Abstract
Purpose
This study is aimed at investigating the significance of gene promoter methylation status and protein expression of p16 INK4A and O6-methylguanine-DNA methyltransferase (MGMT) in the various uterine cervical lesions.
Materials and methods
Methylation status by using methylation-specific polymerase chain reaction (MS-PCR) and protein expression by using immunohistochemistry for p16 INK4A and MGMT genes were performed in cervical squamous intraepithelial neoplasms (CIN), invasive squamous cell carcinomas (SCC), adenocarcinomas and non-neoplastic cervices.
Results
None of 20 non-neoplastic cervices showed p16 INK4A and MGMT gene hypermethylation, whereas at least one of these genes was hypermethylated with 50.0% (5/10) of CIN I, 65.0% (13/20) of CIN II–III, 70.2% (33/47) of SCC and 85.0% (17/20) of adenocarcinoma. p16 INK4A protein was totally negative in non-neoplastic cervices, but positive with 90.0% of CIN I, 100% of CIN II–III and adenocarcinoma, and 78.7% of SCC. MGMT protein was expressed in 10% of non-neoplastic cervices, but significantly increased in SCC (42.5%) and adenocarcinoma (70.0%). The protein expression of p16 INK4A and MGMT was not related to their gene promoter methylation status.
Conclusions
The hypermethylation of p16 INK4A and MGMT genes in the uterine cervix may indicate the presence of malignant cells, and p16 INK4A immunostaining is useful in grading CIN and diagnosing invasive SCC and adenocarcinoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
DNA methylation is an essential mechanism for normal development, X chromosome inactivation, and gene imprinting [8, 44, 46]. However, the aberrant methylation of normally unmethylated CpG islands within the promoter regions of tumor-suppressor or cancer-related genes is a common epigenetic event leading to the silencing of gene expression in human cancers [1, 4, 9, 16, 18, 19, 25, 28, 32, 37].
Uterine cervical cancers are a worldwide common disease, and human papilloma virus (HPV) is a well-known etiologic factor [7, 15]. Cervical cancer development is the result of complex interactions between the host and environmental factors, undergoing stepwise progression from low-grade to high-grade dysplasia to invasive carcinoma. In this pathway, activation or inactivation of various cancer-related genes is involved [3, 17, 31, 39]. Recent studies have demonstrated the promoter hypermethylation of several genes, such as DAPK, p16 INK4A, O6-methylguanine-DNA methyltransferase (MGMT), APC, HIC-1, E-cadherin, RARß, FHIT, GSTP and hMLH1, associated with cervical carcinogenesis [13, 24, 43, 45, 48]. Among these, the p16 INK4A gene controls the cell cycle by inhibiting cyclin-dependent kinase 4 (cdk4)-mediated phosphorylation of several growth regulatory proteins such as retinoblastoma (Rb) [29, 40]. The promoter hypermethylation of p16 INK4A might result in transcriptional silencing, with a loss of functional activity [6, 28, 33, 47]. However, recent studies reported that p16 protein was strongly expressed in dysplastic and malignant cells of squamous and glandular epithelium of the uterine cervix [33, 38, 42], speculating that high-risk HPV E7 binds Rb protein, and that p16 INK4A is overexpressed through a negative feedback [21]. However, the expression of p16 INK4A in HPV-negative cancers should be explained by a HPV-independent pathway.
MGMT is a DNA repair protein, which transfers and accepts alkyl groups from the O6 position of guanine; it is important in protecting the cells from DNA damage [35]. A loss of function is implicated in a variety of human cancers [5, 14]. However, the presence of MGMT can be responsible for chemoresistance and poor prognosis of cancer patients [2, 20, 22, 23, 26]. Several reports have demonstrated the relatively high frequency of hypermethylation in high-grade dysplasia and invasive carcinoma of the cervix, speculating that it plays an important role in cervical carcinogenesis [12, 24, 43, 48].
In this study, the hypermethylation of p16 INK4A and MGMT genes was studied by methylation-specific PCR (MS-PCR). The expression of p16 INK4A and MGMT protein was immunohistochemically investigated to define the significance of the promoter hypermethylation and protein expression of these genes in cervical carcinogenesis.
