Abstract
Pediatricians’ job performance, work engagement, and job satisfaction are essential for both the individual physician and quality of care for their little patients and parents. Therefore, it is important to maintain or possibly augment pediatricians’ individual and professional competencies. In this study, we developed and implemented a psychosocial competency training (PCT) teaching different psychosocial competencies and stress coping techniques. We investigated (1) the influence of the PCT on work-related characteristics: stress perception, work engagement, job satisfaction and (2) explored pediatricians’ outcomes and satisfaction with PCT. Fifty-four junior physicians working in pediatric hospital departments participated in the training and were randomized in an intervention (n = 26) or a control group (n = 28). In the beginning, at follow-up 1 and 2, both groups answered a self-rated questionnaire on perceived training outcomes and work-related factors. The intervention group showed that their job satisfaction significantly increased while perceived stress scores decreased after taking part in the PCT. No substantial changes were observed with regard to pediatricians’ work engagement. Participating physicians evaluated PCT with high scores for training design, content, received outcome, and overall satisfaction with the training.
Conclusion: Professional psychosocial competency training could improve junior pediatricians’ professional skills, reduce stress perception, increase their job satisfaction, and psychosocial skills. In addition, this study indicates that the PCT is beneficial to be implemented as a group training program for junior pediatricians at work.
What is Known: • Junior pediatricians often report experiencing high levels of job strain and little supervisory support. • High levels of job demands make pediatricians vulnerable for mental health problems and decreased work ability. |
What is New: • Development, implementation, and evaluation of a psychosocial competency training for junior pediatricians working in clinical settings • Psychosocial competency training has the potential to improve pediatricians’ psychosocial skills and perceptions of perceived work-related stress and job satisfaction. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Junior pediatricians often report experiencing a high workload, irregular working hours, limited supervisory support, and little autonomy at work [35, 36]. These demands, together with a high degree of work–privacy conflicts, make pediatricians vulnerable for stress-related strain and raise concerns about their mental health and work ability [5, 25]. Self-reported data indicate that the time span during postgraduate training is especially linked with increasing symptoms of anxiety, depression, and high levels of perceived stress [28]. Studies discussed possible reasons, for example, excessive sleep deprivation due to long working hours, high levels of quantitative job demands, poor supervisory support, low job autonomy, and minimal work-related feedback [19]. Despite a rich literature on physicians’ work-related distress, very limited research has been performed on effective initiatives to support junior physicians during their first years at clinical practice. One important method is to improve adequate skills and coping strategies on how to manage different work situations. Individual coping strategies refer to the specific efforts, both behavioral and mental, that individuals can use to handle, tolerate, and reduce stressful events [8].
Some studies of stress management interventions have demonstrated that improving employees’ individual skills such as learning coping techniques lead to reduced job stress and increased job satisfaction [9]. As demonstrated, psychosocial skill training and counseling are effective in decreasing work-related stress, increasing job performance [23, 33], and lowering levels of anxiety, anger, and depressive symptoms among employees [16]. Further investigations demonstrated effects of improved physicians’ job performance and patient care [14].
Aim of this study
The aim of this study was to implement and evaluate a psychosocial competence training (PCT) for junior physicians working in pediatric medicine involving psychosocial skills training and cognitive-behavioral as well as solution-focused. To our knowledge, no previous study evaluated the effects of such a training program for junior physicians in pediatric medicine. Therefore, we investigated (1) the effects of a PCT program on pediatricians’ characteristics that potentially affect the quality of medical care: work engagement, job satisfaction, and stress perception and (2) analyzed pediatricians’ perceptions of a PCT program and its outcomes.
Methods
Study design and participants
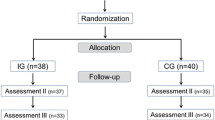
This study was designed as a randomized controlled trial. Junior physicians working in clinic departments of pediatrics were recruited from ten hospitals. Pediatricians were contacted via email and/or direct communication to participate in the psychosocial skills training and counseling program. Inclusion criteria were (1) employment in pediatrics (2) working full-time in a hospital (3) work experience of less than 2 years (4) being able and willing to participate (5) agreement to complete three questionnaires.
Fifty-four junior pediatricians gave their consent to be included in this study. Study participants were randomized into two groups (intervention and comparison group): (1) names of the pediatricians were listed in alphabetical order and (2) afterwards each name got a random number. The numbers had been allocated from number tables to the intervention or comparison group. In sum, 26 physicians took part in the intervention group and 28 participated in the comparison group. The study was performed between May and October 2014.
