Abstract
Background and aims
The clinical value of synbiotics in surgical patients remains unclear. The aim of this study was to investigate the effect of synbiotics on intestinal integrity and microflora, as well as on surgical outcome, in patients undergoing high-risk hepatectomy.
Methods
Fifty-four patients with biliary cancer were randomly allocated to two groups before hepatectomy. One group received postoperative enteral feeding that included synbiotics; the other received enteral feeding only. Lactulose/mannitol (L/M) ratio, serum diamine oxidase (DAO) activity, and fecal microflora and organic acid concentrations were determined. Postoperative infectious complications were recorded.
Results
Of the 54 patients, 44 completed the trial (21 receiving synbiotics and 23 others as controls). Postoperative changes in L/M ratios and serum DAO activities were identical between the two groups. Numbers of beneficial bacteria increased in the synbiotics group after surgery but decreased in controls. Numbers of harmful microorganisms decreased in the synbiotics group but increased in controls. Total organic acid concentrations increased in the synbiotics group but decreased in controls. Incidence of infectious complications was 19% (4/21) in the synbiotics group and 52% (12/23) in controls (P<0.05). All study patients tolerated surgery (mortality 0%).
Conclusions
Synbiotics, combined with early enteral nutrition, can reduce postoperative infections. This beneficial effect presumably involves correction of an intestinal microbial imbalance induced by surgical stress.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Resection is used increasingly to manage neoplasms of the liver. Today, thanks to improvements in surgical techniques and refinements in preoperative and postoperative management, hepatectomy for metastatic liver cancer can be performed with acceptably low mortality. However, hepatectomy for biliary cancer still is associated with high morbidity and mortality rates [1–4], and septic complications after hepatectomy remain a major problem [5–7]. Patients with biliary cancer that involves the hepatic hilus are prone to immune compromise because the tumor is usually diagnosed at an advanced stage and is associated with obstructive jaundice. In addition, hepatectomy exacerbates immune dysfunction, as the liver is the principal organ of metabolism and constitutes the major part of the reticuloendothelial system [8]. Many reports have suggested that infections in immunocompromised hosts often arise from their intestinal microflora [8, 9]. Indigenous enteric Gram-negative bacteria, such as the Enterobacteriaceae, are among the leading causes of infections.
Lilly and Stillwell [10] first introduced the term “probiotics” for bacteria that benefit the host by improving intestinal microbial balance. Probiotics include Lactobacilli and Bifidobacteria and are widely used as a viable microbial food supplement [11]. Additionally, the term prebiotics has been adopted to refer to a non-digestive food constituent that selectively alters the growth and/or activity of one or a limited number of bacteria in the colon, thus potentially improving the health of the host [11–13]. Several types of ingredients, such as fructo-oligosaccharides, galacto-oligosaccharides, and inulin, are used as prebiotics. Combined use of probiotics and prebiotics is called synbiotics [13]. Synbiotic combinations are considered to have beneficial effects on human health, but their clinical value in surgical patients remains unclear because only a few clinical studies have been conducted [14–16].
The aim of the present prospective randomized study was to investigate the effect of synbiotics on intestinal permeability, integrity, and microflora, as well as on surgical outcome, in a clinical setting.
Materials and methods
Patients
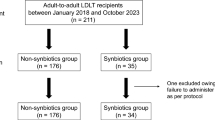
This study involved 54 patients with biliary cancer (perihilar cholangiocarcinoma or gallbladder cancer involving the hepatic hilus) who were scheduled to undergo combined liver and extrahepatic bile duct resection with hepaticojejunostomy at the Nagoya University Hospital between July 2000 and December 2002. Patients scheduled to undergo hepatopancreatoduodenectomy were not included. Subjects were randomly allocated to two groups before surgery: one group received postoperative enteral feeding with synbiotics, and the other received enteral feeding only. Written informed consent for participation was obtained from each patient before enrollment in the study, which was approved by the Human Research Review Committee of Nagoya University Hospital.
