Abstract
The aim of this study was to compare selected parameters of two swallow evaluations: fiberoptic endoscopic evaluation of swallowing (FEES) and the modified barium swallow (MBS) study. This was a cross-sectional, descriptive study. Fifty-five clinicians were asked to watch video recordings of swallow evaluations of 2 patients that were done using fluoroscopy and endoscopy simultaneously. In a randomized order, clinicians viewed 4 edited videos from simultaneous evaluations: the FEES and MBS videos of patient 1 and 2 each taking one swallow of 5 mL applesauce. Clinicians filled out a questionnaire that asked (1) which anatomical sites they could visualize on each video, (2) where they saw pharyngeal residue after a swallow, (3) their overall clinical impression of the pharyngeal residue, and (4) their opinions of the evaluation styles. Clinicians reported a significant difference in the visualization of anatomical sites, 11 of the 15 sites were reported as better-visualized on the FEES than on the MBS video (p < 0.05). Clinicians also rated residue to be present in more locations on the FEES than on the MBS. Clinicians’ overall impressions of the severity of residue on the same exact swallow were significantly different depending on the evaluation type (FEES vs. MBS for patient 1 χ2 = 20.05, p < 0.0001; patient 2 χ2 = 7.52, p = 0.006), with FEES videos rated more severely. FEES advantages were: more visualization of pharyngeal and laryngeal swallowing anatomy and residue. However, as a result, clinicians provided more severe impressions of residue amount on FEES. On one hand, this suggests that FEES is a more sensitive tool than MBS studies, but on the other hand, clinicians might provide more severe interpretations on FEES.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
When a patient presents with a suspected dysphagia, clinicians commonly look to one of the two most common instrumental swallowing evaluations: a modified barium swallow (MBS), performed with videofluoroscopy, or a fiberoptic endoscopic evaluation of swallowing (FEES). Many studies have compared the parameters of MBS and FEES studies for evaluating dysphagia. These parameters include clinical indications [1], outcomes [2], and exam sensitivity to certain aspects of dysphagia such as aspiration [3–7, 21]. Experts in the field have subjectively compared the two evaluations, citing MBS advantages like better oral and esophageal phase visualization and FEES advantages such as better assessment of pharyngeal timing and better visualization of point of entry for aspiration [1, 5, 8]. As studies continue to compare the instrumental evaluations, more and more are citing FEES as an equivalent gold standard [9, 10], if not better [4, 5]. However, most evaluation comparisons have been subjective and based on expert opinion [1, 8, 9]. When not, the evaluations are compared using videos that have been performed one after the other, increasing the influence of uncontrolled variables from evaluations performed at different times [3, 5, 11–15]. The majority of what is currently known is based on these studies that have used sequential and not simultaneous evaluations for comparison.
Only a handful of studies to date have used simultaneous evaluations when investigating parameters of swallowing evaluations [6, 7, 16, 31, 32]. Using simultaneous evaluations, the researchers could be sure that the exact same event was occurring on each video and it was the style of the evaluations that caused a different impression rather than a different event. In 2003, Rao and colleagues investigated penetration, aspiration, and pharyngeal residue using simultaneous evaluations, capturing the same swallow on MBS and FEES at the same time [6]. The researchers analyzed the sensitivity and specificity of each evaluation by using the other as the gold standard. They found that when using the MBS evaluation as a gold standard, FEES ratings regarding penetration, aspiration, and pharyngeal residue differed from the MBS ratings. But when FEES was the gold standard, the MBS ratings were nearly the same. For instance, FEES detected penetration in 10 out of 10 instances, while the MBS detected none of these instances. The same pattern occurred for aspiration. In all 3 instances of aspiration, FEES detected it when the MBS did not. For pharyngeal residue, FEES detected it in 14/15 instances, while the MBS detected 1/15. Their results suggest that the bolus was better visualized on FEES. Other studies have since used simultaneous evaluations and demonstrated similar results of a more severe impression from FEES. In 2 of the studies, clinicians gave higher penetration-aspiration scale scores and reported more severe impressions of residue when rating FEES than when rating MBS videos [7, 16].
