Abstract
Purpose
The purpose of the present study was to explore the risk for complications and reoperations following open repairs for sliding groin hernias.
Method
All primary indirect inguinal hernia repairs registered in the Swedish Hernia Register 1998–2011 were identified. Repeated and bilateral procedures were excluded. The epidemiology, the incidence of per- and postoperative complications, and the reoperation rate due to recurrences were analyzed.
Results
100 240 non-repeated unilateral repairs were registered with sliding hernias in 13 132 (13.1 %) (male 14 %, female 5 %) procedures. The methods of repair for sliding and non-sliding hernias were Lichtenstein and other open anterior mesh repairs (N = 10865, 82.7 % and N = 60790, 69.8 %), endoscopic techniques (N = 136, 1.0 % and N = 4352, 5.0 %), and other techniques (N = 2131, 16.2 % and N = 21966, 25.2 %). In multivariate analyses with adjustment for gender, acute/planned surgery, reducibility, method of repair and age, sliding hernias were associated with a low but slightly increased risk for perioperative complications (hazard ratio 1.30, 95 % confidence interval 1.04–1.62, p = 0.023) and postoperative hematoma (hazard ratio 1.13, confidence interval 1.02–1.26, p = 0.019). There was no increased risk of reoperation due to recurrences.
Conclusion
Compared to older reports, the incidence of repairs due to primary indirect sliding inguinal hernias has increased over time and it is not just a male disease. The overall results are good with low and comparable complication rates, and no increased risk of reoperations due to recurrences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal hernia is one of the most common conditions requiring surgical treatment. Sliding hernias constitute a part of the inguinal hernias, by some considered to be among the more difficult ones to repair. A sliding inguinal hernia is defined as a protrusion of a retroperitoneal organ (viscus) through an opening in the inguinal part of the abdominal wall [1]. In clinical praxis, this means that at least part of the hernial sac is made up by the viscus or its mesentery including the blood supply [1]. Although the sigmoid colon is the most common sliding organ many others have been reported so far including the cecum, appendix, urinary bladder, ureters, and female reproductive organs [1]. The recommended repair techniques have varied a lot over time [2–11].
Most publications on this subject have been case reports or reports on small series [2, 3, 5–7, 12, 13]. Since the mid 1900s, some publications with results based on larger series of repair of sliding inguinal hernias have been published [1, 11, 14–21]. At least five of them emanate from the Shouldice clinic and probably at least some of the repairs are included in several publications [1, 15, 18, 20, 21]. In other publications on large series of inguinal hernia repairs, one can also find data on the subject of sliding hernias [22]. The role of the different laparoscopic repair techniques in surgery sliding inguinal hernia has been explored [23]. In a recent report from Denmark [24], endoscopic techniques were found to be feasible and safe for sliding hernias.
The limited number of modern studies focusing on sliding inguinal hernias motivates the present study. The first aim is to report the complication rate, the occurrence of a perioperative bowel resection, and the cumulative incidence of reoperations due to recurrences after primary indirect sliding inguinal hernia repair (PISIHR), in a nationwide register not dominated by surgery performed at specialized centers. The second aim is to analyze the incidence and characteristics of PISIHR in a population based cohort. Finally, the third aim is to analyze the incidence and outcome following surgery for PISIHR in women.
Methods
The present study is based on data from the Swedish Hernia Register (SHR) (www.svensktbrackregister.se) [25]. The SHR was founded in 1992. Since then, it has gradually grown and today it covers more than 98 % of all groin hernia repairs performed on patients ≥15 years of age, in Sweden. At the time of the study, 253,625 repairs had been included in the SHR. The register includes data on the patient, the hernia, the repair technique, and complications to the repair. Among these parameters, the presence of a sliding hernia is recorded in the register (yes/no). The register continuously validates its data. Because every Swedish citizen can be traced by their unique personal registration number, any further groin hernia repair on the same patient, performed in Sweden, can be traced.
All registered repairs due to a primary indirect inguinal hernia, performed between 1998 and 2013, were identified. Since the register had not reached the present coverage of more than 98 %, procedures performed before 1998 were not included. In a second selection procedure, simultaneous bilateral repairs and repeated primary indirect inguinal hernia repairs on the same patient’s opposite side were excluded. These procedures were excluded in order to avoid the potential bias caused by repeated procedures on the same individual, which would have resulted in a relative predominance of factors related to individuals undergoing more than one procedure. Simultaneous bilateral repairs were omitted in order to avoid confusion between operated side and subsequent complications. Indirect hernias in combination with direct or femoral hernias were also excluded.
