Abstract
Oral squamous cell carcinoma (OSCC) is a malignant disease in the world which has a profound effect on human health and life quality. According to tumor stage and pathological diagnosis, OSCC is mainly treated by combinations of surgery, radiotherapy and chemotherapy. However, traditional treatment methods suffer from some limitations, such as systemic toxicity, limited therapeutic effect and drug resistance. With the rapid development of nanotechnology, nanodrug delivery systems (DDSs) and intelligent DDSs have been widely used in targeted therapy for OSCC. Meanwhile, the newly developed therapeutic techniques such as immunotherapy, gene therapy and bionic technology provide the possibility to realize the active targeted therapy. Here, the latest advances of target therapy for OSCC are reviewed, and their therapeutic remarks, current limits and future prospects are also systematically interpreted. It is believed that active and passive targeted therapies have great potentials for clinical transformation and application of OSCC, which will greatly improve human quality of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Head and neck cancer, developed in the mucosal lining of the upper-aerodigestive tract, is a tumor that arises in the oral cavity, oropharynx, hypopharynx, and larynx, ranks top ten of all cancers. A majority of head and neck cancers are squamous cell carcinomas (SCCs) and the 5-year survival rate is approximately 50% (van Harten and Brakenhoff 2021). OSCC, constituting 48% of head and neck cancer cases, refers to tumors that occur at the lips, gums, tongue, mouth, and palate, while pharyngeal squamous cell carcinoma (PSCC) comprises cancers of the tonsils, base of tongue, soft palate, and uvula (Chen et al. 2021; Nakashima et al. 2017; Tshering Vogel et al. 2010). OSCC and PSCC comprise the most common subtype of head and neck squamous cell carcinomas (HNSCC) (Torre et al. 2015). Even though anatomically adjacent to each other, a growing body of data prove that OSCC is significantly different from other subtypes of HNSCC from different perspectives. OSCC is mainly associated with smoking and betel nut consumption, while the incidence of PSCC is on the rise in recent decades due to chronic latent infections of human papillomavirus (HPV) and 85–96% are caused by HPV-16 infections (Hussein et al. 2017; Sturgis and Cinciripini 2007). From molecular biology perspective, OSCC, PSCC, and laryngeal squamous cell carcinoma (LSCC) show significant differences in genetic change patterns. In general, PSCC and LSCC have more copy number aberrations per tumor than OSCC. Different chromosome aberrations may play a role in the occurrence and development of different subgroups of HNSCC (Huang et al. 2002). Besides, in the direct comparison of oral and pharyngeal tumors, 46 miRNAs were found to be differentially expressed, and there were differences in miRNA expression patterns between oral and pharyngeal normal epithelium and SCCs (Johnson et al. 2020). In terms of angiogenesis, due to the differential expression of vascular endothelial growth factor (VEGF), OSCC and PSCC are clinically invasive compared with LSCC (Boonkitticharoen et al. 2008). Oral cancers may develop from some premalignant dysplastic lesions, such as leukoplakia, erythroplakia and lichen planus, while patients with advanced-stage HNSCC without a clinical history of a premalignancy (Kerawala et al. 2016; Montero and Patel 2015). Therefore, oral cavity and larynx cancer can be diagnosed at an early stage because patients perceive mass lesions and symptoms that interfere with eating and speaking. In contrast, due to its hidden anatomical location, the oropharyngeal primary tumor usually presents symptoms at a later stage which poses a great challenge to clinical treatment and prognosis. According to the stage of the disease, oral cancer is usually treated with surgical resection, followed by chemotherapy or radiotherapy plus radiation. Chemoradiation has been the main treatment for pharyngeal or laryngeal cancer (Johnson et al. 2020). However, all these modalities have nonnegligible sides and adverse effects. For example, surgery is the most effective method for the treatment of OSCC, but surgery trauma significantly affects the functions and esthetics of the oral and maxillofacial region. Besides, chemotherapy can bring about hair loss, nausea, vomiting, and infections, while radiation therapy can cause transient or permanent damage to healthy tissues and severely affect the quality of life (Argiris et al. 2008; Zhang et al. 2020). Moreover, about one-third of patients are still at risk of recurrence and resistance to radiotherapy and chemotherapy after receiving these traditional treatments, which poses a serious threat to public health (Greenberg et al. 2003).
With recent advances in nanotechnology, DDSs have been widely used in passive targeted therapy for OSCC. Owing to the abnormal and high porosity of tumor blood vessels, DDSs can pass through high permeability tumor vessels and stay there without being cleared quickly, which is named enhanced permeability and retention (EPR) effect (Greish 2012; Nakamura et al. 2016). Through EPR effect or by targeting active modifications, DDSs enable targeted drug delivery and thus have been widely explored in OSCC therapy (Greish 2012; Wu et al. 2015). Recently, a new generation of DDSs with tumor environmental stimulus response have been applied to OSCC treatment (Kalaydina et al. 2018; Ketabat et al. 2019). In response to the unique tumor microenvironment (TEM) stimuli, these smart DDSs can achieve specific drug delivery and release, improving treatment effect and reducing side effects (Li et al. 2019a, b). Besides, low pH, high levels of reactive oxygen species (ROS), up-regulated antioxidant capacity and overexpression of specific enzymes and receptors in tumor areas provide another opportunity for targeted therapy of OSCC. Although TME has their unique characteristics compared with normal conditions, the uncontrollable and unstable nature of TEM limits the application of internal stimulus–response DDSs. Some recently developed novel active targeted therapies, such as gene therapy and immunotherapy, have shown promise as an additional treatment option in oral cancer (Marcazzan et al. 2018; Veigas et al. 2021). Gene therapy has the potential to target cancer tissues while preserving normal tissue. This strategy is useful for recurrent and adjuvant therapy for OSCC. Nevertheless, gene delivery and transfection efficiency need to be optimized before this technology can be used in clinic. Immunotherapy, a recently developed modality, can prevent the development of OSCC by blocking the pathway that cancer cells escape from the immune system or enhancing the immune response of patients against tumor cells (Cheng et al. 2019). Immunotherapy for oral cancer target multiple immune processes and key checkpoints, such as cytotoxic T lymphocyte-associated antigen-4 (CTLA4) and programmed death (PD-1) and its ligand (PD-L1) (Veigas et al. 2021). However, only a small percent of patients perceive clinical benefit.
Here, we conducted a literature review on current trends of targeted therapy for OSCC. Our review is divided into the following three parts: the common methods of passive and active targeted therapy for OSCC are summarized, respectively. Based on previous literature we show the current trends and several future prospects in OSCC therapy.
Passive targeted therapy of OSCC
As tumor cells metabolize vigorously and need more nutrients than normal cells, VEGF and other factors are secreted in tumors to promote angiogenesis. Compared with that of normal vessels, the endothelial gap of neovascularization is larger, which facilitates the transport of macromolecules to tumor tissues through blood vessels. In addition, the lack of lymphatic vessels in the tumor leads to lymphatic reflux asphyxia. In this dual case, macromolecules or nanoparticles (NPs) accumulate in the tumor tissue through the EPR effect, which is the basis of passive targeted therapy of OSCC.
Nanoparticles-based drug delivery for OSCC-targeted therapy
Anticancer drugs, such as cisplatin (CDDP), paclitaxel (PTX),5-fluorouracil (5-FU), and doxorubicin (DOX), are used alone or in combination for OSCC treatment (Ketabat et al. 2019). However, some shortcomings, including high toxicity, limited solubility, permeability and poor biocompatibility, have prevented their further clinical application (Kruijtzer 2002; Zhang et al. 2020). To address the issues mentioned above, there is a great demand for the targeted DDSs with the potentials to improve drug bioavailability and biological distribution at the site of the primary tumor. Due to the excellent physical and chemical characteristics, NPs can be tailored to achieve targeted drug delivery with improved biocompatibility and therapeutic efficiency, reducing its systemic toxicity of oral cancer treatment. Commonly used NPs include polymeric NPs, liposomes, gold NPs (AuNPs), and hydrogels (Fig. 1).
Polymeric nanoparticles for OSCC-targeted therapy
The ideal drug carriers should have high loading capacity, good biocompatibility, biodegradability, and site-specific administration, and avoid adverse drug reactions. Naturally sourced or synthetical polymers, such as polysaccharides, poly (lactic acid) (PLA), polycaprolactone (PCL), poly (glycolic acid) (PGA), and polyethylene glycol (PEG) have received much attention. Through encapsulating, absorbing or bounding, therapeutic agents can be entrapped in polymer or adhered to their surface. These submicron-sized polymer NPs can improve the effectiveness, bioavailability, and solubility of drug molecules and can further provide targeted delivery by modifying with active targeting moieties. For example, to increase the antitumor effects and reduce the toxicity problems, based on a PEG–poly (glutamic acid) block copolymer, Endo et al. prepared a kind of polymeric NPs carrying CDDP. With a prolonged circulation time and EPR capability, CDDP accumulates in an orthotopic tongue cancer model and showed equivalent antitumor effects (Endo et al. 2013). Other studies also prepared NPs composed of polymers, including poly (lactic-co-glycolic acid) (PLGA), PEG, polyethylenimine (PEI), PCL, and N-vinylpyrrolidone/acrylic acid, and then loaded with photosensitizer or radiosensitizing drug for oral cancer treatment (Ma et al. 2017; Parul et al. 2018; Pornpitchanarong et al. 2019; Ren et al. 2017). Besides, to achieve the targeted therapy, Wang et al. formulated CDDP-loaded PLGA-NPs and further conjugated them with NR7 peptide, which can specifically bind to the epidermal growth factor receptor (EGFR) domain. In EGFR receptor-overexpressed OSCC cancer cells, the feasibility of using NR7 peptide to achieve superior anticancer effects and enhanced cytotoxic effect has been proved (Wang et al. 2015). Similarly, Wang et al. formulated PEGylated doxorubicin (PD) NPs and further modified by HN-1 peptide which can specifically bind to and be efficiently internalized in HNSCC cells. The in vitro and in vivo results showed that PD NPs modified with HN-1 peptide have enhanced tumor-targeting properties and exhibited significantly higher cellular uptake and toxicity (Wang et al. 2017a, b). Wu et al. also reported modifying polymeric NPs by folic acid (FA), which can bind very firmly to folate receptors over-expressed in oral cancer, and both the in vitro and in vivo results proved hybrid NPs are a controllable and targeted anticancer drug delivery system to OSCC (Wu et al. 2015). At the same time, polymeric NPs are also used for the delivery of RNA interference in the therapy of OSCC, which will be covered in more detail later.
Another ideal and biocompatible nanocarrier is hyaluronic acid (HA), one of the main components of the extracellular matrix (Huang et al. 2014). Moreover, HA is one of the ligands of CD44 which was highly expressed on the OSCC cellular membranes and is closely associated with tumor growth, proliferation, and metastasis (A et al. 2015; Cai et al. 2014). In 2019, HA was used to encapsulate CDDP and organic molecule, TQTPA [4,4ʹ-((6,7-bis(4-(hexyloxy)phenyl)-[1,2,5]thiadiazolo [3,4-g]quinoxaline-4,9-diyl)bis(thiophene-5,2-diyl))bis(N,N-diphenylaniline)], forming new tumor-targeted NPs (HT@CDDP). Through in vivo study, Wang et al. proved that HT@CDDP NPs could accumulate at tumor sites through CD44-mediated endocytosis on the surface of OSCC and exert improved antitumor effect in OSCC orthotopic models (Wang et al. 2019a, b, c, d, e). Besides, chitosan NPs are promising cancer drug vehicles and other drugs such as glycyrrhetic acid, ellagic acid, CDDP, and curcumin have been encapsulated for local application of oral tumors, avoiding biological inactivation of the drug (Arulmozhi et al. 2013; Cacciotti et al. 2018; Goldberg et al. 2014; Mazzarino et al. 2015). In addition, chitosan may increase the residence time of the drug device at the absorption site by electrostatic interaction with the negatively charged mucosal surface, showing prospect application in drug delivery (Zheng et al. 2021). Collectively, the polymer nanoplatform can improve the site-specific distribution of chemotherapeutic drugs, which show promise for application in clinical practice.
