Abstract
Congenital anomalies of the kidney and urinary tract are common findings on fetal ultrasound. The aim of this prospective observational study was to describe outcome and risk factors in 115 patients born 1995–2001. All prenatally diagnosed children were stratified into low- and high-risk group and followed postnatally clinically and by imaging at defined endpoints. Risk factors were evaluated using odds ratios. Neonatal diagnosis included pelvi-ureteric junction obstruction (n = 33), vesicoureteral reflux (n = 27), solitary mild pelvic dilatation (postnatal anteroposterior diameter 5–10 mm; n = 25), and further diagnosis as primary obstructive megaureter, unilateral multicystic dysplastic kidney, renal dysplasia and posterior urethral valves. In 38 children with prenatal isolated hydronephrosis, ultrasound normalized at median age of 1.2 years (range 0.1–9). Surgery was performed in 34 children at median age of 0.4 years (0.1–10.8). Persistent renal anomalies without surgery were present in 43 children and followed in 36 for median time of 16 years (12.2–18). Oligohydramnios and postnatal bilateral anomalies were significantly associated with surgery and impaired renal function.
Conclusion: The majority of children had a favourable postnatal outcome, in particular children with prenatally low risk, i.e. isolated uni- or bilateral hydronephrosis. Oligohydramnios and postnatal bilateral anomalies were risk factors for non-favourable outcome.
What is Known: • In congenital anomalies of the kidney and urinary tract significantly poorer outcome is known in patients with bilateral renal hypoplasia or solitary kidney associated with posterior urethral valves. • Other factors as proteinuria and vesicoureteral reflux were associated with a higher risk of progression to chronic renal failure in these patients. |
What is New: • Unlike other studies giving us above-mentioned information, we included all patients with any kind of prenatally diagnosed congenital anomalies of the kidney and urinary tract. Our study shows long-term follow up (median 16 years, range 12.2–18 years), especially in patients not needing surgery, but with persistent anomalies. • During postnatal long-term follow up (median 2.2 years, range 0.1–18 years) one third each showed normalization, need of surgery or persistence of anomalies without need of surgery. Our study revealed a good prognosis in the majority of these children, in particular with prenatally low risk, i.e. isolated uni- or bilateral hydronephrosis, and revealed oligohydramnios and postnatal bilateral anomalies as risk factors for a non-favourable outcome, defined as need of surgery, persistent anomalies with impaired renal function, end stage renal failure or death. |
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Congenital anomalies of the kidney and urinary tract (CAKUT) are the most frequent findings on fetal ultrasound (US) with a prevalence of 0.1–2.3 % [6, 8, 10, 16, 24, 27]. The predictive value of these prenatal findings is often difficult to assess. Parents are concerned about apparently abnormal findings on fetal US and strongly interested in prognosis including need of surgery as many parents are afraid of surgery and associated risks, especially in very young children. Oligohydramnios, renal cysts, bladder outlet obstruction, extra renal malformations, low birth weight and prematurity appear to be negative prognostic factors for postnatal outcome [7, 8]. Which specific prognostic factors promote termination of pregnancy is still a matter of debate [11]. Some studies suggested that the prognostic value of prenatal pelvic dilatation correlated with the postnatal need for active treatment [14, 31]. In CAKUT, significantly poorer outcome was observed in patients with bilateral renal hypoplasia or solitary kidney associated with posterior urethral valves (PUV) [25]. In addition, elevated plasma creatinine at diagnosis, proteinuria and vesicoureteral reflux (VUR) were associated with a risk of progression to chronic renal failure [25].
The primary aim of this study was to describe the course of patients prenatally diagnosed with CAKUT with postnatal follow-up by an interdisciplinary schedule. The secondary aim was to analyse potential risk factors for non-favourable outcome, defined as need of surgery, persistent anomalies with impaired renal function, end-stage renal failure (ESRF) or death.
Patients and methods
Patients
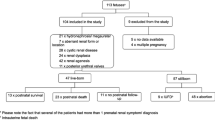
This single centre prospective observational study included a sample of 115 children, prenatally diagnosed with CAKUT between 1995 and 2001, with the aim of enrolling a minimum of 100 patients. Inclusion criteria were both any kind of assumed CAKUT on prenatal US and postnatal follow-up in our hospital based on local guidelines (Fig. 1). Prenatally diagnosed patients were stratified into low- and high-risk group (Fig. 1) and prospectively followed clinically and by imaging from 1995 to 2012. We describe the follow-up prenatally, postnatally and at the most recent clinical assessment.
