Abstract
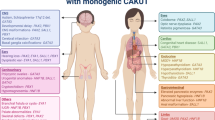
Congenital anomalies of the kidney and urinary tract (CAKUT) occur in 1 in 500 births and are a major cause of morbidity in children. Notably, CAKUT account for the most cases of pediatric end-stage renal disease and predispose the individual to hypertension and cardiovascular disease throughout life. Although some forms of CAKUT are a part of a syndrome or are associated with a positive family history, most cases of renal system anomalies are sporadic and isolated to the urinary tract. Broad phenotypic spectrum of CAKUT and variability in genotype–phenotype correlation indicate that pathogenesis of CAKUT is a complex process that depends on interplay of many factors. This review focuses on the genetic mechanisms (single-gene mutations, modifier genes) leading to renal system anomalies in humans and discusses emerging insights into the role of epigenetics, in utero environmental factors, and micro-RNAs (miRNAs) in the pathogenesis of CAKUT. Common gene networks that function in defined temporospatial fashion to orchestrate renal system morphogenesis are highlighted. Derangements in cellular, molecular, and morphogenetic mechanisms that direct normal renal system development are emphasized as a major cause of CAKUT. Integrated understanding of how morphogenetic process disruptions are linked to CAKUT will enable improved diagnosis, treatment, and prevention of congenital renal system anomalies and their consequences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congenital anomalies of the kidney and urinary tract (CAKUT) occur at a frequency of 1 in 500 live births [1, 2]. CAKUT comprise a spectrum of renal tract malformations that occur at the level of the kidney (e.g. hypoplasia, dysplasia), collecting system (e.g. hydronephrosis, megaureter), bladder (e.g. ureterocele, vesicoureteral reflux), or urethra (e.g. posterior urethral valves) (Table 1). Although some forms of CAKUT are a part of a syndrome or are associated with a positive family history, most cases of renal system anomalies are sporadic and isolated to the urinary tract. Notably, CAKUT are the most common cause of renal failure in childhood, accounting for 31% of children with end-stage renal disease (ESRD) in the United States [3]. All children with ESRD require renal replacement therapy, and up to 70% of them develop hypertension [4]. These observations emphasize the need for development of new strategies aimed at decreasing the incidence of CAKUT, preserving renal function, and preventing morbidity from cardiovascular disease. Despite the diverse anatomical and histological spectrum of kidney and urinary tract malformations, all forms of CAKUT stem from faulty renal system development. To understand the basis of human CAKUT, it is essential to consider how the kidney and urinary tract develop.
Morphologic development of the kidney and urinary tract
Development of the human kidney begins when the nephric duct (ND) is formed from the intermediate mesoderm on embryonic (E) day 22 [5]. The ND extends caudally and induces the adjacent mesoderm to form two transient kidney types, pronephros and mesonephros. Mesonephros gives rise to male reproductive organs and involutes. On E28, ND forms an epithelial outgrowth called the ureteric bud (UB), which invades the adjacent metanephric mesenchyme (MM) to induce permanent metanephric kidney (Fig. 1). Formation of the metanephros occurs via reciprocal inductive interactions between the UB and the mesenchyme [6]. Multiple gene networks have been shown to induce metanephric organogenesis [7–9]. Distal UB will undergo branching morphogenesis to form the renal collecting system (collecting ducts, renal calyces, pelvis, and ureter), whereas MM will give rise to all epithelial cells that form nephrons (from the glomerulus through the distal tubule) [10, 11]. UB branching is completed by 22 weeks of gestation, whereas nephrogenesis continues until 34–36 weeks of fetal life. In the absence of UB branching after 22 weeks of gestation, nephrogenesis continues through the poorly understood process of arcade formation [12]. Initial generations of UB branches are remodeled into the ureter, pelvis, and calyces, whereas subsequent generations give rise to collecting ducts. Linear arrays of inner (medullary) collecting ducts will converge centrally to form the papilla. Following acquisition of the full complement of nephrons, subsequent glomerular development occurs via hypertrophy [13]. The bladder and urethra originate from the urogenital sinus. In turn, urogenital sinus is formed from the cloaca. Proximal UB will form the ureter, which will dissociate from the ND to fuse with the bladder epithelium in the trigone, the muscular region located at the base of the bladder [14].
Normal development of the kidney and urinary tract. a Invasion of the metanephric mesenchyme (MM) by the ureteric bud (UB) on weeks 5–6 of gestation induces MM cells to aggregate around the UB tip. a–c UB outgrowth from the nephric duct (ND), its subsequent iterative branching (branching morphogenesis), and continuous condensation of the MM cells around emerging UB tips are induced primarily by reciprocal interactions among glial-derived neurotrophic factor (GDNF), its receptor c-Ret, and its coreceptor GFRα1. b MM cell aggregates undergo mesenchymal-to-epithelial transformation (MET) to form the renal vesicle (RV) on weeks 6–36 of gestation. c RV elongates along the proximal–distal axis to form comma-shaped and then S-shaped nephrons. Distal ends of S-shaped nephrons fuse with UB-derived collecting ducts, whereas proximal clefts form glomeruli. Endothelial cells migrate into the proximal cleft. UB branching occurs on weeks 6–22 of gestation. Formation of nascent nephrons and their patterning occur on weeks 6–36 of gestation. d Patterning of the S-shaped nephron and UB results in formation of mature nephrons that contain glomerular capillary tuft, podocytes, proximal tubule, loop of Henle, distal tubule, and collecting duct. e Ureter becomes patent, and common ND (CND) fuses with cloaca on weeks 4–5 of gestation. f Apoptosis of the CND accounts for the positioning of the ureter (derived from proximal UB) in proximity of the urogenital sinus on weeks 5–6 of gestation. g Ureter fuses with the bladder by 6 weeks of gestation. Please see text for details
Molecular biology of mammalian kidney and urinary tract development
Genetic manipulations in mice provided critical information on the cellular and molecular mechanisms that orchestrate kidney and urinary tract morphogenesis, yielding new insights into the pathogenesis of CAKUT [6–8, 14]. Organogenesis of the metanephric kidney and lower urinary tract is coordinated by complex interactions among numerous transcription/growth factors and intracellular signaling molecules that may be collectively referred to as renal developmental genes (RDGs) [6–8, 14]. RDGs are expressed in the MM, stroma, angioblasts, UB, and cloaca [6–9, 14]. Here, we review the most significant gene networks that function at multiple stages of renal system development.