Liposomes for OSCC-targeted therapy
Liposomes are variable-sized artificial vesicles made of amphiphilic phospholipid bilayers, which can encapsulate water-soluble and hydrophobic drugs into the selected tissues. Liposome carriers can significantly improve the low water solubility of drugs and enhance the passive targeting ability of tumors based on EPR effects to achieve effective drug delivery. However, drug-loaded liposomes are so easily recognized and cleared by the reticuloendothelial system (RES) that some biocompatible polymers such as PEG have been used to modify the surface of liposomes.
In 2019, El-Hamid et al. investigated the apoptotic effect of DOX and PEGylated liposomal doxorubicin (PLD) on Cal-27 cells (Ibrahim et al. 2019). PLD performed a higher apoptotic effect on Cal-27 cells due to the increased stability of dox after liposome encapsulation and enhanced drug accumulation in tumors through the EPR effect (Kaminskas et al. 2012; Seynhaeve et al. 2013). Narayanan et al. coencapsulated PEGylated liposomal nanocarrier formulation of DOX and resveratrol and evaluated the anticancer efficacy in oral cancer, which proved that the effect of drug combination encapsulated in the liposomal formulation was better than that of free drugs (Mohan et al. 2016). Meanwhile, a liposomal nanoplatform formulation of photosensitizer and anticancer drugs also has great potentials for oral cancer diagnosis and treatment. Wei et al. integrated photosensitizer indocyanine green (ICG) and evodiamine into a liposomal nanoplatform against OSCC. In vitro and in vivo studies proved that the theragnostic liposomes showed enhanced inhibition on tongue tumor (Wei et al. 2021). Other drugs, such as curcumin, paclitaxel, carboplatin, and CDDP also have been incorporated in the liposomes and showed great effect in inducing the apoptosis of cancer cells (Gusti-Ngurah-Putu et al. 2019; Zhang et al. 2015). In summary, with characteristics of good biocompatibility and controlled drug release, liposomes are widely used as drug delivery system for the therapy of OSCC. After modification by a polymer coating, NPs obtained increased the stability and blood circulation time, reaching the target sites of OSCC through leaky blood vessels and pressure in tumor-specific organs. Despite promising preclinical evidence for the use of liposome in oral cancer therapy, some limitations prevent the use of liposomes in clinical practice, mainly due to their limited capacity to deliver drug. Also, the underlying immune response in the organism cannot be ignored.
Gold nanoparticles for OSCC-targeted therapy
Gold NPs have been widely used in biomedicine fields due to their good biocompatibility, tunable optical properties, and high tissue permeability. In the nanometer size range, gold NPs have different geometric shapes, such as nanoshells, nanospheres, nanocages, nanorods, and nanocrystals. AuNPs in these shapes can be used as carriers to achieve delivery of drugs to tumor cells and exert therapeutic effects. Some studies reported AuNPs can limit cancer cell proliferation and improve the efficacy of chemotherapy and radiotherapy (Mackey and El-Sayed 2014; Teraoka et al. 2018; Wu et al. 2011). Photosensitizer, such as rose bengal (RB) and sulfonated aluminum phthalocyanines, have been combined with AuNPs to obtain synergistic effect of photothermal therapy (PTT) and PDT on OSCC (Chu et al. 2016; Wang et al. 2014). To obtain enhanced antitumor efficacy, AuNPs were always coupled with specific OSCC-homing ligands, such as antibodies, aptamer, or peptides. For example, through folate-mediated active targeting, folate–gold bilirubin (FGB) NPs can deliver bilirubin (a potential anticancer agent) to tumor sites and inhibit tumor growth (Rathinaraj et al. 2020). Given the fact that PDPN is a transmembrane protein and highly expressed in several squamous cell carcinomas, Liu et al. prepared a PDPN antibody–AuNP–DOX system and performed a combined chemo-photothermal therapy against oral cancer. PDPN antibody-modified AuNPs can achieve accumulation of the drug and NPs in the tumor site actively, thus realizing the synergistic chemo-photothermal therapy against oral cancer (Liu et al. 2020). Melancon et al. have developed a multifunctional superparamagnetic iron oxide coated with gold nanoshell (SPIO@Au NS), which were further modified with the C225 monoclonal antibody against EGFR overexpressed in more than 90% of OSCC. This system can be selectively heated up and induce tumor destruction (Melancon et al. 2011). In addition, other studies also reported that upconversion nanoparticles (UCNPs) combined with gold nanorod (AuNR) can enhance plasmon-PDT (Chen et al. 2016; Chen et al. 2015a, b). With its unique photothermal function and higher photostability, AgNPs have been widely used in the diagnosis and treatment of OSCC. Since AgNPs are difficult to biodegrade and remove in vivo, it is of great significance to study methods to promote the removal of non-metabolizable AgNPs, which will further promote the application of AgNPs in drug delivery, photoacoustic imaging, and PTT therapy for OSCC.
Hydrogels for OSCC-targeted therapy
As a three-dimensional porous structure, hydrogels not only provide an ideal environment for cell adhesion, proliferation and metabolism, but harbor some advantages in targeted drug delivery (Yan et al. 2020). Injection of various hydrogel formulations directly into the site of injury can be used to locally target drug delivery, avoiding small NPs injected intravenously into the blood circulation. Besides, in contrast to other carriers, hydrogels provide controlled release management of hydrophilic and hydrophobic agents as well as other biomolecules. Li et al. successfully developed a novel poly (ethylene glycol)–poly (ε- caprolactone)–poly (ethylene glycol) (PEG–PCL–PEG,PECE) hydrogel loaded with suberoylanilide hydroxamic acid (SAHA) and CDDP. When it was injected into mice, the drug delivery system showed continued release of SAHA and CDDP in vivo, which improved the therapeutic effect compared with the simple superposition of SAHA and CDDP (Li et al. 2012). Tan et al. prepared a nanohybrid in which metal organic frameworks (MOFs), DOX and celecoxib were coloaded into thermosensitive hydrogels to act against oral cancer. The resulting hybrid nanocomposite showed positive outcomes in achieving high-efficiency drug loading, pH-responsive release and enhanced toxic effects against oral cancer cells (Tan et al. 2020). Additionally, drugs-loaded hydrogel can also achieve coordinated treatment of OSCC with chemotherapy and phototherapy. For example, Wang et al. synthesized matrix metalloproteinase (MMPs)-responsive hydrogel, incorporated with DOX and ICG. Results showed that DOX and ICG were released effectively in the presence of MMPs, greatly enhancing the retention of nanomaterials at the tumor site, thus killing oral cancer cells with 808 nm near-infrared (NIR) irradiation (Wang et al. 2019a, b, c, d, e). In a word, hydrogel has realized the targeted therapy of OSCC in preclinical stage through specific site injection and controllable drug release. But some obstacles such as the high cost, initial burst, and poor mechanical properties limit further use.
Stimuli-responsive drug delivery for OSCC-targeted therapy
The occurrence and development of tumor is a slow and dynamic process. TEM exhibits some unique characteristics during cancer development, including lower pH, overexpression of specific enzymes, higher levels of ROS and antioxidant up-regulation, which enables targeted therapy for oral cancer through stimulus-responsive drug delivery system (Koontongkaew 2013; Weinberg et al. 2019). In the past few years, many studies have fabricated novel stimuli-responsive DDSs for oral cancer. Moreover, these stimuli-responsive DDSs can be further modified to produce multifunctional DDSs, which can be used for active drug administration, integrated diagnosis and combination therapy.
pH-responsive drug delivery for OSCC-targeted therapy
As known, the pH of normal tissue is about 7. 4. In the TEM, due to hypoxia and high anaerobic glycolysis rate, the production of acidic metabolites of tumor cells is increased, resulting in an acidic environment with pH of about 6. 5. Although acidic TEM increases the risk of local invasion, metastasis and therapeutic drug resistance, it also provides an opportunity for the application of pH-responsive drug delivery (Fig. 2A).
In the treatment of OSCC, the mechanism of pH-responsive drug delivery system can be divided into two categories (Li et al. 2019a, b; Taghizadeh et al. 2015). One is that in response to varied pH values, the polymeric systems containing ionizable groups change conformation or dissolve, leading to controlled-drug release. For example, based on hollow mesoporous MnO2 nanoshells, a pH-sensitive intelligent “theranostic” platforms was prepared, which can decompose in the acidic TME and release docetaxel and CDDP, showing a series of antiangiogenic and oxidative antitumor reactions in OSCC treatment (Zhou et al. 2021). Other delivery systems for achieving pH-responsive drug release have been reported such as polymers, graphene quantum dots and hydrogels (Li et al. 2017; Tan et al. 2020; Wei et al. 2018). Another pH-responsive DDS relies on the breaking of acid-sensitive bonds attached on polymers to trigger the release of anticancer drug. For example, in recent two studies, nanomedicines were effectively released via the breaking of acid-labile amide bond in acidic condition, leading to a promising therapeutic performance (Li et al. 2021; Liu et al. 2020). Similarly, Saiyin et al. also reported that DOX was encapsulated into the carriers by acylhydrazone linkages, which broke in TEM, achieving drug release and exerted an increased proliferation inhibition of tumor cells (Saiyin et al. 2014).
Matrix metalloproteinases-responsive drug delivery for OSCC-targeted therapy
MMPs, a family of zinc-containing endopeptidases, play an important role in the degradation of extracellular matrix proteins (Kessenbrock et al. 2010). Normally, the concentration and activity of MMPs are very low in healthy tissues, but they are up-regulated under many pathological conditions, including cancer. This process is usually associated with cancer initiation, growth, and metastasis (Coussens et al. 2002; Gabriel et al. 2011). Specifically for OSCC, many MMPs such as MMPs 2, MMPs 7, and cathepsin B are considered closely related to cancer invasion, progression, recurrence, and metastasis (Aznavoorian et al. 2001; Kawasaki et al. 2002). At the same time, MMPs are also a trigger of stimulus responsive DDSs in recent years (Yao et al. 2018) (Fig. 2B).
For example, based on engineered human ferritin heavy chain, Damiani et al. constructed a novel nano-ferritin complex, which can efficiently entrap and deliver DOX to cancer cells. The carrier contains a short motif sequence and is responsive to MMPs, triggering drug delivery (Damiani et al. 2017). Similarly, in another study, DOX was encapsulated in biodegradable micelles and further loaded into injectable HA hydrogel cross-linked by MMP-2-responsive peptide (GCRDGPQGIWGQDRCG). The DDSs exhibited sustained release of DOX and cytotoxicity against OSCC (Li et al. 2019a, b). Others also reported that MMPs-responsive DDSs also provide a combined chemotherapy and phototherapy for the treatment of OSCC (Tan et al. 2020; Tarassoli et al. 2016; Wang et al. 2019a, b, c, d, e). Tarassoli et al. developed ICG-containing polyglutamate (PGA) NPs, which can be digested by cathepsin B, a matrix metalloproteinase overexpressed in OSCC. Upon NIR exposure, the DDSs demonstrated improved cytotoxicity and antitumor effect in vitro (Tarassoli et al. 2016). Therefore, it is a great potential to have more various kinds of MMPs-responsive DDSs for oral cancer therapy in future.