Five study endpoints were defined: normalization of US findings, surgery (decision taken by an interdisciplinary team of paediatric nephrologists, urologists and radiologists), and persistent anomalies not requiring surgery with or without impaired renal function, ESRF and death.
Written informed consent had been obtained from all parents or guardians.
Prenatal evaluation
Ultrasound was performed by obstetricians of the obstetric unit of the University Hospital Zurich (n = 44), obstetricians of other hospitals in the greater area of Zurich (n = 58) or private obstetricians (n = 13).
The following clinical data were evaluated: diagnosis of CAKUT (some patients had more than one diagnosis), date (weeks of pregnancy) of first diagnosis, prevalence of oligohydramnios (not further defined), extra renal fetal malformations, fetal interventions, duration and complications of pregnancy. Prenatal hydronephrosis was defined as pelvic dilatation with anteroposterior diameter (APD) >7 mm in the third trimester [31].
Postnatal evaluation
Children were divided into two groups according to our local guidelines (Fig. 1): low-risk group patients underwent the first renal US 1 week after birth whereas high-risk group patients had their first imaging within 24–48 h. All children were examined by a paediatrician at least once within the first week after birth.
Ultrasound (US):
Postnatal hydronephrosis was defined as pelvic dilatation measured as APD and graduated in mild (5–9 mm), moderate (≥10–14 mm) or severe (≥15 mm). Size and structure of the kidney, dilatation of calices or ureters, and bladder morphology were also reported.
Voiding cystourethrography (VCUG)
VUR was graded I–V (mild: I–II; severe: III–V) according to the international reflux study [15], except in those children with VUR associated with obstruction of the upper urinary tract, where VUR was not graded.
Functional imaging: Intravenous urography (IVU) was performed until 1999 (n = 27) and was replaced by Mercaptoacetyltriglycine-3 (MAG-3) scintigraphy (n = 38) in 2000. Dimercaptosuccinic acid (DMSA) scintigraphy was performed during the whole study period (n = 19) to detect focal parenchymal defects.
Clinical follow-up and final examination
All patients were followed including measurement of growth [22], blood pressure using age-related charts [1, 7], and US of the kidneys and urinary tract. Renal function was classified according to the KDIGO guidelines stage 1–5 [2] and proteinuria was evaluated in patients with persistent anomalies. Glomerular filtration rate was estimated by the Schwartz formula [26] with a K-factor of 40 based on local comparison with Cr-EDTA clearance measurements [4]. In patients with either normalization of US or surgery, the last examination was defined as the date of normalization and surgery, respectively. Decision for surgical intervention was taken by an interdisciplinary team of paediatric nephrologists, urologists and radiologists. Vesicoureteral reflux in patients on antibiotic prophylaxis was surgically treated if a first break-through urinary tract infection (UTI) occurred. Patients with pelvi-ureteric junction obstruction (PUJO) underwent surgery if ipsilateral renal function on scintigraphy was ≤40 %, function declined during follow-up ≥10 % or the patient suffered complications (e.g. urolithiasis). All patients with PUV underwent surgery in the neonatal period. Nephrectomy or heminephrectomy were performed in case of non-functioning kidneys combined with a risk constellation for UTI (e.g. ipsilateral VUR or ureterocele).
Definitions
Urinary tract infections (UTI):
Pyelonephritis was defined as fever >38.0 °C, elevated C-reactive protein (CRP), leucocyturia and bacteriuria (≥105 CFU/ml; urine collected by catheter). Cystitis was defined as UTI with neither fever nor elevated CRP.
UTI-prophylaxis:
Oral antibiotic prophylaxis during the first 2 months of life consisted of amoxicillin (12.5 mg per kg body weight twice daily) and was given to all children in the high-risk group and to those children in the low-risk group with suspected primary obstructive megaureter (POM), unilateral multicystic dysplastic kidney (MCDK) and/or pelvic dilatation ≥10 mm until VUR was excluded by VCUG. If prophylaxis was continued beyond 2 months of age, medication was changed to cotrimoxazole (9 mg per kg twice daily) and continued up to 2–3 years of age.
