Abstract
Purpose
First evaluation of dual-phase vaginal Er:YAG laser to omit hormonal treatment for atrophy-related symptoms in post-menopausal breast cancer survivors following prolapse surgery.
Methods
Patients with a history of breast cancer at the time of surgery for pelvic organ prolapse were offered non-hormonal vaginal Er:YAG laser treatment when complaining of atrophy-related genitourinary syndrome of menopause. A single 10-min course of dual-phase protocol of pulsed Er:YAG laser (2940 nm, fractional ablative and thermal mode, fluence according to tissue thickness). Follow-up included subjective satisfaction, vaginal pH, vaginal health index (VHI), and complications after 6 weeks.
Results
A total of 16 breast cancer survivors (age 71 years, SD 7) had been seeking treatment for pelvic floor symptoms related to vaginal atrophy at follow-up visits after prolapse surgery. All ablative vaginal Er:YAG laser outpatient procedures were successfully completed, all patients returned to daily activities without a need for analgetic medication. Evaluation was performed after 8.3 (SD 2.5) weeks. Pre-laser VHI scored 16 (SD 4.6) and post-laser VHI 20 (SD 3) with p = 0.01. Patients were satisfied in 94% (n = 15) regarding symptom relief.
Conclusions
Breast cancer survivors with atrophy-related complaints after pelvic floor surgery may benefit from vaginal application of this innovative dual protocol of Er:YAG laser technology as a non-hormonal treatment approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Quality of life (QoL) of breast cancer survivors is frequently comprised due to genitourinary syndrome of menopause (GSM; Portman and Gass 2014). Non-hormonal options including lubricants do not sufficiently treat atrophy symptoms. Local estrogens as standard of care in GSM may have a negative effect on breast cancer outcome and is, therefore, not applied in this patient group.
Due to an aging population, health care systems in industrialized counties will be facing growing numbers of urogynecological patients presenting with oncological co-morbidities. According to Wu et al., 32% of women between the age of 50 and 59 years suffer from one or more pelvic floor disorders (Wu et al. 2014). Topical vaginal hormones are used as basic treatment in post-menopausal patients complaining of symptoms such as stress urinary incontinence (SUI), urgency, recurrent urinary tract infections, or other symptoms related to atrophy of vaginal epithelium such as dryness, burning, itching, dyspareunia, pain and feeling of prolapse.
Breast cancer is amongst the most common cancers in women and especially since death rate dropped 38% from 1989 to 2014 (Siegel et al. 2017) quality of life issues play a growing role for survivors. GSM with atrophy-related pelvic floor symptoms is reported to be a major factor for QoL impairment in breast cancer patients additionally being a side effect of aromatase inhibitors, chemotherapy, and tamoxifen (Biglia et al. 2015). Furthermore, breast cancer survivors should be counseled that oncological safety of low-dose local estrogen therapy has not been scientifically proven (Biglia et al. 2015). However, some authors would consider ultralow-dose local estriol treatment (0.03 mg) in breast cancer patients with severe QoL impairment due to GSM as possible (Donders et al. 2014; Buchholz et al. 2015).
International studies on laser treatment of vaginal epithelium for GSM (Gaspar et al. 2017; Salvatore et al. 2014; Gambacciani et al. 2015; Hutchinson-Colas and Segala 2015; Palacios et al. 2015; Gandhi et al. 2016) promise vaginal laser to be a new, non-hormonal option for the treatment of GSM inducing neocollagenesis, neoangiogenesis, tissue regeneration and leading to significant symptom relief (Gaspar et al. 2017). Especially, breast cancer patients under current anti-hormonal treatment as well as post-menopausal breast cancer survivors may benefit and might be potential target groups for a vaginal laser treatment approach (Pieralli et al. 2016).
Patients after pelvic floor surgery often complain of low-grade residual symptoms such as SUI, urgency, GSM or low-grade prolapse due to connective tissue weakness not justifying further surgical treatment. The “gold standard” treatment in such post-menopausal patients is topical estrogen in combination with other non-surgical treatment options, e.g. pelvic floor exercise, biofeedback, or pessaries. To offer non-hormonal alternatives to urogynecological patients being breast cancer survivors may help to maintain patient´s compliance and trust in the doctor’s overall treatment concept.