Reactive oxygen species (ROS)-responsive drug delivery for OSCC-targeted therapy
ROS, derived from mammalian organelles and NADPH oxidase, are oxygen-carrying active molecules and high concentration of ROS have been associated with various types of cancers, including oral cancer (Alfadda and Sallam 2012). Therefore, it is promising to construct ROS-responsive DDSs to realize tumor site-specific drug release and targeted therapy of oral cancer.
The ROS-responsive DDSs carriers were commonly combined with thioketal (TK) linker that would break in the presence of intracelluar ROS (Fig. 3A). For instance, Li et al. developed an ROS-triggered TK-containing linker and conjugating RGD-containing peptide drug delivery nanoplatform. The NPs showed ROS-triggered drug release and significant inhibition of Cal-27 cells (Li et al. 2016a, b). Similarly, other studies also constructed TK linked DDSs loaded with DOX for OSCC therapy (Li et al. 2016a, b; Wang et al. 2019a, b, c, d, e). To achieve a tumor-targeting effect, Wang et al. modified the DDSs with FA. With the site-specific release of DOX, the DDSs induced the apoptosis of Cal-27 cells, which exhibited an enhanced antitumor efficacy (Wang et al. 2019a, b, c, d, e). In addition to being used for chemotherapy delivery for OSCC, ROS-responsive DDSs have also been reported to be combined with light or pH response to achieve effective treatment for OSCC. In 2019, Wang et al. designed a polymeric NPs system containing both chemotherapeutic agent and photosensitizer for OSCC therapy. Upon the inner ROS stimulus, the TK link was broken and DOX released. Meanwhile, ROS generated by PDT further triggered the degradation of nanocarriers to prompt the release of drugs, which induced an added inhibitory effect on tumor growth (Wang et al. 2019a, b, c, d, e). In 2018, Jin et al. fabricated a novel trimodal photochemotherapy nanoplatform based on mesoporous silica NPs (MSNs)–Fe–AuNPs. Under low pH and a considerable amount of H2O2 tumor condition, the NPs trigger the three therapeutic actions and the tumor can be inhibited after 2 weeks of treatment (Jin et al. 2018). However, the research of ROS-responsive DDSs in OSCC therapy is still limited. Future studies need to further explored in in vivo applications and more controlled in situ ROS levels.
Redox-responsive DDSs drug delivery for OSCC-targeted therapy
As described above, the production of ROS in tumor areas induced a high level of oxidative stress, which led to compensatory up-regulation of antioxidants. It is reported that the concentration of glutathione in tumor tissues is higher than that in normal tissues, and glutathione (GSH)/glutathione disulfide (GSSG) coupling is the most ample redox coupling in cancer cells (Guo et al. 2018). In recent years, the wide study of redox-responsive DDSs has provided another new strategy for the treatment of OSCC (Fig. 3B). Among all redox-responsive bonds, disulfide bonds and diselenide bonds are most broadly involved redox-responsive linkages, which could be cleaved by GSH, and induced controlled drug release (Huo et al. 2014). For example, Fan et al. developed GSH-sensitive and FA-targeted NPs-entrapped paclitaxel (FA–PEG–S–S–PCL@PTX, FA-NPs). In vitro experiments showed PTX would be site specifically released due to disulfide bonds breaking by redox reaction, while FA-NPs can accumulate in tumor and exhibited potent antitumor effects in vivo (Fan et al. 2020a, b). Similarly, Zhang et al. prepared a pH/GSH combined responsive drug delivery system by molecular imprint technique. In this study, with DOX as the template, surface molecular imprinting polymer (SMIP) was prepared on the surface of MSN, which was degraded under high concentration of GSH and acidic conditions, leading to controlled release of DOX. Results confirmed that DOX in SMIP can invade Tca-8113 cancer cells and inhibit its growth (Zhang et al. 2016). The application of multifunctional redox-responsive DDSs in oral cancer should be further studied in future.
Light-responsive DDSs drug delivery for OSCC-targeted therapy
Among various stimuli used for controlled drug release, light-responsive DDSs have been extensively studied with characteristics of non-invasive feature and high spatial and temporal precision. In recent years, light stimulus-responsive therapies have exhibited promising treatment efficacy in many preclinical animal studies and clinical trials. The light-responsive DDSs mainly included PDT and PTT (Fig. 4).
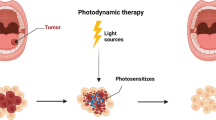
PDT has been regarded as an important method for OSCC treatment, with minimal invasiveness, low systemic toxicity, and negligible drug resistance (Meulemans et al. 2019). In the PDT process, under light with specific wavelength, photosensitizers are activated and then oxygen converted into ROS such as singlet oxygen in cells, resulting in apoptosis, necrosis or autophagy. To achieve favorable PDT, two generations of photosensitizers, including complex mixtures of porphyrins and 5-aminolevulinic acid have been developed, exhibiting their good therapy effect for OSCC (Fan et al. 2020a, b). However, some disadvantages such as hypoxia-induced drug resistance and associated toxicity have limited the application of PDT. At present, more and more studies have developed third-generation photosensitizers, that is, using DDSs to load photosensitizers. A number of nanocarriers have been applied for site-specific drug delivery of OSCC, such as carbon-based NPs, AuNPs, magnetic NPs, lipid-based NPs and other copolymer NPs (Fan et al. 2020a, b).
Based on the fact that cancer cells are more sensitive to temperature, PTT is the recognized effective strategy for cancer therapy. On locally illuminating the tumor areas, PTT agents effectively change light energy into heat, which in turn generates a higher temperature in tumor cells and “burn” them efficiently. Many optical absorbing nanomaterials have been used in PTT therapy. Specifically, AuNPs are commonly applied in PTT (Jiang et al. 2015). However, due to the defense mechanism of cellular heat-shock response and the non-targeted selectivity of nanomaterials, the therapeutic effect of PTT is not ideal. In 2016, Wang et al. prepared a gold nanorod (GNRs)–siRNA platform by loading siRNA oligos targeting BAG3, an efficient gene to block the heat-shock response, which showed improved PTT efficiency (Wang et al. 2016).
Some studies proved that the combination therapy can increase the clinical efficacy of OSCC treatment through potential synergies. For example, in 2014, Wang et al. conjugated GNRs with RB, applying PTT and PDT into the same platform. With the increase of RB uptake by oral cancer cells, RB–GNRs showed improved photodynamic efficacy. In vivo experiments showed RB–GNRs harbored synergetic PDT–PTT effects better than PDT or PTT alone (Wang et al. 2014). By applying gold nanorings and sulfonated aluminum phthalocyanine photosensitizer to OSCC treatment, Chu et al. also demonstrated the improved therapeutic effect of PDT–PTT (Chu et al. 2016). Ren et al. encapsulated ICG and organic compound (C3) in PEG–PCL, forming hybrid NPs (PEG–PCL–C3–ICG NPs). Under the irradiation of 808 nm laser at the tumor sites, the PEG–PCL–C3–ICG NPs inhibited the tumor growth by the PDT–PTT synergistic effect (Ren et al. 2017). Except the treatment of PTT and PDT, some studies have also confirmed the role of phototherapy combined with chemotherapy or gene therapy in OSCC-targeted therapy. For example, to improve the inefficiency of chemotherapy, Wang et al. constructed a novel DDS which simultaneously encapsulated ICG and CDDP. Under NIR irradiation, ICG–CDDP coordination bonds break, and ICG and CDDP are released into OSCC tissues, resulting in the synergistic therapeutic functions of PDT, PTT, and chemotherapy (Wang et al. 2019a, b, c, d, e). Based on MMPs-responsive DDSs, Wang et al. also constructed a collaborative nanotherapy platform integrating the effects of PTT, PDT and chemotherapy, which achieved good antitumor efficacy (Wang et al. 2019a, b, c, d, e).
In a short, based on the OSCC environment, which is different from normal tissue, stimulus-responsive targeted therapy has made progress in preclinical research. However, the unstable and uncontrollable tumor environment also limits the wide application of the internal stimuli-responsive DDSs. Therefore, to improve the sensitivity and controllability of stimulus-responsive DDSs, more strategies are needed. Moreover, it may be a good choice to combine with external stimuli-responsive ability.
Active targeted therapy of OSCC
Compared with passive targeted therapy, active targeted therapy usually targets specific receptors on the surface of tumors, and actively recognizes specific targets on the surface of nanocarriers through modified ligands, effectively enhancing the specificity and targeting of drugs. Active targeting therapy, including immunotherapy, gene therapy and bionic technology, provides a new paradigm in the treatment of OSCC, which is illustrated in Fig. 5.
Gene therapy of OSCC
In recent years, gene therapy has been widely used as a treatment for genetically inherited, monogenic disorders, especially in the field of oncology (Farmer et al. 2019). Several general strategies have been utilized in OSCC treatment, including: (1) up-regulation of genes that inhibit tumor growth or down-regulation of genes that promote tumor growth; (2) delivery of small RNA-targeting drug resistance genes to protect chemotherapy; (3) “suicide” gene therapy. Ma et al. delivered Wnt-1 small interfering RNA (siRNA), which inhibits the expression of epithelial–mesenchymal transformation (EMT)-related genes into the cytoplasm of KB cells and effectively restricted the invasion and migration of cancer cells (Ma et al. 2017). Peng et al. studied the role of circRNA_0000140 in OSCC growth and metastasis. Both in vitro and in vivo results showed that circ_0000140 could repress tumor growth, which was attributed to the fact that circ_0000140 combined with miR-31 can up-regulate the target gene LATS2 and affect the OSCC cellular EMT (Peng et al. 2020). Similarly, Liu et al. explored the role of circular RNAs in OSCC. They confirmed that knockdown of circIGHG can damage the expression of IGF2BP3 and attenuate the invasiveness of OSCC cells. Therefore, circIGHG can be used as a biomarker for early-stage diagnosis and is a great potential target for the treatment of OSCC (Liu et al. 2021). Wu et al. also found that MiR345 induces OSCC cell cycle arrest by inhibiting the expression of its target gene ZEB2, regulating OSCC development negatively (Wu et al. 2020a, b).
Multidrug resistance has always been a significant hurdle during cancer chemotherapy, so it is of great importance to prevent or reverse the effect of multidrug resistance in this process (Gottesman et al. 2002). Multiple drug resistance protein 1 (MDR1) is a cell membrane protein which plays an important part in pumping foreign substances out of cells. Unfortunately, higher levels of MDR1 can also be detected in OSCC, leading to drug resistance and failure of cancer treatment. To avoid the effect of multidrug resistance, Wang et al. fabricated MSNs, encapsulated with DOX and MDR1-siRNA to block MDR1 expression, and then transfected into cancer cells in vitro. MSNs could down-regulate the gene expression of MDR1 and induced the apoptosis of cancer cells (Wang et al. 2017a, b). Study showed that the expression level of long non-coding RNA urothelial cancer associated 1 (UCA1) was strikingly up-regulated and exerted an oncogenic effect in the progress of OSCC (Yang et al. 2016). Fang et al. investigated the role of UCA1 in the progression of OSCC through siRNA targeting UCA1. Results proved that silencing UCA1 not only inhibited the migration and invasion of OSCC cells, but also promoted the early apoptosis in vitro and suppressed the tumor growth in vivo (Fang et al. 2017).