Renal function:
Impaired renal function was defined as GFR <90 ml/min per 1.73 m2 (>1 year) according to the KDIGO guidelines stage 2–5. ESRF was defined as patients undergoing renal replacement therapy.
Outcome:
Normalization of US was defined as normal structure and size of both kidneys, absence of pelvic or ureteral dilatation (APD of renal pelvis not detectable or <5 mm) and normal configuration of the bladder. Non-favourable outcome was defined as need of surgery, persistent anomalies with impaired renal function, ESRF or death.
Statistical analysis
Statistical analysis was performed with SPSS for Windows version 18.0 (IBM Corporation, New York, USA). Differences between subgroups were calculated using the Fisher’s exact test for categorical variables. Bivariate correlation analysis was performed by using the Spearman correlation coefficient (r). To asses risk factors, odds ratios and 95 % confidence interval were calculated. Kaplan-Meier curves were used to analyse timing of events of study endpoint. A p value of <0.05 was considered statistically significant.
Results
A total of 115 children with prenatally assumed diagnosis of CAKUT and postnatal follow-up fulfilled the study criteria (Fig. 2). Patients’ characteristics are given in Table 1.
Prenatal evaluation
Prenatal diagnoses are summarized in Table 2. The prenatal extent of pelvic dilatation was not consistently reported and therefore not included in our data. Oligohydramnios had been diagnosed in 10 pregnancies between 26 and 39 weeks of gestation. Of the 11 fetuses (10 males) with megavesica, three boys underwent prenatal bladder puncture, one of them repeatedly. One fetus each underwent puncture of an abdominal cyst and ureterocele.
Extra renal diagnoses and maternal complications are listed in Table 1. The fetus with hygroma was postnatally diagnosed as Noonan syndrome; the two patients with cardiac anomalies had normal postnatal findings.
Postnatal evaluation
Ninety-one patients (22 girls, 69 boys) were in the low-risk group, and 24 (6 girls, 18 boys) fulfilled the criteria for the high-risk group: oligohydramnios (n = 10; 8 males), suspected PUV (n = 7 males), ureterocele (n = 2 males), megavesica and pelvic dilatation (n = 9; 8 males), or extrarenal anomalies (one girl with hygroma colli and one boy with suspected cardiac malformation). Eight neonates in the low risk and three in the high-risk group were born preterm. Five patients with oligohydramnios had pulmonary complications with wet lung in four and amniotic fluid aspiration and pneumothorax in one (Table 1).
Postnatal US showed hydronephrosis in 92 patients, with 47 unilateral and 45 bilateral pelvic dilatations (i.e. 137 dilated kidneys). Pelvic dilatation was mild, moderate and severe in 58, 60 and 19 kidneys, respectively. The diagnoses at postnatal and most recent examination are summarized in Table 2.
Follow-up at study endpoints
Median follow-up time for all patients reaching their endpoint was 2.2 years (range 0.1–18).
Normalization of ultrasound findings (Table 2)
Thirty-eight children (high-risk group: n = 1) had normal US findings during follow-up, ranging form six patients with a normal (first) US in the first week after birth to 9 years of age (Fig. 3a). Isolated hydronephrosis was the most frequent prenatal diagnosis (n = 33) in this group. Rare prenatal findings were megavesica, duplex kidney, ureteric dilatation and renal cysts.
Need of surgery (Table 2)
Thirty-four patients (high-risk group: n = 14) underwent surgery, ranging form 1 month to 10.8 years of age. Thirteen patients underwent their operation within the first 3 months (Fig. 3b). Impaired renal function was noted in 19 patients (KDIGO: stage 2: n = 7; stage 3: n = 9; stage 4: n = 1; stage 5: n = 2). Unilateral or bilateral hydronephrosis was the most common prenatal diagnosis (n = 28) in the surgery group, followed by ureteric dilatation and megavesica. Surgery included pyeloplasty (n = 10), ureterocystoneostomy (n = 8), transurethral resection of PUV (n = 7), transurethral resection of ureterocele (n = 2), nephrectomy (n = 2), heminephrectomy (n = 2), resection of ureteral stenosis (n = 1), Monti-stoma (n = 1) and dilatation of vaginal introitus (n = 1). The majority of patients with oligohydramnios (n = 7 out of 10) underwent surgery. Eleven patients had break-through UTI on prophylaxis leading to re-implantation of the ureter (n = 8), heminephrectomy (n = 2) or nephrectomy (n = 1). One patient with PUV died in the neonatal period due to severe extrarenal anomalies. Two operated patients with bilateral renal disease (one patient with bilateral renal dysplasia, one with PUV) developed ESRF (age 2.0 and 14.3 years) requiring dialysis with subsequent renal transplantation.