All patients received a regular diet preoperatively; no patient received parenteral or enteral nutritional supplementation. In patients with obstructive jaundice who underwent percutaneous transhepatic biliary drainage, all of the externally drained bile from biliary drainage catheter was replaced per os or by ingestion through a nasoduodenal tube, in order to maintain intestinal integrity [17]. All patients underwent intestinal preparation with an iso-osmotic solution (2 l), given on the day before operation, and received antibiotic prophylaxis as a single intravenous drip infusion 30 min before surgery.
An 8F catheter for enteral feeding was placed through a jejunal limb during surgery. This enteral feeding (Harmonic M, 1 kcal/ml; Mitsubishi Pharma, Tokyo, Japan) was initiated on postoperative day 1, at 100 kcal/day, and was increased gradually to 400 kcal/day by day 6. Oral intake was allowed on day 6 or 7; then, enteral feeding was decreased gradually as oral intake increased. Parenteral nutrition also was supplied via a central venous catheter, placed while the patient was in the operating room, immediately before surgery. This central venous catheter was removed 7 to 10 days postoperatively. The synbiotics used were Yakult BL Seichōyaku (Yakult Honsha, Tokyo, Japan) containing 1×108 living Bifidobacterium breve strain Yakult and 1×108 living Lactobacillus casei strain Shirota/g, as well as galacto-oligosaccharides (Oligomate 55; Yakult Honsha). Yakult BL Seichōyaku (3 g/day) and galacto-oligosaccharides (12 g/day) were administered, through the 8F feeding catheter, from postoperative day 1 to day 14.
The lactulose–mannitol test was performed 1 day before hepatectomy, and 2, 7, and 28 days after hepatectomy. Blood was sampled before and after surgery for standard laboratory tests and measurement of serum diamine oxidase (DAO) activity. Feces, also, were sampled 1 day before hepatectomy and 7 and 28 days after hepatectomy for bacteriological examination.
Lactulose–mannitol test
Intestinal permeability was assessed by the lactulose–mannitol test. The test solution consisted of 10 g of lactulose (Sigma-Aldrich, Tokyo, Japan) and 5 g of mannitol (Sigma-Aldrich), which were mixed in 60 ml of physiological saline. After an overnight fast, the subjects fully voided, and the test solution was administered orally. In the next 6 h, subjects were at rest and were allowed no food or water. All urine was collected for 6 h. A 10-ml sample was taken from the pooled urine and frozen at −20°C until required for analysis. Urinary lactulose and mannitol concentrations were measured by gas–liquid chromatography [18]. Finally, the urinary lactulose–mannitol ratio (L/M ratio) was calculated.
Serum diamine oxidase activity
Blood samples were centrifuged at 1,000 g for 10 min at 4°C, and the sera were stored at −80°C until required for measurement. Serum DAO activity was determined by Takagi’s method [19], which is a simple and sensitive colorimetric assay based on a coupled reaction with peroxidase and a novel chromogen, 10-(carboxymethyl-aminocarbonyl)-3,7-bis(dimethylamino)-phenothiazine sodium salt (DA-67; Wako Pure Chemical Industries, Osaka, Japan). Briefly, 1.5 ml of cadaverine solution [525.3 mg of cadaverine hydrochloride dissolved in 100 ml of piperadine-N,N′-bis (2-ethanesulfonic acid) buffer (25 mmol/l, pH 7.2, containing 0.5% Triton X-100)] and 0.1 ml of the serum sample were incubated at 37°C for 30 min. Then, 1.5 ml of DA-67 (40.8 mg/ml), ascorbate oxidase (cucumber, 5 U/ml), peroxidase (Type X: horseradish, 6 purpurogallin U/ml) were added, followed by incubation for another 60 min. Colorimetric absorption was measured by spectrophotometry (UVIDEC-40; Japan Spectroscopic, Tokyo, Japan) at a wavelength of 668 nm.