UB induction from the ND is mediated by glial-derived neurotrophic factor (GDNF) secreted by MM, which interacts with the c-Ret receptor tyrosine kinase (RTK) expressed in the UB to induce branching [15, 16] (Fig. 1). GDNF levels and its spatial expression are regulated by multiple transcription and growth factors, such as paired box 2 (Pax2), eyes absent homolog 1 (Eya1), SIX homeobox (Six)1, 2, and 4, forkhead/winged-helix transcription factor d1 (FoxC1), roundabout, axon guidance receptor, homolog 2 (Robo2), slit homolog 2 (Slit2), wingless-type MMTV integration site family, member 11, (Wnt11) [6, 7]. c-Ret expression and signaling activity is inhibited by sprouty homolog 1 (Spry1) and induced by Pax2 or retinoic acid [17–19]. Interestingly, other growth factors, such as fibroblast growth factor (FGF) 10, can induce UB branching in the absence of GDNF or c-Ret RTK [20]. Stromal cells stimulate UB branching and nephrogenesis via (Foxd1), retinoic acid, FGF7, bone morphogenetic protein 4 (BMP4), and podocyte 1 (Pod1) [21–23]. UB signals to MM by secreting Wnt9b, a soluble growth factor, that acts via canonical β-catenin to induce expression of FGF8, LIM homeobox 1 (Lhx1), and Wnt4 in the MM [24–26]. In turn, Wnt4 induces MM cells to undergo mesenchymal-to-epithelial transformation (MET) and differentiate into nephron epithelia [24]. Wnt9b-induced MET is regulated by hepatocyte nuclear factor 1β (HNF1β) [27]. In addition to its role in MET, Wnt9b is also required for later nephron patterning [28]. Six2, a homeodomain transcription factor expressed in the MM, maintains MM cells in an undifferentiated state, thereby allowing continued UB branching and nephron formation to proceed [29]. Iterative UB branching and nephron induction are accompanied by their continuous patterning (gradual acquisition of structure characteristic of the mature organ). Examples of patterning include nephron segmentation and UB remodeling into the renal collecting system. With respect to nephrogenesis, pretubular-mesenchymal-cell aggregates are induced at the tips of the UBs and then undergo MET to form the renal vesicle (RV) (Fig. 1). The RV elongates along the proximal–distal axis to form comma-shaped and then mature nephron, which comprises the following distinct regions: glomerulus, proximal tubule, loop of Henle, and distal tubule. Transition form the RV to comma-shaped nephron is induced by transcription factors Lhx1 and POU class 3 homeobox 3 (Brn1) [29]. In turn, comma-shaped nephron elongates to form an S-shaped body. Distal parts of the S-shaped body differentiate into distal tubule segments under control of Brn1 and Iroquois-class homeodomain (Irx) transcription factors Irx1–3 [30], whereas proximal tubule formation is controlled by Notch2 [31]. Notch2 controls proximal nephron development by stabilizing, rather than specifying, its fate via depletion of Six-2-positive progenitor cells [32]. Podocyte differentiation is regulated by transcription factors Wilms tumor 1 (WT1), Pax2, LIM homeobox transcription factor 1β (Lmx1β), and semaphorin3a (Sema3a) [33–35]. Podocytes induce migration of vascular endothelial cells into the vascular cleft by releasing vascular endothelial growth factor (VEGF) [36]. In turn, endothelial cells promote differentiation of mesangial cells via production of platelet-derived growth factor (PDGF) [37]. Dissociation of the ureter from the ND and its fusion with the bladder is regulated by retinoic acid-, c-Ret-, and leukocyte antigen-related (LAR)-family protein tyrosine phosphatase-dependent apoptosis of the common ND [38–40]. Despite new insights into the molecular basis of kidney and urinary tract development, integrated understanding of this process is far from complete. Continued use of model organisms complemented by new technologies will enable identification of novel genes and factors that act in concert to form a kidney.
Developmental origin of CAKUT
Animal model systems have provided evidence for an association between interruption of specific molecular pathways and CAKUT phenotype. For example, absence of UB outgrowth from the ND observed in the presence of GDNF or Ret mutations will lead to renal agenesis [6] (Table 1, Fig. 2). Notably, unilateral renal agenesis occurs in 0.008% of fetuses and in 1 in 5,000 newborns and bilateral in 0.013% fetuses and in 1 in 30,000 newborns [41, 42]. Ectopic UB outgrowth from the ND may lead to obstruction, vesicoureteral reflux (VUR), hydronephrosis, duplex ureters, renal collecting systems, or kidneys [43, 44]. Congenital hydronephrosis has an overall prevalence of 1 in 1,000 live births [45]. Molecular mechanisms leading to hydronephrosis/hydroureter in the absence of anatomic obstruction include T-box transcription factor 18 (Tbx18) or Six-1-dependent delay in differentiation of ureteral smooth muscle cells [46, 47].
Normal and abnormal development of the kidney and urinary tract. Reciprocal inductive interactions between the ureteric bud (UB) and metanephric mesenchyme (MM) are essential for normal metanephric kidney development. a Absence of UB outgrowth from the nephric duct (ND) on weeks 5–6 of gestation results in renal agenesis. b Aberrant interactions between the UB and MM on weeks 5–36 of gestation lead to renal hypodysplasia (small kidney containing normally formed nephrons, immature undifferentiated nephrons or cysts). c, d Normal interactions of the UB with the MM and cloaca on weeks 5–36 of gestation result in formation of normally structured urinary system. Urogenital sinus separates from the rectum on the 4th week of gestation. e Cloaca and urogenital sinus give rise to bladder and urethra on weeks 4–5 of gestation. f A UB that originates at proper site of outgrowth from the ND will join the bladder trigone normally (left). A UB that outgrows too low from the ND joins the trigone lateral and anterior (higher), causing vesicoureteral reflux (VUR) (right). Trigone is formed on the 5th week of gestation. Retention of the remnants of the urogenital membrane lead to formation of posterior urethral valves (PUV). Embryogenesis of PUV and its timing are unknown. g Failure of ascent of the left kidney leads to pelvic kidney. Kidney ascent occurs on weeks 5–8 of gestation. h Defects in renal capsule cause kidney fusion at lower poles (horseshoe kidney). Due to failed upward migration, horseshoe kidney is located lower than usual. i Abnormal migration of the left kidney on weeks 5–8 of gestation leads to crossed ectopia
Aberrant interactions between the UB and MM or stroma result in renal hypodysplasia, which is observed in 0.027% of fetuses by ultrasonography [42] (Fig. 2). Importantly, renal hypodysplasia due to decreased nephron endowment is causally linked to hypertension and eventual progression to chronic renal failure [48, 49]. Horseshoe kidney, which occurs in 1 in 1,000 newborns, may be caused by defects in renal capsule and failed migration due to aberrant stromal Foxd1 signaling [50, 51]. Nephron patterning defects may be due to aberrant cell proliferation, apoptosis, cell movements, or other causes. In this regard, altered balance of cell proliferation and apoptosis is responsible for abnormal patterning of the medulla in Beckwith–Wiedemann syndrome due to mutation in p57 KIP2, an inhibitor of cell proliferation [52]. Polycystic kidney disease (PKD), in which cysts arise from tubules that were formed normally in the context of development, represents another example of patterning defect. Here, increased tubular cell proliferation together with decreased integration of cells into the plane of tubular epithelium or loss of oriented cell division may account for postnatal cyst formation [53]. PUV, observed in 0.003% of fetal ultrasounds, are due to aberrant cloacal development [42]. A concerted effort to provide new insights into pathologic processes underlying the development of CAKUT is in progress within the Genitourinary Development Molecular Atlas Project (GUDMAP) [54].