In this study, we analyze data after 15 years of prolapse surgery at our institution to answer the question of how often overlapping hormone-dependent cancer co-morbidities could be found in our patients undergoing prolapse surgery and if there is a need for further treatment of atrophy-related pelvic floor disorders in these patients, local hormonal treatment has been avoided. We present data on vaginal laser treatment using an innovative dual-phase protocol of ablative Er:YAG technology in residual atrophy-related urogynecological symptoms after prolapse surgery in patients with a history of breast cancer. Patients were evaluated in interviews using the expectation, goal setting, goal achievement, satisfaction (EGGS) approach (Brubaker and Shull 2005; Mothes et al. 2015), vaginal pH, and vaginal health index (VHI; Bachmann et al. 1992) and registered procedural complications were assessed.
Method
Data of a retrospective development and performance analysis of the University urogynecological unit in cooperation with the University Cancer Centre of Jena indicated 151 registered cancer patients amongst 1209 patients who underwent primary prolapse surgery at the institution between 2001 and 2015. Out of 64 (64/151) registered breast cancer patients, 31 (Fig. 1) patients were evaluated for urogynecological symptoms at follow-up. Patients with low-grade complaints of stress urinary incontinence (SUI), urgency, recurrent urinary tract infections, and symptoms related to atrophy of vaginal epithelium such as dryness, burning, itching, dyspareunia, pain and/or feeling of prolapse were offered vaginal Er:YAG laser treatment in the context of other non-surgical guideline-based treatment options, e.g. pelvic floor exercises, biofeedback, or pessaries. All patients underwent extensive counseling by a certified urogynaecologist. Individual counseling included the variety of non-surgical and surgical treatment options according to guidelines and scientific evidence. In addition, all patients gave written informed consent to vaginal laser treatment. Vaginal Er:YAG laser treatment was offered to patients without charges like recognized treatments covered by the public health care system. Interviews focusing on subjective judgement of symptom relief by the patient including an EGGS approach [goal setting, expectations, goal achievement, satisfaction, (Brubaker and Shull 2005; Mothes et al. 2015)] were performed for evaluation. Laser treatment was offered to the patient according to inclusion criteria: grade I SUI (ICS; Bump et al. 1996), urgency without an anatomic cause for residual volume (cystocele), grade I prolapse/complaint of vaginal laxity, and symptoms of vaginal atrophy such as itching, dryness, burning, discomfort, sexual impairment, and genitourinary syndrome of menopause in the context of other conservative treatment options. Abnormal PAP smear, vaginal wounds or infections, urinary tract infection, any abnormal finding on gynecological examination, pregnancy, menstrual period, intake of photosensitive drugs or topical estrogens and a previous history of malignant pelvic or systemic disease were exclusion criteria. Patients with a previous history of genital herpes infection were asked to take oral Aciclovir (Aciclovir-ratiopharm™, ratiopharm GmbH, Ulm, Germany) for prevention purposes. All patients gave informed consent in the context of other established treatment alternatives and were counseled not to have sexual intercourse for 72 h after treatment.
The dual-phase protocol of a pulsed ablative Er:YAG laser (MCL 31 Dermablate; Asclepion Laser Technologies, Jena, Germany) of defined wavelength of 2940 nm was performed in a single 10-min treatment course. The parameter fluence was adjusted depending on individual vaginal tissue thickness in each phase of protocol. Briefly, the first phase utilized the physical parameters, 300-µs pulse duration, 15–35 J/cm2 fluence, 0.5–2-s pulse interval, and 45° rotation. The fractional mode was realized by a squared 9 × 9 mm microspot optic with stable and precise micro lens array technology, consisting of 169 spots (MicroSpot, Asclepion Laser Technologies, Jena, Germany). The purpose of this ablative phase was to create small canals in the superficial layer of the vaginal epithelium. This phase was followed immediately by the second phase, performed in thermal mode using parameters: 1000-µs pulse duration, 3–9 J/cm2 fluence, 0.5–2-s pulse interval, and 22.5° rotation.