Materials and methods
Materials
One hundred seventeen paraffin-embedded uterine cervical tissues, including 47 invasive squamous-cell carcinomas (nine stage IA, 19 stage IB, 11 stage IIA and eight stage IIB), 20 adenocarcinomas (12 stage IB and eight stage IIA), 30 cervical squamous intraepithelial neoplasia (ten CIN I, three CIN II and 17 CIN III), and 20 non-neoplastic cervices were selected from the Department of Pathology, Anam Hospital of Korea University. The tissues were routinely processed with 10% buffered formalin fixation and paraffin embedding. The hematoxylin-eosin (H-E) stained slides were reviewed, and one appropriate block from each case was selected for this study.
Methods
DNA extraction and methylation-specific PCR
Tissue sections from 117 paraffin-embedded blocks were deparaffinized in xylene before dehydration with 100% ethanol. Then, DNA was extracted by using the ‘High Pure PCR Template Preparation Kit’ (Roche, Germany). For the relatively specific cancer and CIN specimen selection, H-E slides were reviewed and selected the area of numerous cancer/CIN tumor cells and minor stroma as the target of DNA extraction. The Kai Sterile Dermal Biopsy Punch (Kai Industries, Japan) was used in some difficult cases. One μg of genomic DNA was denatured with 5 M NaOH, and bisulfite treatment was carried out for 16 h at 55°C. DNA samples were then purified using the Wizard DNA Clean-Up System (Promega, Madison, WI), treated again with NaOH, ethanol-precipitated and re-suspended in water, as described by Herman et al. [10].
The modified DNA was used as a template for methylation-specific PCR (MS-PCR). The primer sequences of p16 INK4A for the unmethylated reaction were sense 5′-TTATTAGAGGGTGGGGTGGATTGT-3′ and antisense 5′-CAACCCCAAACCACAACCATAA-3′, which amplify a 151-bp product (annealing temperature: 65°C). The primer sequences of p16 INK4A for methylated reaction were sense 5′-TTATTAGAGGGTGGGGCGGATCGC-3′ and antisense 5′-GACCCCGAACCGCGACCGTAA-3′, which amplify a 150-bp product (annealing temperature: 60°C). The primer sequences of MGMT for the unmethylated reaction were sense 5′-TTTGTGTTTTGATGTTTGTAGGTTTTTGT-3′ and antisense 5′-AACTCCACACTCTTCCAAAAACAAAACA-3′, which amplify a 93-bp product (annealing temperature: 66°C). The primer sequences of MGMT for methylated reaction were sense 5′-TTTCGACGTTCGTAGGTTTTCGC-3′ and antisense 5′-GCACTCTTCCGAAAACGAAACG-3′, which amplify an 81-bp product (annealing temperature: 66°C). [19].
PCR reactions were performed in a 25 μl reaction volume and hot-started at 95°C for 5 min. This was followed by 40 cycles of 95°C for 45 s, appropriate annealing temperature for 45 s and 72°C for 45 s, and concluded at 72°C for 5 min. PCR products were analyzed on 12% polyacrylamide gel, stained with ethidium bromide and visualized under UV light.
Immunohistochemistry for p16INK4A and MGMT
For an immunohistochemical study with DAKO LSAB kit (DAKO A/S, Denmark), 4-μm thick tissue sections were deparaffinized and rehydrated. Endogenous peroxidase activity was eliminated by incubation with 3% H2O2 in methanol for 15 min. The antigen was retrieved at 103 kPa for 2 min by placing the slides in 0.01 M sodium citrate buffer (pH 6.0). The slides were incubated with the primary monoclonal antibodies for p16 INK4A (1:25, mtm Laboratories, Germany) and MGMT (1:50, NeoMarkers, Fremont, CA) for 1 h at room temperature. After incubation at room temperature for 30 min with biotinylated link, the sections were incubated with streptavidin-peroxidase complex at room temperature for 30 min. Immunostaining was visualized by using 3,3′diaminobenzidine. The sections were counterstained with hematoxylin. As a negative control, 0.1 M Tris buffer (pH 7.6) replaced the primary antibody.