Persistent anomalies without surgery (Table 2)
Forty-three patients showed persistent renal anomalies on US without need of surgery during the observation period. In 30 patients, renal function remained normal. Thirteen patients, however, had impaired GFR. Stage 2 chronic kidney disease (GFR 62–85 ml/min per 1.73 m2) was present in 12 patients, including five with unilateral MCDK (two of them with contralateral VUR), two with autosomal dominant polycystic kidney disease (ADPKD), and one each with unilateral PUJO, bilateral PUJO, unilateral PUJO with bilateral VUR, unilateral POM with bilateral VUR, and mutation in the HNF1-beta gene; none had hypertension or proteinuria. One boy with ADPKD and stage 3 chronic kidney disease (GFR 58 ml/min per 1.73 m2) was on ACE-inhibitors for hypertension and proteinuria. No patient so far developed ESRF.
Outcome risk factors and high risk versus low risk group (Tables 3 and 4)
In total, 68 (58 %) patients had a favourable outcome with either normalization of the US findings or persistent renal anomalies with normal renal function.
Significantly more children in the low-risk group as compared with the high-risk group had normalized US findings (p = 0.016). In contrast, non-favourable outcome was more common in the high-risk group as compared to the low-risk group, and significantly associated with oligohydramnios and postnatal bilateral anomalies (p < 0.05). Significantly more high-risk patients required surgery (p = 0.005); impaired renal function was also more frequent, but without statistical significance. Forty-five episodes of UTI occurred in 26 children, both in the low-risk group (n = 19; 21 %) and the high-risk group (n = 7; 29 %).
Discussion
Congenital anomalies of the kidney and urinary tract (CAKUT) are the most common prenatal diagnoses with a prevalence of 1 in 70–1000 live births [5, 18, 29] accounting for 30–50% of all fetal anomalies [10, 12]. CAKUT is the most common cause for chronic kidney disease in childhood [9]. There is a broad range of fetal anomalies, ranging from mild unilateral pelvic dilatation to severe malformations of both kidneys and the urinary tract, the latter being the leading cause of paediatric end-stage renal disease [28]. Recommendations for infants with prenatally diagnosed hydronephrosis remain controversial, especially regarding diagnostic criteria, fetal interventions, risk classification and postnatal diagnostic and therapeutic management [33].
Our study deliberately encompassed a non-selected group of children with assumed prenatal renal anomalies. In addition, the follow-up time showed a broad range from 1 month to 18 years, based on the various defined endpoints. Our study showed that the majority of the patients had a favourable outcome.
One third of the children had an excellent prognosis with normalization of the US findings. Their prenatal US had mostly displayed isolated uni- or bilateral pelvic dilatation. The postnatal US most often showed unilateral or bilateral mild hydronephrosis; PUJO, POM and VUR were also reported. The time to normalization ranged from the first week of life up to 9 years. A study by John et al. reported a normalization rate of 25 % at the age of 3 months, including children with fetal hydronephrosis defined as APD ≥4 mm until 33 weeks of gestation and APD ≥7 mm thereafter [14]. It might be assumed that mild prenatal and postnatal hydronephrosis is a normal variant without clinical relevance. However, (long-term) postnatal follow-up until normalization of the US is mandatory as unequivocal prenatal identification of the child with good postnatal prognosis is not possible. In 2010, the Society for Fetal Urology (SFU) defined hydronephrosis as mild (APD 7 to <9 mm), moderate (APD 9 to <15 mm) and severe (APD >15 mm) in the third trimester, similar to our study criteria. A German study suggested a pelvic dilatation in the third trimester of ≥7 mm as clinically significant, whereas a comparable Swiss study reported ≥10 mm [14, 19, 31].