Intervention
The intervention group participated in a psychosocial skills training, combined with cognitive-behavioral and solution-focused counseling. Two qualified psychologists, both trained in cognitive-behavioral and solution-focused work performed the PCT in two training groups. The PCT consisted of 12 weekly sessions of 1.5 h, which focused on current working situations and problems, coping strategies, and support between colleagues and future professional goals. The training sessions included theoretical input, watching videos, oral group discussions, experimental exercises, and home assignments. In each session, a topic was introduced and discussed: (1) introduction: “working life of a pediatrician”, (2) first work experiences in pediatrics, (3) and (4) psychosocial skills for pediatricians (mindfulness, self-awareness, resilience), (5) handling conflict in the work setting, (6) seeking guidance about one’s own clinical performance in pediatric medicine, (7) relaxation techniques (progressive muscle relaxation), (8) organizational culture, reporting one’s own mistakes and dealing with mistakes caused by others, (9) communication in the hospital setting, (10) dealing with difficult decisions, social support, how to speak up to supervisors and senior physicians, (11) self-care, coping with work-related stress, and lastly, (12) session evaluation. The comparison group received no intervention but was asked to complete the questionnaire at baseline and at follow-up 1 and 2. The comparison group did not receive any support related to the intervention topic like any other psychosocial skills training, counseling, or therapy.
Survey procedure
Pediatricians of both groups (ig and cg) were asked to complete an online survey prior to receiving the first intervention lesson (baseline), after 12 weeks (follow-up 1) and after 6 months (follow-up 2). The survey was conducted by using a secure web-based survey system, via links within email messages. The link to the baseline survey was sent after the participating pediatrician signed a consent form. The follow-up survey link was emailed 12 weeks after the last session, the link for the follow-up 2 survey another 6 months later.
Pediatricians’ evaluation of the PCT intervention program
Job satisfaction, perceived stress, and work engagement were the main study outcome variables. Baseline outcome measures evaluated at baseline and after 3 month included the Perceived Stress Questionnaire (PSQ), Copenhagen Psychosocial Questionnaire (COPSOQ), and the Work Engagement Scale (UWES).
Pediatricians’ psychological job stress was measured with the PSQ [18]. The items of the PSQ can be answered with a 4-point rating scale and (1= almost never, 2= sometimes, 3= often, and 4= usually) and refer to the period of the last month. The COPSOQ was used to analyze pediatricians’ job satisfaction [15, 22]. Pediatricians’ job satisfaction was measured with four items on a four-point Likert scale (very satisfied, satisfied, not satisfied, very dissatisfied) with higher scores indicating more job satisfaction. Sufficient quality criteria have been stated for the German version of the COPSOQ [22, 24].
Pediatricians’ work engagement was measured using the short version of the Utrecht Work Engagement Scale (UWES-9). The scale includes nine items/questions on three main factors: physicians’ vigor, absorption, and dedication. Answers could be given on a 7-point rating scale ranging from ‘never’ to ‘always/daily’. Higher scores represent a higher level of work engagement [27, 29]. The German version of the UWES has shown sufficient quality criteria (i.e., internal consistency) [26].
To evaluate pediatricians’ perception of the PCT intervention program, we developed a questionnaire based on the four ‘levels’ of the training evaluation criteria from Kirkpatrick’s model [13]. Course evaluation also included questions on training outcome and design (e.g., practice transfer of techniques and skills learned, interest, usefulness, etc. (see Table 3). Pediatricians were asked to respond to the questions on a scale ranging from 1 (‘totally disagree’) to 5 (‘totally agree’). In addition to these outcome parameters as reported, the pediatricians were asked to give grades as an overall course evaluation (1-fail to 5-best).
Statistics
Descriptive statistics were used to describe the study sample. We also analyzed whether at baseline, the intervention and comparison groups differed in mean scores of socio-demographic factors and outcome measures (e.g., job satisfaction) with t tests for independent samples. Pediatricians’ mean scores on work engagement, job satisfaction, and perceived stress were measured at baseline and two follow-up time slots for the intervention and comparison groups. Regression analyses were performed to analyze effects of the PCT program on pediatricians’ job satisfaction, perceived stress, and work engagement. We reported the results as regression coefficients (b) and 95 % confidence intervals (CI) and P values where relevant. The quantitative analyses were performed using the statistical software IBM SPSS Statistics Version 22.0.