Genetic mutations associated with human renal hypodysplasia
It is well appreciated that many instances of human CAKUT have a genetic basis and are associated with hereditary syndromes (Supplemental Table 1) [55]. The inheritance pattern of some nonsyndromic cases of CAKUT (e.g. autosomal-dominant or -recessive polycystic kidney disease) is well known [56]. Evidence is accumulating to suggest that mutations in select RDGs may be causally linked to the pathogenesis of nonsyndromic forms of CAKUT in humans (Table 1). Interestingly, mutations in a given RDG may be associated with a spectrum of urinary system anomalies. For example, Branchio-oto-renal (BOR) syndrome due to Eya1 mutations may be accompanied by renal agenesis or dysplasia, hypoplasia, or renal collecting system anomalies [57]. It is therefore conceivable that Eya1 plays an important role at multiple stages of renal system morphogenesis. One of the mechanisms accounting for stage-specific impact of Eya1 mutation on renal system phenotype may involve cell-type-dependent interplay of up- or downstream regulators of Eya1. This possibility is supported by the findings that HNF1β, developmentally regulated transcription factor induces expression of uromodulin (UMOD) [58]. Although HNF1β or UMOD mutations in humans cause renal hypodysplasia, the spectrum of disease phenotypes and age of their manifestations differ. HNF1β mutations manifest earlier in childhood and are associated with glomerulocystic kidney disease, unilateral multicystic dysplastic kidney (MCDK), uni- or bilateral cystic kidneys, renal hypodysplasia without cysts, horseshoe kidney, and oligomeganephronia [59–62]. HNF1β mutations are detected in 33% of children with nonsyndromic MCDK or renal hypodysplasia [61]. Most genetic alterations (64%) in this study were due to complete deletion of the gene, followed by truncating and nonsense mutations. No correlation between type of mutation and phenotype was observed. Interestingly, in 53% of probands, HNF1β mutations occurred de novo [61]. These findings suggest a weak probability of genetic inheritance.
UMOD mutations are identified in medullary cystic kidney disease 2 (MCKD2) and familial juvenile hyperuricemic nephropathy, diseases that manifest later in life [63]. In fact, no known UMOD mutations were identified in children with diverse forms of nonsyndromic CAKUT in a study by Wolf et al. [64]. The authors proposed that unknown UMOD mutations may be causally linked to CAKUT in children. This possibility is supported by recent identification of a novel UMOD sequence variant in a child with decreased kidney function and hyperuricemia accompanied by histologic evidence of immature renal structures [65]. In contrast to the impact of HNF1β or UMOD mutations on renal disease phenotype, Pax2, a transcription factor present in the metanephric mesenchyme, but not GDNF, polymorphism is associated with reduced kidney size in neonates [66, 67]. GDNF/c-Ret pathway is critical for metanephric development and GDNF expression is activated by Pax2 [68]. Again, differential effects of Pax2 and GDNF polymorphism on renal phenotype may be due, in part, to unidentified cell-specific cofactors that regulate gene expression. Interestingly, RDG mutations associated with syndromal CAKUT [HNF1β, Eya1, Six1, sal-like 1 (Sall1), Pax2] are identified only in 5–15% of children from the European population with nonsyndromic CAKUT [69]. Another recent study that examined children from the European population found no association of primary VUR with mutations in Pax2, HNF1β, c-Ret or Robo2 [70].
Several studies report a discrepancy in the impact of genetic mutations on renal-system phenotype between mice and humans. For example, despite severe renal phenotype observed in ROBO2/SLIT2-mutant mice, which includes formation of supernumerary ureters [44], these gene mutations are very rarely associated with familial nonsyndromic VUR in children [71, 72]. Similarly, mutations in homeobox A11 and D11(HoxA11/HoxD11), which cause renal hypoplasia in mice [73], are not associated with CAKUT in children [74]. In addition, uroplakin (UP) UPII or UPIIIA mutations, which, respectively, cause hydronephrosis or VUR in mice [75], are not detected in the majority of children with nonsyndromic cases of CAKUT. However, UPII or UPIIIA mutations may account for CAKUT (e.g. MCDK or VUR) in a minority of these children [76–78]. Functionally, UPs account for impermeability of bladder epithelia to water. Mutations in Six2 and BMP4, which are expressed in the fetal kidney on weeks 9 and 12 of gestation, are identified in children with a broad spectrum of CAKUT ranging from unilateral or bilateral hypodysplasia to cystic dysplasia with or without VUR [79]. Moreover, detected BMP4 mutations are associated with decreased BMP4 messenger RNA (mRNA) levels and enhanced protein degradation [80]. Collectively, these data indicate that aberrant expression of RDGs is associated with diverse forms of CAKUT in humans. Interestingly, RDG mutations are detected in a minority of these patients [68]. These observations point to the potential role for other mechanisms in the developmental origin of CAKUT.
Insights into the mechanisms controlling CAKUT phenotype
Although mutations in many different single RDGs are associated with broad phenotypic spectrum of CAKUT ([6–9, 14], Tables 1 and 2, Supplemental Table 1), variability in genotype–phenotype correlation in renal system anomalies points to the essential roles of other factors. Phenotypic heterogeneity of CAKUT may result from differences in genetic background (variation of gene expression between alleles) [81], genetic [47, 82, 83] or epigenetic modifiers [84–86], and environment [87, 88]. In monogenic diseases, phenotypic outcome and disease severity depend on the mode of inheritance and type of mutation. Recessive diseases, such as autosomal recessive polycystic kidney disease, usually manifest full penetrance and present earlier in life. Disease course is more severe in truncating than missense polycystic kidney and hepatic disease 1 (PKHD1) mutations [89]. The strength of genotype–phenotype correlation is reduced in autosomal dominant nonsyndromic types of CAKUT [90]. This may be due to incomplete penetrance (lack of disease manifestation in the presence of gene mutation) or variable expression (variation in type and severity of disease between individuals with the same gene mutation). Variability in genotype–phenotype correlation in CAKUT may also result from a modifier gene effect. Here, mutation in one gene will cause CAKUT or alter the phenotype only in the presence of genetic change in another gene (epistatic gene interactions). In this regard, nephronophthisis 1 (NPHP1) mutation causes isolated nephronophthisis, whereas NPHP6 mutation alone does not lead to disease. In contrast, a combination of the same mutations in NPHP1 and NPHP6 causes an additional extrarenal disease phenotype [91]. Other RDGs that interact genetically and may influence renal phenotype include Pax2 and LMX1B or Six1 and Tbx18 [47, 82]. Noteworthy, two missense mutations in Six1 identified in patients with BOR syndrome reduce Six1-Tbx18 complex formation [47].
In polygenic diseases, mutations in multiple genes act in concert with environmental effects to cause a phenotype. With respect to renal system anomalies, intrauterine environment and fetal programming have been linked to CAKUT. Maternal low-protein diet initiated at onset of pregnancy reduces nephron number and alters gene expression in the embryonic metanephros in mice [87]. Recent data indicate that environmental factors may act in concert with single-gene mutations to cause CAKUT. In this regard, renal hypodysplasia is caused by salt loading during embryonic development in bradykinin B2 receptor-deficient, but not in wild-type, mice [88]. Exposure to cocaine or alcohol during gestation results in CAKUT in children [92, 93]. Importantly, the mechanistic basis for CAKUT associated with altered intrauterine environment remains to be elucidated.
There is a growing appreciation of the role of epigenetics in the regulation of gene expression and disease causality. The major players in epigenetic mechanisms of gene regulation are DNA or chromatin protein methylation, acetylation, and chromatin remodeling. Posttranslational modifications of histones such as histone acetylation and methylation may affect chromatin function and alter RDG expression in the absence of changes in DNA sequence [94, 95]. Relevant to pathogenesis of CAKUT, a recent study demonstrated a link between Pax2, a transcription factor critical for renal morphogenesis, and chromatin methylation [84]. Gene expression may also be regulated at the posttranscriptional level by noncoding micro-RNAs (miRNAs). A critical role for miRNAs in kidney development is evident from the observation that targeted genetic inactivation of Dicer, the miRNA-processing enzyme, in UB in mice results in hydronephrosis [96]. Collectively, these observations indicate that pathogenesis of CAKUT is a complex process that depends on the interplay of many factors. Moreover, despite advances in elucidation of the cellular and molecular mechanisms linking kidney organogenesis to CAKUT, our understanding of its cause in an individual patient is still too limited.
