Abstract
The aim of this study was to investigate temporal ultrasound measurements of the hyoid bone displacement during swallowing following thyroidectomy in women and to relate these measures to age, clinical outcomes, and upper digestive airway symptoms. The sample was divided into an experimental group (EG) of 20 women who underwent thyroidectomy (mean age = 49.55 years ± 15.14) and a control group (CG) of 20 healthy women volunteers (mean age = 40.75 years ± 15.92). Both groups were submitted to ultrasound assessment to obtain four temporal measurements of hyoid bone displacement during swallowing: elevation, anteriorization, maximum displacement, and maintenance of maximum displacement. In both groups, swallowing of ten milliliters of liquid and the same volume of thickened liquid (honey) were analyzed. The images were recorded on video (30 frames/second) and analyzed according to a standardized protocol. Temporal measurements of hyoid bone elevation and maximum displacement during swallowing of thickened liquid were significantly shorter in EG (p = 0.034 and p = 0.020, respectively). There were no differences in the swallowing of liquid, and no other variable was related to the ultrasound temporal measurements investigated. This study concludes that women who undergo thyroidectomy have a shorter time of hyoid bone elevation and maximum displacement during swallowing of 10 mL of thickened liquid.
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Dysphagia is a common adverse effect during the postoperative period of patients who undergo thyroidectomy whether in the presence of damage to vagus nerve branches or the absence of operative complications [1, 2]. Symptoms can occur in about 55% of cases [1]. They are usually transient, although there are reports of their presence during follow-up [3,4,5,6,7]. The most frequent symptoms reported in questionnaires or interviews after surgery include dry throat, throat clearing, odynophagia, foreign body sensation in the throat, and choking [5, 7,8,9,10]. The last three symptoms are also reported in preoperative moments usually due to compression caused by thyroid disease [2, 11, 12].
There are few studies using instrumental imaging resources to assess swallowing after thyroidectomy [1, 6, 13], especially with quantitative data. One of the aspects of swallowing kinematics that can be explored through quantitative measurements is hyoid bone displacement [14, 15]. It is known that thyroidectomy can limit the movement of the hyoid bone supposedly as a result of involvement of the cervical musculature [16], the postoperative scar tissue [6], and the adhesion between the laryngotracheal unit and the superficial tissue [13].
The hyoid bone plays a key role during the pharyngeal phase. It pulls the larynx anteriorly below the base of the tongue [17], supporting glottic adduction and lowering the epiglottis cartilage [18], with the consequent protection of lower airways [18, 19]. The excursion of the hyoid bone during swallowing is characterized by an elliptical movement with an initial displacement in the upper vertical direction to ensure an adequate laryngeal closure (elevation), and then forwards, at which point the pharyngoesophageal segment relaxes (anteriorization) mediated by the active coordination of the suprahyoid muscle and the relaxation of the infrahyoid muscle. After this trajectory, there is a return to the starting position [6, 20,21,22].
For some authors, this entire sequence of events corresponds to the duration of the pharyngeal response [23]. It is the most common sign of physiological onset of pharyngeal swallowing [24], as well as one of the main kinematic mechanisms for the safety and efficiency of swallowing. It depends on an accurate space–time synchrony [6, 20, 21]. Regarding the temporal dimension, it is known that a delay in the hyoid bone displacement during swallowing interferes with the closure of the laryngeal vestibule. Therefore, it is a potential risk factor for aspiration [25, 26].
The literature presents a great number of studies using videofluoroscopy. It is a reference standard for the diagnosis of oropharyngeal dysphagia to investigate or standardize temporal and spatial kinematic measurements of hyoid bone displacement during swallowing in different populations [14, 17, 18, 24,25,26,27,28,29,30,31,32,33], including individuals who undergo thyroidectomy [6].
However, another instrumental resource that can be used to evaluate parameters related to the kinematics of swallowing is ultrasonography. It is an accessible and low-cost exam [22] with an applicability greater than 90% [34]. It can provide images in real time [35] and does not expose the patient to radiation [22, 36]. Ultrasonography is a method that allows visualizing the hyoid bone and provides information on its displacement during swallowing [19].
Most ultrasound studies have assessed hyoid bone displacement with the transducer positioned in the submental region [15, 22, 37,38,39,40,41,42,43,44]. However, it is also possible to perform this evaluation by transcutaneous laryngeal ultrasonography (TLUS), a procedure by which the transducer is positioned in the anterior or lateral cervical region [45,46,47,48,49,50].