The results from these studies are informative for the field of swallowing evaluation and deserve more investigation because it is clear that clinicians have different impressions from each exam type. In fact, Rao et al. reported that the percent agreement between FEES and MBS, accounting for chance, was low for the three parameters: penetration: 68 %, aspiration: 75 %, pharyngeal residue: 67 % [6]. Clearly, exam type is a significant variable that is influencing clinician impressions of swallowing events and deserves a closer look using tightly controlled stimuli of simultaneous studies (MBS and FEES done at the same time). It would be of value to investigate other parameters using simultaneous studies, such as swallowing anatomy and location of residue. Another factor that has gone unmentioned is clinician attitude toward exam type. After all, the perceived challenges of the clinicians play a large role in their impressions. The goal of this study was to explore these undocumented parameters of FEES and MBS evaluations using archived simultaneous studies. More specifically, this study had four aims:
-
(1)
Report which pharyngeal and laryngeal swallowing anatomy can be seen on FEES and MBS evaluations. Although seemingly obvious, to our knowledge, this has not been systematically studied and published. The oral and the esophageal phases of swallowing are not visible on a FEES and are best viewed on an MBS evaluation. Therefore, this study aimed to only investigate the swallowing anatomy could presumably be seen on either evaluation.
-
(2)
Identify locations where pharyngeal residue can be seen on MBS and FEES evaluations. The presence of residue may outline or obstruct structures, which may be viewed differently from each evaluation type.
-
(3)
Compare differences of residue severity between exam types. While this replicates, in part, extant literature [6, 7, 16], this study aimed to take a closer look at residue by documenting the different definitions of residue severity, as reported by clinicians. It was predicted, based on the literature, that clinicians would judge FEES more severely than MBS studies.
-
(4)
Finally, highlight clinician attitudes toward the two evaluations in a qualitative fashion to shed light on clinician-perceived biases or challenges.
Materials and Methods
Subjects
The subjects were a convenience sample of volunteers from a pool of clinician participants at FEES courses taught by the second author. The course consists of 2 full days of lecture (about swallowing evaluations with emphasis placed on FEES), discussion, and hands-on experience with FEES. Clinicians were sampled across 5 courses, including the standard and advanced courses, occurring between January 2014 and January 2015. The first two courses were used as pilot data for questionnaire refinement; the next 3 courses provided the data reported in this study. An Institutional Review Board reviewed this study and deemed it to be exempt as survey research that used de-identified archived videos. The inclusion criteria for participation were (1) medical professionals who work with patients with dysphagia in any context (SLP, MD, or related field) and (2) the ability to understand and follow oral and written instruction in English. The exclusion criterion was any self-identified students.
Materials
Questionnaire
The questionnaire asked about pharyngeal and laryngeal anatomy, pharyngeal residue location and amount, how to define residue amount, and challenges of each exam (see Appendix in Electronic Supplementary Material). It is a given that the oral and the esophageal phases of swallowing are not visible on a FEES and are best viewed on an MBS evaluation. Therefore, the questionnaire asked about anatomy that could only be reasonably viewed on each exam. Fifteen structures/locations were selected by the authors as anatomy that could be seen on both FEES and MBS. The questionnaire went through 3 preliminary drafts that were reviewed by members of the second author’s research lab. To ensure clarity, it was pilot tested across 88 clinicians from 2 FEES courses.
No existing questionnaires or instruments were discovered that could be used or adapted for this study’s purpose. Therefore, the questionnaire was developed with rigor but was not formally validated. Most of the questions were closed-ended, although the questionnaire contained three open-ended questions asking clinicians to qualitatively describe exam differences. Pilot testing was effective at addressing interpretation problems and leading questions. An Appendix with labeled anatomy on both fluoroscopy and endoscopy views accompanied the questionnaire in order to prevent a lack of response based on uncertainty of anatomy (see Electronic Supplementary Material). Portney and Watkins note that in questionnaire development, an option for “other” or “unsure” should be included, but for this purpose, a forced choice seemed more appropriate [ [17], p. 334].
Videos
A total of 6 de-identified archived videos were used for this study. To address the question of swallowing anatomy, the investigators presented 1 FEES video and 1 MBS video of patients with unaltered anatomy. These videos did not contain any bolus presentation or any swallows, as the goal was for clinicians to identify swallowing anatomy without the influence of food or liquid boluses. Each video was about 10 s long showing normal anatomy at rest, while the patient breathed comfortably.