Renin–angiotensin system and CAKUT
The renin–angiotensin system (RAS) plays a major role in controlling blood pressure, fluid, and electrolyte homeostasis. The developing mammalian metanephros expresses all components of the RAS [9]. Mutations in the genes encoding components of the RAS in mice cause diverse forms of CAKUT, which include hydronephrosis, hypoplastic medulla and papilla, marked thickening of renal arterial walls, duplex ureters, and vesicoureteral reflux [9, 97, 98]. Genetic manipulations in mice provided essential information regarding the mechanisms by which an intact RAS controls proper renal system development. The mechanistic basis of CAKUT due to RAS mutations may involve hypoplastic ureteral smooth-muscle layer, which exhibits impaired peristalsis [99], inhibition of Pax2 [100], GDNF/c-Ret [101, 102], or epidermal growth factor (EGF)-receptor [103] signaling, induction of BMP4 [104], decreased UB cell proliferation/survival resulting in reduced UB branching [101, 104] and reduced glomerular size [100]. Reduction in EGF and PDGF expression in the medulla may account for renal papillary hypoplasia observed in angiotensinogen (AGT)-null mice [105]. In addition, increased PDGF expression in endothelial cells may be responsible for thickening of the renal arteries observed in these mice [105].
With respect to epigenetic modifications of the RAS genes and its impact on CAKUT, recent studies in mice demonstrated that genetic inactivation of histone acetyltransferases such as cyclic adenosine monophosphate (cAMP)-response element-binding protein [CREB; (CBP)] and p300 alters kidney structure and results in a decreased number of renin-positive cells [86]. Notably, kidneys of CBP/p300-null mice exhibit interstitial fibrosis, disorganized vasculature, and medullary and cortical cysts [86]. In addition, targeted genetic inactivation of Dicer in juxtaglomerular cells causes a decrease in renin expression accompanied by striped fibrosis, a decrease in the number of renal vessels, and glomerular sclerosis [106]. These data demonstrate that epigenetic modifications of the RAS and miRNAs play an important role in maintaining renal structural integrity.
Impact of RAS gene mutations on CAKUT in humans
All components of the RAS are expressed in the embryonic kidney as early as the fifth week of gestation [107, 108] when metanephric organogenesis is initiated [5]. Initial evidence to indicate the critical role of the RAS in renal system organogenesis in humans was provided by the findings that the use of angiotensin-converting enzyme (ACE) inhibitors or AT1-receptor antagonists causes fetal anuria, leading to oligohydramnios [109, 110]. Evidence is emerging to suggest that mutations in the RAS genes may be causally linked to the pathogenesis of CAKUT in humans. In this regard, homozygous or compound heterozygous mutations in the genes encoding for AGT, renin, ACE, or AT1 receptors in French children are associated with renal tubular dysgenesis (RTD) [111]. Detected DNA mutations include the following nucleotide alterations: 1124G>A (AGT), 145C>T, 689G>A, 310G>A (renin), 798C>G (ACE), 845C>T (AT1R). In RTD, the kidneys are usually of normal size. Renal cortex exhibits a paucity of proximal tubules. In the medulla, collapsed collecting ducts and abundant interstitial fibrosis are observed [112]. Vascular changes involve thickening of arterial walls. Glomerular number may be normal, low, or increased, whereas glomerular size is normal or enlarged. In addition, all affected individuals exhibit hypotension. Importantly, the majority of children with RTD die in the perinatal period due to anuria combined with pulmonary hypoplasia. Few patients survive beyond the neonatal period. However, no correlation has been identified so far between the type of mutation and clinical course.
Association of single polymorphism in the human AT 2 R gene, 1332A>G transition, with CAKUT have been reported in several, but not all, studies. This alteration in the AT 2 R is described in American and German Caucasian males with ureteropelvic junction (UPJ) stenosis, megaureter, and MCDK [98, 113]. The same transition was detected in Korean children with unilateral MCDK, renal agenesis, and hydronephrosis [114]; in Italian children with VUR, hypoplastic kidney, UPJ stenosis, nonobstructive megaureter, and PUV [115], and in Serbian children with UPJ, VUR, or megaureter [116]. In contrast, there was no association of primary VUR with mutations in AT 2 R in a recent European study [70]. This difference may be due to an insufficient number of patients studied, limitations in study design, low penetrance of AT 2 R mutation, contribution of modifier genes, or other factors. ACE polymorphism is associated with kidney hypodysplasia caused by posterior urethral valves [117]. Collectively, emerging evidence points to an important role for the intact RAS in structural maturation of the kidney and urinary tract in humans.
The reasons for different renal phenotypes, particularly in papillary hypoplasia and hydronephrosis observed in mice but not in humans with RAS gene mutations are not clear. Additional discrepancy includes the presence of severe proximal tubular damage in humans and apparent absence of these changes in mice. One potential mechanism to explain these differences may include timing in completion of nephrogenesis. In this regard, new nephron formation ceases at 36 weeks of gestation in humans but continues for 2 weeks after birth in mice. It is conceivable that postnatal rise in renal blood flow (RBF) contributes to normal proximal tubule patterning in mice. In addition, rising RBF may enhance the postnatal urine flow rate, which, together with decreased ureteral peristalsis [99], will cause hydronephrosis.
Conclusions
Given the broad spectrum of human CAKUT and variable clinical impact of different forms of renal system anomalies ranging from mild asymptomatic cases to severe kidney injury manifesting before or after birth, each patient with CAKUT requires individualized clinical management. Because morbidity in mild cases of CAKUT may not manifest until later in life, these patients should be closely followed throughout life. Medical monitoring should include diet, nutritional status, growth, blood pressure, renal function, proteinuria, and urinary tract imaging. New biomarkers are needed to better assess disease progression and therapeutic strategies (e.g. prenatal correction of obstruction or use of renin system inhibitors to slow progression of renal injury to preserve renal function). Genetic counseling is recommended for all patients with familial cases of CAKUT or newly diagnosed forms of CAKUT that suggest presence of genetic anomalies. Introduction of more sensitive array-based methods that allow screening for multiple gene mutations and unravel a complex network of molecular interactions will help determine and predict occurrence and consequences of CAKUT. Finally, establishment of shared large biorepositories of patients with CAKUT for molecular, genetic, and translational studies will have a major impact on designing novel strategies to prevent and manage CAKUT.