Suicide genes usually encode non-mammalian enzymes which can change non-toxic prodrugs into toxic metabolites. Inducing apoptosis of cancer cells by suicide gene is one of the methods of cancer gene therapy (Ren and Mei-Juan 2009). To improve targeting efficiency, magnetic NPs have been widely used as vehicles for gene therapy (Ren and Mei-Juan 2009). In 2014, PEI-modified Fe3O4 NPs were used to mediate transfection of OSCC by human-TRAIL gene driven with a human telomerase reverse transcriptase tumor-specific promoter (pACTERT-TRAIL) inducing apoptosis to observe its antitumor function in vitro and in vivo. Compared with conventional PEI/lipofectin, pACTERT-TRAIL NPs harbored a higher transfection efficiency and mediated the killing of Tca-8113 cells (Ren and Mei-Juan 2009). Given the unique expression of the SERPINB3 gene in OSCC, Wu et al. prepared a pSERPINB3-PE38KDEL toxin plasmid containing the SERPINB3 gene fragment and then studied the targeted inhibition of the plasmid in the treatment of OSCC. In vitro experiments proved that the pSERPINB3-PE38KDEL plasmid inhibited the proliferation and invasion of Tca-8113 cells and induced cell apoptosis, which may be a novel strategy for targeted OSCC gene therapy (Wu et al. 2020a, b). To improve the transfer efficiency of suicide gene, Yu et al. prepared a hydrophilic–hydrophobic deblock copolymer based on PEG–poly (g-benzyl-lglutamate) (PBLG), which was further loaded with the herpes simplex virus thymidine kinase (HSV-TK) gene. HSV-TK-loaded PEG–PBLG NPs showed higher gene transfer efficiency and a superior killing effect on Tca-8113 cells in vitro (Yu et al. 2008).
In addition, gene therapy combined with other therapies has shown synergistic effects in the treatment of OSCC (Wang et al. 2016, 2021). For example, Wang et al. prepared chitosan NPs loaded with 5-aminolevulinic acid (ALA) photosensitizer and the GBAS gene plasmid DNA (shGBAS) to identify the effect of PDT and gene therapy for OSCC in vitro and in vivo. The resulting co-delivery system displayed a stronger targeted anticancer effect on OSCC (Wang et al. 2021). PDT has been shown to promote hypoxia in tumor areas, leading to overexpression of angiogenic markers such as VEGF. In recent two studies, lipid-–calcium–phosphate NPs (LCPNPs) were used to deliver HIF1α and VEGF-A siRNA to human squamous cell carcinoma cell lines, SCC4, or SAS-xenografted model. When combined with PDT, HIF1α siRNA LCP-NPs and VEGF siRNA LCP-NPs both reduced tumor growth (Chen et al. 2015a, b; Lecaros et al. 2016). Besides, gene therapy was used to block the heat-shock protein response, improving the therapeutic effect of PTT in OSCC treatment (Wang et al. 2016). All in all, as a new promising clue and approach, a large number of cancer researches have been working on the development of gene therapy. Compared with traditional treatment methods, gene therapy provides a new basis for target therapy of OSCC from the molecular level. However, many challenges still remain before gene therapy can be applied to the clinic. For example, to achieve target gene introduction and improve transfection efficiency, suitable vectors are needed. Besides, it would be highly valuable to understand theoretically and experimentally how the nanovectors transfer the gene into target cells. Last but not least, the expression stability and long-term safety of existing gene therapy methods still need to be further studied. In the coming years, with the development of therapeutic gene and technologies relating to transfer-gene expression, gene therapy against OSCC will be used in the clinic.
Immunotherapy of OSCC
Recently, immunotherapy is considered as a promising method in the treatment of some cancers. Immune checkpoint molecules, such as PD-1, and its ligands PD-L1 and CTLA-4, are the normal components of the immune system, which play an important role in normal immunoregulatory pathways (Smyth et al. 2016). However, some immune checkpoint inhibitors (ICIs) targeting PD-1, PD-L1 and CTLA-4 are highly expressed in the tumor environment, and can block these inhibitory pathways, contributing to tumor-promoting immunosuppression. Avelumab is a fully human anti-PD-L1 IgG1 monoclonal antibody. When combined with PD-L1, it can prevent its interaction with PD-1 and inactivate T cells (Heery et al. 2017). Cetuximab is a human–mouse IgG1 monoclonal antibody and can inhibit endogenous ligand-activated receptors by binding to the extracellular ligand binding domain of EGFR, resulting in enhanced cell apoptosis, down-regulated cell proliferation, invasion, metastasis, and angiogenesis (Liu et al. 2019). Besides, cetuximab also down-regulates EGFR expression via internalizing and degrading receptors and thus cut off the downstream cascade signal (Vigneswara and Kong 2018). ICIs can be combined with other therapeutics with complementary effects to improve the therapeutic effect (Chowdhury et al. 2018; Mahoney et al. 2015). Cetuximab, combined or not with cisplatin, showed significant tumor regression rates in platinum-refractory head and neck cancer patients (Baselga et al. 2005; Herbst et al. 2005). In addition, conjugated with therapeutic drugs, checkpoint inhibitors can also produce a cytotoxic effect on cancer cells (Vermorken et al. 2008). Huang et al. examined the effects of the anti-EGFR monoclonal antibody C225 on SCC cell lines. Results showed that C225 culture inhibited SCC proliferation in a time-dependent manner and increased its sensitivity to chemotherapy (Huang et al. 1999). Novaes et al. proved that PD-1 antibody treatment inhibited the progression of precancerous lesions to carcinoma in a 4-nitroquinoline 1-oxide (4NQO)-exposed mouse OSCC model, and this inhibition was low in PD-L1 knockout mice treated with 4NQO (de Oliveira et al. 2021). Further, when combined with radiotherapy, cetuximab improved survival in patients with locally advanced head and neck squamous cell carcinoma (Bonner et al. 2006). Due to the heterogeneity of OSCC patients, many risk factors, such as smoking and drinking, are involved in the occurrence and development of OSCC, so immunotherapy is not the preferred strategy for OSCC treatment. It has been proved that the benefits of ICIs are limited to a small number of patients. Therefore, elucidating the mechanisms associated with immunotherapy and identifying predictive markers of response and resistance are critical to develop rational trial design in the new era of OSCC immuno-oncology.
Highly expressed markers for OSCC-targeted therapy
Numerous studies have directed their attention on changes in gene or protein expression, as well as abnormal genetic and epigenetic mutations in tumor cells. It has been proved that guiding drugs or DDSs targeted at the tumor site using specific molecular markers and receptors that are specifically overexpressed in cancer tissues is a promising therapeutic strategy (Xu et al. 2013). Widely used molecular markers and receptors in OSCC treatment include EGFR receptor, folate receptor, CD44, integrin αvβ6, urokinase plasminogen activator receptor (uPAR) and so on. In 2016, to widen the application of PDT in oral cancer, Lucky et al. developed PEGylated TiO2–UCNPs, which was further modified with EGFR. Compared with conventional photosensitizer Chlorine6 (Ce6), the treatment efficiency of UCNPs-based 980 nm NIR PDT showed delay in tumor growth (Lucky et al. 2016). Some other studies tried to conjugate NPs with anti-EGFR antibodies for targeted photothermal therapy of OSCC cells (Huang et al. 2007; Melancon et al. 2011). Other studies have shown that FA-modified NPs can specifically target tumor sites due to the overexpression of folate receptor in cancer cells (Cheng et al. 2021; Rathinaraj et al. 2020). Currently, folate-mediated DDSs for targeted therapy of OSCC include magnetic NPs, gold NPs and lipid–polymer hybrid NPs. CD44 is a cell-surface glycoprotein highly expressed at the OSCC cellular membranes (Cai et al. 2014). Some studies have reported that it is effective to achieve targeted therapy of OSCC with CD44 participates (Su et al. 2019; Wang et al. 2019a, b, c, d, e). Since integrin αvβ6 and uPAR are also well-characteristic OSCC biomarker, anti-αvβ6 antibodies and AE105 (H-Asp-Cha-Phe- (d)Ser- (d)Arg-Tyr-Leu-Trp-SerOH) peptide against uPAR have been used in the targeted treatment of OSCC (Legge et al. 2019; Zuo et al. 2020). In addition, protein, highly expressed in numerous tumors including OSCC, has also been designed and applied in the clinic. For example, Wang et al. developed a new nanocarrier of human serum albumin indocyanine green cisplatin NPs (HSA–ICG–CDDP NPs). They proved that the secreted protein acidic and rich in cysteine (SPARC) protein, which is highly expressed in OSCC, can bind to HSA and enable HSA–ICG–CDDP NPs to inhibit tumor growth, enabling targeted therapy for OSCC (Wang et al. 2019a, b, c, d, e).
In recent years, with the widespread use of nanodetection systems in cancer detection and diagnosis, a number of novel biomarkers are being researched, which not only provide opportunities for diagnosis, treatment and prognosis of OSCC, but reduce off-target side effects, achieving targeted therapy. Unfortunately, treatment options for patients with late-stage oral cancer are limited. Therefore, a more comprehensive understanding of the molecular pathogenesis of OSCC, especially the interaction between OSCC and their microenvironment, is an unmet need to explore effective systemic therapies.
Biomimetic NP for OSCC-targeted therapy
Cell membrane for OSCC-targeted therapy
Cellular plasma membranes have been reported to take part in many important biological processes. More important, the cellular plasma membranes inherit the merits of the parent cells and have high biocompatibility. As a result, many cell membranes have been explored to generate bioinspired DDSs for the therapy of corresponding diseases. Due to their unique properties, such as immune evasion, longer circulation time and homologous targeting, many cell membranes have been used to camouflage NPs, including red blood cell (RBC) membranes, cancer cell membranes, macrophage membrane and so on (Zhen et al. 2019). Rao et al. pioneerly loaded AuNR into platelets (PLTs) via the electroporation process. The hybrid membrane-coated NPs exhibited longer systematic circulation compared with bare AuNPs. Moreover, upon laser irradiation, the PTT-ablated tumor tissues further recruited PLTs and enhanced tumor accumulation of PLT@AuNRs, proving the unique self-reinforcing characteristic of PLT–PTT in OSCC therapy (Rao et al. 2018). However, PLTs do not endow the ability to target tumor site. Some plasma membrane proteins, such as N-cadherin, galactose agglutinin-3 or epithelial cell adhesion molecule (EpCAM), existed on the cancer cells surface, enabling cancer cells to acquire the ability of homologous targeting and immune escape, which can be leveraged for specific and effective cancer therapy (IURISCI et al. 2009; Osta et al. 2004; Yue et al. 2010). To achieve targeted therapy of OSCC, squamous cell membranes have been widely used in recent years (Rao et al. 2016; Sun et al. 2020; Zhu et al. 2016). Zhu et al. devised a MNP@DOX@CCCM nano-vehicle based on doxorubicin hydrochloride-modified magnetic iron oxide nanoplatform which was further be modified with human SCC membrane. Notably, MNP@DOX@CCCM nano-vehicle not only showed specifically self-recognition to the parent cell lines in vitro, but also superior self-targeting “homing” ability and strong potency for tumor treatment to the homologous tumor in vivo (Zhu et al. 2016). Similarly, Rao et al. developed nanoprobes based on UCNPs coated with cancer cell membrane (Cal-27) for tumor imaging specifically. The obtained NPs displayed characteristics of immune escaping and homologous targeting abilities (Rao et al. 2016). In addition, NPs camouflaged by cancer cell membranes are also used in photothermal therapy for oral cancer. In 2016, Sun et al. prepared AuNR with suitable longitudinal surface plasmon resonance (LSPR) in the second near-infrared (NIR-II) window and further camouflaged with the plasma membrane of oral squamous KB cancer cells. The obtained GNR@Mem demonstrated specific homotypic targeting to parent cells in vitro. Besides, under suitable NIR light and X-ray irradiation, GNR@Mem suppresses tumor growth for the combination of PTT and radiotherapy (Sun et al. 2020). Up to now, due to the homotypic targeting ability of cancer cell membranes, NPs coated with cancer cell membranes can proactively deliver their cargo to the cancer site, achieving targeted, precise and controllable drug release. However, some shortcomings have prevented their clinical translation: first, due to the lack of mature productive technique for preparing membrane-coated biomimetic NPs, there are some unique challenges in achieving industrial scale and manufacturing of biomimetic NPs. Second, it has not been revealed how to accurately characterize the integrity of membrane camouflage NPs in vivo, which is important to keep the functionality during blood circulation. Third, membrane-camouflaged NPs exhibit biocompatibility and cytotoxicity in vivo, but it is necessary to further study their biological effects on living organisms (Zhen et al. 2019). Despite these challenges, these biomimetic NPs and their synthetic materials offer unique and valuable strategies for targeted therapy of OSCC.