Patients were followed up at urogynecological unit performing interviews (EGGS; Brubaker and Shull 2005; Mothes et al. 2015), pH measurements, assessment of VHI (Bachmann et al. 1992) on speculum examination and post-procedural complications at 6 week intervals after laser treatment. Presented data were collected between September 2016 and June 2017.
Results
Out of 31 urogynecological patients with a history of breast cancer evaluated at urogynecological follow-up, 16 patients were seeking treatment for symptoms related to vaginal atrophy and pelvic floor dysfunction and not being fully satisfied after other treatments, such as pelvic floor exercises, bladder training, biofeedback, and anticholinergic drugs (Fig. 1). All patients were post-menopausal at an age of 71 (SD 7) years refusing topical estrogen treatment and complaining of symptoms related to vaginal atrophy such as dyspareunia, dryness, burning, and pain. In the majority (n = 11) of patients, symptoms of vaginal atrophy were combined with SUI, urgency and feeling of prolapse as described in GSM (Portman et al. 2014; Gaspar et al. 2017; Salvatore et al. 2014; Gambacciani et al. 2015; Hutchinson-Colas and Segala 2015; Palacios et al. 2015; Gandhi et al. 2016). Ablative vaginal Er:YAG laser treatment as a non-hormonal alternative to local vaginal estrogen treatment was performed in the above-described manner using a dual-phase protocol. All procedures were successfully completed as an outpatient procedure and all patients could return to normal daily activities immediately. All patients could be evaluated so far. The follow-up interval was 8.3 weeks (SD 2.5). Technically, the parameter fluence was adjusted to the state of atrophy of vaginal epithelium in both phases according to the operators experience and ranged between 15 and 35 J/m2 (phase I) and 3 and 9 J/m2 (phase II). No complications and no need for analgetic medication were observed.
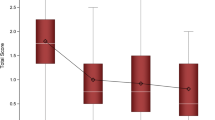
Vaginal health index (VHI; Bachmann et al. 1992) and vaginal pH were taken in all patients. Pre-laser VHI scored 16 (SD 4.6) and pH was 5 (SD 0.6) v/s post-laser VHI 20 (SD 3) with p = 0.01 and pH 4.8 (SD 0.4) with p = 0.14 (Table 1). Overall judgement of patients was positive in 94% (n = 15) and negative in n = 1 (0.6%) of patients who were not satisfied.
Discussion
Data of 1209 patients after prolapse surgery at university urogynecological center were analyzed. We found breast cancer to be the commonest cancer in patients having undergone prolapse surgery. Due to the hormone-dependent nature of this cancer, vaginal Er:YAG laser treatment was offered to this patient group when complaining of residual atrophy-related pelvic floor symptoms as a non-hormonal treatment alternative at follow-up visits. Vaginal Er:YAG laser utilizing a dual-phase protocol with fractional ablative and thermal mode as well as adjustable fluence led to a subjective satisfaction rate of as high as 94% in this patients at follow-up.
Urogynecological treatment of breast cancer survivors is often a challenge because of the need for local hormonal treatment to the atrophic vaginal epithelium. In addition, most elderly post-menopausal patients often do not know the receptor status of their breast cancer or even cannot remember the names of their (anti-hormonal) medication. Due to the multifactorial nature of pelvic floor disorders, residual low-grade symptoms are often found at follow-up after prolapse surgery according to our experience.
Little is known about prevalence of GSM in breast cancer patients presumably due to missing awareness for the need for documentation, assessment, and treatment strategies of this QoL-impairing condition. Cook et al. reviewed 800 medical records from a Breast Cancer Survivorship Clinic at a Comprehensive Cancer Centre. Symptoms of vaginal atrophy have been treated in only 111 patients (Cook et al. 2017). Other studies found, that symptoms caused by vaginal atrophy have a major impact on physical, emotional, and social health of women (Nappi and Palacious 2014; Santoro and Komi 2009). It was observed that this QoL impairment can also lead to interruption of adjuvant oncological therapies (Oyarzun and Castelo-Branco 2017). In a review of literature, Santen et al. estimate that 9.3 million breast cancer survivors globally suffer from several clinical problems associated with estrogen depletion (Santen et al. 2017). Authors conclude that vulvovaginal atrophy is a relevant (Biglia et al. 2017) but still an underestimated problem (Nappi et al. 2016). Treatment of atrophy-related symptoms is still an unmet need in this particular patient group (Santen et al. 2017). Further epidemiological data on GSM in breast cancer survivors are needed and individual treatment concepts should be developed. QoL issues in long-term surviving cancer patients should be a major field of future concerns in modern health care systems.