References
Daneman A, Alton DJ (1991) Radiographic manifestations of renal anomalies. Radiol Clin North Am 29:351–363
Nakanishi K, Yoshikawa N (2003) Genetic disorders of human congenital anomalies of the kidney and urinary tract (CAKUT). Pediatr Int 45:610–616
North American Pediatric Renal Trials and Collaborative Studies (2008) NAPRTCS Annual report. Available at https://web.emmes.com/study/ped/annlrept/Annual%20Report%20-2008.pdf
Baluarte HJ, Gruskin AB, Ingelfinger JR, Stablein D, Tejani A (1994) Analysis of hypertension in children post renal transplantation: a report of the North American Pediatric Renal Transplant Cooperative Study (NAPRTCS). Pediatr Nephrol 8:570–573
Saxen L (1987) Organogenesis of the kidney. Cambridge University Press, Cambridge
Costantini F (2006) Renal branching morphogenesis: concepts, questions, and recent advances. Differentiation 74:402–421
Dressler GR (2009) Advances in early kidney specification, development and patterning. Development 136:3863–3874
Reidy KJ, Rosenblum ND (2009) Cell and molecular biology of kidney development. Semin Nephrol 29:321–337
Yosypiv IV (2009) Renin-angiotensin system-growth factor cross-talk: a novel mechanism for ureteric bud morphogenesis. Pediatr Nephrol 24:1113–1120
Grobstein C (1953) Inductive epithelio-mesenchymal interaction in cultured organ rudiments of the mouse metanephros. Science 118:52–55
Ekblom P (1989) Developmentally regulated conversion of mesenchyme to epithelium. FASEB J 3:2141–2150
al-Awqati Q, Goldberg MR (1998) Architectural patterns in branching morphogenesis in the kidney. Kidney Int 54:1832–1842
Fetterman GH, Shuplock NA, Rhilipp FJ, Gregg HS (1965) The growth and maturation of human glomeruli and proximal convolutions from term to adulthood: studies by microdissection. Pediatrics 35:601–619
Mendelsohn C (2009) Using mouse models to understand normal and abnormal urogenital tract development. Organogenesis 5:306–314
Schuchardt A, D'Agati V, Larsson-Blomberg L, Costantini F, Pachnis V (1994) Defects in the kidney and enteric nervous system of mice lacking the tyrosine kinase receptor. Nature Ret 367:380–383
Chi X, Michos O, Shakya R, Riccio P, Enomoto H, Licht JD, Asai N, Takahashi M, Ohgami N, Kato M, Mendelsohn C, Costantini F (2009) Ret-dependent cell rearrangements in the Wolffian duct epithelium initiate ureteric bud morphogenesis. Dev Cell 17:199–209
Moreau E, Vilar J, Lelièvre-Pégorier M, Merlet-Bénichou C, Gilbert T (1998) Regulation of c-ret expression by retinoic acid in rat metanephros: implication in nephron mass control. Am J Physiol 275:F938–F945
Basson MA, Watson-Johnson J, Shakya R, Akbulut S, Hyink D, Costantini FD, Wilson PD, Mason IJ, Licht JD (2006) Branching morphogenesis of the ureteric epithelium during kidney development is coordinated by the opposing functions of GDNF and Sprouty1. Dev Biol 299:466–477
Clarke JC, Patel SR, Raymond RM Jr, Andrew S, Robinson BG, Dressler GR, Brophy PD (2006) Regulation of c-Ret in the developing kidney is responsive to Pax2 gene dosage. Hum Mol Genet 15:3420–3428
Michos O, Cebrian C, Hyink D, Grieshammer U, Williams L, D'Agati V, Licht JD, Martin GR, Costantini F (2010) Kidney development in the absence of Gdnf and Spry1 requires Fgf10. PLoS Genet 6:1–11
Hatini A, Huh SO, Herzlinger D, Soares VC, Lai E (1996) Essential role of stromal mesenchyme in kidney morphogenesis revealed by targeted disruption of Winged Helix transcription factor BF-2. Genes Dev 10:1467–1478
Mendelsohn C, Batourina E, Fung S, Gilbert T, Dodd J (1999) Stromal cells mediate retinoid-dependent functions essential for renal development. Development 126:1139–1148
Cullen-McEwen LA, Caruana G, Bertram JF (2005) The where, what and why of the developing renal stroma. Nephron Exp Nephrol 99:e1–e8
Stark K, Vainio S, Vassileva G, McMahon AP (1994) Epithelial transformation of metanephric mesenchyme in the developing kidney regulated by Wnt-4. Nature 372:679–683
Carroll TJ, Park JS, Hayashi S, Majumdar A, McMahon AP (2005) Wnt9b plays a central role in the regulation of mesenchymal to epithelial transitions underlying organogenesis of the mammalian urogenital system. Dev Cell 9:283–392
Iglesias DM, Hueber PA, Chu L, Campbell R, Patenaude AM, Dziarmaga AJ, Quinlan J, Mohamed O, Dufort D, Goodyer PR (2007) Canonical WNT signaling during kidney development. Am J Physiol 293:F494–F500
Lokmane L, Heliot C, Garcia-Villalba P, Fabre M, Cereghini S (2010) vHNF1 functions in distinct regulatory circuits to control ureteric bud branching and early nephrogenesis. Development 137:347–357
Karner CM, Chirumamilla R, Aoki S, Igarashi P, Wallingford JB, Carroll TJ (2009) Wnt9b signaling regulates planar cell polarity and kidney tubule morphogenesis. Nat Genet 41:793–799
Kobayashi A, Valerius MT, Mugford JW, Carroll TJ, Self M, Oliver G, McMahon AP (2008) Six2 defines and regulates a multipotent self-renewing nephron progenitor population throughout mammalian kidney development. Cell Stem Cell 3:169–181
Reggiani L, Raciti D, Airik R, Kispert A, Brändli AW (2007) The prepattern transcription factor Irx3 directs nephron segment identity. Genes Dev 21:2358–2370
Cheng HT, Kim M, Valerius MT, Surendran K, Schuster-Gossler K, Gossler A, McMahon AP, Kopan R (2007) Notch2, but not Notch1, is required for proximal fate acquisition in the mammalian nephron. Development 134:801–811
Fujimura S, Jiang Q, Kobayashi C, Nishinakamura R (2010) Notch2 activation in the embryonic kidney depletes nephron progenitors. J Am Soc Nephrol 21:803–810
Ryan G, Steele-Perkins V, Morris JF, Rauscher FJ 3rd, Dressler GR (1995) Repression of Pax-2 by WT1 during normal kidney development. Development 121:867–875
Suleiman H, Heudobler D, Raschta AS, Zhao Y, Zhao Q, Hertting I, Vitzthum H, Moeller MJ, Holzman LB, Rachel R, Johnson R, Westphal H, Rascle A, Witzgall R (2007) The podocyte-specific inactivation of Lmx1b, Ldb1 and E2a yields new insight into a transcriptional network in podocytes. Dev Biol 304:701–712
Reidy KJ, Villegas G, Teichman J, Veron D, Shen W, Jimenez J, Thomas D, Tufro A (2009) Semaphorin3a regulates endothelial cell number and podocyte differentiation during glomerular development. Development 136:3979–3989
Tufro A, Norwood VF, Carey RM, Gomez RA (1999) Vascular endothelial growth factor induces nephrogenesis and vasculogenesis. J Am Soc Nephrol 10:2125–2134
