Abstract
Purpose
Paclitaxel is an important agent in the pharmacological treatment of metastatic breast cancer. Despite its efficacy in selected patients, the majority of patients have a resistance against paclitaxel. The aim of this study was to identify the responding patients and hence prevent the other patients from ineffective treatment. Identifying these patients could spare them an ineffective treatment and could in turn characterize a subgroup of patients with a higher response rate.
Material and methods
Thirty-three patients with metastatic breast cancer received paclitaxel 175 mg/m2 either as first- (15 patients) or as second-line (18 patients) treatment. Immunohistochemistry was performed on the blocks of the primary tumors with monoclonal antibodies against p53, HER-2/neu, P-glycoprotein, Glutathione-S-Transferase-π, and β-tubulin II. The expression of those factors was then correlated with the objective response to paclitaxel.
Results
Ten of 33 patients had an objective response to treatment. A significant correlation with the objective response was found for the expression of p53. None of the tumors with p53 expression (n=11) responded to paclitaxel. In contrast, 10 of the 22 patients without p53 expression showed an objective response (P=0.013). Expression of HER-2/neu, P-glycoprotein, Glutathione-S-Transferase-π, and β-tubulin II did not show a correlation with the response to paclitaxel.
Conclusion
The immunohistochemical detection of p53 characterizes patients with metastatic breast cancer unlikely to respond to paclitaxel.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Paclitaxel has a well-established role in the treatment of metastatic breast cancer. Depending on the administration as a first- or as a second-line chemotherapy, between 18% and 30% objective response can be achieved (Michael et al. 1997; Bishop et al. 1999). Despite this anti-tumor efficacy of paclitaxel, tumors exhibit intrinsic or acquired resistance to paclitaxel in a majority of patients. These patients obviously will not profit from this therapy. Identifying these patients could not only spare them an ineffective treatment, but should also help to identify a subset of patients with an expected higher rate of objective treatment responses.
There exists a plethora of factors which can lead to resistance to certain chemotherapeutic agents. Most of these factors were established in vitro: P-glycoprotein (Pgp) acts as a drug efflux pump contributing to resistance to natural product-based chemotherapeutics such as paclitaxel (Bradley et al. 1989; Eck et al. 1993). Likewise, Glutathione-S-Transferase-π (GST) is involved in mechanisms leading to drug resistance (Meijer et al. 1990). The intracellular target for paclitaxel anti-tumor action is tubulin. Hence, changes in the expression of certain tubulin-isotypes correlate with resistance to paclitaxel in vitro (Mallarino et al. 1995). Mutations of p53 have an influence on DNA repair mechanisms and apoptosis and can thus lead to chemoresistance (Rouby et al. 1993). Finally, HER-2/neu was shown to afford resistance against paclitaxel in vitro (Yu et al. 1996).
Despite these in vitro efforts, the relevance of these predictive factors for therapeutic decision-making in the clinic needs to be established in a prospective clinical trial. In order to identify the most promising predictive factors for such a trial, we investigated the role of the above-mentioned factors in 33 patients with metastatic breast cancer treated with paclitaxel.
Patients and methods
We selected 33 patients (age 34 to 69 years, median 54 years) from our breast clinic treated for metastatic breast cancer with paclitaxel 175 mg/m2 q3w in a first- or a second-line protocol. Inclusion criteria were as follows: first, paraffin-embedded tumor tissue was available for immunohistochemical studies; second, the objective response to treatment was documented in the files. Of the selected 33 patients 15 patients were treated in a first-line and 18 patients were treated in a second-line protocol. An objective response to paclitaxel treatment was found in ten patients (30%). These patients all presented with a partial remission. A complete response to paclitaxel treatment was not found in our collective. Patient characteristics are given in Table 1 and Table 2.