Results
Physicians’ characteristics
Sixty-nine percent of the pediatricians in the intervention group were women (n = 18) and 31 % were men (n = 8) and 71 % women (n = 20) vs. 29 % men (n = 8) in the comparison group. The mean age was 27 years among all participants (SD = 2.1). The average time working as a physician was 1 year (SD = 1.13). Baseline data on socio-demographic differences indicate only small, insignificant differences between our intervention and comparison group.
Pediatricians outcome measure: work engagement, job satisfaction, and perceived stress
Pediatricians’ scores on work engagement, job satisfaction, and perceived stress in both the intervention and control group at baseline (T0) and follow-up (1) and follow-up (2) are described in Table 1. We found that among physicians participating in the PCT program, job satisfaction scores increased significantly by 0.40 (95 % CI 0.28–0.59, P = 0.01). No significant changes were analyzed in the comparison group. For the intervention group, a significant decrease was observed in perceived stress (−0.23; 95 % CI −0.31–0.12) P = 0.01). No significant changes were analyzed in the comparison group.
In addition, no significant changes were found for work engagement (P > .05), neither for the intervention nor the control group.
Table 2 shows the results of the adjusted regression analyses for the influence of the PCT program on pediatricians’ job satisfaction, perceived stress, and work engagement. The study results show that pediatricians’ job satisfaction scores are positively associated with the PCT program (b = 0.39; 95 % CI 0.15–0.62; P = 0.001). In addition, the PCT program was also significantly associated with physicians’ perceptions of work-related stress (b = 0.28; 95 % CI 0.11–0.51; P = 0.02). The study results demonstrated that pediatricians’ work engagement scores were not significantly associated with the PCT program (b = −0.07; 95 % CI 0.04–0.19; P = 0.71).
Pediatricians’ perception of the PCT program
In Table 3, the scores of the training evaluation (e.g., the overall training outcome and design) are illustrated. The evaluation results show an overall training satisfaction median score of 4.02. The median score for training design was 3.98. The evaluation of the training outcome ranged between a median score of 3.01 (practice) and 4.20 (recommendation).
The analysis of the training evaluation demonstrates that after the PCT all four levels of Kirkpatrick’s training criteria could be met and were satisfactory. Pediatricians reported they learned to understand the values and principles of stress management and its practice in every day work (learning criteria). Regarding the criteria impact on behavior, pediatricians mostly stated the usage of the practical everyday instructions that are applicable in their clinical work life. They practice these strategies and skills in stressful work situations. For the fourth criteria, it is important to recognize that the participating physicians report that they feel more at comfort, experience a feeling of more control, and better focused when applying and repeating exercises learned in the psychosocial competency training.
Discussion
Main findings
Physicians in pediatric medicine demonstrated improved psychosocial skills and satisfaction and reduced stress levels after participating in a psychosocial stress management program. Pediatricians rated the training positively, and in terms of changed behavior they integrated practical contents in their daily clinical practice. The alteration of means in some of the outcome variables between the baseline and the follow-up measures may be considered rather small, but a summation of the small differences in all targeted factors may have a clinical significance [4]. The comparison between the intervention and control group, after adjusting for pre-intervention measures, showed a significant difference in the means of all dependent outcome factors except work engagement. All other factors had improved in the intervention group.
Explanation and interpretation of findings
The results of our study as presented showed a significant effect of psychosocial skills training and counseling, indicating the high potential/urgent need of psychosocial skill training for pediatricians.
In addition, physicians’ subjective reports demonstrated that the intervention is relevant and important in clinical practice. Pediatricians’ perceptions of the PCT program show an overall positive evaluation of the training with high scores for training design, training outcomes, and overall satisfaction with the training.
Our outcomes can be compared to similar studies describing a significant decrease on stress perceptions after stress reduction trainings [14, 30]. In line to our assumptions and published literature [3, 6, 12], we were able to show effects of the psychosocial training on subjective scores of perceived stress.
Additional psychosocial and stress management trainings have been implemented in different work settings and have been proven effective in many work collectives [6, 7, 17, 38]. In detail, Krasner et al. published an evaluation of communication training and self-awareness that delivered improved outcomes of physicians’ work-related mindfulness and perceived job stress [14]. Other research groups have studied stress reduction programs offered during residency. They demonstrated similar improvements in stress reduction and decreased emotional exhaustion scores in comparison to the control group [10, 21]. These results might function as burn-out prevention in a long-term perspective considering the influence of, e.g., job satisfaction in this construct.