In general, studies evaluating temporal measurements of hyoid bone displacement by ultrasonography essentially measure the time interval between rest and the maximum hyoid excursion point during swallowing [22, 46, 49]. More traditional studies have evaluated in more detail the duration of each stage of hyoid bone excursion during elevation, anteriorization, and rest [19, 38, 51, 52]. However, no study has evaluated the temporal measurements of hyoid bone displacement in patients who underwent thyroidectomy.
The only study that assessed swallowing after thyroidectomy using ultrasonography measured the distance from laryngotracheal elevation [13]. Even in studies that used videofluoroscopy after thyroidectomy, the hyoid excursion time was not assessed [6, 53].
Thus, the relevance of hyoid bone displacement for swallowing, the signs of functional impairment of swallowing due to thyroidectomy, the lack of knowledge about the temporal measurements related to this kinematical event in the population who undergo surgery, and the possibility of extraction of these measurements by ultrasonography is clear given that this exam is a viable, available, and low-cost tool to carry out such an investigation.
Therefore, the aim of this study was to investigate quantitative ultrasound measurements of hyoid bone displacement time during swallowing following thyroidectomy and relate these measurements with age, clinical outcomes, and patient-reported upper digestive airway symptoms.
Methods
This is a cross-sectional study with a comparison group. It was approved by the institution's Ethics and Research Committee under no. 2.314.731/18. All individuals signed an informed consent.
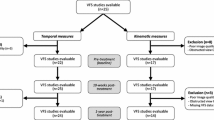
Sample
The study comprised an experimental group (EG) and a control group (CG). In the EG, the inclusion criteria were (1) age equal to or above 18 years, (2) women, and (3) partial or total thyroidectomy. The inclusion criteria in the CG were (1) age equal to or above 18 years, (2) women, (3) no thyroidectomy, and (4) no diagnosis of thyroid disease or self-reported swallow disorders at the time of data collection. In both groups, individuals with (1) neurological diseases, (2) history of radiotherapy or surgery in the head and neck (except thyroidectomy for the EG group), and (3) difficulties in understanding and executing simple orders were excluded.
The sample of both groups was obtained by convenience and followed a 1:1 ratio. In the EG, twenty women aged 22 to 78 years (mean age = 49.55 years; SD = 15.14) were recruited from the Head and Neck Surgery service of the university hospital after a medical consultation of postoperative follow-up. Table 1 shows the clinical characteristics of the EG. The CG comprised twenty women aged 19 to 68 years (mean age = 40.75; SD = 15.92) selected by active search in the hospital and the local community. The results of homogeneity test indicated that the age of both groups was comparable (Z = − 1.78; p = 0.07).
Data Collection
Data collection was carried out between May 2018 and April 2019. At the first stage, personal and clinical data were collected from medical records or through interviews with volunteers.
Then, only in the EG, the questionnaire “Symptoms of the Upper Digestive Airways” (SVADS) was applied [5]. The SVADS was developed by Brazilian researchers. It is specific for patients who undergo thyroidectomy. The SVADS has 18 items divided into vocal and swallowing symptoms. Although it has not yet been validated, it has already been applied by other researchers in Brazil [13]. In this study, the answer options of the SVADS questionnaire were adapted to “yes” or “no” to identify the presence or absence of vocal and swallowing complaints.
Subsequently, the volunteer was directed to TLUS. It was always performed by the same head and neck surgeon with experience in cervical ultrasound with the support of a speech and language therapist. The LOGIQ P6 equipment (GE Healthcare®, Chicago, IL) was used in B mode with a Vascular > Carotid adjustment of 2.0–5.5 MHz linear matrix convex transducer. The ultrasound equipment recorded the video exam in.wmv format and the file was saved on a portable external HD for later analysis.
The TLUS was divided into acquisition and analysis phases following a methodological proposal developed for this study based on the literature [46,47,48,49,50] and consensus among researchers.
At the acquisition phase, the volunteer was seated in a chair, following the Frankfurt plan, with plantar support, and instructed to maintain an angle of 90 degrees (90°) between the submental area and the neck, approaching the functional position of swallowing. The transducer was placed in contact with a layer of water-soluble gel and positioned transversely in the median portion of the anterior cervical area (Fig. 1a). We decided to use the transducer in this position as it allows a better visualization of hyoid bone displacement during swallowing [41, 45, 47,48,49].
The USG equipment was set to B mode (echo processing mode) and calibrated for each volunteer in relation to brightness and contrast in order to obtain the best view of the hyperechoic image of the hyoid bone and the hypoechoic acoustic shadow produced by this structure (Fig. 1b).