The immunohistochemical results were evaluated as (+) when more than 5% of the epithelial cells were stained.
Statistical analysis
Statistical analysis was performed by using the x 2-test of the SPSS software program. A p value of less than 0.05 was considered statistically significant.
Results
Hypermethylation of p16 INK4A and MGMT genes
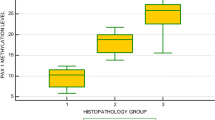
All of the cases showed only unmethylated or methylated DNA band or both. Hypermethylation was detected in 20.0% (2/10) and 30.0% (3/10) of CIN I, 50.0% (10/20) and 35.0% (7/20) of CIN II–III, 53.2% (25/47) and 38.3% (18/47) of SCC, and 60.0% (12/20) and 45.0% (9/20) of adenocarcinoma, respectively. Significantly, at least one of p16 INK4A and MGMT hypermethylation was detected in 50% (5/10) of CIN I, 65.0% (13/20) of CIN II–III, 70.2% (33/47) of SCC, and 85.0% (17/20) of adenocarcinoma. In SCC, stage IIB lesions showed a higher rate of methylation, 87.5% for p16 INK4A and 50.0% for MGMT. The prevalence of methylation in one of the genes was progressively increased according to the stages, without statistical significance. All 20 cases of non-neoplastic cervices showed an unmethylation pattern for both p16 INK4A and MGMT. (Fig. 1 and 2)
Methylation-specific polymerase chain reaction for MGMT methylation. Lanes 1 and 2: non-neoplastic cervices; lanes 3 and 4: squamous cell carcinoma; lanes 5 and 6: cervical adenocarcinoma; lanes 7–9: CIN III. ( M 50 bp size marker, m methylation, u unmethylation, CIN cervical squamous intraepithelial neoplasm)
Immunohistochemistry for p16 INK4A and MGMT protein expression
p16 INK4A was specifically stained in the cytoplasm and/or nucleus of the dysplastic and malignant cells, but not in the reactive and normal cervical epithelial and stromal cells. The staining for MGMT was mainly found in the suprabasal layer of non-neoplastic cervices and stromal lymphocytes. p16 INK4A protein was expressed in 78.7% (37/47) of SCC, 90.0% (9/10) of CIN I, 100% (20/20) of CIN II–III, and 100% (20/20) of adenocarcinoma, but not expressed in any non-neoplastic cervices. However, MGMT protein showed immunoreactivity in 10% (2/20) of non-neoplastic cervices, whereas its expression was seen in 42.5% (20/47) of SCC and 70.0% (14/20) of adenocarcinoma. The positive signals were stronger in SCC and adenocarcinoma than in the non-neoplastic cervices. There were no significant differences among the clinical stages. (Fig. 3 and 4)
Immunostaining for p16 INK4A in the uterine cervical lesions. (LSAB kit, ×200). The staining for p16 INK4A is negative in the normal cervix ( A). The dysplastic squamous epithelium of CIN II is positive for p16 INK4A ( B). Squamous cell carcinoma ( C)and adenocarcinoma ( D) are strongly positive for p16 INK4A ( CIN cervical squamous intraepithelial neoplasm)
Immunostaining for MGMT in uterine cervical lesions. (LSAB kit, ×200). The cells of basal and suprabasal layers of the squamous epithelium are positive for MGMT. The lymphocytes in stroma are also positive ( A). The dysplastic epithelium in CIN II is strongly positive for MGMT, in contrast to the negative staining in the normal gland ( B). Squamous cell carcinoma ( C) and adenocarcinoma ( D) are strongly positive for MGMT ( CIN cervical squamous intraepithelial neoplasm)
Relationship between protein expression and hypermethylation of p16 INK4A and MGMT
The expression of p16 INK4A was higher in methylated groups (91.8%) than in unmethylated groups (60.3%) without statistical significance. The expression of MGMT was similar in methylated (48.6%) and unmethylated (38.8%) groups. The protein expressions of p16 INK4A and MGMT were not correlated with the hypermethylation of promoter genes.