Lindahl P, Hellström M, Kalén M, Karlsson L, Pekny M, Pekna M, Soriano P, Betsholtz C (1998) Paracrine PDGF-B/PDGF-Rbeta signaling controls mesangial cell development in kidney glomeruli. Development 125:3313–3322
Batourina E, Choi C, Paragas N, Bello N, Hensle T, Costantini FD, Schuchardt A, Bacallao RL, Mendelsohn CL (2002) Distal ureter morphogenesis depends on epithelial cell remodeling mediated by vitamin A and Ret. Nat Genet 32:109–115
Batourina E, Tsai S, Lambert S, Sprenkle P, Viana R, Dutta S, Hensle T, Wang F, Niederreither K, McMahon AP, Carroll TJ, Mendelsohn CL (2005) Apoptosis induced by vitamin A signaling is crucial for connecting the ureters to the bladder. Nat Genet 37:1082–1089
Uetani N, Bertozzi K, Chagnon MJ, Hendriks W, Tremblay ML, Bouchard M (2009) Maturation of ureter-bladder connection in mice is controlled by LAR family receptor protein tyrosine phosphatases. J Clin Invest 119:924–935
Hiraoka M, Hori C, Tsukahara H, Kasuga K, Ishihara Y, Sudo M (1997) Congenitally small kidneys with reflux as a common cause of nephropathy in boys. Kidney Int 52:811–816
Wiesel A, Queisser-Luft A, Clementi M, Bianca S, Stoll C (2005) Prenatal detection of congenital renal malformations by fetal ultrasonographic examination: an analysis of 709, 030 births in 12 European countries. Eur J Med Genet 48:131–144
Miyazaki Y, Oshima K, Fogo A, Hogan BL, Ichikawa I (2000) Bone morphogenetic protein 4 regulates the budding site and elongation of the mouse ureter. J Clin Invest 105:863–873
Grieshammer U, Ma L, Plump AS, Wang F, Tessier-Lavigne M, Martin GR (2004) SLIT2-mediated ROBO2 signaling restricts kidney induction to a single site. Dev Cell 6:709–717
Garne E, Loane M, Wellesley D, Barisic I (2009) Congenital hydronephrosis: prenatal diagnosis and epidemiology in Europe. J Pediatr Urol 5:47–52
Airik R, Bussen M, Singh MK, Petry M, Kispert A (2006) Tbx18 regulates the development of the ureteral mesenchyme. J Clin Invest 116:663–674
Nie X, Sun J, Gordon RE, Cai CL, Xu PX (2010) SIX1 acts synergistically with TBX18 in mediating ureteral smooth muscle formation. Development 137:755–765
Brenner BM, Garcia DL, Anderson S (1988) Glomeruli and blood pressure. Less of one, more the other? Am J Hypertens 1:335–347
Lisle SJ, Lewis RM, Petry CJ, Ozanne SE, Hales CN, Forhead AJ (2003) Effect of maternal iron restriction during pregnancy on renal morphology in the adult rat offspring. Br J Nutr 90:33–39
Weizer AZ, Silverstein AD, Auge BK, Delvecchio FC, Raj G, Albala DM, Leder R, Preminger GM (2003) Determining the incidence of horseshoe kidney from radiographic data at a single institution. J Urol 170:1722–1726
Levinson RS, Batourina E, Choi C, Vorontchikhina M, Kitajewski J, Mendelsohn CL (2005) Foxd1-dependent signals control cellularity in the renal capsule, a structure required for normal renal development. Development 132:529–539
Hatada I, Ohashi H, Fukushima Y, Kaneko Y, Inoue M, Komoto Y, Okada A, Ohishi S, Nabetani A, Morisaki H, Nakayama M, Niikawa N, Mukai T (1996) An imprinted gene p57KIP2 is mutated in Beckwith-Wiedemann syndrome. Nat Genet 14:171–173
Nishio S, Tian X, Gallagher AR, Yu Z, Patel V, Igarashi P, Somlo S (2010) Loss of oriented cell division does not initiate cyst formation. J Am Soc Nephrol 21:295–302
McMahon AP, Aronow BJ, Davidson DR, Davies JA, Gaido KW, Grimmond S, Lessard JL, Little MH, Potter SS, Wilder EL, Zhang P (2008) GUDMAP: the genitourinary developmental molecular anatomy project. J Am Soc Nephrol 19:667–671
Rosenblum ND (2008) Developmental biology of the human kidney. Semin Fetal Neonatal Med 13:125–132
Rossetti S, Harris PC (2007) Genotype-phenotype correlations in autosomal dominant and autosomal recessive polycystic kidney disease. J Am Soc Nephrol 18:1374–1380
Abdelhak S, Kalatzis V, Heilig R, Compain S, Samson D, Vincent C, Weil D, Cruaud C, Sahly I, Leibovici M, Bitner-Glindzicz M, Francis M, Lacombe D, Vigneron J, Charachon R, Boven K, Bedbeder P, Van Regemorter N, Weissenbach J, Petit C (1997) A human homologue of the Drosophila eyes absent gene underlies branchio-oto-renal (BOR) syndrome and identifies a novel gene family. Nat Genet 15:157–164
Gresh L, Fischer E, Reimann A, Tanguy M, Garbay S, Shao X, Hiesberger T, Fiette L, Igarashi P, Yaniv M, Pontoglio M (2004) A transcriptional network in polycystic kidney disease. EMBO J 23:1657–1668
Mache CJ, Preisegger KH, Kopp S, Ratschek M, Ring E (2002) De novo HNF-1 beta gene mutation in familial hypoplastic glomerulocystic kidney disease. Pediatr Nephrol 17:1021–1026
Edghill EL, Bingham C, Ellard S, Hattersley AT (2005) Mutations in hepatocyte nuclear factor-1beta and their related phenotypes. J Med Genet 43:84–90
Ulinski T, Lescure S, Beaufils S, Guigonis V, Decramer S, Morin D, Clauin S, Deschênes G, Bouissou F, Bensman A, Bellanné-Chantelot C (2006) Renal phenotypes related to hepatocyte nuclear factor-1beta (TCF2) mutations in a pediatric cohort. J Am Soc Nephrol 17:497–503
Nakayama M, Nozu K, Goto Y, Kamei K, Ito S, Sato H, Emi M, Nakanishi K, Tsuchiya S, Iijima K (2010) HNF1B alterations associated with congenital anomalies of the kidney and urinary tract. Pediatr Nephrol 25:1073–1079
Hart TC, Gorry MC, Hart PS, Woodard AS, Shihabi Z, Sandhu J, Shirts B, Xu L, Zhu H, Barmada MM, Bleyer AJ (2002) Mutations of the UMOD gene are responsible for medullary cystic kidney disease 2 and familial juvenile hyperuricaemic nephropathy. J Med Genet 39:882–892
Wolf MT, Hoskins BE, Beck BB, Hoppe B, Tasic V, Otto EA, Hildebrandt F (2009) Mutation analysis of the Uromodulin gene in 96 individuals with urinary tract anomalies (CAKUT). Pediatr Nephrol 24:55–60
Benetti E, Caridi G, Vella MD, Rampoldi L, Ghiggeri GM, Artifoni L, Murer L (2009) Immature renal structures associated with a novel UMOD sequence variant. Am J Kidney Dis 53:327–331
Quinlan J, Lemire M, Hudson T, Qu H, Benjamin A, Roy A, Pascuet E, Goodyer M, Raju C, Zhang Z, Houghton F, Goodyer P (2007) A common variant of the PAX2 gene is associated with reduced newborn kidney size. J Am Soc Nephrol 18:1915–1921
Zhang Z, Quinlan J, Grote D, Lemire M, Hudson T, Benjamin A, Roy A, Pascuet E, Goodyer M, Raju C, Houghton F, Bouchard M, Goodyer P (2009) Common variants of the glial cell-derived neurotrophic factor gene do not influence kidney size of the healthy newborn. Pediatr Nephrol 24:1151–1157