Then, two swallowing tasks were requested from patients in the following sequence: ten milliliters (mL) of liquid (water) and 10 mL of thickened liquid (honey). Each task was repeated three times, with an interval of 30 s. To prepare the thickened liquid, a thickener based on maltodextrin and modified corn starch was used at a volume recommended by the manufacturer (1½ tablespoon to 100 mL of water). We added a volume corresponding to a spoon of 1 mL of powdered peach-flavored juice.
In all tasks, the volunteer was asked to keep the volume in the oral cavity and swallow only after the command of the researcher. For analysis purposes, only the second or intermediate swallowing was considered. The assessment was recorded in.wmv at 30 frames per second.
At the analysis phase, the videos were initially decomposed into frames using the Free Video to JPG Converter software and subsequently analyzed using the ImageJ software to extract the measurements of interest.
Four temporal measurements related to hyoid bone displacement during swallowing were extracted based on other studies [19, 38, 46, 49]: hyoid bone elevation time (HBET), hyoid bone anteriorization time (HBAT), maximum hyoid bone displacement time (MHBDT), and maximum hyoid bone displacement maintenance time (MHBDMT).
The reference points for extracting each measurement were as follows: HBET—onset: first frame showing the upward movement of the hyoid bone; offset: prior frame to the beginning of the anteriorization; HBAT—onset: first frame showing the diagonal shift of the hyoid bone towards the anterior area; offset: first frame representing the stabilization of the hyoid bone at the maximum anteriorization position; MHBDT—sum of HBET and HBAT; MHBDMT—onset: first frame after the last HBAT frame; offset: frame before the first hyoid bone movement of return to the resting position. Figure 2 shows a sequence of four frames using the ImageJ software.
Each measurement was the result of the time between the initial frame and the final frame of the respective event in seconds (s). As each frame has 0.03 s (30 frames/s), the number of frames for each measurement was calculated. The result was multiplied by 0.03 and thus the temporal measurement was obtained. The data analysis was performed by three previously trained speech and language therapists. Inter- and intrajudge correlation was estimated using the intraclass correlation coefficient (ICC), absolute agreement type. Interjudge ICCs were moderate (0.5 to 0.71) and the measurements of the rater with the best intrajudge correlation (0.75 to 0.92) were considered for final analysis.
Statistical Analysis
Data were analyzed descriptively. To analyze the correlation between quantitative measures, the Spearman's correlation test was applied. To compare the measurements between the EG and CG groups and between categories of clinical variables, the U Mann–Whitney nonparametric test was used. The level of significance for all tests was 5%. All statistical analyses were performed using the software PSPP (https://www.gnu.org/software/pspp/).
Results
Table 2 shows the comparison of the measurements between EG and CG. The HBET and MHBDT were significantly lower in EG compared to CG for the swallowing of thickened liquid. No significant difference was found between the groups in the swallowing of liquid.
Figure 3 shows the EG distribution of patient-reported upper digestive airway symptoms according to the SVADS questionnaire. The most prevalent symptoms were throat clearing (75%), hoarseness (55%), a feeling of bolus in the throat (50%), and dry throat (50%).
Figure 4 shows scatter graphs corresponding to correlations between age and temporal measurements of hyoid bone displacement during swallowing in the EG. Most temporal measurements decreased with aging, but with no significant correlation.
Scatter plots showing correlations between age and temporal measures of hyoid bone displacement during swallowing of ten milliliters of liquid consistency and ten milliliters of thickened liquid (honey). HBET hyoid bone elevation time, HBAT hyoid bone anteriorization time, MHBDT maximum hyoid bone displacement time, MHBDMT maximum hyoid bone displacement maintenance time; p < 0.05. Spearman’s correlation test (rho)
No temporal measurements of hyoid bone displacement during swallowing were related to nosological diagnosis, type of surgery, post-surgical time, and self-reported swallowing or vocal disorders in patients who underwent thyroidectomy (Table 3).
Discussion
This study investigated ultrasound temporal measurements of hyoid bone displacement during swallowing in women following thyroidectomy by comparing them with women without thyroid diseases. The HBET and MHBDT were significantly lower during swallowing of thickened liquid in women who underwent thyroidectomy.
The elevation movement removes the hyoid bone from its resting anchorage to a posterior and cranial direction by the action of the styloglossus and stylopharyngeus muscles, followed by an anteriorization movement activated by the mylohyoid and geniohyoid muscles [54]. Therefore, temporal changes at one of these stages or both can affect total hyoid bone displacement time during swallowing.