Fecal bacteriologic examination
Feces were collected in a test tube, which was maintained anaerobically in an atmosphere of 7% H2 and 5% CO2 in N2. The test tube was refrigerated until culture. VL-G roll tube agar [20], supplemented with 0.2% cellobiose and 0.2% maltose (modified VL-G roll tube agar), was used to determine total anaerobe counts. Various media were used for selective isolation of different microorganisms: modified VL-G roll tube agar to which 80 μg/ml vancomycin and 1μg/ml kanamycin were added for Bacteroidaceae; CW agar (Nikken Bio Medical Laboratory, Kyoto, Japan) for lecitinase-positive Clostridium; MPN agar [21] for Bifidobacterium; COBA agar [22] for Enterococcus; LBS agar (Becton Dickinson, Cockeysville, Md., USA) supplemented with 0.8% Lab Lemco powder (Oxoid, Basingstoke, UK) for Lactobacillus; Staphylococcus medium no. 110 agar (Nissui Pharmaceutical, Tokyo, Japan) for Staphylococcus and Bacillus; DHL agar (Nissui Pharmaceutical) for Enterobacteriaceae; NAC agar (Nissui Pharmaceutical) for Pseudomonas; and GS agar (Nissui Pharmaceutical) for Candida. TOS agar [23], supplemented with 6.25 mg/ml streptomycin sulfate (Sigma, St Louis, Mo., USA) and 1 mg/ml carbenicillin disodium salt (Sigma, T-CBPC agar), was used for quantitation of Bifidobacterium breve strain Yakult. LLV agar [24] was used for quantitation of Lactobacillus casei strain Shirota. CW agar, LBS agar, and T-CBPC agar media were cultured anaerobically at 37°C for 72 h. After incubation, the colonies on the plates were counted and Gram stained. Numbers of viable bacteria per gram of feces (wet weight) were calculated. Bifidobacterium breve strain Yakult and Lactobacillus casei strain Shirota were identified by enzyme-linked immunosorbent assay (ELISA) using strain-specific monoclonal antibodies [24]. All bacterial counts [colony-forming units (CFUs)/g of wet feces] were transformed to logarithms (log10 CFU) for ease of statistical analysis. The lower limit of bacterial detection with this procedure was 1,000 CFUs/g of feces for the obligate anaerobes, Bacteroidaceae and Bifidobacterium and 100 CFUs/g of feces for other bacteria.
Determination of fecal organic acid concentrations
Feces were homogenized in 1 ml of distilled water. The homogenate was placed in an Eppendorf tube and centrifuged at 10,000 rpm at 4°C for 10 min. A mixture of 0.9 ml of the resulting supernatant and 0.1 ml of 1.5 mol/l perchloric acid were mixed well in a glass tube and then allowed to stand at 4°C for 12 h. The suspension was then passed through a filter with a pore size of 0.45 μm (Millipore Japan, Tokyo). The sample was analyzed for organic acids by high-performance liquid chromatography (HPLC) as previously described [25]. The HPLC was performed with a Waters system (Waters 432 conductivity detector; Waters, Milford, Mass., USA) equipped with two columns (Shodex Rspack KC-811; Showa Denko, Tokyo). Concentrations of organic acids were calculated with the use of external standards and were expressed as micromoles per gram of wet feces.
Recording of infectious complications
Detailed daily records of patients’ postoperative courses were kept, and infectious complications were recorded for up to 30 days after surgery. Wound infection was defined as spontaneous or surgically released purulent discharge with positive cultures. Intra-abdominal abscess was defined as purulent discharge with positive cultures from abdominal drains placed at surgery or as fluid collection requiring drainage. Pneumonia was defined as a characteristic pulmonary infiltrate on a chest radiograph accompanied by leukocytosis.
Blood was obtained for cultures if a patient developed a fever exceeding 38.5°C after hepatectomy, irrespective of the presence or absence of other infectious sources. For each set of blood cultures, 10 ml of blood was drawn under sterile conditions and then immediately inoculated into different culture bottles (Organon Teknika, Durham, N.C., USA) for aerobic and anaerobic cultures. The blood was incubated until bacterial growth was detected, or for 7 days. Bacteremia was diagnosed when a single blood culture grew an isolate of organisms, unless the isolate was Staphylococcus epidermidis or coagulase-negative Staphylococcus species. In these cases, diagnosis required isolation from two or more blood cultures [7].
Statistics
Results are expressed as the mean ± standard deviation. Statistical analysis was performed with the Fisher exact probability test and paired and unpaired Student’s t-tests, where appropriate. P<0.05 was considered statistically significant.