To address the residue question, two simultaneous studies of the best quality were selected from the archives of the second author. The simultaneous studies had been performed on patients with dysphagia and unaltered anatomy. The two simultaneous studies were edited into four videos: (1) Patient 1 MBS and (2) Patient 1 FEES demonstrating one swallow of 5 mL of applesauce and (3) Patient 2 MBS and (4) Patient 2 FEES demonstrating one swallow of 5 mL of applesauce. The applesauce boluses contained 40 % barium contrast as well as green food dye to assist with visualization on the FEES. The videos were edited to show only the first swallow with no secondary swallows. The videos ranged from 20 to 30 s long, each with at least 5 s after the swallow to observe residue. For comparison purposes, the authors subjectively labeled the overall amount of residue to be moderate for Patient 1 and mild for Patient 2. Aspiration was not investigated for this study, as it has been elsewhere, but the authors agreed that no aspiration was seen on any video. The MBS videos were digitally recorded at 30 frames per second and saved to an electronic file. All FEES procedures were performed using a Pentax laryngoscope. The FEES and MBS recording devices were manually rigged to record in sync to the same analog file, which was the best available recording option at that time.
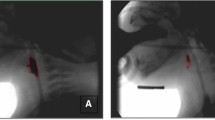
In a simultaneous study, one swallow is documented at the same time by two evaluations (an MBS video and FEES video concurrently recording), resulting in two videos of one swallow (see Fig. 1). The use of simultaneous studies was critical to this study for validity purposes: the FEES video shows the exact same swallow that is documented by the MBS. In other words, they allow for a comparison of differences between the evaluations knowing that what was seen independently on each evaluation represents the same event.
Procedures
On the second morning of the FEES course before the lectures began, participants were asked to volunteer for a lunchtime research session. The data collection was intentionally conducted near the end of the course so that the participants would have already received an anatomy review and background information about both instrumental evaluations, but no discussion directly contrasting the two.
For the study session, participants sat in an auditorium. The questionnaires were distributed, and the directions were read aloud, verbatim. The participants were instructed to refer to the Questionnaire’s Appendix as a means to account for any lack of anatomy knowledge (please refer to Electronic Supplementary Material). A few clarifications were made using the visual aids in the Questionnaire’s Appendix (i.e., pharyngeal walls include both lateral walls and the posterior wall, and the laryngeal rim might also be known as the lip the vestibule). The participants were asked to indicate only one rating of pharyngeal residue severity from each video clip and not choose more than one. If this occurred, the more severe rating was selected. A definition of “severity of pharyngeal residue” was purposely not provided. Participants were asked to use their prior experiences and their own personal definitions to answer that question; of note, the FEES course lectures had not reviewed formal residue definitions or ratings. The participants were blinded to the fact that the videos were simultaneous studies.
Once the questionnaire was reviewed, the FEES anatomy video and the MBS anatomy video were played individually in a randomized order and projected from a high-resolution display projector onto a 9 × 12 foot screen at the front of the classroom. Next, the 4 videos with bolus swallows (patient 1 FEES video, patient 2 FEES video, patient 1 MBS video, patient 2 MBS video) were played individually in a randomized order chosen by a coin flip. The videos were played without the sound and with the classroom lights dimmed to optimize the video quality. Each video was played a minimum of two times and repeated as many times as requested in regular speed, slow motion, and stopped at requested times. Participants were told the bolus consistency and size, but no other feedback was provided. The entire session lasted no longer than 45 min. Upon completion of the videos, participants were asked to hand in their questionnaires. They were then told that the videos they viewed were simultaneous studies and their impressions were discussed.
Statistical Testing
The data were tallied into frequencies or entered as descriptive responses in a Microsoft Excel spreadsheet. Descriptive responses were analyzed in a qualitative manner in 2 cycles of coding for major themes [18]. A report was generated to highlight and tally the coded themes that emerged. To compare frequency counts, a Chi-square test (x 2 test of independence) was used. When the expected frequency in a cell was less than 5, a Fisher’s exact test was used instead. Statistical testing was performed on SAS (version 9.3; SAS Institute Inc. Cary, NC, USA), and a significance value of p < 0.05 was used.
Results
A total of 55 clinicians were surveyed across three FEES courses (n = 17 in June, n = 17 in August, n = 21 in October). Years of FEES experience ranged from 0 to 14 (average 1.16 years ± 2.9); years of MBS experience ranged from 0 to 26 (average 6.34 years ± 6.5).