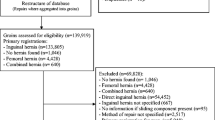
The study cohort was analyzed for epidemiology, complications, and reoperations due to recurrences. The study group consisted of those with an affirmed sliding hernia, and the control group consisted of those where a sliding hernia was negated. A flowchart summarizing the selection process is shown in Fig. 1. The patients were analyzed regarding age, gender, ASA classification, and body mass index (BMI). The hernias were analyzed regarding side, occurrence of a sliding component, and reducibility. The surgeons were analyzed regarding annual volume (≤25 procedures/year versus >25 procedures/year). The operations were analyzed regarding method of repair, emergency or elective operation, occurrence of bowel resection, and perioperative complications. The postoperative complications were analyzed after being divided in two groups (30-day postoperative complications and reoperations due to recurrences). Univariate analyses were used for comparing the two groups. Risk factors for a bowel resection or a postoperative complication were further analyzed with two separate multivariate logistic regression analyses. In the regression analyses, all plug repairs, posterior mesh repairs, and incompletely defined repairs were excluded.
For categorical data, absolute numbers in addition to percentages are given. A probability level of a random difference of P less than 0.05 was considered significant. All analyses were performed with R, version 3.1.0 (2014-04-10).
Results
The total number of primary indirect inguinal hernia repairs identified in the register between 1998 and 2013 was 116,790. The presence of a sliding hernia was affirmed or denied in 111,910 (95.8 %). In the second selection procedure, 6772 simultaneous bilateral repairs and 4898 repeated primary indirect inguinal hernia repairs on the same patient’s opposite side were excluded. The remaining 100,240 were used for further analyses. The baseline epidemiological data on these patients and their hernias also including data regarding the repairs, the surgeons, and the complications are shown in Table 1.
The univariate analysis showed that perioperative complications and bowels resections were more common among those with PISIHR. However, in the multivariate analyses, PISIHR was not a significant risk factor for bowel resection. The postoperative complications among the PISIHR:s were slightly more common in some subgroups regarding the univariate analyzes but not in the multivariate analyzes regarding the same subgroups (Table 2).
The overall reoperation rate due to recurrences (after >30 days) was 1697 (1.95 %) for non-sliding hernias and 247 (1.88 %) for sliding hernias (Fig. 2). The difference was not found to be statistically significant in either a univariate Cox proportional hazard analysis, (hazard ratio 0.90, 95 % confidence interval 0.90–1.18, p = 0.621) or a multivariate analysis with adjustment for gender, acute/planned surgery, reducibility, method of repair, and age (hazard ratio 0.97, 95 % confidence interval 0.84–1.12, p = 0.670). Patients with missing data on BMI or ASA had significantly greater risk of subsequent re-operation (p < 0.05), but there was no significant association with lack of data on surgeon.
Discussion
In most cases, surgery for sliding hernias can be performed without substantial over-risk of complications. There was, however, numerically low, a slightly increased risk for perioperative complications. We consider this could be related to the fact that the study group included more elderly and obese patients with increased ASA-score and more acute repairs. Subgroup analysis of the perioperative complications could not be performed since the register routines changed over the time period.
In the univariate analyses, bowel resections were more common among the PISIHR, but it was not related to whether the hernias were non-reducible or if it was an emergency surgery repair. Thereby, inability to recognize a sliding hernia and accidental perioperative intestinal damage can be one explanation. On the other hand, the incidences of perioperative bowel resections are numerically very low in both groups. Nowadays, the thought of sliding hernias as the dangerous hernias seems to be an overstatement. We suggest that the Swedish education program has increased the awareness for sliding hernias and the knowledge of the best way to repair such hernias. Sliding hernias are in general considered as difficult, requiring experienced surgeons. The percentage of procedures performed by surgeons with high annual volume of hernia surgery was, however, lower in the sliding hernia group than in the non-sliding hernia group.
The incidences of a postoperative complication were very low and did not differ significantly between sliding or non-sliding hernia repairs. When sub-grouping the postoperative complications, only some minor differences were found. We do not think that these minor differences indicate a clinically important over-risk to be paid special attention. In contrast to some older reports [3, 6, 11, 19, 20, 26], we did not find that the presence of a sliding hernia increased the risk of serious complications. This is in agreement with more recent large studies [15, 18, 22].