Results
Demographic characteristics of study patients
Of the 54 patients, ten were excluded because they underwent only laparotomy based on intraoperative findings of peritoneal dissemination, liver metastasis, and/or locally advanced unresectable tumor. The remaining 44 patients who underwent curative resection completed the trial; 23 were assigned to the control group (postoperative enteral feeding without synbiotics), and 21 were assigned to the synbiotics group (postoperative enteral feeding including synbiotics). All patients underwent hemihepatectomy or more extensive resection with en bloc resection of the caudate lobe and the extrahepatic bile duct. Combined vascular resection with reconstruction [3] was performed in seven patients in each of the two groups. Baseline characteristics were well matched between the two groups (Table 1).
Routine laboratory results
Postoperative values for hemoglobin, serum total protein, and serum total bilirubin were equally distributed between the two groups. White blood cell counts and concentrations of C-reactive protein were lower in the synbiotics group, with a significant difference on postoperative day 10 (Table 2).
Lactulose–mannitol ratio and serum diamine oxidase activity
In both the control and synbiotics groups the L/M ratios increased significantly, (P<0.05) on postoperative day 2, and then gradually decreased, returning to the preoperative value by day 28. Postoperative changes in L/M ratio showed no intergroup differences (Fig. 1a).
In both the control and synbiotics groups serum DAO activities decreased significantly (P<0.05) on postoperative day 2, remained low on day 7, and then returned to the preoperative value by day 28. Postoperative changes in serum DAO activity were similar between the two groups (Fig. 1b).
Fecal microflora
Total numbers of anaerobic bacteria and the number of Bacteroidaceae, which were the dominant anaerobic species, were unchanged before and after surgery in both control and synbiotics groups (Table 3). Numbers of beneficial bacteria, including Bifidobacteria and Lactobacilli, were increased in the synbiotics group after surgery, while they were decreased in the control group (Fig. 2a). In contrast, numbers of harmful microorganisms, including Enterobacteriaceae, Pseudomonas, and Candida, were decreased in the synbiotics group but were increased in the control group (Fig. 2b). Numbers of Enterococci were increased after surgery in both groups, without intergroup differences.
Numbers of beneficial bacteria (a) and harmful bacteria (b) before and after hepatectomy. Bifidobacteria in control (open circles) and synbiotics (filled circles) groups; Lactobacilli in control (open squares) and synbiotics (filled squares) groups; Enterobacteriaceae in control (open triangles) and synbiotics (filled triangles) groups; Candida in control (open diamonds) and synbiotics (filled diamonds) groups; Pseudomonas in control (open stars) and synbiotics (filled stars) groups. *P<0.05 between the two groups. †P<0.05 vs before hepatectomy
In the synbiotics group, Lactobacillus casei strain Shirota and Bifidobacterium breve strain Yakult, which were administered postoperatively as Yakult BL Seichōyaku, were confirmed to be isolated from feces, indicating that these two beneficial bacteria had colonized the intestine.
Fecal organic acid concentrations
Total organic acid concentrations in the control group had decreased from 87.1±39.0 μmol/g to 44.1±18.5 μmol/g of feces on postoperative day 7 (P<0.05); these then increased but remained significantly low (P<0.05) compared to preoperative concentrations, even on day 28. In contrast, total organic acid concentrations in the synbiotics group had increased on day 7 and then increased further, reaching 105.6±34.0 μmol/g of feces on day 28 (P<0.05). Thus, total organic acid concentrations on days 7 and 28 were significantly (P<0.05) higher in the synbiotics group than in the control group. Changes in concentrations of short-chain fatty acids (SCFAs), including acetic acid, propionic acid, and butyric acid, paralleled changes in total organic acid concentrations in both groups (Table 4; Fig. 3).
Organic acid concentrations before and after hepatectomy. Total organic acids in control (open circles) and synbiotics (filled circles) groups; acetic acid in control (open squares) and synbiotics (filled squares) groups; propionic acid in control (open triangles) and synbiotics (filled triangles) groups. *P<0.05 between the two groups. †P<0.05 vs before hepatectomy
Surgical outcome
Several kinds of infectious complications occurred after surgery, including bacteremia, intra-abdominal abscess, wound infection, and pneumonia. Urinary tract infection did not develop in any patient. The incidence of each complication was less frequent in the synbiotics group. Of the 23 control patients, 12 (52.2%) had postoperative infectious complications, while only four (19.0%) of the 21 synbiotics patients had infectious complications (P<0.05). Consequently, postoperative hospital stay and cumulative duration of antibiotic therapy were shorter in the synbiotics group than in the control group, although the difference was not statistically significant. All patients tolerated surgery and were discharged from the hospital in good condition (Table 5).