Reduction of perceived stress after such an intervention might be explained by the active usage of coping skills, and a better regulation of one’s own thoughts, feelings, and actions [11].
These findings imply that PCT is suitable to support junior pediatricians: after the PCT, they reported handling (problematic) work situations more successfully. In addition, we found that the pediatricians gained a certain level of reflection and awareness concerning the stressful and challenging character of their work in pediatric medicine. In connection, this study focuses only on junior physicians in pediatric medicine. However, since previous studies showed that physicians from many other medical specialties have to deal with stressful working conditions in German hospitals (i.e., high workload, irregular working hours etc.) [2, 20], we assume this intervention would be of advantage in other medical settings and specialties as well.
In the evaluation of the PCT program, we found that the PCT is related with all training levels of Kirkpatrick [13]: the participating pediatricians demonstrated an increase of attachment and awareness of the relevance for physicians’ well-being, the use of the learned trainings in coping with stressful situations and tasks, and improvement in their professional psychosocial skills. The overall reported positive changes and evaluation in pediatricians’ psychosocial skills after the PCT are inspiring for further intervention studies.
In this study, we also found evidence that the training program could improve self-reported job satisfaction. Former studies also showed effects of stress management interventions on perceptions of job satisfaction [1, 31, 37].
The results of our study also included changes in physicians’ work engagement. However, a significant improvement could not be found. A comparable study performed by van Berkel et al. (2014), also did not find any relations to employees’ work engagement after participating in a mental health worksite intervention [34]. Two additional studies have also examined the effectiveness of a workplace intervention on work engagement. These studies did not find an overall effect on work engagement either [30, 32]. An explanation for the results might be that the ‘ceiling effect’ happened. This could be the case since the baseline scores were at such a high level that a significant improvement is not very likely [34].
Strengths and limitations
This study is the first to evaluate psychosocial competency training for junior pediatricians specifically. The strength of this study is the controlled study design. In addition, the duration of the follow-up was 12 months, which can be considered unique for worksite intervention research. The high response rate in this study demonstrates a further strength: the drop-out rate (loss to follow-up) was very low.
The major limitations of this pilot study are its small sample size in terms of external validity of the study results.
Although we demonstrated significant improvements in the outcome variables, we cannot conclude from our findings whether the intervention has any preventive long-term effect on mental health issues. We recommend that the PCT should be repeated in larger intervention studies with multiple follow-ups and longer periods of time. A further limitation is the assignment of only two experienced trainers who provided the training sessions. Standardization of trainings is difficult, and personal bias is probably influential but could not be measured in this study.
In addition, it cannot be ensured that pediatricians from the comparison group did not engage in self-study or may have been influenced by their colleagues who have been included in the intervention group. We assume that although the physicians in the control group did not take part in the intervention, they used alternative activities and/or strategies to cope with daily challenges (i.e., talking to friends, family or using self-help techniques). Unfortunately, we did not ask them about such alternatives. This can only be strongly recommended for further studies in the future.
Conclusion
The study results suggest that psychosocial competency training could be instrumental in increasing pediatricians’ job outcomes, job satisfaction, and job stress perception. Overall, the participating pediatricians gave positive feedback about psychosocial competency training, thus justifying the implementation of such program in medical education and advanced training.
The advisability of implementing interventions to promote mental health in a clinical setting is the most relevant practical implication of the present study. The fact that, although the comparison group and the intervened group shared similar levels of perceived job stress at baseline, only the intervened group improved their scores for perceived stress and satisfaction, suggests that intervention played an active role in promoting positive effects. More counseling programs developed on a larger scale might very well improve junior physicians’ psychological states and job performance.
Results of such intervention studies combined with topics directed towards physicians’ work environment (i.e., work organization) itself may also show the efficiency of such a program on other work-related outcomes (absenteeism etc.). Provision of opportunities for pediatricians to learn protective coping techniques and skills integrated in the work life should be a future goal for hospitals. A training opportunity like this is generally adaptable and could be easily implemented in different hospital departments.
Continuation of this PCT program for physicians is strongly recommended. Follow-up surveys of the participating pediatricians to evaluate sustainability of the positive findings will hopefully be conducted as requested by the participating pediatricians.