According to a literature review (Biglia et al. 2015), there are limited options in the treatment of atrophy-related pelvic floor disorders in breast cancer patients. While vaginal lubricants can be used for patients with hormone-dependent cancer, its long-term effect could not be proven. The selective estrogen receptor modulator (SERM) ospemifene has been introduced for the treatment of vulvovaginal atrophy in post-menopausal women presenting contraindications for local estrogen treatment (Berga 2013; EMA 2015). Long-term follow-up is still missing and final conclusions on the safety of SERMs for cancer patients should not be drawn yet (Biglia et al. 2015).
Epithelial resurfacing was observed after dermatological laser treatment using different technologies (Majaron et al. 2000; Dmovsek-Olup et al. 2004; Schmitt et al. 2017; Alexiades-Armenakas et al. 2012). Laser applications seems to be an encouraging, non-hormonal, and non-surgical approach to the treatment of vaginal atrophy as well (Lang and Karram 2017), avoiding the long-term use of local or oral medication. Improved vascularization, enhanced metabolism and neocollagenosis was histologically demonstrated in vaginal biopsies after Er:YAG laser (Gaspar et al. 2017). Several studies on vaginal laser treatment utilizing either CO2 (Salvatore et al. 2014; Pieralli et al. 2016) or Er:YAG (Gaspar et al. 2017; Gambacciani et al. 2015; Gambacciani and Palacios 2017; Vizintin et al. 2015) technologies show significant improvement of atrophy-related symptoms like described as GSM. In solid-state lasers, e.g. Er:YAG, the most important energetic conversion is considered to be the generation of thermal energy by water absorption (Fisher 1992). Due to the specific feature of Er:YAG emitting light of 2940 nm wavelength at the peak of water absorption, its absorption coefficient is 16 times higher than compared to the CO2 laser (Tadir et al. 2017). Since other groups reported the use of non-ablative Er:YAG laser for vaginal application (Gaspar et al. 2017), the innovative aspect of the dual protocol introduced by our group and used in this study is the direct combination of a fractional ablation mode (300-µs pulse durations) with a thermal mode (1000-µs pulse durations; Asclepion Laser Technologies, Jena, Germany). Both modes directly follow each other and allow the adjustment of fluence, which is defined as total energy transmitted by the laser beam, divided by the cross-sectional area of the beam (Fisher 1992). Fluence may be adjusted according to the impression of vaginal epithelium to the experienced examiner.
Efficacy of vaginal Er:YAG laser treatment in comparison with topical vaginal estriol treatment has been demonstrated by Gaspar et al. (2017). Authors found that Er:YAG laser treatment relieved atrophy-related symptoms with more pronounced and longer lasting effects compared to topical hormones (Gaspar et al. 2017).
Evaluating vaginal Er:YAG laser treatment of GSM significant symptom improvement was found at a minimum evaluation interval of 4 weeks (Gaspar et al. 2017). Evaluation interval of 6 weeks was chosen because we intended to see consolidation of symptom relieved in GSM within the known interval of connective tissue regeneration. Other groups performed a second or third course of non-ablative Erbium laser treatment after 3–6 weeks (Gaspar et al. 2017). Using the technology of ablative Er:YAG laser (compared to non-ablative), we perform a second treatment course only on demand at follow-up visits after 6 weeks. Due to the preliminary nature and small number of patients included in this study so far, we have not analyzed a subgroup undergoing a second course of laser therapy and, therefore, being not on an extended evaluation schedule yet. Vaginal Er:YAG laser treatment as an innovative treatment option has been introduced to our institution only in April 2016. In a prospective study, which is currently conducted at our institution, evaluation intervals extend to 6 months to examine midterm treatment effects.