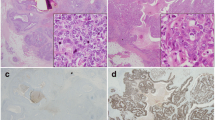
Immunohistochemistry
Serial sections of formalin-fixed, paraffin-embedded blocks were first deparaffinized. Then they were microwaved in 10 mmol/l of citrate buffer, pH 6.0, to unmask the epitopes and treated with 1% hydrogen peroxide for 10 min to block the endogenous peroxidase. The sections were incubated with either monoclonal p53 antibodies (clone DO-1, Calbiochem-Dianova, Boston, USA) diluted 1:100 for 30 min at 37 °C, monoclonal HER-2/neu antibodies (clone CB-11, Novocastra, Newcastle-upon-Tyne, UK) diluted 1:50 for 30 min at 37°, monoclonal P-glycoprotein antibodies (clone ISB-1, Novocastra) diluted 1:50 for 24 h at 4 °C, monoclonal Glutathione-S-Transferase-π antibodies (clone 353–10, Dako, Glostrup, Denmark) diluted 1:30 for 30 min at 37 °C and monoclonal β-tubulin II antibodies (clone IDR-3B8, Bio Genex, San Ramon, USA) diluted 1:60 for 30 min at 37 °C. The sections were then incubated with a biotin-labeled secondary antibody and streptavidin-peroxidase for 20 min each. Tissue was then stained for 5 min with 0.05% 3´3-diaminobenzidine-tetrahydrochloride and counterstained with hematoxylin. All series included appropriate positive and negative controls. All controls gave adequate results. The immunohistochemical evaluation was performed by one of the authors (MS) trained in histological and immunohistochemical diagnostics, unaware of the clinical data. Immunostaining was semiquantitatively scored for both extent (percentage of positive tumor cells: 0%, score = 0; <5%, score = 1; 5–20%, score = 2; 21–50%, score = 3; >50%, score = 4) and intensity (absent, score = 0; weak, score = 1; moderate, score = 2; strong, score = 3). Both scores were multiplied to give a composite score (0–12) for each tumor. In addition to this semiquantitative approach the immunostaining was classified into positive or negative with a cut-off of 10% of the tumor cells.
Statistical analysis
The Statistical Package for Social Science (SPSS, Chicago, Ill., USA) was used for the statistical analysis. Differences in proportion were evaluated by Fisher's exact test. Significance was considered as two-sided P<0.05.
Results
Immunohistochemistry
Six tumors expressed Pgp (18%). A membrane-bound overexpression of HER-2/neu was found in eight cases (24%). Twenty-five tumors expressed β-tubulin II (76%). An expression of GST was found in 22 (67%). Eleven tumors showed an expression of p53 (33%). The composite score for p53 gave similar results using a cut-off value of 2. Immunohistochemical results are given in Table 3.
Clinicopathologic correlations
We then investigated the correlation of the factors determined immunohistochemically both to each immunohistochemical finding and to known clinical data (age, primary tumor size, nodal status, grade, hormone receptor status, hepatic metastasis, disease-free interval, number of chemotherapies, and number of metastatic sites): no correlation with any of these parameters could be found for p53. There were only slight correlations between Pgp, GST, β-tubulin II, and age. β-tubulin II and HER-2/neu showed a slight correlation to the disease-free interval if only the composite score was considered. However, classification as positive or negative alone failed to show such a correlation. Finally, patients with an higher immunohistochemical score for β-tubulin II also had a higher score for GST (P=0,0008) (data not shown).
Analysis of objective response
A significant correlation with the objective response was found for p53 both using the qualitative assessment and the combined score. None of the tumors with p53 expression showed an objective response (Fig. 1). The P-value of Fisher's exact test was 0.013. Of the 22 patients not expressing p53, an objective response was found in 10 patients and no response was documented in the remaining 12 patients (55%).
In the group treated first-line for metastatic disease, three of 11 patients who did not express p53, failed to respond to paclitaxel (27%). In contrast, all four patients who expressed p53 did not profit from the treatment. In the second-line protocol there was no objective response seen in the seven patients expressing p53, and no objective response in nine of 11 patients not expressing p53 (82%).
Pgp, GST, β-tubulin II, and HER-2/neu did not show a correlation with the objective response (Figs. 2, 3, 4, 5). These findings applied to both the quantitative assessment and the combined score. The distribution of the combined score for the different parameters is shown in Fig. 6.