Several kinds of microorganisms were isolated from infectious foci. Enterobacter species were the most common pathogens, followed by Enterococcus species. The total number of isolations of Enterobacteriaceae, including Enterobacter, Serratia, Morganella, and Citrobacter, in the control group was more than double the total in the synbiotics group (nine vs four; Table 6).
Discussion
This prospective randomized study clearly demonstrated that early enteral nutrition, with combined use of viable probiotic bacteria and galacto-oligosaccharides as prebiotics, can achieve a significant reduction in infectious complications after high-risk hepatectomy. Three important randomized studies on the effect of probiotics in surgical patients were reported recently [14–16]. One study by, McNaught et al. [14], failed to demonstrate a beneficial effect; the incidence of bacterial translocation (12% vs 12%) and septic morbidity (15% vs 13%) were almost the same in control and treatment groups. Reasons for a negative result might include less-invasive surgery (e.g., colectomy or resection of the small intestine) and use of probiotic bacteria without the addition of prebiotics. On the other hand, the remaining two studies, by Rayes et al. [15, 16], in which fiber-enriched enteral nutrition, including viable Lactobacilli, was administered, demonstrated a significant reduction of postoperative infectious complications. In particular, their study in liver transplant recipients [15] demonstrated a sepsis rate of 48% (15/32) in patients receiving standard enteral nutrition, compared with only 13% (4/31) in patients receiving the fiber-enriched enteral nutrition including Lactobacilli. Our results are consistent with their observations, strongly suggesting a beneficial effect of synbiotics in surgical patients, especially those undergoing high-risk surgery such as liver transplantation or hepatectomy for biliary cancer.
Early enteral feeding after severe burn injury or major surgery prevents hypermetabolism [26] and maintains immunocompetence [27]. Further, enteral feeding is reported to reduce septic complications, shorten hospital stays, and reduce the risk of death [28]. These findings indicate that enteral nutrition is preferable to parenteral nutrition. However, it is often impossible to provide nutritional support in surgical patients solely by enteral feeding. High-volume enteral feeding after surgery often causes abdominal fullness, nausea, and diarrhea, necessitating discontinuation of enteral feeding. Omura et al. [29] reported that, in rats, enteral feeding corresponding to only 15% of the total caloric intake could prevent an increase in intestinal permeability and bacterial translocation. They recommended combined nutritional support, consisting of parenteral nutrition and a small amount of enteral feeding, for surgical patients. In the present study we also used early low-volume enteral feeding combined with parenteral nutrition. All patients tolerated this modest enteral feeding well.
Among many probiotic bacteria used worldwide, we chose Bifidobacterium breve strain Yakult and Lactobacillus casei strain Shirota. These species were established as probiotics in Japan several decades ago and have a long history of use in humans, without severe complications. Another advantage of these organisms is availability of specific monoclonal antibodies that can detect them by immunological techniques [24, 30]. Importantly, the administered probiotic bacteria were detected at high levels in the feces of our patients.
We determined the L/M ratio (lactulose–mannitol test) and serum DAO activity to assess intestinal integrity. The lactulose–mannitol test is used to assess intestinal permeability [31]. DAO (EC 1.4.3.6), an intracellular enzyme catalyzing oxidation of diamines, exists in high concentrations in the intestinal mucosa. Serum DAO activity has been found to be proportional to the amount of intestinal DAO, making it a reliable marker of intestinal mucosal integrity [32]. While the previously used method for serum DAO analysis [32] required systemic heparinization, the method used in the present study does not. Measuring serum DAO activity by the newer method [19] is an easy, sensitive, and practicable way to assess the mucosa. The present study showed a significant increase in L/M ratios and decrease in DAO activities after surgery, and the extent of postoperative changes in these parameters were similar between the control and synbiotics groups. These findings suggest that use of synbiotics does not reduce the extent of physical damage to intestinal mucosa after surgery.