Our data support the idea of treating breast cancer survivors with atrophy-related complaints after pelvic floor surgery using vaginal application of the dual protocol of Er:YAG laser technology as a non-hormonal treatment approach. Connective tissue weakness and tissue atrophy are considered to be strong risk factors (Mothes et al. 2016; Jelovsek et al. 2007) and found in the vast majority of pelvic floor patients. Underlying causes for pelvic floor disorders on the tissue level should be adequately treated. Additional long-term treatment of pelvic floor patients is often necessary. Due to limited options in breast cancer survivors, vaginal Er:YAG laser treatment should be offered to these symptomatic patients in the context of other conservative treatments. Authors suggest to conduct prospective studies to collect data on vaginal dual protocol Er:YAG laser treatment of GSM in breast cancer survivors.
Further prospective investigations are warranted to observe the effect of Er:YAG laser treatment in breast cancer survivors with urogynecological symptoms, e.g. caused by anti-hormones and without a history of pelvic floor surgery.
Conclusion
In post-menopausal pelvic floor patients with a history of breast cancer and atrophy-related complaints of GSM, the dual-phase protocol of vaginal Er:YAG laser application with ablative fractional and thermal mode was simple, effective and safe. Data suggest the approach to be a promising concept and may be offered to this specific patient group as non-hormonal alternative in the context of other conservative treatment options. A prospective cohort study employing validated evaluation instruments is warranted.
Limitations
The retrospective, single-center study design with missing details on particular breast cancer characteristics and previous adjuvant treatments as well as the small number of patients underline the preliminary character of this study.
In addition, due to the inclusion of patients with low-grade urogynecological symptoms not justifying further surgical intervention, comparisons of pre- and post-procedural results using other evaluation methods than patients’ subjective overall judgements were difficult.
Abbreviations
- QoL:
-
Quality of life
- GSM:
-
Genitourinary syndrome of menopause
- SUI:
-
Stress urinary incontinence
- ICS:
-
International Continence Society
- EGGS:
-
Expectations, goal setting, goal achievement, satisfaction
- SERM:
-
Selective estrogen receptor modulator
References
Alexiades-Armenakas MR, Dover JS, Arndt KA (2012) Fractional laser skin resurfacing. J Drugs Dermatol 11:1274–1287
Bachman GA, Noeyolitz M, Kelly SL (1992) Long-term non-hormonal treatment of vaginal dryness. Clin Pract Sex 8:3–8
Berga SL (2013) Profile of ospemifene in the breast. Reprod Sci 20:1130–1136. https://doi.org/10.1177/1933719113497290
Biglia N, Bounous VE, Sgro LG, D’Alonzo M, Pecchio S, Nappi RE (2015) Genitourinary syndrome of menopause in breast cancer survivors: are we facing new and safe hopes? Clin Breast Cancer 15:413–420. https://doi.org/10.1016/j.clbc.2015.06.005
Biglia N, Bounous VE, D’Alonzo M, Ottino L, Tuninetti V, Robba E, Perrone T (2017) Vaginal atrophy in breast cancer survivors: attitude and approaches among oncologists. Clin Breast Cancer. https://doi.org/10.1016/j.clbc.2017.05.008 (Epub ahead of print)
Brubaker L, Shull B (2005) EGGS for patient-centered outcomes. Int Urogynecol J Pelvic Floor Dysfunct 16:171–173
Buchholz S, Mögele M, Lintermans A, Bellen G, Prasauskas V, Ortmann O, Grob P, Neven P, Donders G (2015) Vaginal estriol–lactobacilli combination and quality of life in endocrine-treated breast cancer. Climacteric 18:252–259. https://doi.org/10.3109/13697137.2014.991301