When performing a search on PubMed (www.ncbi.nlm.nih.gov/pubmed) using the key words (inguinal hernia), one will find more than 13,000 publications. When using the key words (sliding) and (inguinal hernia), there were less than 130 publications (1 ‰). This low number, published over more than one decade, shows that the knowledge on this subject needs to be improved.
The number of operations included in this report, is to our knowledge, by far the largest presented. The incidence of PISIHR in our report was >12 % of all primary indirect inguinal hernia repairs. This incidence is larger than found in the three reports from the Shouldice clinic [15, 18, 21] and in the report from Lichtenstein [22]. A possible explanation could be a tendency to over-diagnose sliding hernias. However, our cohort is, in opposite to those mentioned above, not selected. In the previous reports [15, 18, 21, 22], almost all patients were operated under local anesthesia, and it is well known that the really obese patients are not well suited for that method. In the group of obese patients, the incidence of PISIHR is known to be higher [1]. Contrary to the other reports, we do not include operations performed on children and thereby the incidence in our report may be expected to be higher. The three Shouldice reports partly included the same patients with more added in the later reports [15, 18, 21]. The incidence in the studies increased over time from 1951 to 1967 [15, 18, 21]. In the present report, the operations procedures are performed 32–66 years later and during that time the prevalence of obesity has increased substantially [27, 28]. The newly published report from the world’s second largest hernia register [24] also showed a high incidence of almost 9 %. In Sweden, as well as in most other European countries, opening, inspection, and resection of an indirect inguinal hernial sac are the common methods in anterior repairs. Thereby, a lot of indirect inguinal hernias with a small sliding component are diagnosed. In those clinics and countries where invagination without opening and resection of the indirect inguinal hernial sac is the method of choice, the diagnosed incidence of sliding hernias is presumed to be lower. Altogether, this can at least partly explain the higher incidence we have found. In contrast to the previous Danish study, sliding hernias were not associated with an increased recurrence rate. The reason for this difference is difficult to explain.
The presence of sliding inguinal hernias in females is very scarcely reported and almost never discussed. Among all the reports discussed in this publication, only four mention female cases of inguinal sliding hernias [16, 21, 24, 29]. At least in three of these four reports, the females were grownups, and the sliding inguinal hernias were defined as indirect [16, 24, 29] also in the fourth, the sliding inguinal hernias were defined as indirect but the age of the patients were not noted [21]. When researching PubMed using the key words (female), (inguinal), and (sliding hernia), we have found two more case reports on this subject in grown up females [30, 31]. Altogether, these six reports [16, 21, 24, 29–31] strengthen our finding that primary indirect sliding inguinal hernias can be found in grown up females and that they are more common than earlier presumed. This should be taken into consideration by all surgeons repairing groin hernias in women. In the latest guideline from the European Hernia Society [32], it is stated that groin hernias in females are best repaired by placing a mesh in the preperitoneal space (the space of Bogros). By following this recommendation, the surgeon always deals with the problem of the femoral hernias that are much more common in women (24 %). On the other hand, it will be even more difficult to further study the existence of sliding groin hernias in women since the hernial sac is not routinely explored when in the endoscopic and open anterior approaches. Transabdominal preperitoneal repair (TAPP), however, enables inspection of the hernia sac from the inside of the hernia sac and may be advantageous in the presence of a sliding hernia. As TEP is the dominating endoscopic technique in Sweden and TAPP is only rarely used, we were not able to assess the safety of this approach for sliding hernias.
Sliding hernias are often considered as a problem related mostly to indirect hernias. However, the prevalence of direct sliding hernias is unsure since during such a repair, the hernia sac is usually not opened and inspected from inside. Due to this reason, direct-sliding hernias are not studied and discussed in this publication. The TAPP technique implies exploration of the hernia sac in direct hernias as well, but was only scarcely used during the period of study.
The increased prevalence with high age, obesity, and a left-sided hernia was more common among patients with PISIHR is in accordance with the only large, detailed, previously published study [18] dealing with all these three characteristics. The finding that emergency hernia repairs were more common in the PISIHR-group is in accordance with the study from Denmark [24]. For our other findings that non-reducible hernias were more common in the PISIHR-group, comparisons cannot be done.
