s00455-022-10429-1.
Stone M, Davis EP. A head and transducer support system for making ultrasound images of tongue/jaw movement. J Acoust Soc Am. 1995;98(6):3107–12. https://doi.org/10.1121/1.413799.
Derrick D, Carignan C, Chen WR, Shujau M, Best CT. Three-dimensional printable ultrasound transducer stabilization system. J Acoust Soc Am. 2018;144(5):392. https://doi.org/10.1121/1.5066350.
Ma JK, Wrench AA. Automated assessment of hyoid movement during normal swallow using ultrasound. Int J Lang Commun Disord. 2022;57(3):615–29. https://doi.org/10.1111/1460-6984.12712.
Allen JE, Clunie G, Ma JK, Coffey M, Winiker K, Richmond S, Lowell SY, Volkmer A. Translating ultrasound into clinical practice for the assessment of swallowing and laryngeal function: a speech and language pathology-led consensus study. Dysphagia. 2022;37(6):1586–98. https://doi.org/10.1007/s00455-022-10413-9.
Hollinghurst J, Smithard DG. Identifying dysphagia and demographic associations in older adults using electronic health records: a national longitudinal observational study in Wales (United Kingdom) 2008–2018. Dysphagia. 2022;37(6):1612–22. https://doi.org/10.1007/s00455-022-10425-5.
van den Engel-Hoek L, Erasmus CE, Hendriks JC, Geurts AC, Klein WM, Pillen S, Sie LT, de Swart BJ, de Groot IJ. Oral muscles are progressively affected in Duchenne muscular dystrophy: implications for dysphagia treatment. J Neurol. 2013;260(5):1295–303. https://doi.org/10.1007/s00415-012-6793-y.
Hutcheson KA, Lewin JS, Barringer DA, Lisec A, Gunn GB, Moore MW, Holsinger FC. Late dysphagia after radiotherapy-based treatment of head and neck cancer. Cancer. 2012;118(23):5793–9. https://doi.org/10.1002/cncr.27631.
Acknowledgements
The authors thank Stephen C. Cobb, Ph.D., for his support and guidance in the early phases of this study.
Funding
This research was supported by a College of Health Sciences Stimulus for Extramural Enhancement & Development (SEED) Award, University of Wisconsin Milwaukee.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose. The authors have no conflicts of interest to declare that are relevant to the content of this article. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. The authors have no financial or proprietary interests in any material discussed in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pauloski, B.R., Yahnke, K.M. Reliability of Measuring Geniohyoid Cross-Sectional Area with B-Mode Ultrasound. Dysphagia (2024). https://doi.org/10.1007/s00455-024-10712-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00455-024-10712-3