It is assumed that lower HBET and the consequent decrease in MHBDT in women who underwent thyroidectomy are related to the same etiology factors associated with the range of motion decrease in this area, i.e., adherence of the laryngotracheal unit to the subcutaneous soft tissue of the neck after surgery [13], cervical muscle involvement by surgical manipulation [16], and postoperative scar tissue [6].
Considering that hyoid bone elevation is relevant for swallowing safety [21, 55] and anteriorization is associated with relaxation of the pharyngoesophageal segment [25], a decrease in the hyoid bone displacement time may be related to common findings in the swallowing of patients who undergo thyroidectomy, such as changes in pharyngeal transit of the bolus flow and esophageal motility, in addition to pharyngeal residue [1, 2].
The suprahyoid muscles play an active role in hyoid bone displacement and most muscle fibers are involved with the elevation movement [24]. Therefore, as there is manipulation of the suprahyoid area during thyroidectomy, it appears that the elevation movement is more exposed to damages. This may have occurred in this sample, as EG and CG were different regarding HBET and MHBDT.
This finding can be also related to the decrease in the amplitude of hyoid bone trajectory after thyroidectomy [6]. It is possible that the time required to complete this path will also be shorter. The relation between the space and time measurements also affects movement speed, but the integration between these three properties is not so linear [51, 52]. A study with healthy individuals revealed that hyoid bone displacement performed in a shorter time does not necessarily correspond to a fastest movement [52]. The integration between measurements of space, time, and speed of hyoid bone displacement following thyroidectomy has not yet been investigated and should be the focus of further studies.
The effects of decreased HBET and MHBDT after thyroidectomy occurred only when swallowing thickened liquid. Some previous studies assessed the effects of different types of consistencies on hyoid bone displacement during swallowing [39, 46, 50, 51, 56], but no study explored this finding after thyroidectomy.
In healthy individuals, the swallowing of thicker consistency implies a slower pharyngeal flow and a greater time difference between the onset of various biomechanical swallowing events compared to liquid consistency [11, 25]. Therefore, the shorter times of elevation and maximum hyoid bone displacement when swallowing thickened liquid after thyroidectomy imply a greater exposure of patients to pharyngeal and pharyngoesophageal transition residues, since the time required for the pharyngeal clearance of this consistency may not be enough.
This hypothesis is aligned with complaints such as throat clearing and a feeling of bolus in the throat, two of the most reported symptoms by EG members. In addition, changes in HBET and MHBDT can disturb the temporal coordination between the other kinematic actions of swallowing, which exposes the individual to a greater risk of oropharyngeal dysphagia.
Unlike HBET and MHBDT, the HBAT and MHBDMT did not show any significant differences between EG and CG. This indicates that the impact of the surgery is mainly related to the initial traction of the hyoid bone. Therefore, it is relevant to consider not only a global measurement, but also the analysis of each step of the movement for the most accurate identification of a possible change in temporal hyoid bone displacement.
In this study, no significant correlation was found between age and temporal measurements of the hyoid bone displacement in the EG, although the former is considered a variable that affects swallowing time [20, 57] and hyoid bone excursion in healthy individuals [24, 27, 32, 38]. It is possible that the impact of thyroidectomy on the swallowing kinematics modifies the correlation between age and temporal measurements of hyoid bone displacement, mitigating a possible difference between individuals with distinct ages. However, the results showed a decrease tendency in all studied measurements according to the advancing age, but a broader sample of patients is necessary to confirm this finding.
In the EG group, variables related to surgery, such as nosological diagnosis, type of thyroidectomy (total or partial), and postoperative time, were not related to the temporal measurements investigated. Regarding the postoperative time, one of the few studies on a temporal analysis of swallowing after thyroidectomy [6] verified by videofluoroscopy that the maximum excursion distance of the hyoid bone before surgery was similar to that of the control group in people with no surgical indication. One week after thyroidectomy, this measurement decreased significantly in relation to that of the control group at the preoperative period, remaining for three months after surgery.
In the present study, the temporal measurements of hyoid bone displacement were similar among women who underwent thyroidectomy more than 12 months previously to the study or even more recent. Although the comparison groups, the assessment tool, the measurements, and the postoperative period marker were different from the study by Im et al. [6], the results found in this study also point out that quantitative measurements of hyoid bone displacement during swallowing, in this case temporal measurements, do not suffer the effects of postoperative time in patients who underwent thyroidectomy. It is possible that thyroidectomy promotes impacts on hyoid excursion that are difficult to reverse, or that these measurements are highly variable individually, which requires a larger sample to identify differences between results. This could be better studied in longitudinal studies that follow patients from the preoperative to a longer period.