Discussion
The hypermethylation of promoter regions is one of the major mechanisms by which cancer-related genes, such as p14 ARF, p15 INK4b, p16 INK4a, VHL, Rb1, hMLH, HIC, MGMT, RAR-ß2, and DAPK, are inactivated [4, 13, 16, 28, 37, 45, 47]. This epigenetic alteration has been described in uterine cervical cancers. Dong et al. [13] investigated promoter hypermethylation of six genes, p16 INK4A, APC, HIC-1, DAPK, MGMT and E-cadherin, in squamous cell carcinoma and adenocarcinoma of the uterine cervix, and detected at least the aberrant methylation of one of these genes in 79% of the cases. Virman et al. [43] also analyzed aberrant methylation of p16 INK4A, RARß, FHIT, GSTP1, MGMT, and hMLH1 in normal and neoplastic cervical tissues and cell lines, reporting that the aberrant methylation occurred at an early stage during multistage pathogenesis and increased with a pathologic change. Cohen et al. [12] described the hypermethylation of RASSF1A promoter in uterine cervical adenocarcinoma, but not in squamous cell carcinoma. Recently, Yang et al. [48] detected hypermethylation in one of DAPK, p16 INK4A, and MGMT genes in 75.3% of tumors and 55% of plasma of cervical cancers.
Hypermethylation of p16 INK4A in uterine cervical cancers was detected in 28.2% in a study by Yang et al. [48], and 53% by Lea et al. [24]. Virmani et al. [43] reported a progressive increase of hypermethylation during cervical carcinogenesis; 3% of non-dysplasia/low-grade CIN, 24% of high-grade CIN and 42% of invasive cancers. Dong et al. [13] and Lea et al. [24] reported more frequent hypermethylation of p16 INK4A in SCC than in adenocarcinoma (39% vs 18%, and 61% vs 37%), but this was not found in the study of Yang et al. [48]. In our study, the prevalence of p16 INK4A hypermethylation was 53.2% of SCC and 60.0% of adenocarcinoma.
The reported frequencies of MGMT promoter hypermethylation in uterine cervical cancers were 10% of SCC and 5% of adenocarcinoma in the study by Dong et al. [13] and 3%, 29% and 26% of non-dysplasia/low-grade CIN, high-grade CIN and invasive cancers in the study by Virmani et al. [43]. Yang et al. [48] reported 18.8% of MGMT hypermethylation in cervical cancers (11% of SCC and 5% of adenocarcinoma). In our study, MGMT hypermethylation was seen in 30% of CIN I, 35.0% of CIN II–III, 38.3% of SCC and 45.0% of adenocarcinoma. However, all 20 cases of non-neoplastic cervices showed an unmethylation pattern. MGMT methylation indicates cellular changes of malignant possibility.
Hypermethylation of p16 INK4A and MGMT was more frequent in our study than in the previous ones. It may be due to the scanty contamination of normal cells by selecting the tumor cells by dissection.
Hypermethylation in at least one of p16 INK4A and MGMT genes showed statistically higher frequency in CIN, SCC and adenocarcinoma than in the non-neoplastic cervices; however, it did not show any correlation with histologic types and clinical stages in this study. The combined detection of p16 INK4A and MGMT methylation status might be useful in detecting a possible presence of cervical dysplasia and malignancy.
The results of p16 INK4A immunohistochemistry showed that all cases of non-neoplastic cervices were negative. The positive rate increased significantly in CIN I (90.0%), CIN II–III (100%), SCC (78.7%) and adenocarcinoma (100%). The positive signals were specifically located in the cytoplasm and nucleus of the dysplastic or malignant cells, but not in the reactive and normal cervical epithelium and stromal components. The data were consistent with other previous studies [21, 38, 42], strongly indicating that p16 INK4A immunostaining is useful in grading CIN, and evaluating the glandular lesions. Depending on the antibodies used in immunohistochemistry, some of the normal or reactive squamous and glandular epithelial cells were positive for p16 INK4A [30]. The antibody used in our study was consistently negative in non-neoplastic cells. The expression of p16 in high-grade CIN and invasive squamous cell carcinoma has been considered the result of high-risk HPV E7-mediated degradation of protein Rb (pRb). However, the fact that adenocarcinoma, less commonly associated with high-risk HPV than squamous lesions, showed a strong expression of p16 in almost all cases, suggesting that other mechanisms should be defined.