Also, approximately one third of the patients underwent surgery, with the majority in early life. The most frequent procedures in the first months of life were resection of PUV and pyeloplasty in patients with PUJO. Increased risk for surgery was present in the high-risk group patients, in particular in patients with oligohydramnios. Some patients underwent surgery up to the age of 10 years including patients with persistent VUR and break-through UTI undergoing anti-reflux surgery. A substantial number of the surgical patients had impaired renal function requiring a combined urological-nephrological long-term follow-up. In an Italian study, 53 % of patients needed surgery; however, only those with solitary kidney and VUR were considered, and patients with isolated ureteral anomalies were excluded [25]. In a study of Quirino et al., surgery was needed in 28 % and PUJO was the most prevalent diagnosis leading to surgery [23].
Another third of our patients had persistent anomalies without requiring surgery. The majority of these patients had normal renal function, with the most recent evaluation taking place in adolescence. Their anomalies were generally unilateral and included mild or moderate hydronephrosis, megaureter, MCDK with normal contralateral kidney or VUR. A minority of this group had a non-favourable outcome, i.e. impaired renal function. Risk factors were the prevalence of oligohydramnios and/or postnatal bilateral anomaly. Preterm birth was not revealed as significant risk factor, as reported in other studies [17, 21], but incidence of preterm birth was low in our population.
Except two surgical patients, no other patient developed ESRF during the observation period. This favourable outcome might result from prenatal selection as no information was available on antenatally diagnosed CAKUT leading to termination of pregnancy. However, all patients with non-favourable outcome, and also some patients with persistent renal anomalies (and still normal renal function) or successful surgery, are at risk of progressive renal failure in the long-term, requiring life-long medical follow-up. Wuhl et al. recently reported a high risk of ESRF among adult patients with congenital moderate and severe renal hypoplasia or dysplasia [32].
Based on different patient collective, other authors found a lower incidence [13] or a different distribution [25] of described nephro-uropathies indicating the difficulty in comparing our diagnosis and outcome with others studies, as we included any kind of prenatal anomalies of the kidney and the urogenital tract. However, our data confirmed already known risk factors (e.g. oligohydramnios and bilateral anomalies) [3, 8, 17, 20, 30]. In addition, the results emphasized the clinical usefulness of the impact of our algorithm and stratification into low- and high-risk group.
Especially in pregnancies with identified risk factors, proactive involvement of paediatric nephrologists in prenatal counselling is valuable to discuss the range of diagnoses and the postnatal course. Prenatal counselling also includes discussion of the potential need of postnatal treatment, ranging from postnatal diagnostic imaging to antibiotic administration and (early) surgery. Parents are particularly afraid of surgery and associated risks in very young children.
Limitations
The difficulty of obtaining precise information from obstetricians is an important limitation of our study, but underlines the importance of close collaboration, communication and data exchange between obstetrician, neonatologist, paediatric urologist and nephrologist. The deliberate inclusion of a non-selected “real world” population resulted in a heterogeneous study population with a broad spectrum of findings making any statistical analysis problematic. However, our intention was to focus on all anomalies during pregnancy aiming to describe the follow-up of any kind of CAKUT. This intention was based on the idea to counsel parents during pregnancy with any kind of urological anomalies on fetal US. Pre- and postnatal genetic testing for patients with CAKUT, nowadays standard in many centres, was not regularly available at the beginning of our study. Although diagnostic options have changed during the last 2 decades, indications for surgery did not change in our institution, i.e. surgical treatment for patients with VUR and break-through UTI, and for significant obstruction in case of PUJO or POM. However, antibiotic prophylaxis in patients with VUR is currently limited to high-grade reflux only.
In summary, the majority of children with prenatally assumed CAKUT had a favourable outcome, in particular children with prenatal isolated uni- or bilateral hydronephrosis. Oligohydramnios and postnatal bilateral anomalies were risk factors for non-favourable outcome, i.e. need of surgery and/or persistent renal anomalies with impaired renal function. These findings may be helpful for all involved medical professionals when counselling pregnant women and parents. Close multidisciplinary collaboration between obstetricians, neonatologists, paediatricians and paediatric urologists and nephrologists, and long-term postnatal follow-up is mandatory.
