Abstract
The epithelial monolayer of the intestine is a selective barrier permitting nutrient and electrolyte absorption yet acting to protect the underlying tissue compartments and cellular components from attack and infiltration by antigens, bacteria and bacterial products present in the lumen. Disruption of this barrier has been associated with inflammatory bowel disease (IBD). The adherens junction (AJ), together with tight junctions (TJ) and desmosomes, form an apical junction complex that controls epithelial cell-to-cell adherence and barrier function as well as regulation of the actin cytoskeleton, intracellular signalling pathways and transcriptional regulation. Numerous studies and reviews highlight the responses of TJs to physiological and pathological stimuli. By comparison, the response of AJ proteins, and the subsequent consequences for barrier function, when exposed to the IBD inflammatory milieu, is less well studied. In this review, we will highlight the roles and responses of the AJ proteins in IBD and provide suggestions for future studies. We will also consider recently proposed therapeutic strategies to preserve or restore epithelial barrier functions to prevent and treat IBD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The epithelial monolayer of the intestine functions as a vital barrier protecting the underlying tissue compartments and cellular components from exposure to antigens, bacteria and bacterial products in the lumen. The adherens junction (AJ), together with tight junctions (TJ) and desmosomes, form an apical junction complex (AJC) that controls epithelial cell-to-cell adherence and barrier function as well as regulation of the actin cytoskeleton, intracellular signalling pathways and transcriptional regulation. Numerous studies and reviews highlight the responses of AJC components to physiological and pathological stimuli. However, most have focused on the role of the TJ proteins in epithelial cells; for example, the induction of endocytosis by proinflammatory cytokines such as interferon-gamma (IFN-γ) (reviewed in Utech et al. 2010). Chronic inflammatory bowel diseases [IBD; Crohn’s disease (CD) and ulcerative colitis (UC)] are characterised by prolonged cytokine stimulation in the gut, which is known to induce endocytosis of a number of TJ proteins (Bruewer et al. 2003; Prasad et al. 2005; Weber and Turner 2007; Zeissig et al. 2007). By comparison, the response of AJ proteins to the inflammatory milieu to which they are exposed is less well studied. In this review, we will highlight the roles and responses of the AJ proteins in epithelial cells when exposed to the inflammatory conditions associated with IBD. We will provide perspectives for future studies and consider recently proposed therapeutic strategies to preserve or restore epithelial barrier functions to prevent and treat IBD.
The structure and function of adherens junction
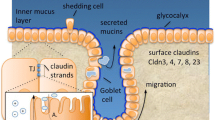
AJs are located in the apical part of the lateral plasma membrane of a cell immediately inferior to the TJ. The structure of the AJ is summarised in Fig. 1. The transmembrane component of AJs, epithelial cadherin (E-cadherin), is a single-pass glycoprotein that belongs to the classical cadherin family of Ca2+-dependent adhesion proteins (Takeichi 1988). E-cadherin has characteristic extracellular cadherin repeat domains, which create homophilic trans-cadherin interaction with the cadherin molecules of the neighbouring cell (Nose et al. 1990). The exact mechanism of this cell–cell trans-cadherin interaction has been a topic of debate for some time and has yet to be fully resolved.
The membrane-bound AJ complex in health and intestinal inflammation. The membrane-bound AJ is shown in the centre. The extracellular domain of E-cadherin binds to E-cadherin molecules on adjacent cells. The intracellular domain binds to both p120-catenin and β-catenin at separate sites forming an armadillo repeat domain. The cadherin–β-catenin–α-catenin complex interacts with actin and actin-associated proteins as shown. In addition, afadin links transmembranous nectin to actin and actin-associated proteins via the AJ complex. During inflammation, a number of stress factors affect the AJ complex. The combination of pro-inflammatory cytokines IFNγ and TNFα causes a greater proportion of cellular E-cadherin to be cytoplasmic rather than membranous, whereas S1P has the opposite effect. JAK3 inhibits a similar process involving β-catenin. CD97 has been shown to exert a protective effect against the dissipation of the entire AJ complex. Oxygen radicals, PDGF and calcium depletion all increase internalisation of AJ proteins for degradation via endocytosis. Tissue hypoxia, a common consequence of inflammation, causes induction of CK isoenzymes in a HIF2-dependent manner, which co-localise with AJ proteins and enhance E-cadherin function through myosin II ATPase function. AJ adherens junction, IFNγ interferon gamma, TNFα tumour necrosis factor alpha, S1P sphingosine-1-phosphate, JAK3 janus kinase 3, HIF2 hypoxia-inducible factor 2, PDGF platelet-derived growth factor, CK creatine kinase, ADIP afadin DIL domain-interacting protein, LM07 LIM domain only
Intracellularly, the cytoplasmic component of E-cadherin binds to p120-catenin, also known as γ-catenin, and β-catenin (Nagafuchi and Takeichi 1989; Ozawa et al. 1989). These proteins comprise characteristic amino acids repeat folded to form a rigid elongated, armadillo repeat domain. P120-catenin binds to the juxtamembrane domain (JMD) of the E-cadherin adjacent to the cell membrane whereas β-catenin binds at a catenin-binding domain (CBD) located further down along the tail of E-cadherin (Aberle et al. 1994; Yap et al. 1998). Both JMD and CBD are thought to be involved in the regulation of the adhesive property of the E-cadherin. P120-catenin is believed to prevent internalisation and proteolytic degradation of cadherin as well as being responsible for stabilisation of cadherin within the cell membrane (Davis et al. 2003; Xiao et al. 2003). On the other hand, β-catenin was believed to provide a link to α-catenin forming the cadherin–β-catenin–α-catenin complex (Aberle et al. 1994; Pokutta and Weis 2000) which in turn interacts with actin and actin-associated proteins such as α-actinin, vinculin, and formin-1. This hypothesis has been questioned, and there is evidence that α-catenin does not bind to the cadherin–β-catenin complex and actin filaments (Drees et al. 2005). A recent study suggests that the cadherin–catenin complex may act as a mechanical adhesion stress sensor that sends signals to actin and actin-associated proteins regulating the structural integrity of the cell (Michael and Yap 2013).
One of the main functions of AJs is to provide the dynamic adhesive connection between epithelial cells. Its interaction with actin and actin-associated proteins through bidirectional signalling pathways is believed to create a dynamic protein system that facilitates and regulates cell-to-cell integrity as well as the overall tissue structure which allows migration and dispersal of cells (Han and Yap 2012). Another function of AJs is an involvement in gene regulation: catenins such as p120-catenin and β-catenin are known to interact with transcriptional machinery in the nucleus acting as transcriptional co-factors (Perez-Moreno and Fuchs 2006). A phosphorylation-dependent cadherin–catenin complex could recruit or release catenins, in turn altering the free cytoplasmic availability of the catenins and affecting the transcription of genes (Daugherty and Gottardi 2007). One of the best examples is β-catenin and the transcription factor T cell factor/lymphoid enhancer factor (TCF/LEF) in the Wnt pathway, which promotes trancription of numerous genes involved in cell proliferation and differentiation (Nelson and Nusse 2004).