Bacterial analysis of stool is a long, complex procedure. Bacterial concentrations differ, depending on the intestinal segment from which samples are taken. Furthermore, analysis of samples rather than 24-h stool collections may certainly result in loss of some information, as artificial nutrition is known to modify the volume of daily stools [33]. Nevertheless, sampling of feces is the most practicable approach, because more systematic stool collection is often difficult in surgical patients, and sampling still provides important information concerning the intestinal microflora [34]. The technique that we used here provided detailed information about the fecal microflora; measurement of organic acids also contributed to bacterial identification [35]. To our knowledge, this is the first report to fully describe postoperative changes in fecal microflora and organic acids in surgical patients.
An important finding of this study is that use of synbiotics notably changed the fecal microflora of surgical patients. In the control group, beneficial bacteria, including Bifidobacteria and Lactobacilli, decreased postoperatively, and harmful microorganisms, including Enterobacteriaceae, Pseudomonas, and Candida, increased after surgery. In the synbiotics group, however, trends were totally opposite; beneficial bacteria increased and harmful microorganisms decreased. Our results strongly suggest that synbiotics use improves the intestinal microbial imbalance induced by surgical stress, leading to fewer postoperative infections. Harmful bacteria form certain putrefactive substances, including ammonia, hydrogen sulfate, amines, phenols, indoles, and secondary bile acids [33], which may injure the intestine and have more generalized toxicity. On the other hand, lactic acid-producing bacteria, such as Bifidobacteria and Lactobacilli, are considered beneficial bacteria, ferment carbohydrate to produce lactic acid, but do not produce putrefactive products. In addition, these beneficial bacteria are reported to stimulate various immune functions, showing mitogenic activity [36], adjuvant activity [37], enhanced macrophage activation [38], enhancement of antibody [39] and interferon production [38], and even an anti-tumor effect [40]. Beneficial intestinal flora protect the intestinal tract from proliferation of harmful bacteria, while harmful bacteria manifest pathogenicity when host resistance is decreased [33]. Considering these findings, increasing beneficial bacteria and decreasing harmful bacteria are important for maintaining host defenses, especially during recovery from major surgery.
SCFAs such as acetate, propionate, and butyrate are end products of microbial fermentation of indigestible carbohydrates that reach the colon. These play various important roles in the colon, including activation of epithelial proliferation [41], stimulation of intestinal motility [42], and enhancement of epithelial mucin secretion [43], as well as being an energy source of the epithelial cells. Colonic SCFAs, thus, possibly have beneficial effects on epithelial cells integrity and may be involved in a defense system of the colon. Fecal SCFAs concentrations in the control group markedly decreased postoperatively, suggesting impairment of microbial fermentation of carbohydrates. An increase in SCFAs, coupled with an increase in beneficial bacteria in the synbiotics group, suggests that use of synbiotics contributes to maintenance of the levels of SCFAs in colonic contents after surgery. As expected, the galacto-oligosaccharides administered were used as a substrate not only by the administered probiotic bacteria but also by indigenous beneficial bacteria.
Conclusion
In conclusion, use of synbiotics, combined with early enteral nutrition, can reduce postoperative infections. This beneficial effect most likely results from correction of an intestinal microbial imbalance induced by surgical stress. The synbiotics therapy presented here, including two probiotics (Bifidobacterium breve and Lactobacillus casei) together with a prebiotic (galactooligosaccharides), is promising as a contribution to patient management following high-risk liver surgery.