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Cook ED, Iglehart EI, Baum G, Schover LL, Newman LL (2017) Missing documentation in breast cancer survivors: genitourinary syndrome of menopause. Menopause https://doi.org/10.1097/GME.0000000000000926. (Epub ahead of print)
Dmovsek-Olup B, Beltram M, Pizern J (2004) Repetitive Er:YAG laser irritation of human skin: a histological evaluation. Lasers Surg Med 35:146–151
Donders G, Neven P, Moegele M, Lintermans A, Bellen G, Prasauskas V, Grob P, Ortmann O, Buchholz S (2014) Ultra-low-dose estriol and Lactobacillus acidophilus vaginal tablets (Gynoflor(®)) for vaginal atrophy in postmenopausal breast cancer patients on aromatase inhibitors: pharmacokinetic, safety, and efficacy phase I clinical study. Breast Cancer Res Treat 145:371–379. https://doi.org/10.1007/s10549-014-2930-x
European Medicines Agency (2015). http://www.ema.europa.eu/ema. Assessment report EMA/78875/2015
Fisher JC (1992) Photons, physiatrics, and physicians: A practical guide to understanding laser light interaction with living tissue, part 1. J Clin Laser Med Surg 10:419–426
Gambacciani M, Palacios S (2017) Laser therapy for the restoration of vaginal function. Maturitas 99:10–15. https://doi.org/10.1016/j.maturitas.2017.01.012
Gambacciani M, Levancini M, Cervigni M (2015) Vaginal erbium laser: the second-generation thermotherapy for the genitourinary syndrome of menopause. Climacteric 18:757–763. https://doi.org/10.3109/13697137.2015.1045485
Gandhi J, Chen A, Dagur G, Suh Y, Smith N, Cali B, Ali Khan S (2016) Genitourinary syndrome of menopause: an overview of clinical manifestations, pathophysiology, etiology, evaluation, and management. Am J Obstet Gynecol 215:704–711. https://doi.org/10.1016/j.ajog.2016.07.045
Gaspar A, Brandi H, Gomez V, Luque D (2017) Efficacy of Erbium:YAG laser treatment compared to topical estriol treatment for symptoms of genitourinary syndrome of menopause. Laser Surg Med 49:160–168. https://doi.org/10.1002/lsm.22569
Hutchinson-Colas J, Segala S (2015) Genitourinary syndrome of menopause and the use of laser therapy. Maturitas 82:342–345. https://doi.org/10.1016/j.maturitas.2015.08.001
Jelovsek JE, Maher C, Barber MD (2007) Pelvic organ prolapse. Lancet 369:1027–1038
Lang P, Karram M (2017) Lasers for pelvic floor dysfunction: is there evidence? Curr Opin Obstet Gynecol 2017 29(5):354–358. https://doi.org/10.1097/GCO.0000000000000399
Majaron B, Srinivas SM, Huang HE, Nelson JS (2000) Deep coagulation of dermal collagen with repetetive Er:YAG laser irritation. Lasers Surg Med 26:215–222
Mothes AR, Wanzke L, Radosa MP, Runnebaum IB (2015) Bilateral minimal tension sacrospinous fixation in pelvic organ prolapse: an observational study. Eur J Obstet Gynecol Reprod Biol 188:1–5. https://doi.org/10.1016/j.ejogrb.2015.02.022
Mothes AR, Radosa MP, Altendorf-Hofmann A, Runnebaum IB (2016) Risk index for pelvic organ prolapse based on established individual risk factors. Arch Gynecol Obstet 293:617–624. https://doi.org/10.1007/s00404-015-3863-2
Nappi RE, Palacious S (2014) Impact of vulvovaginal atrophy on sexual health and quality of life at postmenopause. Climacteric 17:3–9. https://doi.org/10.3109/13697137.2013.871696
Nappi RE, Palacious S, Panay N, Particco M, Krychman ML (2016) Vulvar and vaginalatrophy in four European countries: evidence from the European REVIVE Survey. Climacteric 19:188–197. https://doi.org/10.3109/13697137.2015.1107039
Oyarzun MFG, Castelo-Branco C (2017) Local hormone therapy for genitourinary syndrome of menopause in breast cancer patients: is it safe? Gynecol Endocrinol 33:418–420. https://doi.org/10.1080/09513590.2017.1290076
Palacios S, Mejia A, Neyro L (2015) Treatment of genitourinary syndrome of menopause. Climacteric 18:23–29. https://doi.org/10.3109/13697137.2015.1079100
Pieralli A, Fallani MG, Becorpi A, Bianchi C, Corioni S, Longinotti M, Trdici Z, Guaschina S (2016) Fractional CO2 laser for vulvovaginal atrophy (VVA) dyspareunia relief in breast cancer survivors. Arch Gynecol Obstet 294:841–846. https://doi.org/10.1007/s00404-016-4118-6
