Abstract
Previous studies have shown that basal-type cytokeratins (CKs) can distinguish usual ductal hyperplasia (UDH) from the spectrum of atypical ductal hyperplasia (ADH), ductal carcinoma in situ (DCIS) and lobular carcinoma in situ (LCIS). Indeed, expression of these CKs is weak or absent in ADH, DCIS and LCIS. However, the diagnostic usefulness of D5/16B4 antibody (anti-CK5/6) has never been compared with that of 34βE12 antibody (anti-CK1/5/10/14). We performed immunostaining of CK 5/6 and CK1/5/10/14 on 100 breast lesions, including UDH (n=31), ADH (n=5), DCIS (n=54) and LCIS (n=10). Abundant immunostaining was observed in all UDH using both antibodies. Four of five of the ADH cases showed less than 5% of CK5/6 stained cells, the remaining case showed 30% of labeled cells. With 34βE12 antibody, three of five of the ADH cases showed less than 5% labeled cells, while two cases showed more than 30% of stained cells. None of the 54 DCIS or the 10 LCIS was labeled by D5/16B4, while a lack of 34βE12 immunostaining was observed in only 15 of 54 DCIS and 2 of 10 LCIS. We confirmed that D5/16B4 antibody directed against CK5/6 is useful in distinguishing UDH from the spectrum of ADH/DCIS/LCIS. We also demonstrated that D5/16B4 is far a more specific marker than 34βE12 antibody.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epithelial proliferations of the breast encompass a variety of proliferative and neoplastic lesions. Those formed in the terminal ductal-lobular units are categorized as ductal hyperplasia of usual type (UDH) or epitheliosis, atypical ductal hyperplasia (ADH), ductal carcinoma in situ (DCIS) and lobular carcinoma in situ (LCIS). The clinical management of these differs as the related risk of developing an invasive carcinoma is different in each case [1, 8, 18, 20, 26]. Distinction between these lesions is based on cyto-architectural analysis [24]. However, distinction often remains a challenge, as shown by the lack of interobserver reproducibility [17]. Some authors have proposed quantitative data as a useful means in separating ADH from DCIS, but controversies still exist regarding which criterion to apply [25, 26].
Immunohistochemistry may be of useful diagnostic assistance, as the expression of several molecules has been correlated to specific types of epithelial proliferations [22, 27]. Several studies have investigated the value of cytokeratin (CK) expression in such lesions [3, 7, 9, 10, 11, 13, 15].
Normal breast epithelium is complex and known to have three population cells, defined by the CK immunoprofile. The luminal layer is composed of a dual population, one of glandular-type epithelial cells associated with simple-epithelium keratins (CK7, CK8, CK18, CK19), and one of basal-type epithelial cells expressing basal-type keratins (CK5, CK14, CK17) but not smooth muscle actin α (SMAα) [2, 3, 9, 11, 14, 28]. The basal layer is composed of myoepithelial cells expressing basal-type keratins (CK5, CK14, CK17) and SMAα [2, 7, 9, 28]. Immunohistochemical studies with anti-CK antibodies have provided evidence for a distinct phenotype between UDH and the spectrum of ADH/DCIS. UDH is composed of a dual population, one associated with simple-epithelium keratins, and one associated with basal-type keratins [3, 7, 11, 13, 14, 15]. In contrast, previous studies have shown that most of ADH/DCIS are composed of a homogeneous population associated with simple-epithelium keratins [3, 9, 11, 13, 15, 28]. However, the immunohistological distinction between UDH and ADH/DCIS/LCIS is not always clear, as basal-type keratins may sometimes be found in ADH, DCIS and LCIS [3, 9, 13, 15].
Only rare studies of these lesions have investigated the practical value of CK5/6 immunostaining with D5/16 B4, a commercially available anti-basal-type keratin monoclonal antibody (mAb) which does not react with CK14 and which can be routinely used on formalin-fixed, paraffin-embedded specimens [4, 14]. Furthermore, no study has yet compared the CK5/6 immunostaining with the 34βE12 antibody (anti-CK 1/5/10/14) immunostaining in these lesions. Herein, we report the comparison of CK5/6 and 34βE12 labelings in 100 breast lesions including UDH, ADH, DCIS and LCIS.