a Distribution of the immunohistochemical scores for p53 in relation to the objective response. * >3 × interquartile range; b distribution of the immunohistochemical scores for β-tubulin II, P-glycoprotein (Pgp), Glutathione-S-Transferase-π (GST), and HER-2/neu in relation to the objective response. °1.5–3 × interquartile range; bars, mean
Discussion
The objective anti-tumor response to a treatment with paclitaxel monotherapy is strongly influenced by its administration as either first-line or as second-line chemotherapy. Michael et al. (Michael et al. 1997) found an overall response in 18% of the patients with metastatic breast cancer treated with a second-line paclitaxel chemotherapy. In contrast Bishop and colleagues (Bishop et al. 1999) reported an objective response rate of 30% in patients with metastatic breast cancer treated first-line with paclitaxel. Our own results compare with an objective response of 30% for combined first and second-line treatment. Beside the number of chemotherapy regimens, clinically useful factors to assess the prognosis in metastatic breast cancer are a short disease-free interval and the presence of hepatic metastases (Yamamoto et al. 1998). These factors are established at the time of diagnosis of metastatic disease and influence the choice of therapy. However, these factors alone are not sufficient to accurately predict the actual response to individual therapeutic agents.
During the last few years a number of possible mechanisms of resistance against paclitaxel have been characterised. While these were mainly evaluated under in vitro conditions, data on their clinical relevance are completely lacking.
The most intensively studied factor is Pgp. Pgp has been suggested to contribute to resistance to natural product-based chemotherapeutic agents like paclitaxel (Gan et al. 1995). Pgp works as a drug efflux pump and diminishes the cellular concentration of paclitaxel, which in turn leads to the development of drug resistance (Mechetner et al. 1998).
There is extensive in vitro evidence for this proposed role in paclitaxel resistance (Gan et al. 1998; van Ark-Otte et al. 1998). However, in analogy to our present results (Fig. 2), the role of Pgp in metastatic breast cancer appears to play only a limited role in the clinical setting (Linn et al. 1997; Yang et al. 1999).
Another widely investigated mechanism of resistance against paclitaxel is the overexpression of HER-2/neu. Yu and co-workers (Yu et al. 1996) found that HER-2/neu overexpression leads to paclitaxel resistance in vitro via mdr-1-independent mechanisms. This finding was later confirmed by the in vitro demonstration that downregulation of HER-2/neu, either with adenoviral type 5 E1A (Ueno et al. 2000) or with the tyrosine kinase inhibitor emodin (Zhang et al. 1999), sensitizes HER-2/neu overexpressing cells to paclitaxel. However, to overcome the problem of combined genetic changes in established cancer cell lines Orr and co-workers (Orr et al. 2000) studied the effect of HER-2/neu overexpression on paclitaxel sensitivity of normal human mammary epithelial cells. These authors found that HER-2/neu overexpression was not sufficient by itself to induce changes in chemosensitivity. Indeed, in vivo data are conflicting. In our present study (Fig. 5) we found no effect of HER-2/neu overexpression on the objective response of patients with metastatic breast cancer treated with paclitaxel. To further complicate matters, Baselga and co-workers (Baselga et al. 1997) found patients with HER-2/neu overexpressing breast cancer to respond three times better to paclitaxel, rather than worse.
Antitubulin agents like paclitaxel block cell division by inhibition of the mitotic spindle. To accomplish this, paclitaxel stabilizes the microtubules (Schiff et al. 1979). Furthermore, it inhibits the microtubule dynamics (Derry et al. 1995). Microtubules are composed of a- and β-tubulins which exist under the form of isotypes (Luduena 1998).
In vitro evidence links an increased expression of the β-tubulin II isotype to the development of a high level of resistance to paclitaxel (Haber et al. 1995). This important study has so far not been investigated in an in vivo setting. Even though we found a trend towards higher immunoreactive scores for β-tubulin II in the paclitaxel-resistant tumors, the difference to paclitaxel-responsive tumors failed to yield statistical significance (Fig. 4). Newer in vitro studies (Nicoletti et al. 2001) also failed to find a correlation between isotype expression and paclitaxel sensitivity.
Because of the importance of the intracellular levels of glutathione on the development of chemoresistance (Arrick and Nathan 1984), we investigated a potential influence of Glutathione-S-Transferase-π (GST-π) on paclitaxel responsiveness. GST-π catalyzes the conjugation of glutathione to several chemotherapeutic drugs (Dirven et al. 1994) and Masanek and co-workers (Masanek et al. 1997) showed that ovarian cancer lines resistant to paclitaxel overexpressed GST-π. In contrast to these promising in vitro data, Shiga and coworkers (Shiga et al. 1999) failed to see an effect of GST-π on the response of head and neck cancers on a therapy with cisplatin/paclitaxel in a neoadjuvant setting. Our present findings (Fig. 3) are hence in line with the lack of a clinical relevance of GST-π in chemotherapy resistance.