In addition, the cystic fibrosis transmembrane conductance regulator (CFTR) is localised at the apical membrane of epithelial cells and a link between CFTR and epithelial cell polarity has long been recognised. CFTR is also required for the organisation and integrity of TJs. CFTR was shown recently to interact with a novel intracellular junction protein AF-6/afadin, which interacts with the immunoglobulin-like nectin cell adhesion molecules at AJs (Sun et al. 2014). Nectins form AJs in cooperation with cadherins interacting in trans with each other via their extracellular regions and with afadin through their cytoplasmic tails. Afadin links nectins to the actin cytoskeleton (Takai and Nakanishi 2003; Harris and Tepass 2010; Kurita et al. 2011). As a consequence of the E-cadherin-based AJs and cell–cell adhesion organisation, the afadin/nectin interaction plays a role in the regulation of cellular activities, such as directional motility and proliferation (Takai and Nakanishi 2003).
The relationship between adherens junction and inflammatory bowel disease
Idiopathic IBD encompasses UC and CD, and is associated with recurrent episodes of chronic intestinal inflammation followed by resolution, mucosal healing and epithelial regeneration during periods of remission. Insights in understanding the pathophysiology of the disease are rapidly evolving, although the exact etiology remains poorly understood and a cure is elusive. IBD is a multifactorial disease with environmental and genetic contributions associated with dysbiosis of the intestinal microbiota and dysregulation of the mucosal immune system. Although the epithelial cells within the mucosal layers of the gut represent a physical barrier between the gut lumen and the underlying tissues, epithelial cells are shed continuously from the intestinal surface. The epithelium maintains the integrity of the epithelial barrier, in part, by reorganisation of TJ and AJ proteins (Watson and Hughes 2012). This process fills any gaps left following cellular ejection from the epithelium, but inflammation can cause serious disturbance of this dynamic process by a marked increase in rates of cell shedding compromising the maintenance of barrier function. The importance of this is highlighted by the consequences of abnormal intestinal permeability seen in CD (Peeters et al. 1997; Breslin et al. 2001) and UC (Schmitz et al. 1999).
As discussed above, cadherin is the main transmembrane glycoprotein localised in AJs and is fundamental in mediating cell-to-cell adhesions through the extracellular domain. In a classic experiment, Hermiston and Gordon (1995) used chimeric mice that expressed the dominant-negative cadherin in some intestinal epithelial stem cells to demonstrate the disruption of AJs and numerous other epithelial cell defects: incomplete polarisation; disruption to both the brush border and actin cytoskeleton; enhanced crypt–villus migration and premature apoptosis. In addition, the mucus layer was disrupted where underlying epithelial cells expressed the dominant negative cadherin; numerous adherent bacteria were present at these sites (Hermiston and Gordon 1995). These features mirror closely characteristics of IBD pathology. Interestingly, genome-wide association studies have identified multiple susceptibility loci for both CD (Duerr et al. 2006; Hampe et al. 2007; Wellcome Trust Case Control Consortium 2007; Barrett et al. 2008) and UC (Dubois and van Heel 2008; UK IBD Genetics Consortium et al. 2009; McGovern et al. 2010), which include members of the cadherin families, CDH1 and CDH3 (van Heel et al. 2003), that encode E-cadherin and p-cadherin, respectively. More recently, Elding and colleagues have confirmed this causal variant link to CDH1 and CDH3 (Elding et al. 2011), indicating that alterations in these genes may be important for the development of IBD.
Early ex vivo experiments performed on isolated crypts and epithelial cells from mucosa of UC, CD and control patients showed a perturbation of the epithelial barrier in IBD (Gibson et al. 1988, 1995). Protein expression of AJ molecules was investigated in a number of studies using human mucosal samples from IBD patients and healthy controls. For example, Doğan and colleagues showed strong expression of E-cadherin in normal and inflamed tissues, but a significant reduction of staining was observed in ulcer-associated cell lineage (UACL) cells bordering ulcerated mucosa in CD patients (Doğan et al. 1995). This cell lineage arises from mucosal stem cells and is associated with chronic inflammation and ulceration stimulating cell proliferation, regeneration and ulcer healing (Wright et al. 1990). The phenomenon of E-cadherin loss around ulcerated mucosa in both UC and CD was confirmed by subsequent studies (Karayiannakis et al. 1998; Demetter et al. 2000; Kucharzik et al. 2001; Jankowski et al. 1998; Gassler et al. 2001). Along the gastrointestinal tract, mucosal ulceration is linked with the migration of epithelial cells as part of a well-recognised repair mechanism to reconstitute the damaged epithelial barrier. Down-regulation of the E-cadherin–catenin complex during this process allows regenerating cells to differentiate and migrate over the denuded mucosal areas (Hanby et al. 1996). However, this absence of E-cadherin–catenin expression becomes a double-edged sword in the context of IBD when this loss of cell–cell adhesion further impairs the integrity of the mucosal barrier allowing the exposure of the luminal content to the underlying mucosal immune system which can lead to disease relapse particularly in CD (Wyatt et al. 1993; Arnott et al. 2000).
Other catenin proteins associated with AJs such as α-catenin (Gassler et al. 2001), p120-catenin (Karayiannakis et al. 1998) and β-catenin (Kucharzik et al. 2001) were found to be decreased around regions of ulceration in IBD mucosa compared to control samples. β-catenin cytoplasm and nuclear expression can distinguish the two subtypes of IBD as this protein was significantly increased in UC compared to CD (Soletti et al. 2013). β-catenin is a key player of the Wnt signalling pathway and its dysregulation is highly associated with colorectal cancer (CRC) and likely to play a role in IBD-associated CRC in particular in UC-CRC (Aust et al. 2001; Kinugasa et al. 2010; Shenoy et al. 2012). Whether this is due to activation of the canonical Wnt signalling pathway or if membrane-bound β-catenin plays a role is under debate. However, a recent study indicated that Wnt signalling activation could destabilise AJs to increase cytoplasmic β-catenin and further activate Wnt signalling (Vlad-Fiegen et al. 2012).
Despite being linked with both CD and UC by GWAS, expression levels of p-cadherin (CHD3) has not widely been investigated in IBD. P-cadherin is usually expressed in normal mammary epithelial cells and breast cancer tissue, although reports have shown aberrant expression at the early stages of abnormal colon crypt formation (Hardy et al. 2002). In ex vivo IBD samples, p-cadherin was up-regulated in both UC and CD mucosa compared to control mucosa, in particular in dysplastic regions of UC (Jankowski et al. 1998). In addition, p-cadherin’s promoter is activated by β-catenin in a LEF/TCF-independent manner (Faraldo et al. 2007). Therefore, it is tempting to speculate that p-cadherin is involved in UC-associated dysplasia, although more ex vivo and in vitro cell experiments are needed to elucidate the exact role for p-cadherin and how its dysregulation alters AJ function in early neoplastic changes in IBD.
Taken together, maintaining intestinal barrier integrity is crucial to preserve a selective barrier permitting nutrients and electrolytes yet protecting us against exposure to the external environment and avoiding infiltration of toxins and enteric flora. The next section will focus on the role of AJ proteins in intestinal inflammation in animal models and how inflammatory mediators can disrupt the homeostasis of these proteins.