Materials and methods
Case selection
All the specimens studied were obtained from the surgical pathology file of the Department of Pathology at the Institut Claudius Regaud, Toulouse, France, during the year 1999. No patient had previously received hormone or cytotoxic therapy. Sections stained with hematoxylin and eosin were reviewed independently by five pathologists (three seniors and two junior residents), and diagnosis discrepancies were resolved during a multi-head microscope session. The sections consisted of 100 consecutive female breast intraepithelial lesions showing either UDH (n=31), ADH (n=5), DCIS (n=54) and LCIS (n=10). The lesions were classified according to the criteria of Tavassoli et al. [24, 26]. DCIS cases were classified according to the Van Nuys grading system [21], based on nuclear grade and necrosis. The 54 specimens of DCIS were categorized as follows: 30 cases of grade 1, 12 cases of grade 2 and 12 cases of grade 3.
The tissue samples were fixed in formalin (32 cases) or in ethanol-based Bouin'fluid (Duboscq-Brasil) (68 cases) and paraffin embedded.
Immunohistochemical techniques
Immunohistochemistry was performed on 4-μm-thick routinely processed paraffin sections. A prior antigen retrieval based on microwave oven heating in 10 mM citrate buffer, pH 6, was used for all the immunostainings [19]. The primary monoclonal antibodies used were directed against keratins 5 and 6 (clone D5/16 B4; Dako, Glostrup, Denmark; dilution 1:100), and keratins 1, 5, 10 and 14 (clone 34βE12; Dako, dilution 1:200). The slides were processed using a Techmate Horizon (Dako) slide processor. Antibodies were incubated for 1 h and revealed using a streptavidin-biotin complex reagent (StrepABComplex/HRP Duet, Dako) according to the manufacturer's protocol. The chromogenic substrate was DAB (3,3′-diaminobenzidine). Slides were counterstained with hematoxylin. Staining was cytoplasmic, with or without membrane cell enhancement. Intensity of this staining was graded from weak to strong. Adjacent normal epithelial structures were used as positive (basal and myoepithelial cells) and negative (glandular cells) controls. Non-tumoral peripheral (myoepithelial) cell labeling was not taken into account. The percentage of labeled tumoral cells was reported for each case.
Results
Normal breast
All of the 100 specimens had normal breast tissue next to the lesion. Normal tissue showed a slightly different reactivity with CK5/6 and 34βE12 mAbs: both antibodies stained heterogeneously peripheral myoepithelial cells, but CK5/6 mAb stained a few luminal epithelial cells while 34βE12 mAb stained most luminal epithelial cells. Intensity of the staining was moderate to strong with both mAbs. Number of epithelial and myoepithelial labeled cells varied greatly from case to case and even within a single case. Columnar cell and apocrine metaplasias showed no reactivity with CK5/6 mAb, whereas a weak immunostaining was observed with 34βE12 mAb in both metaplasias. The pattern and intensity of the immunostainings were not modified by the fixative used.
Ductal hyperplasia of usual type
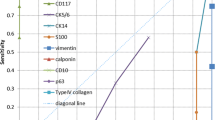
The results of the UDH immunostainings are summarized in Fig. 1. The UDH immunostainings obtained using CK5/6 and 34βE12 mAbs were very similar. All the cases showed an intense intracytoplasmic staining with cell membrane enhancement of more than 50% of the intraluminal cells with both antibodies (Fig. 2).