Abbreviations
- ADPKD:
-
Autosomal dominant polycystic kidney disease
- APD:
-
Anteroposterior diameter
- CAKUT:
-
Congenital anomalies of the kidney and urinary tract
- CRP:
-
C-reactive protein
- DMSA:
-
Dimercaptosuccinic acid scintigraphy
- ESRF:
-
End-stage renal failure
- GFR:
-
Glomerular filtration rate
- IVU:
-
Intravenous urography
- MAG-3:
-
Mercaptoacetyltriglycine-3 scintigraphy
- MCDK:
-
Multicystic dysplastic kidney
- POM:
-
Primary obstructive megaureter
- PUV:
-
Posterior urethral valves
- PUJO:
-
Pelvi-ureteric junction obstruction
- US:
-
Ultrasound
- UTI:
-
Urinary tract infections
- VCUG:
-
Voiding cystourethrography
- VUR:
-
Vesicoureteral reflux
References
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114:555-576
Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group (2009) KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int Suppl:S1-130
Asl AS, Maleknejad S (2012) Clinical outcome and follow-up of prenatal hydronephrosis. Saudi J Kidney Dis Transpl 23:526–531
Chantler C, Barratt TM (1972) Estimation of glomerular filtration rate from plasma clearance of 51-chromium edetic acid. Arch Dis Child 47:613–617
Colodny AH (1987) Antenatal diagnosis and management of urinary abnormalities. Pediatr Clin North Am 34:1365–1381
Dudley JA, Haworth JM, McGraw ME, Frank JD, Tizard EJ (1997) Clinical relevance and implications of antenatal hydronephrosis. Arch Dis Child Fetal Neonatal Ed 76:F31–F34
Flynn JT (2000) Neonatal hypertension: diagnosis and management. Pediatr Nephrol 14:332–341
Gunn TR, Mora JD, Pease P (1995) Antenatal diagnosis of urinary tract abnormalities by ultrasonography after 28 weeks’ gestation: incidence and outcome. Am J Obstet Gynecol 172:479–486
Harambat J, van Stralen KJ, Kim JJ, Tizard EJ (2012) Epidemiology of chronic kidney disease in children. Pediatr Nephrol 27:363–373
Helin I, Persson PH (1986) Prenatal diagnosis of urinary tract abnormalities by ultrasound. Pediatrics 78:879–883
Hogan J, Dourthe ME, Blondiaux E, Jouannic JM, Garel C, Ulinski T (2012) Renal outcome in children with antenatal diagnosis of severe CAKUT. Pediatr Nephrol 27:497–502
Hutson JM, McNay MB, MacKenzie JR, Whittle MJ, Young DG, Raine PA (1985) Antenatal diagnosis of surgical disorders by ultrasonography. Lancet 1:621–623
Ismaili K, Avni FE, Wissing KM, Hall M (2004) Long-term clinical outcome of infants with mild and moderate fetal pyelectasis: validation of neonatal ultrasound as a screening tool to detect significant nephrouropathies. J Pediatr 144:759–765
John U, Kahler C, Schulz S, Mentzel HJ, Vogt S, Misselwitz J (2004) The impact of fetal renal pelvic diameter on postnatal outcome. Prenat Diagn 24:591–595
Lebowitz RL, Olbing H, Parkkulainen KV, Smellie JM, Tamminen-Mobius TE (1985) International system of radiographic grading of vesicoureteric reflux. International Reflux Study in Children. Pediatr Radiol 15:105–109
Livera LN, Brookfield DS, Egginton JA, Hawnaur JM (1989) Antenatal ultrasonography to detect fetal renal abnormalities: a prospective screening programme. BMJ 298:1421–1423
Melo BF, Aguiar MB, Bouzada MC, Aguiar RL, Pereira AK, Paixao GM, Linhares MC, Valerio FC, Simoes ESAC, Oliveira EA (2012) Early risk factors for neonatal mortality in CAKUT: analysis of 524 affected newborns. Pediatr Nephrol 27:965–972
Nakanishi K, Yoshikawa N (2003) Genetic disorders of human congenital anomalies of the kidney and urinary tract (CAKUT). Pediatr Int 45:610–616
Nguyen HT, Herndon CD, Cooper C, Gatti J, Kirsch A, Kokorowski P, Lee R, Perez-Brayfield M, Metcalfe P, Yerkes E, Cendron M, Campbell JB (2010) The Society for Fetal Urology consensus statement on the evaluation and management of antenatal hydronephrosis. J Pediatr Urol 6:212–231