Exosomes for OSCC-targeted therapy
Exosomes are vesicles with a diameter of 30–120 nm secreted by various types of cells (Batrakova and Kim 2015). Exosomes contain many types of biomolecules, such as mRNAs, microRNAs, lipids and proteins, so they play a significant role in intercellular communication (Bunggulawa et al. 2018). Several pioneering reports have shown that exosomes are ideal nanocarriers owing to their characteristics of small size and deformable cytoskeleton (Bunggulawa et al. 2018). More importantly, exosomes can not only escape the degradation or clearance by the immune system, but cross biological barriers, even the blood–brain barrier (Batrakova and Kim 2015; Hood 2016). Given exosomes can efficiently fuse with cell membranes, non-coding RNA or peptide, drugs can be packaged into exosomes and delivered to OSCC tumors for treatment. Furthermore, exosomes combined with tumor-targeting proteins, antibodies or peptides can achieve targeted therapy of OSCC (Lu et al. 2021).
In addition, some studies have also reported active targeted therapy of OSCC via exosomes. In 2019, Rosenberger et al. studied the effect of exosomes derived from menstrual mesenchymal stem cell (MenSC-exosomes) on endothelial cells and assessed their effect on angiogenesis and tumor growth on the OSCC model. This work demonstrated for the first time that MenSC-exosomes exerted cytotoxic effects on endothelial cells and inhibited tumor growth by decreasing tumor angiogenesis (Rosenberger et al. 2019). In 2020, Tomita et al. suggested that macrophage-derived exosomes play an important role in reducing the sensitivity of OSCC cells to chemotherapeutic drugs by activating the AKT/GSK-3β signaling pathway, which reduced the proliferation inhibition of 5-FU and CDDP and apoptosis of OSCC cells (Tomita et al. 2020). Compared with activated antigen-presenting cells, exosomes are more stable and can be easily engineered, so it is a promising therapy for oral cancer treatment by functional exosomes. All in all, due to their biocompatibility, nontoxicity, low immunogenicity, long life span and high delivery efficiency, exosomes may be used as a novel nanocarrier to a great extent. Besides, exosomes contain a diversity of proteins, mRNAs, and non-coding RNAs, which could serve as non-invasive biomarkers and therapeutic targets for the screening and treatment of OSCC (Lu et al. 2021). Moreover, to avoid metastasis and improve the prognosis of OSCC, exosomes derived from OSCC may be an important diagnostic tool (Chen et al. 2012). However, there is still a significant gap to overcome before exosomes can be used for the diagnosis, prognosis, and targeted therapy of OSCC, such as efficient separation of exosomes, strict purity process, efficient drug delivery rate, and elimination of potential biosafety risks (Ha et al. 2016).
Conclusion and future outlook
In this article, the current progress of passive and active targeted therapy of OSCC was reviewed. The ultimate goal of targeted therapy for OSCC is to produce a "magic bullet", which can escape immune system recognition, specifically target tumors, and effectively enter cancer cells. Due to the fact that passive targeting is usually influenced by the distribution of blood vessels in tumor tissues, and the tumor environment is unstable and uncontrollable, the degree of targeting for various tumors is not the same. To improve the targeting of NPs, active targeting components (e.g., small molecules, monoclonal antibodies, peptides) and stimulus-responsive DDSs have been widely used in preclinical studies of OSCC therapy.
Although targeted therapy is a promising approach of oral cancer, most studies still need further exploration. Few NPs can evade multiple biological barriers, and none of these NPs are Food and Drug Administration (FDA) and/or European Medicines Agency (EMA) approved (Blanco et al. 2020; Wicki et al. 2015). Given most investigations are still focused on in vitro or in vivo studies and few clinic studies have been performed so far, it is indicated that achieving precise drug delivery, reducing drug side effect and translating research into clinical application are highly challenging. A personalized and reliable DDS explicitly tailored on the specific genetic, molecular, and histological aspects of a given tumor in specific patients seems an ideal approach in OSCC treatment. At the same time, with the advancement of high-throughput sequencing technology, the emergence of a large amount of information from transcriptome, genomics, epigenome, and metabolomics will provide novel approaches for the treatment of OSCC. Obviously, recent data suggest that we are at the dawn of a new era. It is expected that the prevention and treatment of OSCC will lead to major breakthroughs, improving human survival rate in the future.
References
Alfadda AA, Sallam RM (2012) Reactive oxygen species in health and disease. J Biomed Biotechnol 2012:936486. https://doi.org/10.1155/2012/936486
Argiris A, Karamouzis MV, Raben D, Ferris RL (2008) Head and neck cancer. The Lancet 371:1695–1709. https://doi.org/10.1016/S0140-6736(08)60728-X
Aznavoorian S, Moore BA, Alexanderlister LD, Hallit SL, Windsor LJ, Engler JA (2001) Membrane type I-matrix metalloproteinase-mediated degradation of type I collagen by oral squamous cell carcinoma cells. Cancer Res 61: 6264–6275. https://cancerres.aacrjournals.org/content/canres/61/16/6264.full.pdf.
Baselga J, Trigo J, Bourhis J, Tortochaux J, Cortés-Funes H, Hitt R, Gascón P, Amellal N, Harstrick A, Eckardt A (2005) Phase II multicenter study of the antiepidermal growth factor receptor monoclonal antibody cetuximab in combination with platinum-based chemotherapy in patients with platinum-refractory metastatic and/or recurrent squamous cell carcinoma of the head and neck. J Clin Oncol 23:5568–5577. https://doi.org/10.1200/JCO.2005.07.119
Batrakova EV, Kim MS (2015) Using exosomes, naturally-equipped nanocarriers, for drug delivery. J Control Release 219:396–405. https://doi.org/10.1016/j.jconrel.2015.07.030
Blanco E, Shen H, Ferrari M (2020) Principles of nanoparticle design for overcoming biological barriers to drug delivery. Nat Biotechnol 33:941–951. https://doi.org/10.1038/nbt.3330
Bonner JA, Harari PM, Giralt J, Azarnia N, Shin DM, Cohen RB, Jones CU, Sur R, Raben D, Jassem J, Ove R, Kies MS, Baselga J, Youssoufian H, Amellal N, Rowinsky EK, Ang KK (2006) Radiotherapy plus cetuximab for squamous-cell carcinoma of the head and neck. N Engl J Med 354:567–578. https://doi.org/10.1056/NEJMoa053422
Boonkitticharoen V, Kulapaditharom B, Leopairut J, Kraiphibul P, Larbcharoensub N, Cheewaruangroj W, Chintrakarn C, Pochanukul L (2008) Vascular endothelial growth factor a and proliferation marker in prediction of lymph node metastasis in oral and pharyngeal squamous cell carcinoma. Arch Otolaryngol-Head Neck Surg 134:1305–1311. https://doi.org/10.1001/archotol.134.12.1305
Bunggulawa EJ, Wang W, Yin T, Wang N, Durkan C, Wang Y, Wang G (2018) Recent advancements in the use of exosomes as drug delivery systems. J Nanobiotechnology 16:1–13. https://doi.org/10.1186/s12951-018-0403-9
Cai S, Alhowyan A, Yang Q, Forrest W, Shnayder Y, Forrest ML (2014) Cellular uptake and internalization of hyaluronan-based doxorubicin and cisplatin conjugates. J Drug Target 22:648–657. https://doi.org/10.3109/1061186X.2014.921924
Chen X, Liang H, Zhang J, Zen K, Zhang CY (2012) Horizontal transfer of microRNAs: molecular mechanisms and clinical applications. Protein Cell 3:28–37. https://doi.org/10.1007/s13238-012-2003-z
Chen CW, Lee PH, Chan YC, Hsiao M, Chen CH, Wu PC, Wu PR, Tsai DP, Tu D, Chen X (2015a) Plasmon-induced hyperthermia: hybrid upconversion NaYF4:Yb/Er and gold nanomaterials for oral cancer photothermal therapy. J Mater Chem B 3:8293–8302. https://doi.org/10.1039/C5TB01393C
Chen WH, Lecaros R, Tseng YC, Huang L, Hsu YC (2015b) Nanoparticle delivery of HIF1α siRNA combined with photodynamic therapy as a potential treatment strategy for head-and-neck cancer. Cancer Lett 359:65–74. https://doi.org/10.1016/j.canlet.2014.12.052
Chen CW, Chan YC, Hsiao M, Liu RS (2016) Plasmon-enhanced photodynamic cancer therapy by upconversion nanoparticles conjugated with Au nanorods. ACS Appl Mater Interfaces 8:32108–32119. https://doi.org/10.1021/acsami.6b07770
Chen S-H, Hsiao S-Y, Chang K-Y, Chang J-Y (2021) New insights into oral squamous cell carcinoma: from clinical aspects to molecular tumorigenesis. Int J Mol Sci 22:2252. https://doi.org/10.3390/ijms22052252
Cheng C, Castro G, Liu Ch, Lau P (2019) Advanced nanotechnology: an arsenal to enhance immunotherapy in fighting cancer. Clin Chim Acta 492:12–19. https://doi.org/10.1016/j.cca.2019.01.027
Cheng X, Zhang L, Liu X, Xu L, Liu J (2021) Folic acid mediated cisplatin magnetic nanodrug targeting in the treatment of oral squamous cell carcinoma. Mater Express 11:1299–1305. https://doi.org/10.1166/mex.2021.2036
Chowdhury PS, Chamoto K, Honjo T (2018) Combination therapy strategies for improving PD-1 blockade efficacy: a new era in cancer immunotherapy. J Intern Med 283:110–120. https://doi.org/10.1111/joim.12708
Chu C-K, Tu Y-C, Hsiao J-H, Yu J-H, Yu C-K, Chen S-Y, Tseng P-H, Chen S, Kiang Y-W, Yang CC (2016) Combination of photothermal and photodynamic inactivation of cancer cells through surface plasmon resonance of a gold nanoring. Nanotechnology 27:115102. https://doi.org/10.1088/0957-4484/27/11/115102
Coussens LM, Fingleton B, Matrisian LM (2002) Matrix metalloproteinase inhibitors and cancer: trials and tribulations. Science 295:2387–2392. https://doi.org/10.1126/science.1067100
Damiani V, Falvo E, Fracasso G, Federici L, Pitea M, De Laurenzi V, Sala G, Ceci P (2017) Therapeutic efficacy of the novel stimuli-sensitive nano-ferritins containing doxorubicin in a head and neck cancer model. Int J Mol Sci 18:1555. https://www.mdpi.com/1422-0067/18/7/1555.