Comparative percentage results of CK5/6 and 34βE12 labeled cells according to the mammary ductal and lobular proliferation type [31 cases of usual ductal hyperplasia (UDH), 5 cases of atypical ductal hyperplasia (ADH), 54 cases of ductal carcinoma in situ (DCIS) and 10 cases of lobular carcinoma in situ (LCIS)]. Peripheral myoepithelial cell labeling was not taken into account
Comparative immunostainings with D5/16 B4 (anti CK5/6, right side) and 34βE12 (anti-CK1/5/10/14, left side) antibodies. Ductal hyperplasia (A and A', ×200): immunostaining of epithelial and myoepithelial cells is quite similar with the two antibodies. Atypical ductal hyperplasia (B and B', ×100): some proliferative epithelial cells are weekly stained by 34βE12 mAb, while only residual normal cells are stained by D5/16B4 mAb. Ductal carcinoma in situ (C and C', ×200) and lobular carcinoma in situ (D and D', ×200): immunostaining of several carcinomatous cells with 34βE12 but not with D5/16B4 mAb. Residual entrapped normal cells are strongly marked with both antibodies
Ductal carcinoma in situ
The results of the DCIS immunostainings are summarized in Fig. 1. All 54 cases of DCIS showed less than 51% of CK5/6 stained cells (Fig. 1). However, the labeled cells seem to be residual normal cells, as they were easily distinguished from tumoral cells according to their different morphological features (Fig. 2). Indeed, labeled cells were flattened and showed no cytological atypia. Moreover, they were often lifted by carcinomatous cells from the basal myoepithelial layer, as in a pagetoid pattern. Therefore, taking these distinctive and previously described features [14, 15] into account, careful microscopic examination showed that no carcinomatous cell was labeled by CK5/6 mAb in all DCIS cases (Fig. 3).
Comparative percentage results of CK5/6 and 34βE12 neoplastic labeled cells according to the mammary ductal and lobular proliferation type [31 cases of usual ductal hyperplasia (UDH), 5 cases of atypical ductal hyperplasia (ADH), 54 cases of ductal carcinoma in situ (DCIS) and 10 cases of lobular carcinoma in situ (LCIS)]. Residual entrapped normal cell labeling was not taken into account
In contrast, in addition to residual cells, a large proportion of carcinomatous cells were stained by 34βE12 mAb in DCIS cases (Fig. 1 and Fig. 3). These cells were moderately labeled in comparison with the intense staining observed in residual cells. More than 50% of labeled cells were observed in ten cases, and a very strong reaction (more than 70% of stained cells) was observed in four of the cases (Fig. 3). The 34βE12 immunostaining results did not differ according to the Van Nuys grade (Fig. 4).
Atypical ductal hyperplasia
The results of the ADH immunostainings are summarized in Fig. 1. All five cases of ADH showed less than 50% of CK5/6 stained cells. The staining concerned 30% of cells in one case and was very patchy (less than 5% of stained cells) in four cases. Not surprisingly, the labeled cells in these four cases shared the same morphological features as the residual cells in DCIS. They were often isolated and lifted by negative cells (Fig. 2).
Four cases of the ADH showed less than 50% of 34βE12 stained cells, while more than 50% of labeled cells were observed in one case. These results were similar to those obtained in the DCIS cases.
Lobular carcinoma in situ
The results of the LCIS immunostainings are summarized in Fig. 1 and Fig. 3. The CK5/6 immunostaining pattern was most often characterized by nonreactive neoplastic cells, sometimes surrounded by immunoreactive nonneoplastic residual cells in the ductal extension of the lesion (Fig. 2). Therefore, none of the LCIS showed CK5/6 immunostaining.
In contrast, 34βE12 mAb labeled more than 50% of the cells in most of the LCIS (eight) cases. The staining was weak-to-moderate and cytoplasmic in a perinuclear pattern.
Discussion
Normal breast epithelium is a "mixed" bistratified glandular epithelium composed of three populations of cells, i.e., glandular-type epithelial, basal-type epithelial and myoepithelial cells. Earlier immunohistochemical reports provided evidence that each UDH is composed of a biphasic population, one type associated with simple-epithelium keratins, the other associated with basal-type keratins. In contrast, most DCIS and ADH cases have been reported to be composed of a predominantly or exclusively monophasic population of cells expressing simple-epithelium type keratins; but, in a minority of cases, tumoral cells expressed basal-type CK [3, 9, 11, 13, 14, 15, 28].