The induction of apoptosis linked to an intact p53 is of pivotal importance for the action of several chemotherapeutic agents (Lowe et al. 1994). In an attempt to elucidate the effects of paclitaxel in vitro, Milross and co-workers (Milross et al. 1996) found that the antitumor effect of paclitaxel was strongly correlated with paclitaxel-induced apoptosis, but not with mitotic arrest. Since an intact p53 plays a major role in apoptosis, we evaluated the p53 status by means of immunohistochemistry on the primary tumor tissue. The concordance between p53 expression immunohistochemically and gene mutation is reported to be 79% for breast cancer specimens (Soong et al. 1996). The p53 status of the primary tumor measured immunohistochemically predicts the p53 status of the metastasis correctly in almost all cases (Shimizu et al. 2000). Hence, the setting of this study is adequate to assess the impact of p53 on the response of patients with metastatic breast cancer treated with paclitaxel. Most reports dealing with the influence of p53 on the resistance for paclitaxel are limited by the fact that they are either purely in vitro or that they are conflicting. Giannakakou and co-workers (Giannakakou et al. 2000) and Lanni and co-workers (Lanni et al. 1997) found cells with deficient p53 being resistant to paclitaxel. Nielsen and co-workers (Nielsen et al. 1998) as well as Gurnani and co-workers (Gurnani et al. 1999) showed that adenovirus-mediated p53 gene therapy was synergistic with paclitaxel. This could point to an important role of functioning p53 for the effects of paclitaxel. However, others (Chadderton et al. 2000; Oldham et al. 2000) failed to show an effect of p53 on paclitaxel activity in vitro. Wahl and coworkers (Wahl et al. 1996) showed that in vitro paclitaxel anti-tumor activity was enhanced—rather than reduced—in tumors with defective p53. This in vitro finding was supported by a study of primary breast cancer treated in a neoadjuvant setting with paclitaxel (Kandioler-Eckersberger et al. 2000). In this study eight of 12 tumors which expressed p53 responded to the treatment. This observation led the authors to conclude that loss of cell cycle control due to p53 deficiency could allow tumor cells to more effectively enter mitosis, hence supporting the tubulin-specific cytotoxicity of paclitaxel. However, results of Milross and co-workers (Milross et al. 1996) suggested that the antitumor effect of paclitaxel are correlated with paclitaxel-induced apoptosis and not with mitotic arrest. The role of p53 in paclitaxel-induced apoptosis was also studied by Woods and coworkers (Woods et al. 1995) who showed that paclitaxel can induce two independent apoptotic pathways. One of those is p53 dependent while the other is p53 independent. More recently, other in vitro studies showed different results concerning the influence of p53 on the response to paclitaxel: for ovarian carcinoma cell lines Cassinelli and co-workers (Cassinelli et al. 2001) found enhanced sensitivity to paclitaxel only in p53 mutant cells and Das and co-workers (Das et al. 2001) found no significant effect of wild-type p53 on the level of paclitaxel induced apoptotic cell death in lung cancer cell lines.
The influence of p53 in metastatic breast cancer treated with paclitaxel has been investigated only recently. Linn and coworkers (Linn et al. 1997) evaluated nine patients with metastatic breast cancer treated with paclitaxel. The p53 status was known in five patients. None of those patients responded to the treatment and one expressed p53. Clearly, it was not possible to draw reliable conclusions from such a limited number of patients.
More recently, Van Poznak and co-workers (Van Poznak et al. 2002) retrospectively analyzed the p53 status in 144 patients with single-agent taxane therapy but failed to see an effect of p53 status on the objective treatment response. In contrast to these results, our present findings suggest that p53 positive tumors entirely fail to respond to paclitaxel. This discrepancy could be explained in several ways: first, the population of Poznak and co-workers is rather heterogeneous. Patients were treated with either paclitaxel or docetaxel in different dosages and schedules; second, they used a p53 antibody which was different from the antibody used in our study. All of this might conceal the differences in objective response to paclitaxel treatment observed in our study.