In this study, the reoperation incidences due to recurrences were almost identical between the two groups. This is not in accordance with the Danish study [24]. We suggest that the good results regarding the reoperation incidence can at least partly be explained by the increased national education on groin hernia surgery. To some extent, however, the differences between the present study and the previous Danish one may be the higher proportion of procedures with a sliding hernia than the Danish study. This study may have included more hernias with small-sliding hernia components that would have been overlooked if the hernia sac would not have been explored before resection. This could have resulted in a relatively greater preponderance of minor sliding components.
The diagnose of an indirect sliding inguinal hernia is in most cases clinical, i.e., it is diagnosed during the repair of an inguinal hernia [18]. There are at least two reasons why indirect sliding inguinal hernias are considered more difficult and dangerous to repair than other inguinal hernias. The first reason is the difficulty in recognizing a sliding hernia when dissecting the sac, especially if the hernia is non-reducible. Thereby, there is a risk of injuring the slided viscus or its blood supply when dissecting the sac, especially when using repair techniques where the sac is to be resected. The second reason is if the surgeon does not have the knowledge of how to repair a sliding hernia. A complete reposition of the hernia sac or at least the viscus forming part of it is necessary to achieve a hernia repair of acceptable quality and without an increased risk of complications related to the repair.
Among the repair methods used in our report, the Lichtenstein repair method dominates like it has in Sweden for the last 12 years [25]. Notably, the frequency of the endoscopic methods used is very low. This is probably explained by the fact that even many experienced endoscopic hernia surgeons are reluctant to repair large or irreducible hernias by endoscopy. These surgeons are also more common in day-surgery clinics that do not perform emergency surgery.
As BMI and ASA were not registered the first years, there was relatively large proportion of patients with missing data in the group with the longest follow-up. This probably also explains the higher re-operation rate in this group.
Large randomized studies on this subject are not available. To analyze prospectively registered data on large cohorts is for the moment the best way to gain more evidence on this subject. The strength of this register study is that since SHR covers almost all groin hernia repairs performed on grown-ups in Sweden, there are large normal variations within the cohort and the risk of selection is minimal. Despite its possibilities, a register study has its limitations. A possible weakness of this study is the risk of a tendency to over-diagnose sliding hernias. This could have diminished the result. We do not know if all surgeons have been well aware of the correct criteria for sliding hernias. On the other hand, nowadays, the outcome of groin hernia repairs in Sweden is mainly based on high and medium volume centers [33]. Regarding the reoperation incidence, one should also bear in mind, that in a validation study, the recurrence rate has been shown to be approximately twice as high [34].
In conclusion, the incidence of PISIHR has increased over time, and sliding inguinal indirect hernia is not just a male disease. The overall results are good with low and comparable complication rates and no increased risk of reoperations due to recurrences. Further studies on this subject are needed also for women. The incidence of PISIHR is theoretically high enough for randomized studies but the problem with recognizing this entity among all groin hernias preoperatively remains a problem when designing such studies. Perhaps meticulous modern repair techniques and improved education are good enough to improve the results and to motivate further studies only on a retrospective basis like register studies.