The majority of previous studies of the basal-type CK in in situ breast lesions used antibodies directed against at least the CK14 or CK17 [2, 3, 11, 13, 15, 28]. Antibody directed against CK5 (clone D5/16 B4) without cross reactivity against CK14 or CK17 has been rarely used [14].
The present study is the first to evaluate the practical value of CK5/6 expression in in situ epithelial breast lesions as a comparative study with 34βE12 mAb. The pattern of reactivity of CK5/6 mAb in normal breast was not exactly the same as that of 34βE12 mAb. Both antibodies reacted with some epithelial and myoepithelial cells in normal ducts and lobules as previously described for 34βE12 mAb. However, this later antibody labeled more cells in the inner layer of the ductal epithelium. Therefore, one can hypothesize that CK5/6 mAb is less sensitive for the basal cell detection than 34βE12 mAb. Another explanation could be that 34βE12 mAb not only labels basal cells, but also some glandular cells that express CK14 but not CK5/6, leading to this immunostaining discrepancy.
The present results demonstrate that CK5/6 is strongly expressed in all cases of UDH (31 of 31). This result is in agreement with that we obtained with 34βE12 mAb and those previously reported in the literature [2, 11, 13, 15, 28]. This result also demonstrates that most of the cells in UDH have a true basal-cell immunophenotype, not only due to CK14 but also to CK5 or, less probably, to CK6.
In contrast, CK5/6 and 34βE12 immunostainings were significantly different in atypical/malignant in situ lesions. CK5/6 immunostaining was negative, while 34βE12 mAb labeled more than 50% of cells in 31% of atypical/malignant lesions.
Our results with 34βE12 mAb in ADH/DCIS appear higher than those of previous studies performed using 34βE12 mAb [13, 15, 23]. One can attribute this discrepancy to technical parameters such as antibody dilution or the type of fixative used. Indeed, in our study, the staining intensity was most often low in these lesions, even if the percentage of labeled cells was high (Fig. 2). This staining might not have been detected if a higher antibody dilution had been used. The different fixatives used could also partially explain our results, but no modification of the pattern of staining was observed with regard to the fixative used. However, the staining was a specific one, as negative controls were not labeled without background staining.
CK5/6 immunostaining appears to be much more specific than the 34βE12 immunostaining in distinguishing between UDH and ADH/DCIS/LCIS. Thus, this antibody can be helpful in differential diagnosis between UDH and ADH/DCIS/LCIS when cyto-architectural diagnosis is difficult. CK5/6 use allows for a more simple approach than those used in a recent study to improve 34βE12 mAb specificity, which combined percentage of labeled cells and staining intensity [13].
ADH lesions share similar CK5/6 and 34βE12 immunophenotype with DCIS. The diagnosis of ADH was made according to Tavassoli's criteria, i.e., when the lesions displayed cyto-architectural aspects similar to DCIS but were lower than 2 mm in diameter, or when the cells displayed atypia but did not fulfill all the DCIS criteria [26]. The "DCIS-like" immunophenotype of the ADH cells and the loss of the biphasic population suggests a common pathogenetic mechanism with DCIS, leading to basal-type keratin loss and clonal proliferation. In these particularly difficult-to-recognize lesions, CK5/6 immunostaining appears to be a very helpful tool.
For the first time, we report here the immunostaining of LCIS using 34βE12 and CK5/6 mAbs. The LCIS CK5/6 immunophenotype was close to that of DCIS, implying that CK5/6 mAb cannot be used to distinguish solid variant of low-grade DCIS that mimics LCIS from true LCIS. And yet these lesions, which have overlapping ductal and lobular morphological features, must be separated, as they have different clinical implication. Interestingly, we frequently observed more than 50% of 34βE12 immunostained cells in LCIS. This important 34βE12 mAb labeling was much more frequent in LCIS (8 of 10 cases) than in DCIS (24% of the cases). These results are in accordance with those of Bratthauer et al. (2002), which have demonstrated that lobular lesions show cytoplasmic reactivity with 34βE12 mAb, often in a perinuclear pattern, and lack any immunoreactivity for E-cadherin [5]. Bratthauer et al., therefore, suggested that the combination of 34βE12 and E-cadherin mAbs could be useful in distinguishing lobular and ductal lesions that have overlapping morphological features [5].