Brophy PD, Ostrom L, Lang KM, Dressler GR (2001) Regulation of ureteric bud outgrowth by Pax2-dependent activation of the glial derived neurotrophic factor gene. Development 128:4747–4756
Weber S, Moriniere V, Knüppel T, Charbit M, Dusek J, Ghiggeri GM, Jankauskiené A, Mir S, Montini G, Peco-Antic A, Wühl E, Zurowska AM, Mehls O, Antignac C, Schaefer F, Salomon R (2006) Prevalence of mutations in renal developmental genes in children with renal hypodysplasia: results of the ESCAPE study. J Am Soc Nephrol 17:2864–2870
Cordell HJ, Darlay R, Charoen P, Stewart A, Gullett AM, Lambert HJ, Malcolm S, Feather SA, Goodship TH, Woolf AS, Kenda RB, Goodship JA (2010) Whole-genome linkage and association scan in primary, nonsyndromic vesicoureteric reflux. J Am Soc Nephrol 21:113–123
Bertoli-Avella AM, Conte ML, Punzo F, de Graaf BM, Lama G, La Manna A, Polito C, Grassia C, Nobili B, Rambaldi PF, Oostra BA, Perrotta S (2008) ROBO2 gene variants are associated with familial vesicoureteral reflux. J Am Soc Nephrol 19:825–831
Zu S, Bartik Z, Zhao S, Sillen U, Nordenskjöld A (2009) Mutations in the ROBO2 and SLIT2 genes are rare causes of familial vesico-ureteral reflux. Pediatr Nephrol 24:1501–1508
Patterson LT, Pembaur M, Potter SS (2001) Hoxa11 and Hoxd11 regulate branching morphogenesis of the ureteric bud in the developing kidney. Development 128:2153–2161
Bouba I, Siomou E, Stefanidis CJ, Emmanouilidou A, Galidi A, Hatzi E, Markoula S, Mitsioni A, Siamopoulou A, Georgiou I (2009) Absence of mutations in the HOXA11 and HOXD11 genes in children with congenital renal malformations. Pediatr Nephrol 24:1569–1572
Wu XR, Kong XP, Pellicer A, Kreibich G, Sun TT (2009) Uroplakins in urothelial biology, function, and disease. Kidney Int 75:1153–1165
Jenkins D, Bitner-Glindzicz M, Malcolm S, Allison J, de Bruyn R, Flanagan S, Thomas DF, Belk RA, Feather SA, Bingham C, Southgate J, Woolf AS (2006) Mutation analyses of Uroplakin II in children with renal tract malformations. Nephrol Dial Transplant 21:3415–3421
Jenkins D, Bitner-Glindzicz M, Thomasson L, Malcolm S, Warne SA, Feather SA, Flanagan SE, Ellard S, Bingham C, Santos L, Henkemeyer M, Zinn A, Baker LA, Wilcox DT, Woolf AS (2007) Mutational analyses of UPIIIA, SHH, EFNB2 and HNF1beta in persistent cloaca and associated kidney malformations. J Pediatr Urol 3:2–9
Schönfelder EM, Knüppel T, Tasic V, Miljkovic P, Konrad M, Wühl E, Antignac C, Bakkaloglu A, Schaefer F, Weber S (2006) Mutations in Uroplakin IIIA are a rare cause of renal hypodysplasia in humans. Am J Kidney Dis 47:1004–1012
Weber S, Taylor JC, Winyard P, Baker KF, Sullivan-Brown J, Schild R, Knüppel T, Zurowska AM, Caldas-Alfonso A, Litwin M, Emre S, Ghiggeri GM, Bakkaloglu A, Mehls O, Antignac C, Network E, Schaefer F, Burdine RD (2008) SIX2 and BMP4 mutations associate with anomalous kidney development. J Am Soc Nephrol 19:891–903
Tabatabaeifar M, Schlingmann KP, Litwin M, Emre S, Bakkaloglu A, Mehls O, Antignac C, Schaefer F, Weber S (2009) Functional analysis of BMP4 mutations identified in pediatric CAKUT patients. Pediatr Nephrol 24:2361–2368
Lo HS, Wang Z, Hu Y, Yang HH, Gere S, Buetow KH, Lee MP (2003) Allelic variation in gene expression is common in the human genome. Genome Res 13:1855–1862
Marini M, Giacopelli F, Seri M, Ravazzolo R (2005) Interaction of the LMX1B and PAX2 gene products suggests possible molecular basis of differential phenotypes in Nail-Patella syndrome. Eur J Hum Genet 13:789–792
Fain PR, McFann KK, Taylor MR, Tison M, Johnson AM, Reed B, Schrier RW (2005) Modifier genes play a significant role in the phenotypic expression of PKD1. Kidney Int 67:1256–1267
Patel SR, Kim D, Levitan I, Dressler GR (2007) The BRCT-domain containing protein PTIP links PAX2 to a histone H3, lysine 4 methyltransferase complex. Dev Cell 13:580–592
Pogribny IP, Beland FA (2009) DNA hypomethylation in the origin and pathogenesis of human diseases. Cell Mol Life Sci 66:2249–2261
Gomez RA, Pentz ES, Jin X, Cordaillat M, Sequeira Lopez ML (2009) CBP and p300 are essential for renin cell identity and morphological integrity of the kidney. Am J Physiol 296:H1255–H1262
Welham SJ, Riley PR, Wade A, Hubank M, Woolf AS (2005) Maternal diet programs embryonic kidney gene expression. Physiol Genomics 22:48–56
El-Dahr SS, Harrison-Bernard LM, Dipp S, Yosipiv IV, Meleg-Smith S (2000) Bradykinin B2 null mice are prone to renal dysplasia: gene-environment interactions in kidney development. Physiol Genomics 3:121–131
Furu L, Onuchic LF, Gharavi A, Hou X, Esquivel EL, Nagasawa Y, Bergmann C, Senderek J, Avner E, Zerres K, Germino GG, Guay-Woodford LM, Somlo S (2003) Milder presentation of recessive polycystic kidney disease requires presence of amino acid substitution mutations. J Am Soc Nephrol 14:2004–2014
McPherson E, Carey J, Kramer A, Hall JG, Pauli RM, Schimke RN, Tasin MH (1987) Dominantly inherited renal adysplasia. Am J Med Genet 26:863–872
Tory K, Lacoste T, Burglen L, Morinière V, Boddaert N, Macher MA, Llanas B, Nivet H, Bensman A, Niaudet P, Antignac C, Salomon R, Saunier S (2007) High NPHP1 and NPHP6 mutation rate in patients with Joubert syndrome and nephronophthisis: potential epistatic effect of NPHP6 and AHI1 mutations in patients with NPHP1 mutations. J Am Soc Nephrol 18:1566–1575
Battin M, Albersheim S, Newman D (1995) Congenital genitourinary tract abnormalities following cocaine exposure in utero. Am J Perinatol 12:425–428
Qazi Q, Masakawa A, Milman D, McGann B, Chua A, Haller J (1979) Renal anomalies in fetal alcohol syndrome. Pediatrics 63:886–889
Smith CL (2008) A shifting paradigm: histone deacetylases and transcriptional activation. Bioessays 30:15–24
Nottke A, Colaiácovo MP, Shi Y (2009) Developmental roles of the histone lysine demethylases. Development 136:879–889
Pastorelli LM, Wells S, Fray M, Smith A, Hough T, Harfe BD, McManus MT, Smith L, Woolf AS, Cheeseman M, Greenfield A (2009) Genetic analyses reveal a requirement for Dicer1 in the mouse urogenital tract. Mamm Genome 20:140–151
Oshima K, Miyazaki Y, Brock JW, Adams MC, Ichikawa I, Pope JC (2001) Angiotensin type II receptor expression and ureteral budding. J Urol 166:1848–1852