Even though ours is a retrospective study with a rather small number of patients, these findings could potentially have clinical impact. In particular, in a palliative situation, such as metastatic breast cancer, it is mandatory to spare the patients a presumably ineffective therapy. Furthermore, response rates need to be corrected in that patients without p53 expression can be expected to have higher response rates than hitherto described in the literature for a population with unstratified p53 status. Taking the p53 expression into account could potentially help to tailor a therapy to the individual molecular phenotype of a particular tumor. Since we used immunohistochemistry on the primary tumor block, which is easily accessible for most of the patients and which translates well to the p53 status in the metastatic tumor cells (Shimizu et al. 2000), these results could be applicable to the vast majority of patients with metastatic breast cancer. We believe the observation precluded herein warrants confirmation in a larger series of patients which would then open the door towards a more effective tailoring of chemotherapy regimens based on the expected anti-tumor efficacy.
References
Arrick BA, Nathan CF (1984) Glutathione metabolism as a determinant of therapeutic efficacy: a review. Cancer Res 44:4224–4232
Baselga J, Seidman AD, Rosen PP, Norton L (1997) HER2 overexpression and paclitaxel sensitivity in breast cancer: therapeutic implications. Oncology 11[Suppl 2]:43–48
Bishop JF, Dewar J, Toner G, Smith J, Tattersall MH, Olver I, Ackland S, Kennedy I, Goldstein D, Gurney H, Walpole E, Levi J, Stephenson J, Canetta R (1999) Initial paclitaxel improves outcome compared with CMFP combination chemotherapy as front-line therapy in untreated metastatic breast cancer. JCO 17:2355–2364
Bradley G, Naik M, Ling V (1989) P-Glykoprotein expression in multidrug resistant human ovarian carcinoma cell lines. Cancer Res 49:2790–2796
Cassinelli G, Supino R, Perego P, Polizzi D, Lanzi C, Pratesi G, Zunino F (2001) A role for loss of p53 function in sensitivity of ovarian carcinoma cells to taxanes. Int J Cancer 92:738–747
Chadderton A, Villeneuve DJ, Gluck S, Kirwan-Rhude AF, Gannon BR, Blais DE, Parissenti AM (2000) Role of specific apoptotic pathways in the restoration of paclitaxel-induced apoptosis by valspodar in doxorubicin-resistant MCF-7 breast cancer cells. Breast Cancer Res Treat 59:231–244
Das GC, Holiday D, Gallardo R, Haas C (2001) Taxol-induced cell cycle arrest and apoptosis: dose response relationship in lung cancer cells of different wild-type p53 status under isogenic condition. Cancer Lett 165:147–153
Derry WB, Wilson L, Jordan MA (1995) Substoichiometric binding of taxol suppresses microtubule dynamics. Biochem 34:2203–2211
Dirven HA, van Ommen B, van Bladeren PJ (1994) Involvement of human glutathione S-transferase isoenzymes in the conjugation of cyclophosphamide metabolites with glutathione. Cancer Res 54:6215–6220
Eck L, Pavich D, Fruehauf JP (1993) MDR-1 expression by human ovarian tumors is associated with taxol resistance. Proc Am Assoc Cancer Res 34:232
Gan YB, Balturshot G, Millenbaughm NJ, Chen CT, Kalns JE, Lim C, Wientjes MG, Au JL (1995) P-Glykoproteinexpression in human tumors and its correlation with chemosensitivity to taxol and cell mobility. Proc Am Assoc Cancer Res 36:334
Gan YB, Wientjes MG, Au JL (1998) Relationship between paclitaxel activity and pathobiology of human solid tumors. Clin Cancer Res 4:2949–2955
Giannakakou P, Poy G, Zhan Z, Knutsen T, Blagosklonny MV, Fojo T (2000) Paclitaxel selects for mutant or pseudo-null p53 in drug resistance associated with tubulin mutations in human cancer. Oncogene 19:3078–3085