In the literature, there are reports indicating a greater number of voice and swallowing complaints in patients who underwent total thyroidectomy [58]. Thus, there is a hypothesis according to which cases with a more severe nosological diagnosis, total thyroidectomy, and the presence of upper digestive airway symptoms could influence the temporal measurements of displacement of the hyoid bone in this study, but this did not occur.
The results indicated that the temporal measurements of hyoid bone displacement are independent from these variables, and that the possible causes of changes in these measurements need to be further investigated, including vagus nerve injuries during surgery [11] and the post-thyroidectomy syndrome, in which the patient presents pharyngolaryngeal symptoms even in the absence of surgical complications [11, 59].
Although the prevalent postoperative symptoms found in this study were comparable to findings of previous studies, such as throat clearing [10], hoarseness [5, 10], a feeling of a lump in the throat [10], and dry throat [5], the presence of complaints is not related to temporal measurements of hyoid bone displacement. This information evidences that the self-reported outcome does not always reflect the objective clinical measurements of swallowing, as other authors already pointed out [7]. Therefore, these dimensions must be complementary.
The findings show that thyroidectomy can affect the temporal aspects of an essential kinematic event of swallowing safety and efficiency. It is important to highlight that temporal measurements should not be used in isolation for the diagnosis of oropharyngeal dysphagia, as the study of temporal measurements makes it possible to understand only a specific swallowing event. Swallowing assessment is comprehensive and needs to be contextualized together with other tests used in clinical routines.
The absence of a relation between temporal measurements of hyoid bone displacement and the other studied variables highlights that further studies are needed to identify the associated risk factors of changes in these measurements after thyroidectomy.
Finally, TLUS used to assess hyoid bone displacement should be analyzed together with other kinematic measurements (amplitude and velocity) and incorporated as a complementary instrumental examination in the diagnosis of swallowing disorders after thyroidectomy. It is an available, non-invasive, and easily accessible exam that can be used as a support resource for clinical decision-making and monitoring of oropharyngeal dysphagia.
Limitations of the study
This study has some limitations. The sampling was by convenience and the volunteers were from a single health service. Future multicenter researches may minimize such biases. There was no investigation of damage to the vagus nerve branches in the EG, or laryngeal investigations in both groups. In addition, there was no collection at the preoperative period and all swallowing tasks were performed only with the researcher’s command. Future studies with a longitudinal design should better control these aspects.
Conclusion
The time of hyoid bone elevation and the maximum displacement during swallowing of 10 mL of thickened liquid are shorter after thyroidectomy. The temporal measurements of hyoid bone displacement after thyroidectomy are not related to age, post-surgical time, type of surgery, diagnosis, and patient-reported upper digestive airway symptoms.
Data Availability
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
References
Arakawa-Sugueno L, Ferraz AR, Morandi J, et al. Videoendoscopic evaluation of swallowing after thyroidectomy: 7 and 60 days. Dysphagia. 2015;30:496–505. https://doi.org/10.1007/s00455-015-9628-z.
Scerrino G, Tudisca C, Bonventre S, et al. Swallowing disorders after thyroidectomy: What we know and we are. A systematic review. Int J Surg. 2017;41:S94–S102. https://doi.org/10.1016/j.ijsu.2017.03.078.
Wasserman JM, Sundaram K, Alfonso AE, et al. Determination of the function of the internal branch of the superior laryngeal nerve after thyroidectomy. Head Neck. 2008;30:21–7. https://doi.org/10.1002/hed.20648.
Lombardi CP, Raffaelli M, D’Alatri L, et al. Voice and swallowing changes after thyroidectomy in patients without inferior laryngeal nerve injuries. Surgery. 2006;140:1026–32. https://doi.org/10.1016/j.surg.2006.08.008.
Silva IC, de Netto I, Vartanian JG, et al. Prevalence of upper aerodigestive symptoms in patients who underwent thyroidectomy with and without the use of intraoperative laryngeal nerve monitoring. Thyroid. 2012;22:814–9. https://doi.org/10.1089/thy.2011.0118.
Im I, Jun J-P, Crary MA, Carnaby GD, Hong KH. Longitudinal kinematic evaluation of pharyngeal swallowing impairment in thyroidectomy patients. Dysphagia. 2018;34:161–9. https://doi.org/10.1007/s00455-018-9949-9.
Krekeler BN, Wendt E, Macdonald CL, Connor NP. Patient-reported dysphagia after thyroidectomy: A qualitative study. JAMA Otolaryngol Head Neck Surg. 2018;144:342–8. https://doi.org/10.1001/jamaoto.2017.3378.