Nuovo et al. [34] nicely detected hypermethylation of the p16 INK4A gene by methylation-specific PCR in situ hybridization (MSP-ISH) and demonstrated a loss of protein in hypermethylated cervical cancer cells. Considering the fact that the high proportion of the cervical squamous lesions is associated with HPV and shows positive staining for p16 INK4A, hypermethylation of p16 INK4A does not seem related with the loss of protein. In our study, the expression of p16 INK4A was strong and high in both squamous lesions and adenocarcinoma, without regard to gene hypermethylation status. According to Dong et al. [13], there was no correlation between the promoter hypermethylation of p16 INK4A and the presence of HPV.
According to the cell type, the amount of MGMT protein differs and decreases in some tumors in comparison with their normal counterparts [10, 11]. Several studies have demonstrated that the inactivation of a repair gene by promoter hypermethylation resulted in the impaired expression of MGMT protein [2, 9, 14, 18, 22]. The loss of protein was uniform in lymphoma, but tumors of the colon, lung, and brain showed cellular heterogeneity or stronger expression than adjacent normal tissues [14, 23, 27, 36, 41, 49]. According to Kokkinakis et al. [23], MGMT protein was absent in the hyperplastic and normal components of pancreatic tissues, but invariably present in dysplastic foci and especially strong in the invasive component of pancreatic cancer. They suggested that MGMT activity is up-regulated in dysplastic epithelium and that its expression increases during a tumor progression. In our study, only two of 20 non-neoplastic cervices showed MGMT expression in the suprabasal layers of squamous epithelium, whereas dysplastic and malignant lesions showed a significantly increased expression (40% and 42.5%, respectively, of CIN II–III and SCC, and 70.0% of adenocarcinoma). However, the protein expression of MGMT was not correlated with promoter hypermethylation. This result was concordant with the previous reports [36]. Since MGMT is a DNA repair protein, the intracellular localization should be nuclear. However, our study showed that the immunohistochemical staining for MGMT was found both in the cytoplasm and nucleus. Belanich et al. [5] demonstrated the clear cytoplasmic and nuclear localization of MGMT in brain tumors, but only nuclear localization in the breast cancer. The significance of cytoplasmic localization of MGMT should be defined.
The protein expression and methylation status of both p16 INK4A and MGMT genes were not different in the various stages of cervical cancers, suggesting that p16 INK4A and MGMT gene alterations might play a role in early carcinogenesis. Furthermore, the lack of difference of p16 INK4A and MGMT expression between methylated and unmethylated lesions raises the possibility of other mechanisms participating in controlling p16 INK4A and MGMT protein expression.
In conclusion, p16 INK4A and MGMT hypermethylation may play an important role in the progression of uterine cervical cancer. Consequently, p16 INK4A immunostaining can be used as a diagnostic marker of intraepithelial and invasive neoplasm of squamous and glandular epithelium.