Gurnani M, Lipari P, Dell J, Shi B, Nielsen LL (1999) Adenovirus-mediated p53 gene therapy has greater efficacy when combined with chemotherapy against human head and neck, ovarian, prostate and breast cancer. Cancer Chemother Pharmacol 44:143–151
Haber M, Burkhart CA, Regl DL, Madafiglio J, Norris MD, Horwitz SB (1995) Altered expression of M beta 2, the class II beta-tubulin isotype, in an murine J774.2 cell line with a high level of taxol resistance. J Biol Chem 270:31269–31275
Kandioler-Eckersberger D, Ludwig C, Rudas M, Kappel S, Janschek E, Wenzel C, Schlagbauer-Wadl H, Mittlboeck M, Gnant M, Steger G, Jakesz R (2000) TP53 mutation and p53 overexpression for prediction of response to neoadjuvant treatment in breast cancer patients. Clin Cancer Res 6:50–56
Lanni JS, Lowe SW, Licitra EJ, Liu JO, Jacks T (1997) p-53 independent apoptosis induced by paclitaxel through an indirect mechanism. Proc Natl Acad Sci USA 94:9679–9683
Linn SC, Pinedo HM, van Ark-Otte J, van der Valk P, Hoekman K, Honkoop AH, Vermorken J, Giaccone G (1997) Expression of drug resistance proteins in breast cancer, in relation to chemotherapy. Int J Cancer 71:787–795
Lowe SW, Bodis S, McClatchey A, Remington L, Ruley HE, Fisher DE, Housman DE, Jacks T (1994) p53 status and the efficacy of cancer therapy in vivo. Science 266:807–810
Luduena RF (1998) Multiple forms of tubulin: different gene products and covalent modifications. Int Rev Cytol 178:207–275
Mallarino MC, Duran GE, Dumontet CM, Sikic BI (1995). Mechanisms of resistance in a human sarcoma cell line continuously selected with paclitaxel (Taxol, TAX) and SDZ PSC 833. Proc Am Assoc Cancer Res 36:320
Masanek U, Stammler G, Volm M (1997) Messenger RNA expression of resistance proteins and related factors in human ovarian carcinoma cell lines resistant to doxorubicin, taxol and cisplatin. Anti-Cancer Drugs 8:189–198
Mechetner E, Kyshtoobayeva A, Zonis S, Kim H, Stroup R, Garcia R, Parker RJ, Fruehauf JP (1998) Levels of multidrug resistance (MDR-1) P-glycoprotein expression by human breast cancer correlate with in vitro resistance to taxol and doxorubicin. Clin Cancer Res 4:389–398
Meijer C, Mulder NH, De Vries EGE (1990) The role of detoxifying systems in resistance of tumor cells to cisplatin and adriamycin. Cancer Treat Rev 7:389–407
Michael M, Bishop JF, Levi JA, Bell DR, Zalcberg JR, Friedlander ML, Olver IN, Smith JG, Toner GC (1997) Australian multicenter phase II trial of paclitaxel in women with metastatic breast cancer and prior chemotherapy. Med J Austral 10:520–523
Milross CG, Mason K, Hunter NR, Chung VK, Peters LJ, Milas L (1996) Relationship of mitotic arrest and apoptosis to antitumor effect of paclitaxel. J Natl Cancer Inst 88:1308–1314
Nicoletti MI, Valoti G, Giannakakou P, Zhan Z, Kim JH, Lucchini V, Landoni F, Mayo JG, Giavazzi R, Fojo T (2001) Expression of beta-tubulin isotypes in human ovarian carcinoma xenografts and in a sub-panel of human cancer cell lines from the NCI-Anticancer Drug Screen: correlation with sensitivity to microtubule active agents. Clin Cancer Res 7:2912–2922
Nielsen LL, Lipari P, Dell J, Gurnani M, Hajian G (1998) Adenovirus-mediated p53 gene therapy and paclitaxel have synergistic efficacy in models of human head and neck, ovarian, prostate, and breast cancer. Clin Cancer Res 4:835–846
Oldham EA, Li C, Ke S, Wallace S, Huang P (2000) Comparison of action of paclitaxel and poly(L-glutamic acid)-paclitaxel conjugate in human breast cancer cells. Int J Oncol 16:125–132
Orr MS, O´Connor PM, Kohn KW (2000) Effects of c-erbB2 overexpression on the drug sensitivities of normal human mammary epithelial cells. J Natl Cancer Inst 92:987–994