Inflammatory mediators and adherens junctions
The AJ proteins play a vital role in the maintenance of epithelial cellular contact and adhesion. However, cellular adhesion in the gut is often compromised during episodes of inflammation, resulting in increased epithelial permeability. Acute inflammatory infiltrates of neutrophils, monocytes, macrophages, eosinophils and T cells within the gut wall characterise many intestinal disorders including those caused by infection and infarction. Non-resolution of intestinal permeability and non-removal of these infiltrates drives chronic inflammatory cascades. Therefore, it is necessary to understand not only the effects of inflammation on the AJ protein regulation that serves to maintain AJs and barrier function but also how non-resolution of intestinal permeability impacts on failure to achieve remission in IBD patients. An appreciation of the mechanism of endocytosis of these proteins during normal cellular homeostasis is fundamental. Endocytosis is the process used by cells to internalise macromolecules and particles into transport vesicles that are derived from the plasma membrane. This process is important for embryological development and tissue morphogenesis (Polak-Charcon et al. 1980; Miller and McClay 1997; Oda et al. 1998). Endocytosis also controls pathogen entry and the immune response, neurotransmission, intercellular communication, signal transduction, and cellular and tissue homeostasis. Defects in endocytosis have been linked to cancer and heart disease (Conner and Schmid 2003). In general, endocytosis mechanisms can be grouped into three classes: clathrin-mediated endocytosis, caveolar-mediated endocytosis and macropinocytosis. A comprehensive overview of these processes is beyond the scope of this article, but has been examined previously (Mukherjee et al. 1997; Utech et al. 2010). Physiological turnover involves constitutive internalisation of AJ proteins followed by either degradation by late endosomes or recycling to the membrane by recycling endosomes. Ongoing internalisation and processing does not compromise membrane integrity.
A number of studies have demonstrated that endocytosis of TJ proteins occurs under various physiological and pathological stimuli, both in vivo and in vitro, including inflammatory cytokines (Kevil et al. 1998; McNamara et al. 2001; Harhaj et al. 2002; Talavera et al. 2004; Wrobel et al. 2004). TJ protein loss increases membrane permeability and compromises membrane barrier function. Studies on AJ protein endocytosis are more limited, but increased AJ protein degradation does occur in intestinal epithelial cells exposed to calcium depletion (Ivanov et al. 2004a), treatment with platelet-derived growth factor (Harhaj et al. 2002) or oxygen radicals (Rao et al. 2002; Ivanov et al. 2004b).
Again, much is known about the effects of the inflammatory milieu on the distribution and function of TJ proteins, whilst there are far fewer studies examining the effects on AJs. One such study found no difference in E-cadherin or β-catenin expression in intestinal epithelial cells treated with IFN-γ. However, combined cytokine treatment of IFN-γ plus TNF-α resulted in reduced E-cadherin membrane localisation as assessed by immunofluorescence with unchanged total cellular E-cadherin levels (Table 1). This was accompanied by an increase in paracellular permeability in vitro, unrelated to apoptosis, as measured by trans-epithelial electrical resistance (TER) (Bruewer et al. 2003). Since IFN-γ and TNF-α are two of the dominant pro-inflammatory cytokines in IBD, and anti-TNF-α agents have clinical efficacy in the treatment of IBD, it is possible that this mechanism is not only relevant pathophysiologically but also therapeutically.
Another molecule implicated in the reduction of intestinal permeability associated with AJs and inflammation is CD97 (Table 1) (Becker et al. 2010), a member of the epidermal growth factor receptor transmembrane (EGF-TM7) family of adhesion G-protein coupled receptors (Yona et al. 2008). Transgenic mice overexpressing CD97 in intestinal epithelial cells are relatively protected from dextran sodium sulfate (DSS)-induced colitis, both in terms of clinical parameters and histological severity (Becker et al 2010). Mice exposed to azoxymethane/DSS-induced tumorigenesis also developed significantly fewer inflammation-associated CRCs. Interestingly, cytoplasmic segments of AJs were strengthened in CD97-overexpressing mice and characterised by dense arrangements into which thickened cytoskeletal microfilaments were anchored (Becker et al 2010). Conversely, CD97-deficient mice displayed much weaker AJs and showed dissipation of microfilaments, which appeared confined to AJs, with preservation of TJ function and TER. Moreover, CD97 was found to co-localise with both E-cadherin and β-catenin with little or no co-localisation with TJ proteins such as desmoplakin. CD97 appeared to be related to higher amounts of membranous β-catenin but not cytoplasmic or nuclear β-catenin, which were related to alterations in Akt/GSK-3β signalling. Interestingly, a genetic susceptibility locus for IBD has been identified close to the EGF-TM7 cluster on chromosome 19p13 (Rioux et al. 2000; Mathew and Lewis 2004). Therefore, CD97 appears to exert a protective effect on the conservation of AJ function, contrasting with the many other molecules studied which tend to act in the opposite manner. Further studies confirming this work and exploring the potentially therapeutic value of this pathway are merited.
Hypoxia is a key feature of inflamed tissue and hypoxic signalling mechanisms, including the hypoxia-induced factor (HIF) complex, have been implicated in intestinal epithelial barrier regulation during inflammation (Schofield and Ratcliffe 2004; Majmundar et al. 2010). A recent study examining epithelial junctional responses to hypoxia demonstrated creatine kinase (CK) metabolism as a distinctive downstream target of HIF-2 in Caco-2 intestinal epithelial cells, using ChIP analysis (Glover et al. 2013). CK isozymes were increased at both the mRNA and protein levels, and were inducible in a HIF-2-dependent fashion. These same CK isozymes (CKM, CKB and CKMT1A) co-localised with AJs and cadherin proteins, and were found to play a role in myosin II ATPase function, known co-ordinators of E-cadherin-dependent AJ utility (Table 1). HIF-2-deficient cells displayed increased intestinal permeability (with increased TER), and CK inhibition was found to impair epithelial barrier recovery during calcium switch. Finally, murine colitis induced by administration of DSS led to greater intestinal permeability in HIF1β knockout mice compared to WT mice, and was associated with a more severe clinical colitis picture. The hypoxic environment generated by inflammation, therefore, may independently be responsible for AJ dysfunction and increased epithelial permeability, which are both hallmarks of IBD.
JAK3 is a tyrosine kinase expressed in the gut among other tissues. JAK3 mediates cytokine signalling through activation of a number of cytokine receptors including IL-2, IL-9 and IL-15 (Safford et al. 1997). Recent work has suggested a role for JAK3 in intestinal barrier function in the context of inflammation (Table 1). Mishra and colleagues found that the colons of JAK3 knockout mice displayed higher levels of inflammation at baseline, characterised by increased levels of myeloperoxidase activity and IL-6 and IL-17a expression (Mishra et al. 2013). Upon treatment with DSS, JAK3 knockout mice suffered a more severe colitis phenotype than wild-type controls. Co-immunoprecipitation of JAK3 with β-catenin from intestinal epithelial cell lysates suggested co-localisation, and the association of β-catenin with AJs appeared to be impaired in JAK3 knockout mice colonic epithelia, suggesting a contributory role of JAK3 in β-catenin–AJ interactions (Mishra et al. 2013). Further studies to explore this mechanism in human ex vivo models are warranted.