References
Ahluwalia A, Hurteau JA, Bigsby RW, Nephew KP (2001) DNA methylation in ovarian cancer. Gynecol Oncol 82:299–304
Anda T, Shabani HK, Tsunoda K, Tokunaga Y, Kaminogo M, Shibata S, Hayashi T, Iseki M (2003) Relationship between expression of O6-methylguanine-DNA methyltransferase, glutathione-S-transferase pi in glioblastoma and the survival of the patients treated with nimustine hydrochloride: an immunohistochemical analysis. Neurol Res 25:241–248
Aoyama C, Peters J, Senadheera S, Liu P, Shimada H (1998) Uterine cervical dysplasia and cancer: identification of c-myc status by quantitative polymerase chain reaction. Diagn Mol Pathol 7:324–330
Baylin SB, Herman JG, Graff JR, Vertino PM, Issa JP (1998) Alterations in DNA methylation: a fundamental aspect of neoplasia. Adv Cancer Res 72:141–196
Belanich M, Randall T, Pastor MA, Kibitel JT, Alas LG, Dolan ME, Schold SC, Gander M, Lejeune FJ, Li BFL, White AB, Wasserman P, Citron ML, Yarosh DB (1996) Intracellular localization and intercellular heterogeneity of the human DNA repair protein O6-methylguanine-DNA methyltransferase. Cancer Chemother Pharmacol 37:547–555
Belinsky SA, Nikula KJ, Palmisano WA, Michels R, Saccomanno G, Gabrielson E, Baylin SB, Herman JG (1998) Aberrant methylation of p16 INK4a is an early event in lung cancer and a potential biomarker for early diagnosis. Proc Natl Acad Sci U S A 95:11891–11896
Castle PE, Wacholder S, Lorincz AT, Scott DR, Sherman ME, Glass AG, Rush BB, Schussler JE, Schiffman M (2002) A prospective study of high-grade cervical neoplasia risk among human papillomavirus-infected women. J Natl Cancer Inst 94:1406–1414
Cedar H (1998) DNA methylation and gene activity. Cell 53:3–4
Choy KW, Pang CP, To KF, Yu CB, Ng JS, Lam DS (2002) Impaired expression and promoter hypermethylation of O6-methylguanine-DNA methyltransferase in retinoblastoma tissues. Invest Ophthalmol Vis Sci 43:1344–1349
Citron M, Decker R, Chen S, Schneider S, Graver M, Kleynerman L, Kahn LB, White A, Schoenhaus M, Yarosh D (1991) O6-methylguanine-DNA methyltransferase in human normal and tumor tissue from brain, lung, and ovary. Cancer Res 51:4131–4134
Citron M, Graver M, Schoenhaus M, Chen S, Decker R, Kleynerman L, Kahn LB, White A, Fornace AJ Jr, Yarosh D (1992) Detection of messenger RNA from O6-methylguanine-DNA methyltransferase gene MGMT in human normal and tumor tissues. J Natl Cancer Inst 84:337–340
Cohen Y, Singer G, Lavie O, Dong SM, Beller U, Sidransky D (2003) The RASSF1A tumor suppressor gene is commonly inactivated in adenocarcinoma of the uterine cervix. Clin Cancer Res 9:2981–2984
Dong SM, Kim HS, Rha SH, Sidransky D (2001) Promoter hypermethylation of multiple genes in carcinoma of the uterine cervix. Clin Cancer Res 7:1982–1986
Esteller M, Hamilton SR, Burger PC, Baylin SB, Herman JG (1999) Inactivation of the DNA repair gene O6-methylquanine-DNA-methyltransferase by promoter hypermethylation is a common event in primary human neoplasia. Cancer Res 59:793–797
Ferenczy A, Franco E (2002) Persistent human papillomavirus infection and cervical neoplasia. Lancet Oncol 3:11–16
Gonzalez-Zulueta M, Bender CM, Yang AS, Nguyen T, Beart RW, Van Tornout JM, Jones PA (1995) Methylation of the 5′ CpG island of the p16/CDKN2 tumor suppressor gene in normal and transformed human tissues correlates with gene silencing. Cancer Res 55:4531–4535
Hellend A, Karlsen F, Due EU, Holm R, Kristensen G, Borresen-Dale A (1998) Mutations in the TP53 gene and protein expression of p53, MDM 2 and p21/WAF-1 in primary cervical carcinomas with no or low human papillomavirus load. Br J Cancer 78:69–72