Swallowing Anatomy
The majority of clinicians indicated that the base of tongue, valleculae, epiglottis, and trachea were seen on both the FEES and MBS anatomy videos. These four anatomical areas did not have a statistical difference in the proportion of yes/no responses for each evaluation type. However, all other locations had a statistically significant difference in the number of yes/no responses between the FEES and MBS view (see Table 1).
Residue
Patient #1
Figure 2 demonstrates the 10 locations (out of 15 choices) for which clinicians indicated significantly more residue on the FEES video (*) than on the MBS video for the simultaneous study of Patient 1. The residue results of Patients 1 and 2 were analyzed separately because the videos displayed different amounts of residue in different locations.
Patient #2
Figure 3 demonstrates the locations where residue was noted on the FEES and MBS videos for Patient 2. There were 4 locations (*) for which clinicians noted significantly more residue on the FEES video than on the MBS video for this swallow. A fifth location (the laryngeal rim*) had significantly more ratings for residue in the MBS view.
Global Impression
Clinicians were asked, “Overall, how much residue did you see?” The results of the global impression are shown in Fig. 4a and b. The distribution of ratings was significantly different across the FEES and MBS ratings for both patients (for patient 1: χ2 = 20.05, p < 0.0001; for patient 2: χ2 = 7.52, p = 0.006). Clinicians’ impressions of FEES residue severity ranged from mild to severe for Patient 1’s FEES video and from mild to moderate–severe for Patient 2’s FEES video. Similarly, clinicians’ impressions of MBS residue severity ranged from mild to moderate–severe for both Patient 1 and Patient 2’s MBS videos.
a The number of clinicians who rated overall impression of pharyngeal residue in Patient 1’s FEES and MBS videos. *Significant discrepancies across the ratings scales between FEES and MBS categories at p < 0.05 b The number of clinicians who rated overall impression of pharyngeal residue in Patient 2’s FEES and MBS videos. *Significant discrepancies across the ratings scales between FEES and MBS at p < 0.05
Scale Definitions
Clinicians reported a variety of definitions and descriptors for residue. The majority (20.3 %, n = 13) reported that they defined the amount of residue based on the percentage of a cavity or an area filled or covered by residue. Almost as many clinicians (18.8 %, n = 12) reported using the percentage of ingested bolus remaining or left behind, and 17.2 % (n = 11) gave unclear definitions such as “trace” or “10 %.” Table 2 provides a summary of emergent themes across the clinicians’ definitions.
Challenges
Finally, clinicians were asked to report the challenges of each exam, the themes of which are summarized in Tables 3 and 4. Clinicians reported 83 challenges of MBS exams that fit into 10 themes. The most-mentioned MBS challenge (13.3 %, n = 11) was the theme of poor visual quality/black and white images. Examples of clinician responses were “sometimes the picture is hard to read,” “structures are hazy,” and “shadows.” Other responses (n = 9) related to not being able to visualize surface anatomy and function, especially for laryngeal structures (“limited view of the TVF function”). A theme of not being able to differentiate structures appeared 8 times (“not being able to visualize structures unless they become coated”), and difficulty locating residue (n = 8, “seeing trace residue” and “where specifically is the residue?”). Some responses concerned limitations of the lateral view (n = 7, “not being able to determine L/R location of residue”) and positioning challenges (n = 7, “patient movement” and “due to positioning limitations, worse view of the tracheal entrance”). Another theme of MBS challenges was radiation concerns causing limited evaluation time (7.2 %, n = 6).
Clinicians reported 76 challenges of FEES that fit into 12 themes. The top-reported FEES challenge (31 %, n = 18) was poor visualization at the height of the swallow during white out (the brief but intense white glare that obscures the view at maximal contraction of the swallow), with responses such as “worse ability to view during the swallow” and “the whiteout period.” Other frequently reported challenges were poor visualization of other structures and movements (n = 8, “can’t see passage of bolus into esophagus” and “oral prep phase”), and difficulty interpreting the exam (n = 5, “sometimes hard to judge” and “inferring results”).