The final pathway implicating a link between inflammation and AJs relates to p120-catenin (p120) (Table 1). P120 stabilises E-cadherin interactions in AJs and is an important regulator of cellular adhesion (Hu 2012). However, the literature also suggests a role of p120 as a functionally relevant anti-inflammatory mediator in different organ systems. For example, p120 deficiency in murine pulmonary vasculature has been shown to predispose to greater inflammatory responses to endotoxin exposure characterised by neutrophil homing and increased expression of TNF-α and Il-6 (Wang et al. 2011). Similarly, work with intestine-specific p120 knockout mice has demonstrated an association with increased colonic inflammatory exudates (Smalley-Freed et al. 2010). Indeed, the majority of the mice in this study died within 23 days from the sequelae of severe colitis. Defects in cellular adhesion were apparent in both the small and large intestines, with preserved TJ structure. Although the focus of the majority of studies examining AJ function during inflammation has been on the effects on E-cadherin and β-catenin, it would be worthwhile considering the function of the entire AJ complex, including p120; the biological relevance of p120 may be greater than has been previously realised.
Whether modulation of AJ protein levels at cellular junctions can be used as a therapeutic option remains to be seen. Greenspon and colleagues showed that increasing levels of E-cadherin at the cell–cell junctions led to improved barrier integrity in cultured intestinal epithelial cells (Greenspon et al. 2011). They showed that treatment with sphingosine-1-phosphate (S1P), a protein which is highly expressed in the intestine and has a pivotal role in enhancing barrier function in several non-intestinal tissues, can increase levels of E-cadherin mRNA and protein in intestinal epithelial cells leading to strong E-cadherin localisation to the cell–cell border. S1P treatment also improved the barrier function by decreasing permeability and increasing transepithelial electrical resistance (Greenspon et al. 2011). Once again, more focus is required to identify further modulators of AJ protein localisation and function, as well as examining effects on intestinal permeability and ultimately gut inflammation.
Therapeutic strategies to strengthen epithelial barrier function
Targeting AJ proteins and restoring epithelial barrier function are attractive treatment concepts in IBD, given that mucosal healing is associated with improved patient outcomes (Frøslie et al. 2007). Characteristics of any ideal AJ-modulating agent in IBD are shown in Table 2. Very few studies have been conducted in this area and none have identified a suitable therapeutic option, although the studies themselves have been heterogenous.
Vitamin D and the vitamin D receptor (VDR) have key roles in human disease pathogenesis. Significantly, vitamin D deficiency is a critical factor in IBD (Holick 2004; Narula and Marshall 2012), and other autoimmune diseases, as well as numerous additional pathologies including cancer (Holick 2004). Zhang and colleagues have recently drawn attention to an interesting link between vitamin D and Vitamin D receptor (VDR) signalling and barrier function (Zhang et al. 2013). Vitamin D, taken in the diet, has potential in treating defective tissue barriers as observed in the IBD intestine (Zhang et al. 2013). Currently, there is only limited and indirect data from colon cancer cells that suggest a role for vitamin D and VDR in regulating the adhesion complexes and AJs. For example, β-catenin expression can be repressed by VDR activation (Shah et al. 2006), and both vitamin D and VDR affect the Wnt signalling in colon cancer cells (Pendás-Franco et al. 2008; Larriba et al. 2007). Furthermore, 1,25(OH)2D3, the active metabolite of vitamin D, can promote the differentiation of colon carcinoma cells via induction of E-cadherin and inhibition of β-catenin signalling in SW480 cells that express VDR, but not in a malignant or metastatic sublines which lack VDR (Pálmer et al. 2001). Kong and colleagues used the DSS-induced colitis model to investigate the role of the vitamin D receptor (VDR) in mucosal barrier homeostasis (Kong et al. 2008). VDR null mice exposed to 2.5 % DSS had a marked colitic response with severe ulceration and impaired wound healing and diarrhea, rectal bleeding, and body weight loss culminating in death within 2 weeks. In contrast, wild-type mice were significantly more resistant to the DSS dose. Greater loss of TER and severe disruption in epithelial junctions was observed in colons of VDR−/− animals compared to VDR+/+ mice (Kong et al. 2008). Furthermore, administration of 1,25(OH)2D3 enhances E-cadherin expression in CaCo-2 human epithelial colorectal adenocarcinoma cells (Kong et al. 2008). These observations suggest that VDR plays a critical role in mucosal barrier homeostasis by preserving the integrity of junction complexes and the healing capacity of the colonic epithelium.
Vitamin D deficiency may compromise the mucosal barrier, leading to increased susceptibility to mucosal damage and increased risk of IBD. Clearly, further studies are needed on the function of vitamin D and VDR in murine and cellular colitis models, which should also include culturing of ex vivo IBD biopsies, to assess the link with AJs and the associated barrier repair and stability. Such models can also be used to elucidate new therapeutic targets for IBD patients with defective barrier functions. Furthermore, if vitamin D is to be used in IBD chemoprevention then further study is necessary. For example, the optimal level of the active vitamin D in patients with IBD is currently unknown, as is the best therapeutic modality. Understanding the role of AJs and the mechanisms critical to barrier function will allow more effective and efficient use of this relatively inexpensive and easy to use supplement.
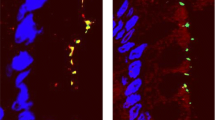
Another class of agent, similarly inexpensive, safe and subject to much recent research in the IBD field is probiotics. Khailova et al. (2009) examined the effects of Bifidobacterium bifidum on intestinal integrity in a neonatal rat model of necrotising enterocolitis (NEC). NEC is a significant cause of mortality in preterm infants with parallels to IBD in that altered intestinal permeability leading to bacterial invasion is a key feature. Compared to premature rats (NEC-model) given standard feed, those given feed supplemented with B. bifidum showed less histological mucosal damage and reduced mucosal IL-6 expression within the terminal ileum when exposed to asphyxia and cold stress to develop NEC. In addition, in the intestinal epithelium of NEC-rats on standard feed, both E-cadherin and α-catenin were predominantly cytoplasmic in location, whereas in the B. bifidum supplemented group, both AJ proteins were demonstrated to be mainly membranous, resembling the distribution observed in healthy animals. Overall, B. bifidum supplementation was associated with reduced ileal inflammation, maintenance of the mucosal layer, and improved intestinal integrity (Khailova et al. 2009). Although clinical trials have been undertaken to assess the efficacy of different probiotics in IBD, the majority were unsuccessful. Some probiotics have been found to reduce intestinal permeability in IBD models (Carlsson et al 2013; Hering et al 2014) by altering TJ function and expression, but alterations in AJ complexes have not been studied. Examining the effects of probiotics on AJ structure, distribution and function in models closer to IBD may provide insights into how some of the less efficacious therapies could be improved, for example in combination with other agents.
Other studies examining the effects of therapies on AJs have been performed in murine intestinal tumour models. Both carnosol (a constituent of the herb rosemary) (Moran et al. 2005) and post-ovariectomy estradiol (Javid et al. 2005) reduced tumour burden in an APC-mutation mouse model of intestinal polyposis, when delivered orally. Both treatments led to a reversal of intestinal epithelial AJ protein distribution associated with tumours: namely, increased membranous E-cadherin and an increased association of E-cadherin with β-catenin. Although the improved function of AJs in this setting was inferred, this was not demonstrated explicitly.