Portman DJ, Gass ML, Vulvovaginal Atrophy Terminology Consensus Conference Panel (2014) Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and The North American Menopause Society. Climacteric 17:557–563. https://doi.org/10.3109/13697137.2014.946279
Salvatore S, Nappi RE, Zerbinati N et al (2014) A 12-week treatment with fractional CO2 laser for vulvovaginal atrophy: a pilot study. Climacteric 17:363–369. https://doi.org/10.3109/13697137.2014.899347
Santen RJ, Stuenkel CA, Davis SR, Pinkerton JV, Gompel A, Lumsden MA (2017) Managing menopausal symptoms and associated clinical issues in breast cancer survivors. J Clin Endocrinol Metab. https://doi.org/10.1210/jc.2017-01138 (Epub ahead of print)
Santoro N, Komi J (2009) Prevalence and impact of vaginal symptoms among postmenopausal women. J Sex Med 6:2133–2142. https://doi.org/10.1111/j.1743-6109.2009.01335
Schmitt L, Amann PM, Marquardt Y, Heise R, Czaja K, Gerber PA, Steiner T, Hölzle F, Baron JM (2017) Molecular effects of fractional ablative erbium:YAG laser treatment with multiple stacked pulses on standardized human three-dimensional organotypic skin models. Lasers Med Sci 32:805–814. https://doi.org/10.1007/s10103-017-2175-0
Siegel RL, Miller KD, Jemal A (2017) Cancer statistics, 2017. CA Cancer J Clin 67:7–30. https://doi.org/10.3322/caac.2138
Tadir Y, Gaspar A, Lev-Sagie A, Alexiades M, Alinsod R, Bader A, Calligaro A, Elias JA, Gambaciani M, Gaviria JE, Iglesia CB, Selih-Martinec K, Mwesigwa PL, Ogrinc UB, Salvatore S, Scollo P, Zerbinati N, Nelson JS (2017) Light and energy based therapeutics for genitourinary syndrome of menopause: consensus and controversies. Lasers Surg Med 49:137–159. https://doi.org/10.1002/lsm.22637
Vizintin Z, Lukac M, Kazic M, Tettamanti M (2015) Erbium laser in gynecology. Climacteric 18:4–8. https://doi.org/10.3109/13697137.2015.1078668
Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter HE, Markland AD (2014) Prevalence and trends of symptomatic pelvic floor disorders in US women. Obstet Gynecol 123:141–148. https://doi.org/10.1097/AOG.0000000000000057
Funding
MCL31 Dermablate was used at the expense of the company Asclepion Laser Technologies GmbH at the University Women’s Hospital, Jena University Hospital, Germany. Otherwise, only institutional funding has supported this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
ARM: Medical advisor for Asclepion Laser Technologies GmbH; received speaker honoraria; using MCL31 Dermablate at the expenses of the company at Jena University Hospital. MR: The Skin and Laser Center Landgrafen in Jena, Germany, is a reference center for Asclepion Laser Technologies GmbH; MR did not receive funding for this study. IBR: Chairman of the University Women´s Hospital Jena was supported by Asclepion Laser Technologies GmbH to use the MCL31 Dermablate at the expenses of the company.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. Ethical approval was granted on the 11th of August 2017 (No. 5246–8/17) by the Ethics Commission of the Faculty of Medicine and the University Hospital. Additional ethical approval was not necessary from the Ethics Commission of the Faculty of Medicine and the University Hospital, as anonymised data only were analyzed in this study.
Informed consent
Informed consent was obtained from all patients prior to treatment.
Rights and permissions
About this article
Cite this article
Mothes, A.R., Runnebaum, M. & Runnebaum, I.B. Ablative dual-phase Erbium:YAG laser treatment of atrophy-related vaginal symptoms in post-menopausal breast cancer survivors omitting hormonal treatment. J Cancer Res Clin Oncol 144, 955–960 (2018). https://doi.org/10.1007/s00432-018-2614-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-018-2614-8