Discussion
The present study was a preliminary attempt to describe how clinician impressions of swallowing could differ depending on the type of instrumental swallowing evaluation (FEES vs. MBS). Ample previous literature has discussed the sensitivity and specificity of each evaluation, but only 5 studies have used simultaneous FEES and MBS evaluations [6, 7, 16, 31, 32]. This study aimed to explore simultaneous evaluations and elaborate on evaluation influences by systematically exploring clinician report of (1) what swallowing anatomy could be seen, (2) pharyngeal residue location, (3) pharyngeal/laryngeal residue amount and definition, and (4) attitude toward the two evaluations. The results suggest that the type of swallowing evaluation is indeed an influential factor in clinician impressions of dysphagia that should not be ignored in clinical and research settings.
First, when choosing from swallowing anatomy that could be seen on either exam, clinicians reported that only 4 structures could be seen with the same frequency across endoscopic and videofluoroscopic views: the base of tongue, valleculae, epiglottis, and trachea. The 11 other anatomical structures/spaces were not seen with the same frequency between the two evaluations. This may reflect a lack of anatomical competency and highlight the need for better training in identifying important swallowing structures. Other studies have highlighted the importance of adequate training of clinicians in swallowing evaluation [19, 20]. However, it might also suggest that the majority of these swallowing structures are better visualized on a FEES. For instance, about 93 % of clinicians indicated that they saw the interarytenoid space on the endoscopic view, but only 38 % of clinicians reported that they saw it in the videofluoroscopic view. Similar discrepancies reporting better visualization on FEES were also noted for the posterior pharyngeal wall, lateral channel, piriform sinuses, and laryngeal structures. These results suggest that endoscopy may be the better tool to identify these swallowing structures and support the prior claims of experts in the field [1, 8, 9]. An article in Turkish found similar results of better visualization of “internal anatomy” on FEES [21], but a full-text English version could not be obtained. If pharyngeal or laryngeal anatomy is a considerable factor in an evaluation, then FEES should be the preferred evaluation. In routine instrumental exams, clinicians must identify the swallowing structures to describe and assess physiology. Proper identification becomes even more important when determining swallow safety including visualization and detection of secretions in the vestibule upon entry, an important advantage to identify those at risk of aspiration on their secretions. Although previous reviews have suggested it [1], to our knowledge, this is the first study to systematically report on this significant advantage of pharyngeal and laryngeal visualization of anatomy. It is worth repeating that the oral and esophageal phases are best assessed on MBS evaluations and they were not included in this investigation for that very reason.
Second, this study asked in which locations could pharyngeal residue be seen, because residue location has been associated with aspiration risk [22, 23]. The present study found that across the 2 simultaneous studies, pharyngeal residue was seen in more locations on the FEES than on the MBS. This could be interpreted to mean that not only is FEES more sensitive at detecting pharyngeal residue, but that residue might go undetected on an MBS view. This agrees with other results that FEES allows for better visualization of the bolus within the pharynx and larynx [5, 6, 21], lending support to why FEES has been called the “first choice” for swallowing evaluations in Europe [19]. Noticing residue within the larynx is a critical diagnostic advantage in that it identifies patients who are at higher risk for aspiration. This advantage becomes even more critical in the acutely ill populations who need to be evaluated accurately and reliably for detection of aspiration at bedside. It would be a worthy investigation to repeat this study design with videos that demonstrate aspiration.
The third aim was to describe the differences in clinicians’ judgment of residue severity. Impressions of residue differed significantly depending on the evaluation type. More specifically, FEES impressions were more severe than MBS impressions, which is in concurrence with previous literature using simultaneous evaluations [6, 7, 16]. Another finding was that clinician ratings demonstrated a great range of severity, in one case from mild to severe on one video. This occurred for both MBS or FEES videos. It is concerning that clinicians interpreted the residue amount so differently. Such differences in interpretations and low inter-rater reliability likely occur in clinical practice everyday, putting patients at risk for varying diagnoses and treatment recommendations. Recent studies have documented excellent inter-rater agreement on FEES in ratings of penetration and aspiration [24, 25], but evidence is sparse regarding agreement of residue ratings. The few studies that have investigated the dilemma of rating residue relied on general agreement or consensus between expert judges as the ‘gold standard’ to determine how much residue was actually present [26, 27]. The gold standard for rating residue on FEES remains elusive.