Abbreviations
- b:
-
Beta weight
- CI:
-
Confidence interval
- COPSOQ:
-
Copenhagen Psychosocial Questionnaire
- N:
-
Numbers
- M:
-
Mean
- MD:
-
Median
- P:
-
Probability
- PCT:
-
Psychosocial competency training
- SD:
-
Standard deviation
- UWES:
-
Utrecht Work Engagement Scale
References
Ayres J, Malouff JM (2007) Problem-solving training to help workers increase positive affect, job satisfaction, and life satisfaction. Eur J Work Organ Psychol 16:279–294
Bernburg M, Vitzthum K, Groneberg DA, Mache S (2016) Physicians’ occupational stress, depressive symptoms and work ability in relation to their working environment: a cross-sectional study of differences among medical residents with various specialties working in German hospitals. BMJ Open 15:6
Bourbonnais R, Brisson C, Vinet A, Vezina M, Abdous B, Gaudet M (2006a) Effectiveness of a participative intervention on psychosocial work factors to prevent mental health problems in a hospital setting. Occup Environ Med 63:335–342
Bourbonnais R, Brisson C, Vinet A, Vézina M, Lower A (2006b) Development and implementation of a participative intervention to improve the psychosocial work environment and mental health in an acute care hospital. Occup Environ Med 63:326–334
Brooks SK, Chalder T, Gerada C (2011) Doctors vulnerable to psychological distress and addictions: treatment from the Practitioner Health Programme. J Ment Health 20:157–164
Buchberger B, Heymann R, Huppertz H, Friepörtner K, Pomorin N, Wasem J (2011) The effectiveness of interventions in workplace health promotion as to maintain the working capacity of health care personal. GMS Health Technol Assess 1
Burton NW, Pakenham KI, Brown WJ (2008) Feasibility and effectiveness of psychosocial resilience training: a pilot study of the READY program. Psychol Health Med 15:266–277
Carver CS, Scheier MF, Weintraub JK (1989) Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol 56:267–283
Czabała C, Charzyńska K, Mroziak B (2011) Psychosocial interventions in workplace mental health promotion: an overview. Health Promot Int 26(Suppl 1):i70–i84. doi:10.1093/heapro/dar1050
Goldhagen BE, Kingsolver K, Stinnett SS, Rosdahl JA (2015) Stress and burnout in residents: impact of mindfulness-based resilience training. Adv Med Educ Pract 25:525–532
Holton MK, Barry AE, Chaney JD (2015) Employee stress management: an examination of adaptive and maladaptive coping strategies on employee health. Work
Irving JA, Dobkin PL, Park J (2009) Cultivating mindfulness in health care professionals: a review of empirical studies of mindfulness-based stress reduction (MBSR. Complement Ther Clin Pract 15:61–66
Kirkpatrick DL, Kirkpatrick DJ (2006) Evaluating training programs: the four levels. Berrett-Koehler Publishers
Krasner MS, Epstein RM, Beckman H (2009) Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physician. JAMA 302:1284–1293
Kristensen T, Hannerz H, Høgh A, Borg V (2005) The Copenhagen Psychosocial Questionnaire (COPSOQ)—a tool for the assessment and improvement of the psychosocial work environment. Scand J Work Environ Health 31:438–449
Lagerveld SE, Blonk RW, Brenninkmeijer V, Wijngaards-de Meij L, Schaufeli WB (2012) Work-focused treatment of common mental disorders and return to work: a comparative outcome study. J Occup Health Psychol 17:220–234
Leppin AL, Gionfriddo MR, Sood A, Montori VM, Erwin PJ, Zeballos-Palacios C, Bora PR, Dulohery MM, Brito JP, Boehmer KR, Tilburt JC (2014) The efficacy of resilience training programs: a systematic review protocol. Syst Rev. doi:10.1186/2046-4053-3-20
Levenstein S, Prantera C, Varvo V, Scribano ML, Berto E, Luzi C (1993) Development of the Perceived Stress Questionnaire: a new tool for psychosomatic research. J Psychsom Res 37:19–32
Li J, Weigl M, Glaser J, Petru R, Siegrist J, Angerer P (2013) Changes in psychosocial work environment and depressive symptoms: a prospective study in junior physicians. Am J Ind Med 56:1414–1422
Mache S, Vitzthum K, Nienhaus A, Klapp BF, Groneberg DA (2009) Physicians’ working conditions and job satisfaction: does hospital ownership in Germany make a difference? BMC Health Serv Res 9:148
McCue JD, Sachs CL (1991) A stress management workshop improves residents’ coping skills. Arch Intern Med 151:2273–2277
Nuebling M, Hasselhorn HM (2010a) The Copenhagen Psychosocial Questionnaire in Germany: from the validation of the instrument to the formation of a job-specific database of psychosocial factors at work. Scand J Public Health 38:120–124
