Abstract
Purpose
Sliding inguinal hernias represent a small proportion of inguinal hernias but become more common with advancing age. The most recent review is based on a series published over 50 years ago. There are, however, many case reports of unusual presentations in girls.
Methods
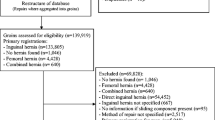
We performed a review of a prospectively kept electronic record of all operations performed at Logan Hospital since 2003 in order to document the clinical characteristics of sliding inguinal hernias in the twenty-first century.
Results
Thirty-one males underwent predominantly anterior repair of a sliding hernia after a median of 9 months of symptoms (2.9% of all hernia repairs—32/1,092). Approximately two-thirds of hernias were left sided. There were five minor and two technical complications. Follow-up ranged from 3 weeks to 3 years. Two recurrences have been repaired.
Conclusions
Sliding inguinal hernias continue to test the surgeon’s understanding of the inguinal canal’s anatomy and technical expertise with a significant rate of technical complications and recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-operative management of inguinal hernia was described in Babylon as far back as 1700 BC [1]. Currently, inguinal hernia repair is one of the most common procedures performed by general surgeons. The operative technique has evolved remarkably over the last 125 years but, surprisingly, very little is published regarding this uncommon type of inguinal hernia.
The 5-year reoperation rate for recurrence after primary elective inguinal hernia repair is between 3 and 7% depending on the type of repair [2]. Direct and indirect hernias occur with almost equal frequency (46 and 54% out of 43,043 mesh repairs, respectively) but most recurrences after anterior hernia repair are directs [3]. However, no mention is made of the fate of sliding hernias in this latter paper. An article by Bendavid represents the most recent review on adult sliding inguinal hernias but is based on publications from the 1950s and 1960s [4]. Recent publications are predominantly case reports in girls [5]. We wanted to describe the characteristics of adult patients with sliding hernias in the twenty-first century (Table 1).
Methods
The surgical department at Logan Hospital has maintained an electronic record (Microsoft Excel license held by Queensland Health) of all operations (and complications) performed since 2003. Each operation note was searched for the term sliding inguinal hernia. The operative findings (side, sac composition, type of repair) were recorded. Preoperative symptoms and complications were noted. Literature was identified by using Medline with PubMed as the search engine.
Results
Thirty-two sliding inguinal hernias were repaired between January 2003 and October 2008 in 31 patients. All patients were male with a median age of 62 years (range 26–86 years). The duration of preoperative symptoms was recorded in 21 patients (median 9 months, mean 16 months). Median post-operative length of stay was 1 day (mean 1.2; range 0–4). Twenty-five operations were elective and six emergency. There were no instances of strangulation. Twenty-eight sliding hernias were diagnosed at time of unilateral hernia repair and four at bilateral. Thirty patients had a unilateral sliding hernia and one patient had bilateral sliding hernias. Twenty indirect hernias were on the left (63%) and 12 indirects on the right (37%). Hernial sac composition was not recorded in 15 patients (6 on left, 8 on right and the 1 patient with bilateral sliding hernias). Otherwise, 13 were formed by the sigmoid colon, 2 ileocaecal segment and 1 bladder. The 31 open repairs were split evenly between Lichtenstein (16) and Perfix plug-and-patch (15). One patient underwent primary totally extra peritoneal (TEP) repair. Thirty hernias were primary and two represented recurrence (one on each side). The level of detail recorded in the operation note varied significantly from patient to patient.
Six of the 31 patients did not have preoperative symptoms recorded. Four patients presented with groin discomfort only. Twenty-one presented with a groin lump (7 enlarging lump, 5 irreducible lump, 5 painless and 4 pain/discomfort). All emergency presentations were with a tender irreducible groin lump but only three patients had abdominal pain and vomiting. None of the patients presented with groin symptoms together with a change in bowel habit.
During this period of time there were 1,092 inguinal hernia repairs in adults: 173 bilateral, 412 on right and 334 on left. A sliding hernia was identified at 2.9% of hernia repairs (32/1,092).
A technical complication occurred in two patients: colotomy and ligation of the testicular artery for bleeding—both patients developed a wound haematoma. Five minor complications were recorded (5/32 or 16%): one acute urinary retention, three wound haematomas (managed non-operatively) and one seroma (re-operation). Thus, 26 patients had a complication-free outcome (84%). There were no instances of surgical site infection. Intra-operatively, 24 patients received cefalothin, three received various combinations of antibiotics and four patients received no antibiotics. Twenty-six patients have been followed-up at a mean of 3.2 months (range: 18–1,062 days). One patient was diagnosed with pseudomyxoma peritonei. One patient died from unrelated disease 9 months post-operatively (exacerbation of chronic obstructive airways disease). Two patients underwent subsequent TEP repair for indirect recurrence (11 months after Lichtenstein and 34 months after Perfix plug-and-patch repair).