Herfarth KK, Brent TP, Danam RP, Remack JS, Kodner IJ, Wells (1999) A specific CpG methylation pattern of the MGMT promoter region associated with reduced MGMT expression in primary colorectal cancers. Mol Carcinog 24:90–98
Herman JG, Graff JR, Myohanen S, Nelkin BD, Baylin SB (1996) Methylation-specific PCR: A novel PCR assay for methylation status of CpG islands. Proc Natl Acad Sci U S A 93:9821–826
House MG, Guo M, Efron DT, Lillemoe KD, Cameron JL, Syphard JE, Hooker CM, Abraham SC, Montgomery EA, Herman JG, Brock MV (2003) Tumor suppressor gene hypermethylation as a predictor of gastric stromal tumor behavior. J Gastrointest Surg 7:1004–1014
Kleas R, Friedrich T, Spitkovsky D, Ridder R, Rudy W, Petry U, Dallenbach-Hellweg G, Schmidt D, von Knebel Doeberitz M (2001) Overexpression of p16(INK4A) as a specific marker for dysplastic and neoplastic epithelial cells of the cervix uteri. Int J Cancer 92:276–284
Kohya N, Miyazaki K, Matsukura S, Yakushi H, Kitajima Y, Kitahara K, Fukuhara M, Nakabeppu Y, Sekiguchi M (2002) Deficient expression of O6-methylguanine-DNA methyltransferase combined with mismatch-repair proteins hMLH1 and hMSH2 is related to poor prognosis in human biliary tract carcinoma. Ann Surg Oncol 9:371–379
Kokkinakis DM, Ahmed MM, Delgado R, Fruitwala MM, Mohiuddin M, Albores-Saavedra J (1997) Role of O6-methylguanine-DNA methyltransferase in the resistance of pancreatic tumors to DNA alkylating agents. Cancer Res 57:5360–5368
Lea JS, Coleman R, Kurien A, Schorge JO, Miller DS, Minna JD, Muller CY (2004). Aberrant p16 methylation is a biomarker for tobacco exposure in cervical squamous cell carcinogenesis. Am J Obstet Gynecol 190:674–679
Lin H, Huber R, Schessinger D, Morin PJ (1999) Frequent silencing of the GPC3 gene in ovarian cancer cell lines. Cancer Res 59:807–810
Ma S, Egyhazi S, Ueno T, Lindholm C, Kreklau EL, Stierner U, Ringborg U, Hansson J (2003) O6-methylguanine-DNA-methyltransferase expression and gene polymorphisms in relation to chemotherapeutic response in metastatic melanoma. Br J Cancer 89:1517–1523
Mattern J, Koomagi R, Volm M (1998) Smoking-related increase of O6-methylguanine-DNA methyltransferase expression in human lung carcinomas. Carcinogenesis 19:1247–1250
Merlo A, Herman JG, Mao L, Lee DJ, Gabrielson E, Burger PC, Baylin SB, Sidransky D (1995) 5′CpG island methylation is associated with transcriptional silencing of the tumour suppressor p16/CDKN2/MTS1 in human cancers. Nat Med 1:686–692
Medema RH, Herrera RE, Lam F, Weinberg RA (1995) Growth suppression by p16ink4 requires functional retinoblastoma protein. Proc Natl Acad Sci U S A 92:6289–6293
Milde-Langosch K, Riethdorf S, Kraus-Poppinghaus A, Riethdorf L, Loning T (2001) Expression of cyclin-dependent kinase inhibitors p16MTS1, p21WAF1, and p27KIP1 in HPV-positive and HPV-negative cervical adenocarcinomas. Virchows Arch 439:55–61
Muller CY, O’Boyle JD, Fong KM, Wistuba II, Biesterveld E, Ahmadian M, Miller DS, Gazdar AF, Minna JD (1998) Abnormalities of fragile histidine triad genomic and complementary DNAs in cervical cancer: association with human papillomavirus type. J Natl Cancer Inst 90:433–439
Myohanen SK, Baylin SB, Herman JG (1998) Hypermethylation can selectively silence individual p16 INK4A alleles in neoplasia. Cancer Res 58:591–593
Negri G, Egarter-Vigl E, Kasal A, Romano F, Haitel A, Mian C (2003) p16 INK4A is a useful marker for the diagnosis of adenocarcinoma of the cervix uteri and its precursors. An immunohistochemical study with immunocytochemical correlations. Am J Surg Pathol 27:187–193