De Oliveira M, Novaes JA, Hirz T, Guijarro I, Nilsson M, Pisegna MA, Poteete A, Barsoumian HB, Fradette JJ, Chen LN, Gibbons DL, Tian X, Wang J, Myers JN, Mcarthur MJ, Bell D, William WN, Heymach JV (2021) Targeting of CD40 and PD-L1 pathways inhibits progression of oral premalignant lesions in a carcinogen-induced model of oral squamous cell carcinoma. Cancer Prev Res 14:313–324. https://doi.org/10.1158/1940-6207.CAPR-20-0418
Endo K, Ueno T, Kondo S, Wakisaka N, Murono S, Ito M, Kataoka K, Kato Y, Yoshizaki T (2013) Tumor-targeted chemotherapy with the nanopolymer-based drug NC-6004 for oral squamous cell carcinoma. Cancer Sci 104:369–374. https://doi.org/10.1111/cas.12079
Fan H-Y, Zhu Z-L, Zhang W-L, Yin Y-J, Tang Y-L, Liang X-H, Zhang L (2020a) Light stimulus responsive nanomedicine in the treatment of oral squamous cell carcinoma. Eur J Med Chem 199:112394. https://doi.org/10.1016/j.ejmech.2020.112394
Fan L, Wang J, Xia C, Zhang Q, Pu Y, Chen L, Chen J, Wang Y (2020b) Glutathione-sensitive and folate-targeted nanoparticles loaded with paclitaxel to enhance oral squamous cell carcinoma therapy. J Mater Chem B 8:3113–3122. https://doi.org/10.1039/C9TB02818H
Fang Z, Zhao J, Xie W, Sun Q, Wang H, Qiao B (2017) LncRNA UCA1 promotes proliferation and cisplatin resistance of oral squamous cell carcinoma by sunppressing miR-184 expression. Cancer Med 6:2897–2908. https://doi.org/10.1002/cam4.1253
Farmer ZL, Kim ES, Carrizosa DR (2019) Gene therapy in head and neck cancer. Oral Maxillofac Surg Clin 31:117–124. https://doi.org/10.1016/j.coms.2018.08.006
Gabriel D, Zuluaga MF, Lange N (2011) On the cutting edge: protease-sensitive prodrugs for the delivery of photoactive compounds. Photochem Photobiol Sci 10:689–703. https://doi.org/10.1039/C0PP00341G
Gottesman MM, Fojo T, Bates SE (2002) Multidrug resistance in cancer: role of ATP–dependent transporters. Nat Rev Cancer 2:48–58. https://doi.org/10.1038/nrc706
Greenberg JS, Naggar AKE, Mo V, Roberts D, Myers JN (2003) Disparity in pathologic and clinical lymph node staging in oral tongue carcinoma. Implication for therapeutic decision making. Cancer 98:508–515. https://doi.org/10.1002/cncr.11526
Greish K (2012) Enhanced permeability and retention effect for selective targeting of anticancer nanomedicine: are we there yet? Drug Discov Today Technol 9:e161–e166. https://doi.org/10.1016/j.ddtec.2011.11.010
Guo X, Cheng Y, Zhao X, Luo Y, Chen J, Yuan W-E (2018) Advances in redox-responsive drug delivery systems of tumor microenvironment. J Nanobiotechnology 16:1–10. https://doi.org/10.1186/s12951-018-0398-2
Gusti-Ngurah-Putu EP, Huang L, Hsu YC (2019) Effective combined photodynamic therapy with lipid platinum chloride nanoparticles therapies of oral squamous carcinoma tumor inhibition. J Clin Med 8:2112. https://doi.org/10.3390/jcm8122112
Ha D, Yang N, Nadithe V (2016) Exosomes as therapeutic drug carriers and delivery vehicles across biological membranes: current perspectives and future challenges. Acta Pharm Sinica B 6:287–296. https://doi.org/10.1016/j.apsb.2016.02.001
Heery CR, O’sullivan-Coyne G, Madan RA, Cordes L, Rajan A, Rauckhorst M, Lamping E, Oyelakin I, Marté JL, Lepone LM, Donahue RN, Grenga I, Cuillerot J-M, Neuteboom B, Heydebreck AV, Chin K, Schlom J, Gulley JL (2017) Avelumab for metastatic or locally advanced previously treated solid tumours (JAVELIN Solid Tumor): a phase 1a, multicohort, dose-escalation trial. Lancet Oncol 18:587–598. https://doi.org/10.1016/S1470-2045(17)30239-5
Herbst RS, Arquette M, Shin DM, Dicke K, Vokes EE, Azarnia N, Hong WK, Kies MS (2005) Phase II multicenter study of the epidermal growth factor receptor antibody cetuximab and cisplatin for recurrent and refractory squamous cell carcinoma of the head and neck. J Clin Oncol 23:5578–5587. https://doi.org/10.1200/JCO.2005.07.120
Hood JL (2016) Post isolation modification of exosomes for nanomedicine applications. Nanomedicine 11:1745–1756. https://doi.org/10.2217/nnm-2016-0102
Huang S-M, Bock JM, Harari PM (1999) Epidermal growth factor receptor blockade with C225 modulates proliferation, apoptosis, and radiosensitivity in squamous cell carcinomas of the head and neck. Cancer Res 59:1935–1940. http://cancerres.aacrjournals.org/content/59/8/1935.abstract.
Huang Q, Yu GP, Mccormick SA, Mo J, Datta B, Mahimkar M, Lazarus P, Schäffer AA, Desper R, Schantz SP (2002) Genetic differences detected by comparative genomic hybridization in head and neck squamous cell carcinomas from different tumor sites: construction of oncogenetic trees for tumor progression. Genes Chromosom Cancer 34:224–233. https://doi.org/10.1002/gcc.10062
Huang X, Qian W, El-Sayed IH, El-Sayed MA (2007) The potential use of the enhanced nonlinear properties of gold nanospheres in photothermal cancer therapy. Lasers Surg Med 39:747–753. https://doi.org/10.1002/lsm.20577
Huo M, Yuan J, Tao L, Wei Y (2014) Redox-responsive polymers for drug delivery: from molecular design to applications. Polym Chem 5:1519–1528. https://doi.org/10.1039/C3PY01192E
Hussein AA, Helder MN, De Visscher JG, Leemans CR, Braakhuis BJ, De Vet HCW, Forouzanfar T (2017) Global incidence of oral and oropharynx cancer in patients younger than 45 years versus older patients: a systematic review. Eur J Cancer (oxford, England:1990) 82:115–127. https://doi.org/10.1016/j.ejca.2017.05.026
Ibrahim I, Gamal-Eldeen AM, Eldeen A (2019) Liposome-coated nano doxorubicin induces apoptosis on oral squamous cell carcinoma CAL-27 cells. Arch Oral Biol 103:47–54. https://doi.org/10.1016/j.archoralbio.2019.05.011
Iurisci I, Cumashi A, Sherman AA, Tsvetkov YE, Tinari N, Piccolo E, D’egidio M, Adamo V, Natoli C, Rabinovich GA, Iacobelli S, Nifantiev NE, The Consorzio Interuniversitario Nazionale Per La Bio-Oncologia I (2009) Synthetic inhibitors of galectin-1 and -3 selectively modulate homotypic cell aggregation and tumor cell apoptosis. Anticancer Res 29: 403–410. https://ar.iiarjournals.org/content/anticanres/29/1/403.full.pdf.
Jiang Y, Fei W, Cen X, Tang Y, Liang X (2015) Near-infrared light activatable multimodal gold nanostructures platform: an emerging paradigm for cancer therapy. Curr Cancer Drug Targets 15:406–422. https://doi.org/10.2174/1568009615666150407125333
Jin R, Liu Z, Bai Y, Zhou Y, Gooding JJ, Chen X (2018) Core-satellite mesoporous silica-gold nanotheranostics for biological stimuli triggered multimodal cancer therapy. Adv Func Mater 28:1801961. https://doi.org/10.1002/adfm.201801961
Johnson DE, Burtness B, Leemans CR, Lui VWY, Bauman JE, Grandis JR (2020) Head and neck squamous cell carcinoma. Nat Rev Dis Primers 6:1–22. https://doi.org/10.7150/ijms.10083
Kalaydina R-V, Bajwa K, Qorri B, Decarlo A, Szewczuk MR (2018) Recent advances in “smart” delivery systems for extended drug release in cancer therapy. Int J Nanomed 13:4727–4745. https://doi.org/10.2147/IJN.S168053
Kaminskas LM, Mcleod VM, Kelly BD, Sberna G, Boyd BJ, Williamson M, Owen DJ, Porter C (2012) A comparison of changes to doxorubicin pharmacokinetics, antitumor activity, and toxicity mediated by PEGylated dendrimer and PEGylated liposome drug delivery systems. nanomedicine: nanotechnology. Biol Med 8:103–111. https://doi.org/10.1016/j.nano.2011.05.013
Kawasaki G, Kato Y, Mizuno A (2002) Cathepsin expression in oral squamous cell carcinoma: Relationship with clinicopathologic factors. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 93:446–454. https://doi.org/10.1067/moe.2002.122834
Kerawala C, Roques T, Jeannon JP, Bisase B (2016) Oral cavity and lip cancer: United Kingdom national multidisciplinary guidelines. J Laryngol Otol 130:S83–S89. https://doi.org/10.1017/s0022215116000499
Kessenbrock K, Plaks V, Werb Z (2010) Matrix metalloproteinases: regulators of the tumor microenvironment. Cell 141:52–67. https://doi.org/10.1016/j.cell.2010.03.015
Ketabat F, Pundir M, Mohabatpour F, Lobanova L, Koutsopoulos S, Hadjiiski L, Chen X, Papagerakis P, Papagerakis S (2019) Controlled drug delivery systems for oral cancer treatment—current status and future perspectives. Pharmaceutics 11:302. https://doi.org/10.3390/pharmaceutics11070302
Koontongkaew S (2013) The tumor microenvironment contribution to development, growth, invasion and metastasis of head and neck squamous cell carcinomas. J Cancer 4:66–83. https://doi.org/10.7150/jca.5112
Kruijtzer CMF (2002) Improvement of oral drug treatment by temporary inhibition of drug transporters and/or cytochrome P450 in the gastrointestinal tract and liver: an overview. Oncologist 7:516–530. https://doi.org/10.1634/theoncologist.7-6-516
Lecaros RLG, Huang L, Lee T-C, Hsu Y-C (2016) Nanoparticle delivered VEGF-A siRNA enhances photodynamic therapy for head and neck cancer treatment. Mol Ther 24:106–116. https://doi.org/10.1038/mt.2015.169
Legge CJ, Colley HE, Lawson MA, Rawlings AE (2019) Targeted magnetic nanoparticle hyperthermia for the treatment of oral cancer. J Oral Pathol Med 48:803–809. https://doi.org/10.1111/jop.12921
Li J, Gong C, Feng X, Zhou X, Xu X, Xie L, Wang R, Zhang D, Wang H, Deng P (2012) Biodegradable thermosensitive hydrogel for SAHA and DDP delivery: therapeutic effects on oral squamous cell carcinoma xenografts. PLoS ONE 7:e33860. https://doi.org/10.1371/journal.pone.0033860
Li Q, Wen Y, Wen J, Zhang Y-P, Xu X-D, Victorious A, Zavitz R, Xu X (2016a) A new biosafe reactive oxygen species (ROS)-responsive nanoplatform for drug delivery. RSC Adv 6:38984–38989. https://doi.org/10.1039/C5RA25913D
Li Q, Wen Y, You X, Zhang F, Shah V, Chen X, Tong D, Wei X, Yin L, Wu J, Xu X (2016b) Development of a reactive oxygen species (ROS)-responsive nanoplatform for targeted oral cancer therapy. J Mater Chem B 4:4675–4682. https://doi.org/10.1039/C6TB01016D