Finally, inhibition of Jak has been considered as a treatment modality in IBD patients. The Jak1/Jak3 inhibitor tofacitinib has been evaluated in a recent phase II clinical trial in UC patients. Targeting both Jak1 and Jak3 will block the action of numerous Jak1/Jak3-dependent cytokines (IL-2, IL-4, IL-7, IL-9, IL-15, and IL-21) (Liao et al. 2011; Sandborn et al. 2012) and may influence the function of cytokines dependent on Jak1/Jak2 (IL-6, IL-11, IFN-g, and IFN-a/IFN-b). Although broad pleiotropic effects on multiple cytokines may raise drug safety concerns, response and remission rates were significantly higher in tofacitinib-treated UC patients compared with placebo-treated controls (Sandborn et al. 2012). Interestingly, endoscopic assessment of patients revealed that tofacitinib treatment induced mucosal healing in many patients. These observations appear to run counter to those of Mishra and colleagues who showed that JAK3 knockout mice suffered a severe colitis phenotype on exposure to DSS (Mishra et al. 2013). The possibility that the association of β-catenin with AJs was impaired in JAK3 knockout mice colonic epithelia, suggesting a contributory role of JAK3 in β-catenin-AJ interactions (Mishra et al. 2013), also runs contrary to the observations in tofacitinib treated UC patients. Clearly, further studies are necessary to resolve this paradox.
Conclusion
The AJs form an integral and critical component of the selective epithelial barrier in the intestine. Much remains to be discovered about AJ structure and function in the developing and normal gut, and how homeostasis of the barrier is maintained throughout life. Significant disruption of AJs occurs during the inflammatory response. How early this happens in the disease process or whether an unknown underlying weakness of the AJ barrier contributes to disease pathogenesis requires investigation. Restoration of barrier integrity is a key goal for therapy in IBD patients. The identification and design of novel therapies will require detailed observational studies on IBD mucosa during the disease process to inform the design of better model systems. A much more comprehensive understanding of AJ barrier function and dysfunction has the potential to provide key inputs to improve the clinical management of IBD patients.
References
Aberle H, Butz S, Stappert J, Weissig H, Kemler R, Hoschuetzky H (1994) Assembly of the cadherin-catenin complex in vitro with recombinant proteins. J Cell Sci 107:3655–3663
Arnott ID, Kingstone K, Ghosh S (2000) Abnormal intestinal permeability predicts relapse in inactive Crohn disease. Scand J Gastroenterol 35:1163–1169
Aust DE, Terdiman JP, Willenbucher RF, Chew K, Ferrell L, Florendo C, Molinaro-Clark A, Baretton GB, Löhrs U, Waldman FM (2001) Altered distribution of beta-catenin, and its binding proteins E-cadherin and APC, in ulcerative colitis-related colorectal cancers. Mod Pathol 14:29–39
Barrett JC, Hansoul S, Nicolae DL, Cho JH, Duerr RH, Rioux JD, Brant SR, Silverberg MS, Taylor KD, Barmada MM, Bitton A, Dassopoulos T, Datta LW, Green T, Griffiths AM, Kistner EO, Murtha MT, Regueiro MD, Rotter JI, Schumm LP, Steinhart AH, Targan SR, Xavier RJ, NIDDK IBD Genetics Consortium, Libioulle C, Sandor C, Lathrop M, Belaiche J, Dewit O, Gut I, Heath S, Laukens D, Mni M, Rutgeerts P, Van Gossum A, Zelenika D, Franchimont D, Hugot JP, de Vos M, Vermeire S, Louis E, Belgian-French IBD Consortium; Wellcome Trust Case Control Consortium, Cardon LR, Anderson CA, Drummond H, Nimmo E, Ahmad T, Prescott NJ, Onnie CM, Fisher SA, Marchini J, Ghori J, Bumpstead S, Gwilliam R, Tremelling M, Deloukas P, Mansfield J, Jewell D, Satsangi J, Mathew CG, Parkes M, Georges M, Daly MJ (2008) Genome-wide association defines more than 30 distinct susceptibility loci for Crohn's disease. Nat Genet 40:955–962
Becker S, Wandel E, Wobus M, Schneider R, Amasheh S, Sittig D, Kerner C, Naumann R, Hamann J, Aust G (2010) Overexpression of CD97 in intestinal epithelial cells of transgenic mice attenuates colitis by strengthening adherens junctions. PLoS ONE 5:e8507
Breslin NP, Nash C, Hilsden RJ, Hershfield NB, Price LM, Meddings JB, Sutherland LR (2001) Intestinal permeability is increased in a proportion of spouses of patients with Crohn's disease. Am J Gastroenterol 96:2934–2938
Bruewer M, Luegering A, Kucharzik T, Parkos CA, Madara JL, Hopkins AM, Nusrat A (2003) Proinflammatory cytokines disrupt epithelial barrier function by apoptosis-independent mechanisms. J Immunol 171:6164–6172
Carlsson AH, Yakymenko O, Olivier I, Håkansson F, Postma E, Keita AV, Söderholm JD (2013) Faecalibacterium prausnitzii supernatant improves intestinal barrier function in mice DSS colitis. Scand J Gastroenterol 10:1136–44
Conner SD, Schmid SL (2003) Regulated portals of entry into the cell. Nature 422:37–44
Daugherty RL, Gottardi CJ (2007) Phospho-regulation of Beta-catenin adhesion and signaling functions. Physiology (Bethesda) 22:303–309
Davis MA, Ireton RC, Reynolds AB (2003) A core function for p120-catenin in cadherin turnover. J Cell Biol 163:525–534
Demetter P, De Vos M, Van Damme N, Baeten D, Elewaut D, Vermeulen S, Mareel M, Bullock G, Mielants H, Verbruggen G, De Keyser F, Veys EM, Cuvelier CA (2000) Focal up-regulation of E-cadherin-catenin complex in inflamed bowel mucosa but reduced expression in ulcer-associated cell lineage. Am J Clin Pathol 114:364–370
Doğan A, Wang ZD, Spencer J (1995) E-cadherin expression in intestinal epithelium. J Clin Pathol 48:143–146
Drees F, Pokutta S, Yamada S, Nelson WJ, Weis WI (2005) Alpha-catenin is a molecular switch that binds E-cadherin-beta-catenin and regulates actin-filament assembly. Cell 123:903–915
Dubois PC, van Heel DA (2008) New susceptibility genes for ulcerative colitis. Nat Genet 40:686–688
Duerr RH, Taylor KD, Brant SR, Rioux JD, Silverberg MS, Daly MJ, Steinhart AH, Abraham C, Regueiro M, Griffiths A, Dassopoulos T, Bitton A, Yang H, Targan S, Datta LW, Kistner EO, Schumm LP, Lee AT, Gregersen PK, Barmada MM, Rotter JI, Nicolae DL, Cho JH (2006) A genome-wide association study identifies IL23R as an inflammatory bowel disease gene. Science 314:1461–1463