Rouby S, Thomas A, Costin D, Rosenberg CR, Potmesil M (1993) p53 mutation in B-cell chronic lymphocytic leukemias associated with drug resistance and is independent of MDR1/MDR3 gene expression. Blood 82:3452–3459
Schiff PB, Fant J, Horwitz SB (1979). Promotion of microtubule assembly in vitro by taxol. Nature 277:665–667
Shiga H, Heath EI, Rasmussen AA, Trock B, Johnston PG, Forastiere AA, Langmacher M, Baylor A, Lee M, Cullen KJ (1999) Prognostic value ofp53, glutathione-S-transferase π, and thymidylate synthase for neoadjuvant cisplatin-based chemotherapy in head and neck cancer. Clin Cancer Res 5:4097–4104
Shimizu C, Fukutomi T, Tsuda H, Akashi-Tanaka S, Watanabe T, Nanasawa T, Sugihara K (2000) c-erbB-2 protein overexpression and p53 immunoreaction in primary and recurrent breast cancer tissues. J Surg Oncol 73:17–20
Soong R, Robbins PD, Dix BR, Grieu F, Lim B, Knowles S, Williams KE, Turbett GR, House AK, Iacopetta BJ (1996) Concordance between p53 protein overexpression and gene mutation in a large series of common human carcinomas. Hum Pathol 27:1050–1055
Ueno NT, Bartholomeusz C, Herrmann JL, Estrov Z, Shao R, Andreeff M, Price J, Paul RW, Anklesaria P, Yu D, Hung MC (2000) E1A-mediated paclitaxel sensitisation in HER-2/neu-overexpressing ovarian cancer SKOV3.ip1 through apoptosis involving the caspase-3 pathway. Clin Cancer Res 6:250–259
van Ark-Otte J, Samelis G, Rubio G, Lopez Saez JB, Pinedo HM, Giaccone G (1998) Effects of tubulin-inhibiting agents in human lung and breast cancer cell lines with different multidrug resistance phenotypes. Oncol Rep 5:249–255
van Poznak C, Tan L, Panageas KS, Arroyo CD, Hudis C, Norton L, Seidmann AD (2002) Assessment of molecular markers of clinical sensitivity to single-agent taxane therapy for metastatic breast cancer. JCO 20:2319–2326
Wahl AF, Donaldson KL, Fairchild C, Lee FY, Foster SA, Demers GW, Galloway DA (1996) Loss of normal p53 function confers sensitisation to taxol by increasing G2/M arrest and apoptosis. Nature Med 2:72–79
Woods CM, Zhu J, McQueney PA, Bollag D, Lazarides E (1995) Taxol-induced mitotic block triggers rapid onset of a p53-independent apoptotic pathway. Molec Med 1:506–526
Yamamoto N, Watanabe T, Katsumata N, Omuro Y, Ando M, Fukuda H, Tokue Y, Narabayashi M, Adachi I, Takashima S (1998) Construction and validation of a practical prognostic index for patients with metastatic breast cancer. J Clin Oncol 16:2401–2408
Yang X, Uziely B, Groshen S, Lukas J, Israel V, Russell C, Dunnington G, Formenti S, Muggia F, Press MF (1999) MDR1 gene expression in primary and advanced breast cancer. Lab Invest 79:271–280
Yu D, Liu B, Tan M, Li J, Wang SS, Hung MC (1996) Overexpression of c-erbB-2/neu in breast cancer cells confers increased resistance to taxol via mdr-1-independent mechanisms. Oncogene 13:1359–1365
Zhang L, Lau YK, Xia W, Hortobagyi GN, Hung MC (1999) Tyrosise kinase inhibitor emodin suppresses growth of HER-2/neu-overexpressing breast cancer cells in athymic mice and sensitises these cells to the inhibitory effect of paclitaxel. Clin Cancer Res 5:343–353
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported in part by a grant from Bristol Myers Squibb. The results were partly presented at the annual meeting of the German Society for Senology in Berlin 2001.
Rights and permissions
About this article
Cite this article
Schmidt, M., Bachhuber, A., Victor, A. et al. p53 expression and resistance against paclitaxel in patients with metastatic breast cancer. J Cancer Res Clin Oncol 129, 295–302 (2003). https://doi.org/10.1007/s00432-003-0430-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-003-0430-1