One may infer that the most frequent staining observed with 34βE12 mAb in DCIS and LCIS lesions is due to CK14 detection. Previous studies that used other antibodies have shown that CK14 expression signifies the worst prognosis in infiltrative carcinomas [6, 12, 16]. Further studies are needed to evaluate the prognostic value of 34βE12 mAb staining in in situ lesions.
In conclusion, anti-CK5/6 mAb appears to be a new, very sensible and specific tool to assist in the differential diagnosis between benign and malignant in situ epithelial proliferations of the breast—far more specific than the 34βE12 mAb.
References
Bodian CA, Perzin KH, Lattes R, Hoffman P, Abernathy TG (1993) Prognostic significance of benign proliferative breast disease. Cancer 71:3896–3907
Boecker W, Bier B, Freytag G, Brommelkamp B, Jarasch ED, Edel G, Dockhorn-Dworniczak B, Schmid KW (1992) An immunohistochemical study of the breast using antibodies to basal and luminal keratins, alpha-smooth muscle actin, vimentin, collagen IV, and laminin. Part I: normal breast and benign proliferative lesions. Virchows Arch 421:315–322
Boecker W, Bier B, Freytag G, Brommelkamp B, Jarasch ED, Edel G, Dockhorn-Dworniczak B, Schmid KW (1992) An immunohistochemical study of the breast using antibodies to basal and luminal keratins, alpha-smooth muscle actin, vimentin, collagen IV, and laminin. Part II: epitheliosis and ductal carcinoma in situ. Virchows Arch 421:323–330
Boecker W, Buerger H, Schmitz K, Ellis IA, Van Diest PJ, Sinn HP, Geradts J, Diallo R, Poremba C, Herbst H (2001) Ductal epithelial proliferations of the breast: a biological continuum? Comparative genomic hybridization and high-molecular-weight cytokeratin expression patterns. J Pathol 195:415–421
Bratthauer GL, Moinfar F, Stamatakos MD, Mezzetti TP, Shekitka KM, Man YG, Tavassoli FA (2002) Combined E-cadherin and high molecular weight cytokeratin immunoprofile differentiates lobular, ductal, and hybrid mammary intraepithelial neoplasias. Hum Pathol 33:620–627
Dairkee SH, Mayall BH, Smith HS, Hackett AJ (1987) Monoclonal marker that predicts early recurrence of breast cancer. Lancet 1:514
Dairkee SH, Puett L, Hackett AJ (1988) Expression of basal and luminal epithelium-specific keratins in normal, benign, and malignant breast tissue. J Natl Cancer Inst 80:691–695
Dupont WD, Parl FF, Hartmann WH, Brinton LA, Winfield AC, Worrel JA, Schuyler PA, Plummer BS (1993) Breast cancer risk associated with proliferative breast disease and atypical hyperplasia. Cancer 71:1258–1265
Guelstein VI, Tchypysheva TA, Ermilova VD, Litvinova LV, Troyanovski SM, Bannikov GA (1988) Monoclonal antibody mapping of keratins 8 and 17 and of vimentin in normal human mammary gland, benign tumors, dysplasias and breast cancer. Int J Cancer 42:147–153
Heatley M, Maxwell P, Whiteside C, Toner P (1995) Cytokeratin intermediate filament expression in benign and malignant breast disease. J Clin Pathol 48:26–32
Jarasch ED, Nagle RB, Kaufmann M, Maurer C, Böcker WJ (1988) Differential diagnosis of benign epithelial proliferations and carcinomas of the breast using antibodies to cytokeratins. Hum Pathol 19:276–289
Malzahn K, Mitze M, Thoenes M, Moll R (1998) Biological and prognostic significance of stratified epithelial cytokeratins in infiltrating ductal breasts carcinomas. Virchows Arch 433:119–129