It is assumed that clinicians vary in their impressions of residue because they define it differently for various reasons such as training and experience. The results of this study verify that clinicians use their own internalized definitions of residue severity. In fact, when asked to describe how they defined residue, this sample of clinicians gave definitions that fit into 8 different themes, many of which were vague. They were unsure and unclear about how to rate residue. These results raise two points of concern: (1) clinician interpretations of residue are subjective and (2) their impressions of residue are influenced by the type of evaluation used (likely to be more severe on FEES). As such, instrumental evaluations of pharyngeal residue present a diagnostic dilemma that needs to be addressed, especially considering the potential impact that varying interpretations have on patient safety. Patients should receive the same clinical recommendations regardless of who rated the evaluation or what type of evaluation was employed. Possible solutions are better competencies, better training, and a standardized approach. Research is only just now attempting to standardize perceptual measurement of pharyngeal residue. While the phrase ‘standardize perceptual measurement’ may seem contradictory, other areas such as perceptual ratings of voice quality ratings have done so and subsequently increased the inter-rater agreement [28]. Two recent scales have been designed to rate impressions of pharyngeal residue on endoscopy [26, 27]. An interesting continuation of the present study would be to have clinicians rate videos using these published scales, in hopes that there would be more consistent impressions.
Finally, clinicians highlighted the challenges of each evaluation. Many did not like the visual quality of MBS studies (hazy structures and black and white images), and the white-out period was the most-reported challenge of the FEES exam. These results could be usefully incorporated into training and teaching clinicians how to navigate around these issues. For instance, ‘lack of experience’ was a common response to FEES challenges. This is likely due to sampling clinicians who were attending a FEES course, but should also be addressed as a pertinent factor in FEES training. In the same way, many clinicians reported difficulty on MBS studies in identifying structures. Even after hearing anatomy lectures as part of the FEES course and even with an Appendix labeling the anatomy, this sample of clinicians was still unsure of the anatomy in the videos. More robust training is necessary to ensure adequate knowledge of clinicians who are performing instrumental evaluations of dysphagia.
As of this writing, no literature could be found highlighting clinician-described challenges of instrumental evaluations for dysphagia. The results from the current study may be useful in informing educators what should be addressed for clinical competency and technique. For example, while the white-out period was an often-reported disadvantage of FEES here and elsewhere [29], a useful technique is to change the endoscope’s lighting setting from automatic adjustment to the manual setting so that the period of white out is minimized, and the view of the epiglottis and larynx will be optimized immediately after white out. This may enable better assessment of epiglottic retroflexion on FEES, as it had for these authors. Further, research studies should consider the challenges documented by this study when designing research involving instrumental evaluations of dysphagia. Clinicians reported a challenge of a limited amount of time for MBS studies due to safety concerns about radiation exposure. Future study designs should consider this important limitation to ensure capture of all the necessary information while avoiding lengthier evaluations.
This study was a preliminary investigation on a convenience sample of clinicians and, as such, there are several limitations. First and foremost, this convenience sample of clinicians at a FEES course may have contained bias. However, it was a unique opportunity to collect feedback from a variety of clinicians from geographically and clinically different settings. Recruiting participants from one or two sites would have also presented bias. Every effort was made to reduce any influence of one exam over the other: both evaluations were covered in lecture and a labeled Appendix of both views was provided. It is also possible that there was new learning bias that occurred in FEES impressions, but this could have been balanced by clinicians’ experiences with MBS. Further, very few clinicians are experienced in both FEES and MBS exams, so this design, while not perfect, capitalized on this type of clinician. The study’s questionnaire could be a threat to internal validity in that it did not undergo reliability testing. However, it did undergo 3 drafts and was pilot tested twice in the same FEES course setting. Internal validity is threatened in other ways: variability in clinician experience, preselected anatomy choices, and using only a select few videos for presentation. The limitations of the simultaneous evaluations should also be acknowledged: MBS videos only in the lateral view, and the visual quality of both the MBS and FEES videos was reduced due to the archived quality. However, they were recorded onto the same device that was the highest quality available at that time. Figure 1 represents the quality of the videos, and the authors felt they were appropriate to use as stimuli. Additionally, the range of dysphagia was limited, and no aspiration was seen in these videos. Ideally, many more simultaneous videos would have been used as stimuli. But due to their rarity (for equipment, clinical, and cost reasons), the archived videos were used based on the authors’ preference to use old simultaneous videos instead of new sequential videos that were not simultaneous. Future research should strive to use simultaneous evaluations when making comparisons to eliminate confounding variables. Further, there was no way to verify the ‘truth’ behind the videos, for example, exactly how much residue was present? For MBS studies, standardized and objective measures have progressed greatly [19, 30], but the absence of a gold standard of continues to be a problem, especially for FEES.