Discussion
Surprisingly, very little is published regarding the acute complications and long-term outcomes of patients with a sliding inguinal hernia when as many as 8% of groin hernias are said to be sliders [4]. Bendavid defines a sliding hernia as a “protrusion through an abdominal wall opening of a retroperitoneal organ, with or without its mesentery, with or without an adjacent peritoneal sac” [4]. He describes three types: Type I occurs when a part of the peritoneal sac is made up by the wall of a viscus (95% of sliding hernias). Type II occurs when the mesentery of a retroperitoneal viscus forms part of the wall of the peritoneal sac (5% of sliding hernias). Type III is exceedingly rare and occurs when the viscus itself protrudes (without a peritoneal sac).
The pathogenesis of sliding hernias is unclear but Moschowitz’ pulling and pushing hypothesis seems the most plausible [6]. Variably, the viscus, its lymphovascular pedicle and overlying peritoneum enter the inguinal canal via the postero-lateral aspect of the dilated deep inguinal ring [4]. The surgeon suspects a sliding hernia at anterior hernia repair upon finding an eccentrically thick walled sac; this is confirmed by opening the anterior surface of the sac [6]. One must then recognise that the viscus is not attached to the sac but actually forms the wall of the sac and there should be no attempts at liberating the viscus as it may be injured or devascularised. The sac is then returned to the peritoneal cavity and the hernial defect repaired. Sliding hernias are probably under-recognised at TEP repair: the viscus forms the postero-lateral aspect of the sac while the camera provides a supero-medial view. This contrasts with the 360 degree view of the sac afforded the surgeon at anterior repair.
Drawing clinical conclusions by interpreting retrospective data is difficult. Until the results of a prospectively maintained database are published, the true incidence, rate of complications and recurrence can only be estimated by studies such as this. The main limitations of this retrospective study include: incomplete descriptions of the operative findings, the possibility that not all sliding hernia repairs were identified, and short follow-up.
In this series, the typical patient with a sliding hernia is a 62-year-old male with 9 months of symptoms from an indirect left inguinal hernia who undergoes elective anterior repair. Median post-operative length of stay was 1 day but 16% of patients developed an early complication (5/31). A technical complication occurred in two patients (6%). A sliding hernia was identified at 3% of all inguinal hernia repairs over a period of 6 years, which is less than in Bendavid’s review [4]. In accordance with current evidence, single dose antibiotic prophylaxis was prescribed for the majority of patients undergoing mesh inguinal hernia repair [7]. Two patients (6%) have undergone TEP repair for indirect recurrence.
It would be useful if future publications regarding inguinal hernia repair reported the outcome for sliders, as anterior repair of these continues to be a challenge given the rate of technical complications and a significant recurrence rate.
References
Medscape (2000) http://www.medscape.com/viewarticle/420354_2. Accessed 22 February 2009
Kehlet H, Bay-Nielsen M (2008) Nationwide quality improvement of groin hernia repair from the Danish Hernia database of 87, 840 patients from 1998 to 2005. Hernia 12:1–7
Bisgaard T, Bay-Nielsen M, Christensen IJ, Kehlet H (2007) Risk of recurrence 5 years or more after primary Lichtenstein mesh and sutured inguinal hernia repair. Br J Surg 94:1038–1040
Bendavid R (2002) Sliding hernias. Hernia 6:137–140
Ozkan OV, Semerci E, Aslan E, Ozkan S, Dolapcioglu K, Besirov E (2008) A right sliding indirect inguinal hernia containing paraovarian cyst, fallopian tube, and ovary: a case report. Arch Gynecol Obstet 279:897–899
Moschcowitz AV (1925) The rational treatment of sliding hernia. Ann Surg 81:330–334
Gravante G, Venditti D, Filingeri V (2008) The role of single-shot antibiotic prophylaxis in inguinal hernia repair: a meta-analysis approach of 4336 patients. Ann Surg 248:496–497
Conflict of interest statement
No conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Adams, R.A., Wysocki, A.P. Outcome of sliding inguinal hernia repair. Hernia 14, 47–49 (2010). https://doi.org/10.1007/s10029-009-0563-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-009-0563-5