Nishimura H, Yerkes E, Hohenfellner K, Miyazaki Y, Ma J, Hunley TE, Yoshida H, Ichiki T, Threadgill D, Phillips JA 3rd, Hogan BM, Fogo A, Brock JW 3rd, Inagami T, Ichikawa I (1999) Role of the angiotensin type 2 receptor gene in congenital anomalies of the kidney and urinary tract, CAKUT, of mice and men. Mol Cell 3:1–10
Miyazaki Y, Tsuchida S, Nishimura H, Pope JC 4th, Harris RC, McKanna JM, Inagami T, Hogan BL, Fogo A, Ichikawa I (1998) Angiotensin induces the urinary peristaltic machinery during the perinatal period. J Clin Invest 102:1489–1497
Chen YW, Tran S, Chenier I, Chan JS, Ingelfinger JR, Inagami T, Zhang SL (2008) Deficiency of intrarenal angiotensin II type 2 receptor impairs paired homeo box-2 and N-myc expression during nephrogenesis. Pediatr Nephrol 23:1769–1777
Yosypiv IV, Boh MK, Spera M, El-Dahr SS (2008) Downregulation of Spry-1, an inhibitor of GDNF/Ret, as a mechanism for angiotensin II-induced ureteric bud branching. Kidney Int 74:1287–1293
Song R, Spera M, Garrett C, Yosypiv IV (2010) Angiotensin II-induced activation of c-Ret signaling is critical in ureteric bud branching morphogenesis. Mech Dev 127:21–27
Yosypiv IV, Schroeder M, El-Dahr SS (2006) AT1R-EGFR crosstalk regulates ureteric bud branching morphogenesis. J Am Soc Nephrol 17:1005–1014
Song R, Spera M, Garrett C, El-Dahr S, Yosypiv IV (2010) Angiotensin II AT2 Receptor Regulates Ureteric Bud Morphogenesis. Am J Physiol 298:F807–F817
Niimura F, Labosky PA, Kakuchi J, Okubo S, Yoshida H, Oikawa T, Ichiki T, Naftilan AJ, Fogo A, Inagami T (1995) Gene targeting in mice reveals a requirement for angiotensin in the development and maintenance of kidney morphology and growth factor regulation. J Clin Invest 96:2947–2954
Sequeira-Lopez ML, Weatherford ET, Borges GR, Monteagudo MC, Pentz ES, Harfe BD, Carretero O, Sigmund CD, Gomez RA (2010) The microRNA-processing enzyme dicer maintains juxtaglomerular cells. J Am Soc Nephrol 21:460–467
Schütz S, Le Moullec JM, Corvol P, Gasc JM (1996) Early expression of all the components of the renin-angiotensin-system in human development. Am J Pathol 149:2067–2079
Mounier F, Hinglais N, Sich M, Gros F, Lacoste M, Deris Y, Alhenc-Gelas F, Gubler MC (1987) Ontogenesis of angiotensin-I converting enzyme in human kidney. Kidney Int 32:684–690
Schaefer C (2003) Angiotensin II-receptor-antagonists: further evidence of fetotoxicity but not teratogenicity. Birth Defects Res A Clin Mol Teratol 67:591–594
Tabacova S, Little R, Tsong Y, Vega A, Kimmel CA (2003) Adverse pregnancy outcomes associated with maternal enalapril antihypertensive treatment. Pharmacoepidemiol Drug Saf 12:633–646
Gribouval O, Gonzales M, Neuhaus T (2005) Mutations in genes in the renin-angiotensin system are associated with autosomal recessive renal tubular dysgenesis. Nat Genet 37:964–968
Lacoste M, Cai Y, Guicharnaud L, Mounier F, Dumez Y, Bouvier R, Dijoud F, Gonzales M, Chatten J, Delezoide AL, Daniel L, Joubert M, Laurent N, Aziza J, Sellami T, Amar HB, Jarnet C, Frances AM, Daïkha-Dahmane F, Coulomb A, Neuhaus TJ, Foliguet B, Chenal P, Marcorelles P, Gasc JM, Corvol P, Gubler MC (2006) Renal tubular dysgenesis, a not uncommon autosomal recessive disorder leading to oligohydramnios: role of the renin-angiotensin system. J Am Soc Nephrol 17:2253–2263
Hohenfellner K, Hunley TE, Schloemer C, Brenner W, Yerkes E, Zepp F, Brock JW 3rd, Kon V (1999) Angiotensin type 2 receptor is important in the normal development of the ureter. Pediatr Nephrol 13:187–191
Hahn H, Ku SE, Kim KS, Park YS, Yoon CH, Cheong HI (2005) Implication of genetic variations in congenital obstructive nephropathy. Pediatr Nephrol 20:1541–1544
Rigoli L, Chimenz R, di Bella C, Cavallaro E, Caruso R, Briuglia S, Fede C, Salpietro CD (2004) Angiotensin-converting enzyme and angiotensin type 2 receptor gene genotype distributions in Italian children with congenital uropathies. Pediatr Res 56:988–993
Stanković A, Zivković M, Kostić M, Atanacković J, Krstić Z, Alavantić D (2010) Expression profiling of the AT2R mRNA in affected tissue from children with CAKUT. Clin Biochem 43:71–75
Peruzzi L, Lombardo F, Amore A, Merlini E, Restagno G, Silvestro L, Papalia T, Coppo R (2005) Low renin-angiotensin system activity gene polymorphism and dysplasia associated with posterior urethral valves. J Urol 174:713–717
Skinner MA, Safford SD, Reeves JG, Jackson ME, Freemerman AJ (2008) Renal aplasia in humans is associated with RET mutations. Am J Hum Genet 82:344–351
Wolf MT, Beck BB, Zaucke F, Kunze A, Misselwitz J, Ruley J, Ronda T, Fischer A, Eifinger F, Licht C, Otto E, Hoppe B, Hildebrandt F (2007) The Uromodulin C744G mutation causes MCKD2 and FJHN in children and adults and may be due to a possible founder effect. Kidney Int 71:574–581
O'Toole JF, Liu Y, Davis EE, Westlake CJ, Attanasio M, Otto EA, Seelow D, Nurnberg G, Becker C, Nuutinen M, Kärppä M, Ignatius J, Uusimaa J, Pakanen S, Jaakkola E, van den Heuvel LP, Fehrenbach H, Wiggins R, Goyal M, Zhou W, Wolf MT, Wise E, Helou J, Allen SJ, Murga-Zamalloa CA, Ashraf S, Chaki M, Heeringa S, Chernin G, Hoskins BE, Chaib H, Gleeson J, Kusakabe T, Suzuki T, Isaac RE, Quarmby LM, Tennant B, Fujioka H, Tuominen H, Hassinen I, Lohi H, van Houten JL, Rotig A, Sayer JA, Rolinski B, Freisinger P, Madhavan SM, Herzer M, Madignier F, Prokisch H, Nurnberg P, Jackson P, Khanna H, Katsanis N, Hildebrandt F (2010) Individuals with mutations in XPNPEP3, which encodes a mitochondrial protein, develop a nephronophthisis-like nephropathy. J Clin Invest 120:791–802
Nakano T, Niimura F, Hohenfellner K, Miyakita E, Ichikawa I (2003) Screening for mutations in BMP4 and FOXC1 genes in congenital anomalies of the kidney and urinary tract in humans. Tokai J Exp Clin Med 28:121–126
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental Table 1
Multiorgan syndromes associated with congenital anomalies of the kidney and urinary tract (CAKUT) in humans (DOC 64.5 kb)
Supplemental Table 2
Glossary of genes (DOC 56.5 kb)
Rights and permissions
About this article
Cite this article
Song, R., Yosypiv, I.V. Genetics of congenital anomalies of the kidney and urinary tract. Pediatr Nephrol 26, 353–364 (2011). https://doi.org/10.1007/s00467-010-1629-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-010-1629-4