Despite the limitations, multiple strengths support this preliminary data. This study used simultaneous videos, which allowed for a precise comparison of the two views without internal validity issues of sequential evaluations. Another strength is the novelty of the research questions. A plethora of articles have discussed logistical differences (bedside evaluation for FEES vs. transport of the patient to a radiology suite for a MBS) and safety concerns (exposure to radiation, contraindications of endoscopy) between FEES and MBS evaluations that need not be duplicated here. And others have investigated differences between the two evaluations such as penetration-aspiration scale scores, effect of bolus order, and assessment of maneuvers [16, 31, 32]. But few to none have considered the simplest components, like visualization of anatomy and clinician challenges. These additions could enhance the knowledge of and indications for FEES and MBS evaluations.
Conclusion
In conclusion, clinician impressions of several swallowing parameters were influenced by evaluation type. Clinicians visualized more pharyngeal and laryngeal structures and detected residue in more locations on FEES than on MBS evaluation. Clinicians also provided more severe impressions of residue amount on FEES. This result has implications for informing clinicians’ choice of exam and also for informing possible future scales that may attempt to rate parameters such as residue on FEES, MBS studies, or both. Lastly, clinicians should be aware of the potential influence of evaluation type, likely to be a more severe impression on FEES, when making dysphagia diagnoses and measuring outcomes.
References
Kidder T, Langmore S, Martin B. Indications and techniques of endoscopy in evaluation of cervical dysphagia: comparison with radiographic techniques. Dysphagia. 1994;9:256–61.
Aviv JE. Prospective, randomized outcome study of endoscopy vs. modified barium swallow in patients with dysphagia. Laryngoscope. 2000;100:563–74.
Langmore SE, Schatz K, Olsen N. Endoscopic and videofluoroscopic evaluations of swallowing and aspiration. Ann Otol Rhinol Laryngol. 1991;100:678–81.
Wu CH, Hsiao TY, Chen JC, Chang YC, Lee SY. Evaluation of swallowing safety with fiberoptic endoscope: comparison with videofluoroscopic technique. Laryngoscope. 1997;107:396–401.
Leder SB, Sasaki CT, Burrell MI. Fiberoptic endoscopic evaluation of dysphagia to identify silent aspiration. Dysphagia. 1998;13:19–21.
Rao N, Brady S, Chaudhuri G, Donzelli J, Wesling M. Gold standard? Analysis of the videofluoroscopic and fiberoptic endoscopic swallow examinations. J App Res. 2003;3:89–96.
Kelly AM, Leslie P, Beale T, Payten C, Drinnan MJ. Fibreoptic endoscopic evaluation of swallowing and videofluoroscopy: does examination type influence perception of pharyngeal residue severity? Clin Otolaryngol. 2006;31(5):423–5.
Langmore SE. Endoscopic evaluation of oral and pharyngeal phases of swallowing. GI Motility. 2006; online 16 May. doi:10.1038/gimo28.
Brady S, Donzello J. The modified barium swallow and the functional endoscopic evaluation of swallowing. Otolaryngol Clin North Am. 2013;46(6):1009–22.
Nordally SO, Sohawon S, DeGieter M, Bellout H, Verougstraete G. A study to determine the correlation between clinical, fiber-optic endoscopic evaluation of swallowing and videofluoroscopic evaluations of swallowing after prolonged intubation. Nutr Clin Pract. 2011;26(4):457–62.
Willging JP, Miller CK, Hogan MJ, Rudolph CD. Fiberoptic endoscopic evaluation of swallowing in children: a preliminary report of 100 procedures. Dysphagia. 1996;11(2):162.
Wu CH, Hsiago TY, Chen JC, Chang YC, Lee SY. Evaluation of swallowing safety with fiberoptic endoscope: comparison with videofluroscopic technique. Laryngoscope. 1997;107:396–401.
Kaye GM, Zoroqitz RD, Baredes S. Role of flexible laryngoscopy in evaluating aspiration. Ann Otol Rhinol Laryngol. 1997;106:705–9.
Perie S, Laccourreye L, Flahault A, Hazebroucq V, Chaussade S, St Guily JL. Role of videoendoscopy versus modified barium swallow in patients with dysphagia. Laryngoscope. 2000;110:563–74.