Li X, Li L, Huang Y, Liu B, Chi H, Shi L, Zhang W, Li G, Niu Y, Zhu X (2017) Synergistic therapy of chemotherapeutic drugs and MTH1 inhibitors using a pH-sensitive polymeric delivery system for oral squamous cell carcinoma. Biomater Sci 5:2068–2078. https://doi.org/10.1039/C7BM00395A
Li L, Yang W-W, Xu D-G (2019a) Stimuli-responsive nanoscale drug delivery systems for cancer therapy. J Drug Target 27:423–433. https://doi.org/10.1080/1061186x.2018.1519029
Li W, Tao C, Wang J, Le Y, Zhang J (2019b) MMP-responsive in situ forming hydrogel loaded with doxorubicin-encapsulated biodegradable micelles for local chemotherapy of oral squamous cell carcinoma. RSC Adv 9:31264–31273. https://doi.org/10.1039/C9RA04343H
Li Z, Liu Q, Zhang Y, Yang Y, Zhou X, Peng W, Liang Z, Zeng X, Wang Q, Gao N (2021) Charge-reversal nanomedicine based on black phosphorus for the development of a novel photothermal therapy of oral cancer. Drug Deliv 28:700–708. https://doi.org/10.1080/10717544.2021.1909176
Liu L, Chen J, Cai X, Yao Z, Huang J (2019) Progress in targeted therapeutic drugs for oral squamous cell carcinoma. Surg Oncol 31:90–97. https://doi.org/10.1016/j.suronc.2019.09.001
Liu Z, Shi J, Zhu B, Xu Q (2020) Development of a multifunctional gold nanoplatform for combined chemo-photothermal therapy against oral cancer. Nanomedicine 15:661–676. https://doi.org/10.2217/nnm-2019-0415
Liu J, Jiang X, Zou A, Mai Z, Huang Z, Sun L, Zhao J (2021) circIGHG-induced epithelial-to-mesenchymal transition promotes oral squamous cell carcinoma progression via miR-142-5p/IGF2BP3 signaling. Can Res 81:344–355. https://doi.org/10.1158/0008-5472.CAN-20-0554
Lu Y, Zheng Z, Yuan Y, Pathak JL, Yang X, Wang L, Ye Z, Cho WC, Zeng M, Wu L (2021) The emerging role of exosomes in oral squamous cell carcinoma. Front Cell Dev Biol 9:324. https://doi.org/10.3389/fcell.2021.628103
Lucky SS, Idris NM, Huang K, Kim J, Li Z, Thong PSP, Xu R, Soo KC, Zhang Y (2016) In vivo biocompatibility, biodistribution and therapeutic efficiency of titania coated upconversion nanoparticles for photodynamic therapy of solid oral cancers. Theranostics 6:1844–1865. https://doi.org/10.7150/thno.15088
Ma C, Shi L, Huang Y, Shen L, Peng H, Zhu X, Zhou G (2017) Nanoparticle delivery of Wnt-1 siRNA enhances photodynamic therapy by inhibiting epithelial–mesenchymal transition for oral cancer. Biomater Sci 5:494–501. https://doi.org/10.1039/C6BM00833J
Mackey MA, El-Sayed MA (2014) Chemosensitization of cancer cells via gold nanoparticle-induced cell cycle regulation. Photochem Photobiol 90:306–312. https://doi.org/10.1111/php.12226
Mahoney KM, Rennert PD, Freeman GJ (2015) Combination cancer immunotherapy and new immunomodulatory targets. Nat Rev Drug Discov 14:561–584. https://doi.org/10.1038/nrd4591
Marcazzan S, Varoni EM, Blanco E, Lodi G, Ferrari M (2018) Nanomedicine, an emerging therapeutic strategy for oral cancer therapy. Oral Oncol 76:1–7. https://doi.org/10.1016/j.oraloncology.2017.11.014
Melancon MP, Lu W, Zhong M, Zhou M, Liang G, Elliott AM, Hazle JD, Myers JN, Li C, Jason Stafford R (2011) Targeted multifunctional gold-based nanoshells for magnetic resonance-guided laser ablation of head and neck cancer. Biomaterials 32:7600–7608. https://doi.org/10.1016/j.biomaterials.2011.06.039
Meulemans J, Delaere P, Vander Poorten V (2019) Photodynamic therapy in head and neck cancer: indications, outcomes, and future prospects. Curr Opin Otolaryngol Head Neck Surg 27:136–141. https://doi.org/10.1097/MOO.0000000000000521
Mohan A, Narayanan S, Balasubramanian G, Sethuraman S, Krishnan UM (2016) Dual drug loaded nanoliposomal chemotherapy: a promising strategy for treatment of head and neck squamous cell carcinoma. Eur J Pharm Biopharm 99:73–83. https://doi.org/10.1016/j.ejpb.2015.11.017
Montero PH, Patel SG (2015) Cancer of the oral cavity. Surg Oncol Clin North Am 24:491–508. https://doi.org/10.1016/j.soc.2015.03.006
Nakamura Y, Mochida A, Choyke PL, Kobayashi H (2016) Nanodrug delivery: is the enhanced permeability and retention effect sufficient for curing cancer? Bioconjug Chem 27:2225–2238. https://doi.org/10.1021/acs.bioconjchem.6b00437
Nakashima T, Tomita H, Hirata A, Ishida K, Hisamatsu K, Hatano Y, Kanayama T, Niwa A, Noguchi K, Kato K, Miyazaki T, Tanaka T, Shibata T, Hara A (2017) Promotion of cell proliferation by the proto-oncogene DEK enhances oral squamous cell carcinogenesis through field cancerization. Cancer Med 6:2424–2439. https://doi.org/10.1002/cam4.1157
Osta WA, Chen Y, Mikhitarian K, Mitas M, Salem M, Hannun YA, Cole DJ, Gillanders WE (2004) EpCAM Is overexpressed in breast cancer and is a potential target for breast cancer gene therapy. Can Res 64:5818–5824. https://doi.org/10.1158/0008-5472.CAN-04-0754
Peng Q-S, Cheng Y-N, Zhang W-B, Fan H, Mao Q-H, Xu P (2020) circRNA_0000140 suppresses oral squamous cell carcinoma growth and metastasis by targeting miR-31 to inhibit Hippo signaling pathway. Cell Death Dis 11:1–18. https://doi.org/10.1038/s41419-020-2273-y
Rao L, Bu L-L, Cai B, Xu J-H, Li A, Zhang W-F, Sun Z-J, Guo S-S, Liu W, Wang T-H, Zhao X-Z (2016) Cancer cell membrane-coated upconversion nanoprobes for highly specific tumor imaging. Adv Mater 28:3460–3466. https://doi.org/10.1002/adma.201506086
Rao L, Bu L-L, Ma L, Wang W, Liu H, Wan D, Liu J-F, Li A, Guo S-S, Zhang L, Zhang W-F, Zhao X-Z, Sun Z-J, Liu W (2018) Platelet-facilitated photothermal therapy of head and neck squamous cell carcinoma. Angewandte Chem-Int Ed 57:986–991. https://doi.org/10.1002/anie.201709457
Rathinaraj P, Muthusamy G, Prasad NR, Gunaseelan S, Kim B, Zhu S (2020) Folate–gold–bilirubin nanoconjugate induces apoptotic death in multidrug-resistant oral carcinoma cells. Eur J Drug Metab Pharmacokinet 45:285–296. https://doi.org/10.1007/s13318-019-00600-9
Ren T, Mei-Juan LI (2009) Research status and prospect of suicide gene therapy for malignant tumor. J Modern Oncol 17:2435–2437. https://doi.org/10.1007/s12013-014-9849-z
Ren S, Cheng X, Chen M, Liu C, Zhao P, Huang W, He J, Zhou Z, Miao L (2017) Hypotoxic and rapidly metabolic PEG-PCL-C3-ICG nanoparticles for fluorescence-guided photothermal/photodynamic therapy against OSCC. ACS Appl Mater Interfaces 9:31509–31518. https://doi.org/10.1021/acsami.7b09522
Rosenberger L, Ezquer M, Lillo-Vera F, Pedraza PL, Ortúzar MI, González PL, Figueroa-Valdés AI, Cuenca J, Ezquer F, Khoury M, Alcayaga-Miranda F (2019) Stem cell exosomes inhibit angiogenesis and tumor growth of oral squamous cell carcinoma. Sci Rep 9:1–12. https://doi.org/10.1038/s41598-018-36855-6
Saiyin W, Wang D, Li L, Zhu L, Liu B, Sheng L, Li Y, Zhu B, Mao L, Li G, Zhu X (2014) Sequential release of autophagy inhibitor and chemotherapeutic drug with polymeric delivery system for oral squamous cell carcinoma therapy. Mol Pharm 11:1662–1675. https://doi.org/10.1021/mp5000423
Seynhaeve A, Dicheva BM, Hoving S, Koning GA, Hagen T (2013) Intact Doxil is taken up intracellularly and released doxorubicin sequesters in the lysosome: evaluated by in vitro/in vivo live cell imaging. J Control Release 172:30–340. https://doi.org/10.1016/j.jconrel.2013.08.034
Smyth MJ, Ngiow SF, Ribas A, Teng MWL (2016) Combination cancer immunotherapies tailored to the tumour microenvironment. Nat Rev Clin Oncol 13:143–158. https://doi.org/10.1038/nrclinonc.2015.209
Sturgis EM, Cinciripini PM (2007) Trends in head and neck cancer incidence in relation to smoking prevalence: an emerging epidemic of human papillomavirus-associated cancers? Cancer 110:1429–1435. https://doi.org/10.1002/cncr.22963
Su Z, Liu D, Chen L, Zhang J, Ru L, Chen Z, Gao Z, Wang X (2019) CD44-targeted magnetic nanoparticles kill head and neck squamous cell carcinoma stem cells in an alternating magnetic field. Int J Nanomed 14:7549–7560. https://doi.org/10.2147/IJN.S215087
Sun Q, Wu J, Jin L, Hong L, Wang F, Mao Z, Wu M (2020) Cancer cell membrane-coated gold nanorods for photothermal therapy and radiotherapy on oral squamous cancer. J Mater Chem B 8:7253–7263. https://doi.org/10.1039/D0TB01063D
Taghizadeh B, Taranejoo S, Monemian SA, Salehi Moghaddam Z, Daliri K, Derakhshankhah H, Derakhshani Z (2015) Classification of stimuli–responsive polymers as anticancer drug delivery systems. Drug Deliv 22:145–155. https://doi.org/10.3109/10717544.2014.887157
Tan G, Zhong Y, Yang L, Jiang Y, Liu J, Ren F (2020) A multifunctional MOF-based nanohybrid as injectable implant platform for drug synergistic oral cancer therapy. Chem Eng J 390:124446. https://doi.org/10.1016/j.cej.2020.124446
Tarassoli SP, De Pinillos Bayona AM, Pye H, Mosse CA, Callan JF, Macrobert A, Mchale AP, Nomikou N (2016) Cathepsin B-degradable, NIR-responsive nanoparticulate platform for target-specific cancer therapy. Nanotechnology 28:055101. https://doi.org/10.1088/1361-6528/28/5/055101
Teraoka S, Kakei Y, Akashi M, Iwata E, Hasegawa T, Miyawaki D, Sasaki R, Komori T (2018) Gold nanoparticles enhance X-ray irradiation-induced apoptosis in head and neck squamous cell carcinoma in vitro. Biomed Rep 9:415–420. https://doi.org/10.3892/br.2018.1142
Tomita R, Sasabe E, Tomomura A, Yamamoto T (2020) Macrophagederived exosomes attenuate the susceptibility of oral squamous cell carcinoma cells to chemotherapeutic drugs through the AKT/GSK3β pathway. Oncol Rep 44:1905–1916. https://doi.org/10.3892/or.2020.7748
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A (2015) Global cancer statistics, 2012. CA: A Cancer J Clin 65:87–108. https://doi.org/10.3322/caac.21262
Tshering Vogel DW, Zbaeren P, Thoeny HC (2010) Cancer of the oral cavity and oropharynx. Cancer Imaging: the Official Publ Int Cancer Imaging Soc 10:62–72. https://doi.org/10.1102/1470-7330.2010.0008