Pereira JA, Girvent M, Sancho JJ, et al. Prevalence of long-term upper aerodigestive symptoms after uncomplicated bilateral thyroidectomy. Surgery. 2003;133:318–22. https://doi.org/10.1067/msy.2003.58.
Senise AT, Queija DS, Degani C, et al. Sintomas e sinais de alterações da deglutição após a tireoidectomia. Rev bras cir cabeça pescoço. 2009;38:67–71 [in Portuguese].
Araújo LF, Lopes LW, Silva POC, et al. Sensory symptoms in patients undergoing thyroidectomy. CoDAS. 2017;29:e20150294. https://doi.org/10.1590/2317-1782/20172016294.
Nam IC, Park YH. Pharyngolaryngeal symptoms associated with thyroid disease. Curr Opin Otolaryngol Head Neck Surg. 2017;25:469–74. https://doi.org/10.1097/MOO.0000000000000404.
Pernambuco LA, Silva MP, Almeida MN, et al. Self-perception of swallowing by patients with benign nonsurgical thyroid disease. CoDAS. 2017;29(1):e20160020. https://doi.org/10.1590/2317-1782/20162016020.
Cho JG, Byeon HK, Oh KH, et al. Objective assessment swallowing difficulty through ultrasound in patients undergoing thyroidectomy. Dysphagia. 2020;35:253–60. https://doi.org/10.1007/s00455-019-10020-1.
Kendall KA, McKenzie S, Leonard RJ, et al. Timing of events in normal swallowing: a videofluoroscopic study. Dysphagia. 2000;15:74–83. https://doi.org/10.1007/s004550010004.
Steele C, Sasse C, Bressmann T. Tongue-pressure and hyoid movement timing in healthy liquid swallowing. Int J Lang Commun Disord. 2012;47:77–83. https://doi.org/10.1111/j.1460-6984.2011.00082.x.
Hong KH, Yang WS, Park MJ, et al. Changes in oral vowel sounds and hyoid bone movement after thyroidectomy. Clin Exp Otorhinolaryngol. 2017;10:168–73.
Schiffer BL, Kendall K. Changes in timing of swallow events in Parkinson’s disease. Ann Otol Rhinol Laryngol. 2018;128:22–7. https://doi.org/10.1177/0003489418806918.
Perlman AL, VanDaele DJ, Otterbacher MS. Quantitative assessment of hyoid bone displacement from video images during swallowing. J Speech Hear Res. 1995;38:579–85. https://doi.org/10.1044/jshr.3803.579.
Sonies BC, Wang C, Sapper DJ. Evaluation of normal and abnormal hyoid bone movement during swallowing by use of ultrasound duplex-Doppler imaging. Ultrasound Med Biol. 1996;22:1169–75. https://doi.org/10.1016/s0301-5629(96)00158-5.
Cook IJ, Dodds WJ, Dantas RO. Opening mechanisms of the human upper esophageal sphincter. Am J Physiol. 1989;257:G748–759. https://doi.org/10.1152/ajpgi.1989.257.5.G748.
Sivarao D, Goyal RK. Functional anatomy and physiology of the upper esophageal sphincter. Am J Med. 2000;108:27–37. https://doi.org/10.1016/s0002-9343(99)00337-x.
Kwak H-J, Kim L, Ryu B-J, et al. Influence of nasogastric tubes on swallowing in stroke patients: measuring hyoid bone movement with ultrasonography. Ann Rehabil Med. 2018;42:551–9. https://doi.org/10.5535/arm.2018.42.4.551.
Robbins J, Hamilton JW, Lof GL, Kempster GB. Oropharyngeal swallowing in normal adults of different ages. Gastroenterology. 1992;103:823–9.
Kim Y, McCullough GH. Maximum hyoid displacement in normal swallowing. Dysphagia. 2008;23:274–9. https://doi.org/10.1007/s00455-007-9135-y.
Ishida R, Palmer JB, Hiiemae KM. Hyoid motion during swallowing: factors affecting forward and upward displacement. Dysphagia. 2002;17:262–72. https://doi.org/10.1007/s00455-002-0064-5.
Logemann JA, Kahrilas PJ, Cheng J, et al. Closure mechanisms of laryngeal vestibule during swallow. Am J Physiol. 1992;262:G338–344. https://doi.org/10.1152/ajpgi.1992.262.2.G338.