Elding H, Lau W, Swallow DM, Maniatis N (2011) Dissecting the genetics of complex inheritance: linkage disequilibrium mapping provides insight into Crohn disease. Am J Hum Genet 89:798–805
Faraldo MM, Teulière J, Deugnier MA, Birchmeier W, Huelsken J, Thiery JP, Cano A, Glukhova MA (2007) Beta-Catenin regulates P-cadherin expression in mammary basal epithelial cells. FEBS Lett 581:831–836
Frøslie KF, Jahnsen J, Moum BA, Vatn MH, IBSEN Group (2007) Mucosal healing in inflammatory bowel disease: results from a Norwegian population-based cohort. Gastroenterology 133:412–22
Gassler N, Rohr C, Schneider A, Kartenbeck J, Bach A, Obermüller N, Otto HF, Autschbach F (2001) Inflammatory bowel disease is associated with changes of enterocytic junctions. Am J Physiol Gastrointest Liver Physiol 281:G216–228
Gibson PR, van de Pol E, Barratt PJ, Doe WF (1988) Ulcerative colitis-a disease characterised by the abnormal colonic epithelial cell? Gut 29:516–521
Gibson P, Rosella O, Nov R, Young G (1995) Colonic epithelium is diffusely abnormal in ulcerative colitis and colorectal cancer. Gut 36:857–863
Glover LE, Bowers BE, Saeedi B, Ehrentraut SF, Campbell EL, Bayless AJ, Dobrinskikh E, Kendrick AA, Kelly CJ, Burgess A, Miller L, Kominsky DJ, Jedlicka P, Colgan SP (2013) Control of creatine metabolism by HIF is an endogenous mechanism of barrier regulation in colitis. Proc Natl Acad Sci U S A 110:19820–19825
Greenspon J, Li R, Xiao L, Rao JN, Sun R, Strauch ED, Shea-Donohue T, Wang JY, Turner DJ (2011) Sphingosine-1-phosphate regulates the expression of adherens junction protein E-cadherin and enhances intestinal epithelial cell barrier function. Dig Dis Sci 56:1342–1353
Hampe J, Franke A, Rosenstiel P, Till A, Teuber M, Huse K, Albrecht M, Mayr G, De La Vega FM, Briggs J, Günther S, Prescott NJ, Onnie CM, Häsler R, Sipos B, Fölsch UR, Lengauer T, Platzer M, Mathew CG, Krawczak M, Schreiber S (2007) A genome-wide association scan of nonsynonymous SNPs identifies a susceptibility variant for Crohn disease in ATG16L1. Nat Genet 39:207–211
Han SP, Yap AS (2012) The cytoskeleton and classical cadherin adhesions. Subcell Biochem 60:111–135
Hanby AM, Chinery R, Poulsom R, Playford RJ, Pignatelli M (1996) Downregulation of E-cadherin in the reparative epithelium of the human gastrointestinal tract. Am J Pathol 148:723–729
Hardy RG, Tselepis C, Hoyland J, Wallis Y, Pretlow TP, Talbot I, Sanders DS, Matthews G, Morton D, Jankowski JA (2002) Aberrant P-cadherin expression is an early event in hyperplastic and dysplastic transformation in the colon. Gut 50:513–519
Harhaj NS, Barber AJ, Antonetti DA (2002) Platelet-derived growth factor mediates tight junction redistribution and increases permeability in MDCK cells. J Cell Physiol 193:349–364
Harris TJ, Tepass U (2010) Adherens junctions: from molecules to morphogenesis, Nat. Rev. Mol Cell Biol 11:502–514
Hermiston ML, Gordon JI (1995) In vivo analysis of cadherin function in the mouse intestinal epithelium: essential roles in adhesion, maintenance of differentiation, and regulation of programmed cell death. J Cell Biol 129:489–506
Hering NA, Richter JF, Fromm A, Wieser A, Hartmann S, Günzel D, Bücker R, Fromm M, Schulzke JD, Troeger H (2014) TcpC protein from E. coli Nissle improves epithelial barrier function involving PKCζ and ERK1/2 signaling in HT-29/B6 cells. Mucosal Immunol 2:369–78
Holick M (2004) Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am J Clin Nutr 2004(80):1678S–1688S
Hu G (2012) p120-Catenin: a novel regulator of innate immunity and inflammation. Crit Rev Immunol 32:127–138
Ivanov AI, Nusrat A, Parkos CA (2004a) Endocytosis of epithelial apical junctional proteins by a clathrin-mediated pathway into a unique storage compartment. Mol Biol Cell 15:176–188
Ivanov AI, Nusrat A, Parkos CA (2004b) The epithelium in inflammatory bowel disease: potential role of endocytosis of junctional proteins in barrier disruption. Novartis Found Symp J 263:115–124
Javid SH, Moran AE, Carothers AM, Redston M, Bertagnolli MM (2005) Modulation of tumor formation and intestinal cell migration by estrogens in the Apc(Min/+) mouse model of colorectal cancer. Carcinogenesis 26:587–95
Khailova L, Dvorak K, Arganbright KM, Halpern MD, Kinouchi T, Yajima M, Dvorak B (2009) Bifidobacterium bifidum improves intestinal integrity in a rat model of necrotizing enterocolitis. Am J Physiol Gastrointest Liver Physiol 297:G940–9
Jankowski JA, Bedford FK, Boulton RA, Cruickshank N, Hall C, Elder J, Allan R, Forbes A, Kim YS, Wright NA, Sanders DS (1998) Alterations in classical cadherins associated with progression in ulcerative and Crohn's colitis. Lab Invest 78:1155–1167
Karayiannakis AJ, Syrigos KN, Efstathiou J, Valizadeh A, Noda M, Playford RJ, Kmiot W, Pignatelli M (1998) Expression of catenins and E-cadherin during epithelial restitution in inflammatory bowel disease. J Pathol 185:413–418
Kevil CG, Ohno N, Gute DC, Okayama N, Robinson SA, Chaney E, Alexander JS (1998) Role of cadherin internalization in hydrogen peroxide-mediated endothelial permeability. Free Radicals Biol Med 24:1015–1022
Kinugasa T, Akagi Y, Yoshida T, Ryu Y, Shiratuchi I, Ishibashi N, Shirouzu K (2010) Increased claudin-1 protein expression contributes to tumorigenesis in ulcerative colitis-associated colorectal cancer. Anticancer Res 30:3181–3186
Kong J, Zhang Z, Musch MW, Ning G, Sun J, Hart J, Bissonnette M, Li YC (2008) Novel role of the vitamin D receptor in maintaining the integrity of the intestinal mucosal barrier. Am J Physiol Gastrointest Liver Physiol 294:G208–16
Kucharzik T, Walsh SV, Chen J, Parkos CA, Nusrat A (2001) Neutrophil transmigration in inflammatory bowel disease is associated with differential expression of epithelial intercellular junction proteins. Am J Pathol 159:2001–2009
Kurita S, Ogita H, Takai Y (2011) Cooperative role of nectin-nectin and nectin-afadin interactions in formation of nectin-based cell-cell adhesion. J Biol Chem 286:36297–36303