Oliveira EA, Cabral AC, Pereira AK, Machado IN, Diniz JS, Lana AM, Cunha LK (2001) Outcome of fetal urinary tract anomalies associated with multiple malformations and chromosomal abnormalities. Prenat Diagn 21:129–134
Oliveira EA, Diniz JS, Cabral AC, Leite HV, Colosimo EA, Oliveira RB, Vilasboas AS (1999) Prognostic factors in fetal hydronephrosis: a multivariate analysis. Pediatr Nephrol 13:859–864
Prader A, Largo RH, Molinari L, Issler C (1989) Physical growth of Swiss children from birth to 20 years of age. First Zurich longitudinal study of growth and development. Helv Paediatr Acta Suppl 52:1–125
Quirino IG, Diniz JS, Bouzada MC, Pereira AK, Lopes TJ, Paixao GM, Barros NN, Figueiredo LC, Cabral AC, Simoes e Silva AC, Oliveira EA (2012) Clinical course of 822 children with prenatally detected nephrouropathies. Clin J Am Soc Nephrol 7:444–451
Sairam S, Al-Habib A, Sasson S, Thilaganathan B (2001) Natural history of fetal hydronephrosis diagnosed on mid-trimester ultrasound. Ultrasound Obstet Gynecol 17:191–196
Sanna-Cherchi S, Ravani P, Corbani V, Parodi S, Haupt R, Piaggio G, Innocenti ML, Somenzi D, Trivelli A, Caridi G, Izzi C, Scolari F, Mattioli G, Allegri L, Ghiggeri GM (2009) Renal outcome in patients with congenital anomalies of the kidney and urinary tract. Kidney Int 76:528–533
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Scott JE, Renwick M (1993) Urological anomalies in the Northern Region Fetal Abnormality Survey. Arch Dis Child 68:22–26
Soares CM, Diniz JS, Lima EM, Silva JM, Oliveira GR, Canhestro MR, Colosimo EA, Simoes e Silva AC, Oliveira EA (2008) Clinical outcome of children with chronic kidney disease in a pre-dialysis interdisciplinary program. Pediatr Nephrol 23:2039–2046
Song R, Yosypiv IV (2011) Genetics of congenital anomalies of the kidney and urinary tract. Pediatr Nephrol 26:353–364
Tam JC, Hodson EM, Choong KK, Cass DT, Cohen RC, Gruenewald SM, Hayden LJ (1994) Postnatal diagnosis and outcome of urinary tract abnormalities detected by antenatal ultrasound. Med J Aust 160:633–637
Wollenberg A, Neuhaus TJ, Willi UV, Wisser J (2005) Outcome of fetal renal pelvic dilatation diagnosed during the third trimester. Ultrasound Obstet Gynecol 25:483–488
Wuhl E, van Stralen KJ, Verrina E, Bjerre A, Wanner C, Heaf JG, Zurriaga O, Hoitsma A, Niaudet P, Palsson R, Ravani P, Jager KJ, Schaefer F (2013) Timing and outcome of renal replacement therapy in patients with congenital malformations of the kidney and urinary tract. Clin J Am Soc Nephrol 8:67–74
Yamacake KG, Nguyen HT (2013) Current management of antenatal hydronephrosis. Pediatr Nephrol 28:237–243
Authors’contributions
Samuel Nef: paediatric nephrologist, main autor Thomas Neuhaus, Prof., M.D.: paediatic nephrologist, nephrological counselling, writting, revision Giuseppina Spartà, M.D.: paediatric nephrologist, nephrological counselling Marcus Weitz, M.D.: paediatric nephrologist, nephrological counselling Kathrin Buder, M.D.: statistics Josef Wisser, Prof., M.D.: obbstetrician, prenatal counselling Rita Gobet, Prof., M.D.: paediatric urologist, urological counselling, revision Ulrich Willi, Prof., M.D.: paediatric radiologist, radiological counselling Guido F. Laube, PD, M.D.: paediatric nephrologist, nephrological counselling, writting, revision, man in charge.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare that they have no competing interests.
Informed consent
Written informed consent was obtained from all parents or guardians of each child included in the study.
Additional information
Communicated by Jaan Toelen
Rights and permissions
About this article
Cite this article
Nef, S., Neuhaus, T.J., Spartà, G. et al. Outcome after prenatal diagnosis of congenital anomalies of the kidney and urinary tract. Eur J Pediatr 175, 667–676 (2016). https://doi.org/10.1007/s00431-015-2687-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-015-2687-1