Kang B, Oh B, Kim IS, et al. Influence of aging on movement of the hyoid bone and epiglottis during normal swallowing: a motion analysis. Gerontology. 2010;56:474–82. https://doi.org/10.1159/000274517.
Kendall KA, Leonard RJ. Hyoid movement during swallowing in older patients with dysphagia. Ann Otolaryngol Head Neck Surg. 2001;127:1224–9. https://doi.org/10.1001/archotol.127.10.1224.
Nam HS, Oh BM, Han TR. Temporal characteristics of hyolaryngeal structural movements in normal swallowing. Laryngoscope. 2015;125:2129–33. https://doi.org/10.1002/lary.25229.
Ragland MC, Park T, McCullough G, Kim Y. The speed of the hyoid excursion in normal swallowing. Clin Arch Commun Disord. 2016;1:30–5.
Kraaijenga SA, van der Molen L, Heemsbergen WD, et al. Hyoid bone displacement as parameter for swallowing. Eur Arch Otorhinolaryngol. 2017;274:597–606. https://doi.org/10.1007/s00405-016-4029-y.
Molfenter SM, Steele CM. Physiological variability in the deglutition literature: hyoid and laryngeal kinematics. Dysphagia. 2011;26:67–74. https://doi.org/10.1007/s00455-010-9309-x.
Molfenter SM, Steele CM. Temporal variability in the deglutition literature. Dysphagia. 2012;27:162–77. https://doi.org/10.1007/s00455-012-9397-x.
Wong K-P, Woo J-W, Youn Y-K, et al. The importance of sonographic landmarks by transcutaneous laryngeal ultrasonography in post-thyroidectomy vocal cord assessment. Surgery. 2014;156:1590–6. https://doi.org/10.1016/j.surg.2014.08.061.
Tsui PH, Wan YL, Chen CK. Ultrasound imaging of the larynx and vocal folds: recent applications and developments. Curr Opin Otolaryngol Head Neck Surg. 2012;20:437–42. https://doi.org/10.1097/MOO.0b013e32835896b4.
Cheng S-P, Lee J-J, Liu T-P, et al. Preoperative ultrasonography assessment of vocal cord movement during thyroid and parathyroid surgery. World J Surg. 2012;36:2509–15. https://doi.org/10.1007/s00268-012-1674-1.
Shawker TH, Sonies B, Hall TE, Baum BF. Ultrasound analysis of tongue, hyoid, and larynx activity during swallowing. Invest Radiol. 1984;19:82–6. https://doi.org/10.1097/00004424-198403000-00003.
Sonies BC, Parent LJ, Morrish K, Baum BJ. Durational aspects of the oral-pharyngeal phase of swallow in normal adults. Dysphagia. 1988;3:1–10. https://doi.org/10.1007/bf02406274.
Scarborough DR, Waizenhofer S, Siekemeyer L, et al. Sonographically measured hyoid bone displacement during swallow in preschool children: a preliminary study. J Clin Ultrasound. 2010;38:430. https://doi.org/10.1002/jcu.20733.
Macrae PR, Doeltgen SH, Jones RD, Huckabee ML. Intra- and inter-rater reliability for analysis of hyoid displacement measured with sonography. J Clin Ultrasound. 2012;40:74–8. https://doi.org/10.1002/jcu.20874.
Feng X, Cartwright MS, Walker FO, et al. Ultrasonographic evaluation of geniohyoid muscle and hyoid bone during swallowing in young adults. Laryngoscope. 2015;125:1886–911. https://doi.org/10.1002/lary.25224.
Rocha SG, Silva RG, Berti LC. Qualitative and quantitative ultrasound analysis of oropharyngeal swallowing. CoDAS. 2015;27:437–45. https://doi.org/10.1590/2317-1782/20152015015.
Lee YS, Lee KE, Yang Y, et al. Usefulness of submental ultrasonographic evaluation for dysphagia patients. Ann Rehabil Med. 2016;40:197–205. https://doi.org/10.5535/arm.2016.40.2.197.
Chen YC, Hsiao MY, Wang YC, et al. Reliability of ultrasonography in evaluating hyoid bone movement. J Med Ultrasound. 2017;25:90–5. https://doi.org/10.1016/j.jmu.2017.01.002.
Kuhl V, Eicke BM, Dieterich M, Urban PP. Sonographic analysis of laryngeal elevation during swallowing. J Neurol. 2003;250:333–7. https://doi.org/10.1007/s00415-003-1007-2.
Freitas AB. Relações entre deglutição e qualidade vocal: análise ultrassonográfica e perceptiva. Thesis, Ponticífica Universidade Católica de São Paulo; 2017 [in Portuguese].