Moinfar F, Man YG, Lininger RA, Bodian C, Tavassoli FA (1999) Use of keratin 34βE12 as an adjunct in the diagnosis of mammary intraepithelial neoplasia-ductal type benign and malignant intraductal proliferations. Am J Surg Pathol 23:1048–1058
Otterbach F, Bànkfalvi A, Bergner S, Decker T, Krech R, Boecker W (2000) Cytokeratin 5/6-immunohistochemistry assists the differential diagnosis of atypical proliferations of the breast. Histopathology 37:232–240
Raju U, Crissman JD, Zarbo RJ, Gottlieb C (1990) Epitheliosis of the breast: an immunohistochemical characterization and comparison to malignant intraductal proliferations of the breast. Am J Surg Pathol 14:939–947
Santini D, Cecarelli C, Taffurelli M, Pileri S, Marrano D (1996) Differentiation pathways in primary invasive breast carcinoma as suggested by intermediate filament and biopathological marker expression. J Pathol 179:386–391
Schnitt SJ, Connoly JL, Tavassoli FA, Fechner RE, Kempson RL, Gelman R, Page DL (1992) Interobserver reproducibility in the diagnosis of ductal proliferative breast lesions using standardized criteria. Am J Surg Pathol 16:1133–1143
Schwartz GF, Solin LJ, Olivotto IA, Ernster VL, Pressman PI, and the consensus conference committee (2000) The consensus conference on the treatment of in situ ductal carcinoma of the breast, 22–25 April 1999. Hum Pathol 31:131–138
Shi SR, Key ME, Kalra KL (1991) Antigen retrieval in formalin-fixed, paraffin-embedded tissues: an enhancement method for immunohistochemical staining based on microwave oven heating of tissues sections. J Histochem Cytochem 39:741–748
Shoker BS, Sloane JP (1999) DCIS grading schemes and clinical implications. Histopathology 35:393–400
Silverstein MJ, Poller DN, Waisman JR (1995) Prognostic classification of breast ductal carcinoma in situ. Lancet 345:1154–1157
Sloane JP, Ormerod MG (1981) Distribution of epithelial membrane antigen in normal and neoplastic tissues and its value in diagnostic tumor pathology. Cancer 47:1786–1795
Soini Y, Miettinen M (1992) Immunohistochemical evaluation of the cytoarchitecture of benign and malignant breast lesions. APMIS 100:901–907
Tavassoli FA (1999) Pathology of the breast. Appleton and Lange, Stanford, Connecticut
Tavassoli FA, Man Y (1995) Morphofunctional features of intraductal hyperplasia, atypical intraductal hyperplasia and various grades of intraductal carcinoma. Breast J 1:155–162
Tavassoli FA, Norris HJ (1990) A comparison of the results of long-term follow-up for atypical intraductal hyperplasia and intraductal hyperplasia of the breast. Cancer 65:518–529
Viacava P, Naccarato AG, Bevilacqua G (1999) Different proliferative patterns characterize different preinvasive breast lesions. J Pathol 188:245–251
Wetzels RHW, Kuijpers HJH, Lane EB, Leigh IM, Troyanovsky SM, Holland R, van Haelst UJGM, Ramaekers FCS (1991) Basal cell-specific and hyperproliferation-related keratins in human breast cancer. Am J Pathol 138:751–763
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lacroix-Triki, M., Mery, E., Voigt, JJ. et al. Value of cytokeratin 5/6 immunostaining using D5/16 B4 antibody in the spectrum of proliferative intraepithelial lesions of the breast. A comparative study with 34βE12 antibody. Virchows Arch 442, 548–554 (2003). https://doi.org/10.1007/s00428-003-0808-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-003-0808-0