Madden C, Fenton J, Hughes J, Timon C. Comparison between videofluroscopy and milk-swallow endoscopy in the assessment of swallowing function. Clin Otolaryngol. 2000;25:504–6.
Kelly AM. Assessing penetration and aspiration: how do videofluoroscopy and fiberoptic endoscopic evaluation of swallowing compare? Laryngoscope. 2007;117:1723–7.
Portney LG, Watkins MP. Foundations of clinical practice: applications to practice. 3rd ed. Upper Saddle River: Prentice Hall Health; 2009 (ISBN: 9780131716407).
Saldaña J. The coding manual for qualitative researchers. Thousand Oaks: Sage; 2012.
Martin-Harris B, Brodsky MB, Michel Y, Castell DO, Schleicher M, Sandidge J, Maxwell R, Balir J. MBS measurement tool for swallow impairment—MBSImp: establishing a standard. Dysphagia. 2008;23:392–405.
Hind JA, Gensler G, Brandt DK, et al. Comparison of trained clinician ratings with expert ratings of aspiration on videofluoroscopic images from a randomized clinical trial. Dysphagia. 2009;24(2):211–7. doi:10.1007/s00455-008-9196-6.
Gerek M, Atalay A, Cekin E, Ciyiltepe M, Ozkaptan Y. The effectiveness of fiberoptic endoscopic swallow study and modified barium swallow study techniques in diagnosis of dysphagia. Kulak Burun Bogaz Ihtis Derg. 2005;15(5–6):103–11.
Perlman AL, Grayhack JP, Booth BM. The relationship of vallecular residue to oral involvement, reduced hyoid elevation, and epiglottic function. J Speech Hear Res. 1992;35:734–41.
Molfenter SM, Steel CM. The relationship between residue and aspiration on the subsequent swallow: an application of the Normalized Residue Ratio Scale. Dysphagia. 2013;29:494–500.
Butler SG, Markley L, Sanders B, Stuart A. Reliability of the penetration aspiration scale with flexible endoscopic evaluation of swallowing. Ann Oto Rhinol Laryngol. 2015;124(6):480–3.
Hey C, Pluschinski P, Pajunk R, Almahameed A, Girth L, Sader R, Stöver T, Zaretsky Y. Penetration–aspiration: is their detection in FEES reliable without video recording? Dysphagia. 2015;30:418–22.
Neubauer PD, Rademaker AW, Leder SB. The Yale pharyngeal residue severity rating scale: an anatomically defined and image-based tool. Dysphagia. 2015;. doi:10.1007/s00455-015-9631-4.
Kaneoka A, Langmore SE, Krisciunas GP, Field K, Scheel R, McNally E, Walsh MJ, O’Dea MB, Cabral H. The Boston residue and clearance scale: preliminary reliability and validity testing. Folia Phoniatrica et Logopaedica. 2013;65:312–7.
Zraick RI, Kempster GB, Conner NP, Klaben BK, Bursac Z, Thrush CR, Glaze LE. Establishing validity of the consensus auditory-perceptual evaluation of voice (CAPE-V). Am J Speech-Lang Pathol. 2011;20:14–22.
Nacci A, Ursino F, La Vela R, Matteucci F, Mallardi V, Fattori B. Fiberoptic endoscopic evaluation of swallowing (FEES): proposal for informed consent. Acta Otorhinolaryngol Ital. 2008;28(4):206–11.
Pearson WG Jr, Molfenter SM, Smith Z, Steele CM. Image-based measurement of post-swallow residue: the normalized residue ratio scale. Dysphagia. 2013;. doi:10.1007/s00455-012-9426-9.
Jung SH, Kim J, Jeong H, Lee SU. Effect of the order of test diets on the accuracy and safety of swallowing studies. Ann Rehabil Med. 2014;38(3):304–9.
Fuller SC, Leonard R, Aminpour S, Belafsky PC. Validation of the pharyngeal squeeze maneuver. otolaryngol. Head Neck Surg. 2009;140:391–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pisegna, J.M., Langmore, S.E. Parameters of Instrumental Swallowing Evaluations: Describing a Diagnostic Dilemma. Dysphagia 31, 462–472 (2016). https://doi.org/10.1007/s00455-016-9700-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-016-9700-3