Nuovo GJ, Plaia TW, Belinsky SA, Baylin SB, Herman JG (1999) In situ detection of the hypermethylation-induced inactivation of the p16 gene as an early event in oncogenesis. Proc Natl Acad Sci U S A 96:2754–2759
Pegg AE, Wiest L, Foote RS, Mitra S, Perry W (1983) Purification and properties of O6-methylguanine-DNA transmethylase from rat liver. J Biol Chem 258:2327–2333
Rosas SL, Koch W, da Costa Carvalho MG, Wu L, Califano J, Westra W, Jen J, Sidransky D (2001) Promoter hypermethylation patterns of p16, O6-methylguanine-DNA-methyltransferase, and death-associated protein kinase in tumors and saliva of head and neck cancer patients. Cancer Res 61:939–942
Rood BR, Zhang H, Cogen PH (2003) Intercellular heterogeneity of expression of the MGMT DNA repair gene in pediatric medulloblastoma. Neuro-oncol 6:200–207
Sano T, Masuda N, Oyama T, Nakajima T (2001) Overexpression of p16 and p14ARF is associated with human papillomavirus infection in cervical squamous cell carcinoma and dysplasia. Pathol Int 52:375–383
Sharma A, Pratap M, Sawhney VM, Khan IU, Bhambhani S, Mitra AB (1999) Frequent amplification of C-erbB2 (HER-2/Neu) oncogene in cervical carcinoma as detected by non-fluorescence in situ hybridization technique on paraffin sections. Oncology 56:83–87
Sherr CI (1994) The ins and outs of RB: coupling gene expression to the cell cycle clock. Trends Cell Biol 4:15–18
Silber JR, Mueller BA, Ewers TG, Berger MS (1993) Comparison of O6-methylguanine-DNA methyltransferase activity in brain tumors and adjacent normal brain. Cancer Res 53:3416–3420
Tringler B, Gup CJ, Singh M, Groshong S, Shroyer AL, Heinz DE, Shroyer KR (2004) Evaluation of p16INK4a and pRb expression in cervical squamous and glandular neoplasia. Hum Pathol 35:689–696
Virmani AK, Muller C, Rathi A, Zoechbauer-Mueller S, Mathis M, Gazdar AF (2001) Aberrant methylation during cervical carcinogenesis. Clin Cancer Res 7:584–589
Walsh CP, Bestor TH (1999) Cytosine methylation and mammalian development. Genes Dev 13:26–34
Widschwendter M, Berger J, Hermann M, Muller HM, Amberger A, Zeschnigk M, Widschwendter A, Abendstein B, Zeimet AG, Daxenbichler G, Marth C (2000) Methylation and silencing of the retinoic acid receptor-beta2 gene in breast cancer. J Natl Cancer Inst 92:826–832
Wigler M, Levy D, Perucho M (1982) The somatic replication of DNA methylation. Cell 24:33–40
Wong YF, Chung TK, Cheung TH, Nobori T, Yim SF, Lai KWH, Yu AL, Diccianni MB, Li TL, Chang MZ (1997) p16 INK4A and p15 INK4B alterations in primary gynecologic malignancy. Gynecol Oncol 65:319–324
Yang HJ, Lin VWS, Wang Y, Chan KYK, Tsang PCK, Khoo US, Cheung ANY, Ngan HYS (2004). Detection of hypermethylated genes in tumor and plasma of cervical cancer patients. Gynecol Oncol 93:435–440
Zaidi NH, Liu L, Gerson SL (1996) Quantitative immunohistochemical estimates of O6-alkylguanine-DNA alkyltransferase expression in normal and malignant human colon. Clin Cancer Res 2:577–584
Acknowledgement
This study was supported by Brain Korea 21 Task Force
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Lin, Z., Gao, M., Zhang, X. et al. The hypermethylation and protein expression of p16 INK4A and DNA repair gene O 6-methylguanine-DNA methyltransferase in various uterine cervical lesions. J Cancer Res Clin Oncol 131, 364–370 (2005). https://doi.org/10.1007/s00432-004-0657-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-004-0657-5