Puskar KR, Sereika S, Tusaie-Mumford K (2003) Effect of the Teaching Kids to Cope (TKC) program on outcomes of depression and coping among rural adolescents. J Child Adolesc Psychiatr Nurs 16:71–80
Rabe M, Giacomuzzi S, Nübling M (2012) Psychosocial workload and stress in the workers’ representative. BMC Public Health 12:909
Ramirez AJ, Graham J, Richards MA, Cull A, Gregory WM (1996) Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet 347:724–728
Sautier LP, Scherwath A, Weis J, Sarkar S, Bosbach M, Schendel M, Ladehoff N, Koch U, Mehnert A (2015) Assessment of work engagement in patients with hematological malignancies: psychometric properties of the German version of the Utrecht Work Engagement Scale 9 (UWES-9). Rehabilitation 54:297–303
Schaufeli WB, Bakker AB (2003) Utrecht Work Engagement Scale: preliminary manual. Occupational Health Psychology Unit, Utrecht University, Utrecht Netherlands. pp 1-58
Sen S, Kranzler HR, Krystal JH, Speller H, Chan G, Gelernter J, Guille C (2010) A prospective cohort study investigating factors associated with depression during medical internship. Arch Gen Psychiatry 67:557–565
Sepällä P, Mauno S, Feldt T (2009) The construct validity of the Utrecht Work Engagement Scale: multisample and longitudinal evidence. J Happiness Stud 10:459–481
Shapiro SL, Astin JA, Bishop SR (2005) Mindfulness-based stress reduction for health care professionals: results from a randomized trial. Int J Stress Manag 12:164–176
Sood A, Prasad K, Schroeder D, Varkey P (2011) Stress management and resilience training among Department of Medicine faculty: a pilot randomized clinical trial. J Gen Intern Med 26:858–861
Strijk JE, Proper KI, van Mechelen W, van der Beek AJ (2013) Effectiveness of a worksite lifestyle intervention on vitality, work engagement, productivity, and sick leave: results of a randomized controlled trial. Scand J Work Environ Health 39:66–75
Tan L, Wang MJ, Modini M, Joyce S, Mykletun A, Christensen H, Harvey SB (2014) Preventing the development of depression at work: a systematic review and meta-analysis of universal interventions in the workplace. BMC Med 12:74
van Berkel J, Boot CR, Proper KI, Bongers PM, van der Beek AJ (2014) Effectiveness of a worksite mindfulness-related multi-component health promotion intervention on work engagement and mental health: results of a randomized controlled trial. PLoS One 28:1
Weigl M, Müller A, Angerer P, Hoffmann F (2014) Workflow interruptions and mental workload in hospital pediatricians: an observational study. BMC Health Serv Res 24:433
Weigl M, Schneider A, Hoffmann F, Angerer P (2015) Work stress, burnout, and perceived quality of care: a cross-sectional study among hospital pediatricians. Eur J Pediatr 174:1237–1246
West CP, Dyrbye LN, Rabatin JT, Call TG, Davidson JH, Multari A, Romanski SA, Hellyer JMH, Sloan JA, Shanafelt TF (2014) Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med 174:527–533
Zimber A, Gregersen S, Kuhnert S, Nienhaus A (2010) Workplace health promotion through human resources development part I: development and evaluation of qualification programme for prevention of psychic stresses. Gesundheitswesen 72:209–215
Acknowledgments
We thank Dr. Karin Vitzthum for language editing and proof-reading.
Authors’ contribution
SM, MB, and LB designed the study. MB, LB, and SM performed the investigation. SM and MB analyzed the data. SM and MB wrote the manuscript. SM, MB, LB, and DG interpreted the data and contributed substantially to its revision. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical considerations
Ethical approval was granted by the Free University Berlin. The study is in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1964.
Informed consent
Informed consent was obtained from all individuals participants included in this study.
Funding
No funding support.
Additional information
Communicated by Jaan Toelen
Rights and permissions
About this article
Cite this article
Bernburg, M., Baresi, L., Groneberg, D. et al. Does psychosocial competency training for junior physicians working in pediatric medicine improve individual skills and perceived job stress. Eur J Pediatr 175, 1905–1912 (2016). https://doi.org/10.1007/s00431-016-2777-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-016-2777-8