Larriba MJ, Valle N, Pálmer HG, Ordóñez-Morán P, Alvarez-Díaz S, Becker KF, Gamallo C, de Herreros AG, González-Sancho JM, Muñoz A (2007) The inhibition of Wnt/beta-catenin signalling by 1alpha,25-dihydroxyvitamin D3 is abrogated by Snail1 in human colon cancer cells. Endocr Relat Cancer 14:141–51
Liao W, Lin JX, Leonard WJ (2011) IL-2 family cytokines: new insights into the complex roles of IL-2 as a broad regulator of T helper cell differentiation. Curr Opin Immunol 23:598–604
Majmundar AJ, Wong WJ, Simon MC (2010) Hypoxia-inducible factors and the response to hypoxic stress. Mol Cell 40:294–309
Mathew CG, Lewis CM (2004) Genetics of inflammatory bowel disease: progress and prospects. Hum Mol Genet 13 Spec No 1:R161-168
McGovern DP, Gardet A, Törkvist L, Goyette P, Essers J, Taylor KD, Neale BM, Ong RT, Lagacé C, Li C, Green T, Stevens CR, Beauchamp C, Fleshner PR, Carlson M, D'Amato M, Halfvarson J, Hibberd ML, Lördal M, Padyukov L, Andriulli A, Colombo E, Latiano A, Palmieri O, Bernard EJ, Deslandres C, Hommes DW, de Jong DJ, Stokkers PC, Weersma RK, NIDDK IBD Genetics Consortium, Sharma Y, Silverberg MS, Cho JH, Wu J, Roeder K, Brant SR, Schumm LP, Duerr RH, Dubinsky MC, Glazer NL, Haritunians T, Ippoliti A, Melmed GY, Siscovick DS, Vasiliauskas EA, Targan SR, Annese V, Wijmenga C, Pettersson S, Rotter JI, Xavier RJ, Daly MJ, Rioux JD, Seielstad M (2010) Genome-wide association identifies multiple ulcerative colitis susceptibility loci. Nat Genet 42:332–337
McNamara BP, Koutsouris A, O'Connell CB, Nougayréde JP, Donnenberg MS, Hecht G (2001) Translocated EspF protein from enteropathogenic Escherichia coli disrupts host intestinal barrier function. J Clin Invest 107:621–629
Miller JR, McClay DR (1997) Changes in the pattern of adherens junction-associated beta-catenin accompany morphogenesis in the sea urchin embryo. Dev Biol 192:310–322
Michael M, Yap AS (2013) The regulation and functional impact of actin assembly at cadherin cell-cell adhesions. Semin Cell Dev Biol 24:298–307
Mishra J, Verma RK, Alpini G, Meng F, Kumar N (2013) Role of Janus kinase 3 in mucosal differentiation and predisposition to colitis. J Biol Chem 288:31795–31806
Moran AE, Carothers AM, Weyant MJ, Redston M, Bertagnolli MM (2005) Carnosol inhibits beta-catenin tyrosine phosphorylation and prevents adenoma formation in the C57BL/6 J/Min/+ (Min/+) mouse. Cancer Res 65:1097–104
Mukherjee S, Ghosh RN, Maxfield FR (1997) Endocytosis. Physiol Rev 77:759–803
Nagafuchi A, Takeichi M (1989) Transmembrane control of cadherin-mediated cell adhesion: a 94 kDa protein functionally associated with a specific region of the cytoplasmic domain of E-cadherin. Cell Regul 1:37–44
Narula N, Marshall JK (2012) Management of inflammatory bowel disease with vitamin D: beyond bone health. J Crohns Colitis 6:397–404
Nelson WJ, Nusse R (2004) Convergence of Wnt, beta-catenin, and cadherin pathways. Science 303:1483–1487
Nose A, Tsuji K, Takeichi M (1990) Localization of specificity determining sites in cadherin cell adhesion molecules. Cell 61:147–155
Oda H, Tsukita S, Takeichi M (1998) Dynamic behavior of the cadherin-based cell-cell adhesion system during Drosophila gastrulation. Dev Biol 203:435–450
Ozawa M, Baribault H, Kemler R (1989) The cytoplasmic domain of the cell adhesion molecule uvomorulin associates with three independent proteins structurally related in different species. EMBO J 8:1711–1717
Pálmer HG, González-Sancho JM, Espada J, Berciano MT, Puig I, Baulida J, Quintanilla M, Cano A, de Herreros AG, Lafarga M, Muñoz A (2001) Vitamin D(3) promotes the differentiation of colon carcinoma cells by the induction of E-cadherin and the inhibition of beta-catenin signaling. J Cell Biol 154:369–87
Peeters M, Geypens B, Claus D, Nevens H, Ghoos Y, Verbeke G, Baert F, Vermeire S, Vlietinck R, Rutgeerts P (1997) Clustering of increased small intestinal permeability in families with Crohn's disease. Gastroenterology 113:802–807
Pendás-Franco N, Aguilera O, Pereira F, González- Sancho JM, Muñoz A (2008) Vitamin D and Wnt/beta- catenin pathway in colon cancer: role and regulation of DICKKOPF genes. Anticancer Res 28:2613–23
Perez-Moreno M, Fuchs E (2006) Catenins: keeping cells from getting their signals crossed. Dev Cell 11:601–612
Pokutta S, Weis WI (2000) Structure of the dimerization and β-catenin binding region of α-catenin. Mol Cell 5:533–543
Polak-Charcon S, Shoham J, Ben-Shaul Y (1980) Tight junctions in epithelial cells of human fetal hindgut, normal colon, and colon adenocarcinoma. J Natl Cancer Inst 65:53–62
Prasad S, Mingrino R, Kaukinen K, Hayes KL, Powell RM, MacDonald TT, Collins JE (2005) Inflammatory processes have differential effects on claudins 2, 3 and 4 in colonic epithelial cells. Lab Invest 85:1139–1162
Rao RK, Basuroy S, Rao VU, Karnaky KJ Jr, Gupta A (2002) Tyrosine phosphorylation and dissociation of occludin-ZO-1 and E-cadherin-beta-catenin complexes from the cytoskeleton by oxidative stress. Biochem J 368:471–481
Rioux JD, Silverberg MS, Daly MJ, Steinhart AH, McLeod RS, Griffiths AM, Green T, Brettin TS, Stone V, Bull SB, Bitton A, Williams CN, Greenberg GR, Cohen Z, Lander ES, Hudson TJ, Siminovitch KA (2000) Genomewide search in Canadian families with inflammatory bowel disease reveals two novel susceptibility loci. Am J Hum Genet 66:1863–1870
Safford MG, Levenstein M, Tsifrina E, Amin S, Hawkins AL, Griffin CA, Civin CI, Small D (1997) JAK3: expression and mapping to chromosome 19p12–13.1. Exp Hematol 25:374–386
Sandborn WJ, Ghosh S, Panes J, Su C, Rousell S, Niezychowski W, Study A3921063 Investigators (2012) Tofacitinib, an oral Janus kinase inhibitor, in active ulcerative colitis. N Engl J Med 367:612–624
Schmitz H, Barmeyer C, Fromm M, Runkel N, Foss HD, Bentzel CJ, Riecken EO, Schulzke JD (1999) Altered tight junction structure contributes to the impaired epithelial barrier function in ulcerative colitis. Gastroenterology 116:301–309
Schofield CJ, Ratcliffe PJ (2004) Oxygen sensing by HIF hydroxylases. Nat Rev Mol Cell Biol 5:343–354
Shah S, Islam MN, Dakshanamurthy S, Rizvi I, Rao M, Herrell R, Zinser G, Valrance M, Aranda A, Moras D, Norman A, Welsh J, Byers SW (2006) The molecular basis of vitamin D receptor and beta-catenin crossregulation. Mol Cell 21:799–809