Oh EH, Seo JS, Kang HJ. Assessment of oropharyngeal dysphagia in patients with Parkinson disease: use of ultrasonography. Ann Rehabil Med. 2016;40:190–6. https://doi.org/10.5535/arm.2016.40.2.190.
Ahn SY, Cho KH, Beom J, et al. Reliability of ultrasound evaluation of hyoid-larynx approximation with positional change. Ultrasound Med Biol. 2015;41:1221–5. https://doi.org/10.1016/j.ultrasmedbio.2014.12.010.
Yabunaka K, Sanada H, Sanada S, et al. Sonographic assessment of hyoid bone movement during swallowing: a study of normal adults with advancing age. Radiol Phys Technol. 2011;4:73–7. https://doi.org/10.1007/s12194-010-0107-9.
Lynch CS, Chammas MC, Mansur LL, Cerri GG. Biomecânica ultra-sonográfica da deglutição: estudo preliminar. Radiol Bras. 2008;41:241–4. https://doi.org/10.1590/S0100-39842008000400008.
Chi-Fishman G, Sonies BC. Kinematic strategies for hyoid movement in rapid sequential swallowing. J Speech Lang Hear Res. 2002;45:457. https://doi.org/10.1044/1092-4388.
Chi-Fishman G, Sonies BC. Effects of systematic bolus viscosity and volume changes on hyoid movement kinematics. Dysphagia. 2002;17:278. https://doi.org/10.1007/s00455-002-0070-7.
Jung SP, Kim SH, Bae SY, et al. A new subfascial approach in open thyroidectomy: efficacy for postoperative voice, sensory, and swallowing symptoms. a randomized controlled study. Ann Surg Oncol. 2013;20:3869–76. https://doi.org/10.1245/s10434-013-3163-7.
Ekberg O. The normal movements of the hyoid bone during swallow. Invest Radiol. 1986;21:408–10. https://doi.org/10.1097/00004424-198605000-00009.
Logemann JA. Evaluation and treatment of swallowing disorders. Nerang: Pro-Ed Australia; 1983.
Steele CM, Alsanei WA, Ayanikalath S, et al. The influence of food texture and liquid consistency modification on swallowing physiology and function: a systematic review. Dysphagia. 2015;30:2–26. https://doi.org/10.1007/s00455-014-9578-x.
Mendell DA, Logemann JA. Temporal sequence of swallow events during the oropharyngeal swallow. J Med Speech Lang Pathol. 2007;50:1256–71.
Park YM, Oh KH, Cho JG, et al. Changes in voice- and swallowing-related symptoms after thyroidectomy: one-year follow-up study. Ann Otol Rhinol Laryngol. 2018;127:171–7. https://doi.org/10.1177/0003489417751472.
Park KN, Mok JO, Chung CH, Lee SW. Does postthyroidectomy syndrome really exist following thyroidectomy? Prospective comparative analysis of open vs. endoscopic thyroidectomy. Clin Exp Otorhinolaryngol. 2015;8:76–80. https://doi.org/10.3342/ceo.2015.8.1.76.
Acknowledgements
The authors would like to thank the National Council of Technological and Scientific Development (Conselho Nacional de Desenvolvimento Científico e Tecnológico—CNPq) which had a financial support with Edital Universal (Process: 430286/2016-3); and the Education Ministry’s Coordination for the Improvement of Higher Education Personnel (Ministério da Educação/Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—CAPES) for the scholarship granted to the first author (Social Demand Program/CAPES/MEC).
Funding
This study had a financial support by the National Council of Technological and Scientific Development (Conselho Nacional de Desenvolvimento Científico e Tecnológico—CNPq) with Edital Universal (Process: 430286/2016-3).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by BOIC, DSBR, DDDM, ASS, and RVS. Review and editing were performed by LP, EHMA, and AAFA. LP was responsible for supervision and funding acquisition. The first draft of the manuscript was written by BOIC and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical Approval
All procedures were approved by the ethics and institutional review committee (no. 2.314.731/18 and CAAE: 72723617.2.0000.5183) according to Resolution 466/2012 of the National Health Council (CNS) and according to the World Medical Association Declaration of Helsinki.
Informed Consent
All participants signed the informed consent before participation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Costa, B.O.I., Rodrigues, D.d.B., Magalhães, D.D.D. et al. Quantitative Ultrasound Assessment of Hyoid Bone Displacement During Swallowing Following Thyroidectomy. Dysphagia 36, 659–669 (2021). https://doi.org/10.1007/s00455-020-10180-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-020-10180-5