Van Harten AM, Brakenhoff RH (2021) Targeted treatment of head and neck (pre)cancer: preclinical target identification and development of novel therapeutic applications. Cancers 13:2774. https://doi.org/10.3390/cancers13112774
Veigas F, Mahmoud YD, Merlo J, Rinflerch A, Girotti MR (2021) Immune checkpoints pathways in head and neck squamous cell carcinoma. Cancers 13:1018. https://doi.org/10.3390/cancers13051018
Vermorken JB, Mesia R, Rivera F, Remenar E, Kawecki A, Rottey S, Erfan J, Zabolotnyy D, Kienzer H-R, Cupissol D, Peyrade F, Benasso M, Vynnychenko I, De Raucourt D, Bokemeyer C, Schueler A, Amellal N, Hitt R (2008) Platinum-based chemotherapy plus cetuximab in head and neck cancer. New England J Med 359:1116–1127. https://doi.org/10.1056/NEJMoa0802656
Vigneswara V, Kong A (2018) Predictive biomarkers and EGFR inhibitors in squamous cell carcinoma of head and neck (SCCHN). Ann Oncol off J Eur Soc Med Oncol 29:794–796. https://doi.org/10.1093/annonc/mdy065
Wang B, Wang J-H, Liu Q, Huang H, Chen M, Li K, Li C, Yu X-F, Chu PK (2014) Rose-bengal-conjugated gold nanorods for in vivo photodynamic and photothermal oral cancer therapies. Biomaterials 35:1954–1966. https://doi.org/10.1016/j.biomaterials.2013.11.066
Wang Z-Q, Liu K, Huo Z-J, Li X-C, Wang M, Liu P, Pang B, Wang S-J (2015) A cell-targeted chemotherapeutic nanomedicine strategy for oral squamous cell carcinoma therapy. J Nanobiotechnology 13:1–10. https://doi.org/10.1186/s12951-015-0116-2
Wang B-K, Yu X-F, Wang J-H, Li Z-B, Li P-H, Wang H, Song L, Chu PK, Li C (2016) Gold-nanorods-siRNA nanoplex for improved photothermal therapy by gene silencing. Biomaterials 78:27–39. https://doi.org/10.1016/j.biomaterials.2015.11.025
Wang D, Xu X, Zhang K, Sun B, Wang L, Meng L, Liu Q, Zheng C, Yang B, Sun H (2017a) Codelivery of doxorubicin and MDR1-siRNA by mesoporous silica nanoparticles-polymerpolyethylenimine to improve oral squamous carcinoma treatment. Int J Nanomed 13:187–198. https://doi.org/10.2147/IJN.S150610
Wang Y, Wan G, Li Z, Shi S, Chen B, Li C, Zhang L, Wang Y (2017b) PEGylated doxorubicin nanoparticles mediated by HN-1 peptide for targeted treatment of oral squamous cell carcinoma. Int J Pharm 525:21–31. https://doi.org/10.1016/j.ijpharm.2017.04.027
Wang F, Wang M, Zhao L, Li Q (2019a) A new biosafe reactive oxygen species responsive nanoplatform for targeted oral squamous cell carcinoma therapy. Mater Express 9:1076–1081. https://doi.org/10.1166/mex.2019.1602
Wang H-H, Fu Z-G, Li W, Li Y-X, Zhao L-S, Wen L, Zhang J-J, Wen N (2019b) The synthesis and application of nano doxorubicin-indocyanine green matrix metalloproteinase-responsive hydrogel in chemophototherapy for head and neck squamous cell carcinoma. Int J Nanomed 14:623. https://doi.org/10.2147/IJN.S217586
Wang M, Zhai Y, Ye H, Lv Q, Sun B, Luo C, Jiang Q, Zhang H, Xu Y, Jing Y, Huang L, Sun J, He Z (2019c) High co-loading capacity and stimuli-responsive release based on cascade reaction of self-destructive polymer for improved chemo-photodynamic therapy. ACS Nano 13:7010–7023. https://doi.org/10.1021/acsnano.9b02096
Wang Y, Xie D, Pan J, Xia C, Fan L, Pu Y, Zhang Q, Ni YH, Wang J, Hu Q (2019d) A near infrared light-triggered human serum albumin drug delivery system with coordination bonding of indocyanine green and cisplatin for targeting photochemistry therapy against oral squamous cell cancer. Biomater Sci 7:5270–5282. https://doi.org/10.1039/C9BM01192G
Wang Y, Zhang W, Sun P, Cai Y, Xu W, Fan Q, Hu Q, Han W (2019e) A novel multimodal NIR-II nanoprobe for the detection of metastatic lymph nodes and targeting chemo-photothermal therapy in oral squamous cell carcinoma. Theranostics 9:391–404. https://doi.org/10.7150/thno.30268
Wang X, Li S, Liu H (2021) Co-delivery of chitosan nanoparticles of 5-aminolevulinic acid and shGBAS for improving photodynamic therapy efficacy in oral squamous cell carcinomas. Photodiagn Photodyn Ther 34:102218. https://doi.org/10.1016/j.pdpdt.2021.102218
Wei Z, Yin X, Cai Y, Xu W, Song C, Wang Y, Zhang J, Kang A, Wang Z, Han W (2018) Antitumor effect of a Pt-loaded nanocomposite based on graphene quantum dots combats hypoxia-induced chemoresistance of oral squamous cell carcinoma. Int J Nanomed 13:1505–1524. https://doi.org/10.2147/ijn.S156984
Wei Z, Zou H, Liu G, Song C, Han WJBM (2021) Peroxidase-mimicking evodiamine/indocyanine green nanoliposomes for multimodal imaging-guided theranostics for oral squamous cell carcinoma. Bioactive Mater 6:2144–2157. https://doi.org/10.1016/j.bioactmat.2020.12.016
Weinberg F, Ramnath N, Nagrath D (2019) Reactive oxygen species in the tumor microenvironment: an overview. Cancers 11:1191. https://doi.org/10.3390/cancers11081191
Wicki A, Witzigmann D, Balasubramanian V, Huwyler J (2015) Nanomedicine in cancer therapy: challenges, opportunities, and clinical applications—sciencedirect. J Control Release 200:138–157. https://doi.org/10.1016/j.jconrel.2014.12.030
Wu T-T, Zhou S-H (2015) Nanoparticle-based targeted therapeutics in head-and-neck cancer. Int J Med Sci 12:187–200. https://doi.org/10.7150/ijms.10083
Wu YN, Yang LX, Shi XY, Li IC, Biazik JM, Ratinac KR, Chen DH, Thordarson P, Shieh DB, Braet F (2011) The selective growth inhibition of oral cancer by iron core-gold shell nanoparticles through mitochondria-mediated autophagy. Biomaterials 32:4565–4573. https://doi.org/10.1016/j.biomaterials.2011.03.006
Wu J, Cao J, Li X, Wu B, Zhang S (2020a) MicroRNA-345 functions as a tumor suppressor via targeting ZEB2 in oral squamous cell carcinoma. Arch Oral Biol 116:104732. https://doi.org/10.1016/j.archoralbio.2020.104732
Wu J, Guo Q, Zhang G, Zhao L, Lv Y, Wang J, Liu J, Shi W (2020b) Study on the targeted therapy of oral squamous cell carcinoma with a plasmid expressing PE38KDEL toxin under control of the SERPINB3 promoter. Cancer Med 9:2213–2222. https://doi.org/10.1002/cam4.2880
Xu S, Olenyuk BZ, Okamoto CT, Hamm-Alvarez SF (2013) Targeting receptor-mediated endocytotic pathways with nanoparticles: Rationale and advances. Adv Drug Deliv Rev 65:121–138. https://doi.org/10.1016/j.addr.2012.09.041
Yan X, Chen YR, Song YF, Ye J, Yu JK (2020) Advances in the application of supramolecular hydrogels for stem cell delivery and cartilage tissue engineering. Front Bioeng Biotechnol 8:847. https://doi.org/10.3389/fbioe.2020.00847
Yang Y-T, Wang Y-F, Lai J-Y, Shen S-Y, Wang F, Kong J, Zhang W, Yang H-Y (2016) Long non-coding RNA UCA1 contributes to the progression of oral squamous cell carcinoma by regulating the WNT/β-catenin signaling pathway. Cancer Sci 107:1581–1589. https://doi.org/10.1111/cas.13058
Yao Q, Kou L, Tu Y, Zhu L (2018) MMP-responsive ‘smart’ drug delivery and tumor targeting. Trends Pharmacol Sci 39:766–781. https://doi.org/10.1016/j.tips.2018.06.003
Yu D, Wang A, Huang H, Chen Y (2008) PEG-PBLG nanoparticle-mediated HSV-TK/GCV gene therapy for oral squamous cell carcinoma. Nanomedicine 3:813–821. https://doi.org/10.2217/17435889.3.6.813
Yue X-S, Murakami Y, Tamai T, Nagaoka M, Cho C-S, Ito Y, Akaike T (2010) A fusion protein N-cadherin-Fc as an artificial extracellular matrix surface for maintenance of stem cell features. Biomaterials 31:5287–5296. https://doi.org/10.1016/j.biomaterials.2010.03.035
Zhang NN, Zhang LG, Liu ZN, Huang GL, Zhang L, Yi J, Yao L, Hu XH (2015) Therapeutic efficacy of paclitaxel and carboplatin via arterial or venous perfusion in rabbits with VX-2 tongue cancer. Int J Clin Exp Med 8: 4979–4988. https://pubmed.ncbi.nlm.nih.gov/26131070.
Zhang K, Guan X, Qiu Y, Wang D, Zhang X, Zhang H (2016) A pH/glutathione double responsive drug delivery system using molecular imprint technique for drug loading. Appl Surf Sci 389:1208–1213. https://doi.org/10.1016/j.apsusc.2016.08.107
Zhang M, Liang J, Yang Y, Liang H, Li D (2020) Current trends of targeted drug delivery for oral cancer therapy. Front Bioeng Biotechnol 8:1417. https://doi.org/10.3389/fbioe.2020.618931
Zhen X, Cheng P, Pu K (2019) Recent advances in cell membrane-camouflaged nanoparticles for cancer phototherapy. Small 15:1804105. https://doi.org/10.1002/smll.201804105
Zhou Z-H, Liang S-Y, Zhao T-C, Chen X-Z, Cao X-K, Qi M, Huang Y-Y, Ju W-T, Yang M, Zhu D-W, Pang Y-C, Zhong L-P (2021) Overcoming chemotherapy resistance using pH-sensitive hollow MnO2 nanoshells that target the hypoxic tumor microenvironment of metastasized oral squamous cell carcinoma. J Nanobiotechnology 19:1–14. https://doi.org/10.1186/s12951-021-00901-9
Zhu J-Y, Zheng D-W, Zhang M-K, Yu W-Y, Qiu W-X, Hu J-J, Feng J, Zhang X-Z (2016) Preferential cancer cell self-recognition and tumor self-targeting by coating nanoparticles with homotypic cancer cell membranes. Nano Lett 16:5895–5901. https://doi.org/10.1021/acs.nanolett.6b02786
Zuo J, Huo M, Wang L, Li J, Chen Y, Xiong P (2020) Photonic hyperthermal and sonodynamic nanotherapy targeting oral squamous cell carcinoma. J Mater Chem B 8:9084–9093. https://doi.org/10.1039/d0tb01089h
Funding
This work was supported by funding from the National Natural Science Foundation of China under Grant Agreement No. 31970783. Author Hongjiao Li, Yao Zhang has received research support from Chongqing Medical University.
Author information
Authors and Affiliations
Contributions
HL designed and prepared the manuscript. YZ and MX contributed to data collection. HL and YZ contributed equally to this manuscript. All the authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, H., Zhang, Y., Xu, M. et al. Current trends of targeted therapy for oral squamous cell carcinoma. J Cancer Res Clin Oncol 148, 2169–2186 (2022). https://doi.org/10.1007/s00432-022-04028-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-022-04028-8