References
Bendavid R (2002) Sliding hernias. Hernia 6:137–140
Hotchkiss LW (1909) VI. Large sliding hernias of the sigmoid: with a description of an operation for their relief. Ann Surg 50:470–473
Moschcowitz AV (1925) The rational treatment of sling hernia. Ann Surg 81:330–334
Laroque GP (1924) An improved method of removing hernia from within. Ann Surg 79:375–381
Bevan AD (1930) Sliding hernias of the ascending colon and caecum, the descending colon and sigmoid, and of the bladder. Ann Surg 92:754–760
Graham RR (1935) The operative repair of sliding hernia of the sigmoid. Ann Surg 102:784–792
Mackid LS (1936) Inguinal hernia: with special reference to sliding hernia and a new treatment. Can Med Assoc J 34:269–271
Williams C (1947) Repair of sliding inguinal hernia through the abdominal (LaRoque) approach. Ann Surg 126:612–623
Zimmerman L, Laufman H (1942) Sliding hernia. Surg Gynecol Obstet 75:76–78
Hallen M, Westerdahl J, Nordin P, Gunnarsson U, Sandblom G (2012) Mesh hernia repair and male infertility: a retrospective register study. Surgery 151:94–98
Gaspar MR, Joergenson EJ, Woolley MM (1956) Sliding indirect inguinal hernia. Calif Med 85:330–334
Ponka JL (1966) Surgical management of large bilateral indirect sliding inguinal hernias. Am J Surg 112:52–57
Komorowski AL, Moran-Rodriguez J, Kazi R, Wysocki WM (2012) Sliding inguinal hernias. Int J Surg 10:206–208
Adams RA, Wysocki AP (2010) Outcome of sliding inguinal hernia repair. Hernia 14:47–49
Glassow F (1965) High ligation of the sac in indirect inguinal hernia. Am J Surg 109:460–463
Piedad OH, Stoesser PN, Wels PB (1973) Sliding inguinal hernia. Am J Surg 126:106–107
Ponka JL, Brush BE (1978) Sliding inguinal hernia in patients over 70 years of age. J Am Geriatr Soc 26:68–73
Ryan EA (1956) An analysis of 313 consecutive cases of indirect sliding inguinal hernias. Surg Gynecol Obstet 102:45–58
Sensenig DM, Nichols JB (1955) Sliding hernias; a follow-up study. AMA Arch Surg 71:756–760
Shouldice EE (1953) The treatment of hernia. Ont Med Rev 20:670–684
Welsh D (1969) Repair of the indirect sliding hernias. J Abdom Surg 11:204–209
Lichtenstein IL (1987) Herniorrhaphy. A personal experience with 6,321 cases. Am J Surg 153:553–559
Patle NM, Tantia O, Prasad P, Khanna S, Sen B (2011) Sliding inguinal hernias: scope of laparoscopic repair. J Laparoendosc Adv Surg Tech A 21:227–231
Andresen K, Bisgaard T, Rosenberg J (2015) Sliding inguinal hernia is a risk factor for recurrence. Langenbeck’s Arch Surg 400:101–106
SHR. Available from: http://www.svensktbrackregister.se/ Accessed 8 May 2014
Stoesser PN, Piedad OH (1969) Simplified method for repair sliding inguinal hernia. Am J Surg 118:472–474
WHO. Available from: http://www.who.int/gho/ncd/risk_factors/obesity_text/en/ Accessed 9 Dec 2013
Parikh NI et al (2007) Increasing trends in incidence of overweight and obesity over 5 decades. Am J Med 120:242–250
Maingot R (1961) Operations for sliding herniae and for large incisional herniae. Br J Clin Pract 15:993–996
Gurer A et al (2006) Uncommon content in groin hernia sac. Hernia 10:152–155
Ozkan OV et al (2009) A right sliding indirect inguinal hernia containing paraovarian cyst, fallopian tube, and ovary: a case report. Arch Gynecol Obstet 279:897–899
Simons MP et al (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403
Nordin P, van der Linden W (2008) Volume of procedures and risk of recurrence after repair of groin hernia: national register study. BMJ 336:934–937
Haapaniemi S, Nilsson E (2002) Recurrence and pain three years after groin hernia repair. Validation of postal questionnaire and selective physical examination as a method of follow-up. Eur J Surg 168:22–28
Acknowledgments
The authors would like thank all Swedish groin hernia surgeons who assembled the data in the SHR. Presented in part as an abstract and a speech at the Swedish Surgical Society, 17th Surgical week, Linköping, Sweden, August 20–24, 2012.
Author’s contributions
Gabriel Sandblom, Dan Sevonius, and Magnus Hallén designed the study.
Henrik Holmberg was responsible for data acquisition and analysis.
Magnus Hallén drafted the manuscript together with Gabriel Sandblom and Dan Sevonius.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The SHR is supported financially by the National Board of Health and Welfare, the Swedish Association of Local Authorities, and the County Council of Jämtland. This study was supported by grants from the Anders Borgström Fellowship and the Olle Engqvist Research Foundation. The authors declare no other conflicts of interest.
Research involving human participants and/or animals
All procedures were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments. The study was approved by the Umeå Ethics Review Board.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Hallén, M., Sevonius, D., Holmberg, H. et al. Low complication rate and an increasing incidence of surgical repair of primary indirect sliding inguinal hernia. Langenbecks Arch Surg 401, 215–222 (2016). https://doi.org/10.1007/s00423-016-1392-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-016-1392-5