Smalley-Freed WG, Efimov A, Burnett PE, Short SP, Davis MA, Gumucio DL, Washington MK, Coffey RJ, Reynolds AB (2010) p120-catenin is essential for maintenance of barrier function and intestinal homeostasis in mice. J Clin Invest 120:1824–1835
Shenoy AK, Fisher RC, Butterworth EA, Pi L, Chang LJ, Appelman HD, Chang M, Scott EW, Huang EH (2012) Transition from colitis to cancer: high Wnt activity sustains the tumor-initiating potential of colon cancer stem cell precursors. Cancer Res 72:5091–5100
Soletti RC, Rodrigues NA, Biasoli D, Luiz RR, de Souza HS, Borges HL (2013) Immunohistochemical analysis of retinoblastoma and β-catenin as an assistant tool in the differential diagnosis between Crohn's disease and ulcerative colitis. PLoS ONE 8:e70786
Sun TT, Wang Y, Cheng H, Xiao HZ, Xiang JJ, Zhang JT, Yu SB, Martin TA, Ye L, Tsang LL, Jiang WG, Xiaohua J, Chan HC (2014) Disrupted interaction between CFTR and AF-6/afadin aggravates malignant phenotypes of colon cancer. Biochim Biophys Acta 1843:618–628
Takai Y, Nakanishi H (2003) Nectin and afadin:novel organizers of intercellular junctions. J Cell Sci 116:17–27
Takeichi M (1988) The cadherins: cell-cell adhesion molecules controlling animal morphogenesis. Development 102:639–655
Talavera D, Castillo AM, Dominguez MC, Gutierrez AE, Meza I (2004) IL8 release, tight junction and cytoskeleton dynamic reorganization conducive to permeability increase are induced by dengue virus infection of microvascular endothelial monolayers. J Gen Virol 85:1801–1813
UK IBD Genetics Consortium, Barrett JC, Lee JC, Lees CW, Prescott NJ, Anderson CA, Phillips A, Wesley E, Parnell K, Zhang H, Drummond H, Nimmo ER, Massey D, Blaszczyk K, Elliott T, Cotterill L, Dallal H, Lobo AJ, Mowat C, Sanderson JD, Jewell DP, Newman WG, Edwards C, Ahmad T, Mansfield JC, Satsangi J, Parkes M, Mathew CG, Wellcome Trust Case Control Consortium 2, Donnelly P, Peltonen L, Blackwell JM, Bramon E, Brown MA, Casas JP, Corvin A, Craddock N, Deloukas P, Duncanson A, Jankowski J, Markus HS, Mathew CG, McCarthy MI, Palmer CN, Plomin R, Rautanen A, Sawcer SJ, Samani N, Trembath RC, Viswanathan AC, Wood N, Spencer CC, Barrett JC, Bellenguez C, Davison D, Freeman C, Strange A, Donnelly P, Langford C, Hunt SE, Edkins S, Gwilliam R, Blackburn H, Bumpstead SJ, Dronov S, Gillman M, Gray E, Hammond N, Jayakumar A, McCann OT, Liddle J, Perez ML, Potter SC, Ravindrarajah R, Ricketts M, Waller M, Weston P, Widaa S, Whittaker P, Deloukas P, Peltonen L, Mathew CG, Blackwell JM, Brown MA, Corvin A, McCarthy MI, Spencer CC, Attwood AP, Stephens J, Sambrook J, Ouwehand WH, McArdle WL, Ring SM, Strachan DP (2009) Genome-wide association study of ulcerative colitis identifies three new susceptibility loci, including the HNF4A region. Nat Genet 41:1330–1334
Utech M, Mennigen R, Bruewer M (2010) Endocytosis and recycling of tight junction proteins in inflammation. J Biomed Biotechnol 2010:484987
van Heel DA, Dechairo BM, Dawson G, McGovern DP, Negoro K, Carey AH, Cardon LR, Mackay I, Jewell DP, Lench NJ (2003) The IBD6 Crohn's disease locus demonstrates complex interactions with CARD15 and IBD5 disease-associated variants. Hum Mol Genet 12:2569–2575
Vlad-Fiegen A, Langerak A, Eberth S, Müller O (2012) The Wnt pathway destabilizes adherens junctions and promotes cell migration via β-catenin and its target gene cyclin D1. FEBS Open Bio 2:26–31
Watson AJ, Hughes KR (2012) TNF-α-induced intestinal epithelial cell shedding: implications for intestinal barrier function. Ann N Y Acad Sci 1258:1–8
Wang YL, Malik AB, Sun Y, Hu S, Reynolds AB, Minshall RD, Hu G (2011) Innate immune function of the adherens junction protein p120-catenin in endothelial response to endotoxin. J Immunol 186:3180–3187
Weber CR, Turner JR (2007) Inflammatory bowel disease: is it really just another break in the wall? Gut 56:6–8
Wellcome Trust Case Control Consotrium (2007) Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature 447:661–678
Wright NA, Pike CM, Elia G (1990) Ulceration induces a novel epidermal growth factor-secreting cell lineage in human gastrointestinal mucosa. Digestion 46(Suppl 2):125–133
Wrobel CN, Debnath J, Lin E, Beausoleil S, Roussel MF, Brugge JS (2004) Autocrine CSF-1R activation promotes Src-dependent disruption of mammary epithelial architecture. J Cell Biol 165:263–273
Wyatt J, Vogelsang H, Hübl W, Waldhöer T, Lochs H (1993) Intestinal permeability and the prediction of relapse in Crohn's disease. Lancet 341:1437–1439
Xiao K, Allison DF, Buckley KM, Kottke MD, Vincent PA, Faundez V, Kowalczyk AP (2003) Cellular levels of p120 catenin function as a set point for cadherin expression levels in microvascular endothelial cells. J Cell Biol 163:535–545
Yap AS, Niessen CM, Gumbiner BM (1998) The juxtamembrane region of the cadherin cytoplasmic tail supports lateral clustering, adhesive strengthening, and interaction with p120ctn. J Cell Biol 141:779–789
Yona S, Lin HH, Siu WO, Gordon S, Stacey M (2008) Adhesion-GPCRs: emerging roles for novel receptors. Trends Biochem Sci 33:491–500
Zeissig S, Bürgel N, Günzel D, Richter J, Mankertz J, Wahnschaffe U, Kroesen AJ, Zeitz M, Fromm M, Schulzke JD (2007) Changes in expression and distribution of claudin 2, 5 and 8 lead to discontinuous tight junctions and barrier dysfunction in active Crohn's disease. Gut 56:61–72
Zhang YG, Wu S, Sun J (2013) Vitamin D, Vitamin D Receptor, and Tissue Barriers. Tissue Barriers 1, pii:e23118
Author information
Authors and Affiliations
Corresponding author
Additional information
Shameer Mehta, Anke Nijhuis and Tomoko Kumagai contributed equally.
Andrew Silver and James Lindsay are joint corresponding authors
Rights and permissions
About this article
Cite this article
Mehta, S., Nijhuis, A., Kumagai, T. et al. Defects in the adherens junction complex (E-cadherin/ β-catenin) in inflammatory bowel disease. Cell Tissue Res 360, 749–760 (2015). https://doi.org/10.1007/s00441-014-1994-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-014-1994-6