References
Nagino M, Nimura Y, Hayakawa N, Kamiya J, Kondo S, Sasaki R, Hamajima N (1993) Logistic regression and discriminant analyses of hepatic failure after liver resection for carcinoma of the biliary tract. World J Surg 17:250–255
Pichlmayr R, Weimann A, Klempnauer J, Oldhafer KJ, Maschek H, Tusch G, Ringe B (1996) Surgical treatment in proximal bile duct cancer. A single-center experience. Ann Surg 224:628–638
Nimura Y, Kamiya J, Nagino M, Kanai M, Uesaka K, Kondo S, Hayakawa N (1998) Aggressive surgical treatment of hilar cholangiocarcinoma. J Hepatobiliary Pancreat Surg 5:52–61
Neuhaus P, Jonas S, Bechstein WO, Lohmann R, Radke C, Kling N, Wex C, Lobeck H, Hintze R (1999) Extended resection for hilar cholangiocarcinoma. Ann Surg 230:808–819
Nagino M, Kamiya J, Uesaka K, Sano T, Yamamoto H, Hayakawa N, Kanai M, Nimura Y (2001) Complications of hepatectomy for hilar cholangiocarcinoma. World J Surg 27:1277–1283
Sitzmann JV, Greene PS (1994) Perioperative predictors of morbidity following hepatic resection for neoplasms. Ann Surg 219:13–17
Shigeta H, Nagino M, Kamiya J, Uesaka K, Sano T, Yamamoto H, Hayakawa N, Kanai M, Nimura Y (2002) Bacteremia after hepatectomy: an analysis of single center, 10-year experience with 407 patients. Langenbecks Arch Surg 387:117–124
Wang X, Soltesz V, Andersson R, Bengmark S (1993) Bacterial translocation in acute liver failure induced by 90 per cent hepatectomy in the rat. Br J Surg 80:66–71
Tancrede CH, Andremont AO (1985) Bacterial translocation and gram-negative bacteremia in patients with hematological malignancies. J Infect Dis 152:99–103
Lilly D, Stillwell RJ (1965) Probiotics: growth promoting factors produced by microorganisms. Science 147:747–748
Fuller R (1991) Probiotics in human medicine. Gut 32:439–442
Gibson GR, Beatty ER, Wang X, Cummings JH (1995) Selective stimulation of Bifidobacteria in the human colon by oligofructose and inulin. Gastroenterology 108:975–982
Colins MD, Gibson GR (1999) Probiotics, prebiotics, and synbiotics: approaches for modulating the microbial ecology of the gut. Am J Clin Nutr 69 [Suppl]:1052S–1057S
McNaught CE, Woodcock NP, MacFie J (2002) A prospective randomized study of the probiotic Lactobacillus plantarum 299V on indices of gut barrier function in elective surgical patients. Gut 51:827–831
Rayes N, Seehofer D, Hansen S, Boucsein K, Muller AR, Serke S, Bengmark S, Neuhaus P (2002) Early enteral supply of lactobacillus and fiber versus selective bowel decontamination: a controlled trial in liver transplant recipients. Transplantation 74:123–128
Rayes N, Hansen S, Seehofer D, Muller AR, Serke S, Bengmark S (2002) Early enteral supply of fiber and Lactobacilli versus conventional nutrition: a controlled trial of patients with major abdominal surgery. Nutrition 18:609–615
Kamiya S, Nagino M, Kanazawa H, Komatsu S, Mayumi T, Takagi K, Asahara T, Nomoto K, Tanaka R, Nimura Y (2004) The value of bile replacement during external biliary drainage: an analysis of intestinal permeability, integrity, and microflora. Ann Surg 239:510–517
Jansen G, Muskiet FA, Schierbeek H, Berger R, van der Slik W (1986) Capillary gas chromatographic profiling of urinary, plasma and erythrocyte sugars and polyols as their trimethylsilyl derivatives, preceded by a simple and rapid prepurification method. Clin Chim Acta 157:277–293
Takagi K, Nakao M, Ogura Y, Nabeshima T, Kunii A (1994) Sensitive colorimetric assay of serum diamine oxidase. Clin Chim Acta 226:67–75
Azuma R, Suto T (1970) Validity of transfer of the taxonomical position of Corynebacterium pseudopyogenes from genus Corynebacterium to genus Actinomyces. In: Izuka H, Hasegawa T (eds) Proceeding of the first international conference on culture collection. University of Tokyo Press, Tokyo, pp 493–505
Tanaka R, Mutai M (1980) Improved medium for selective isolation and enumeration of Bifidobacterium. Appl Environ Microbiol 40:866–869
Petts DN (1984) Colistin–oxolinic acid–blood agar: a new selective medium for streptococci. J Clin Microbiol 19:4–7
Sonoike K, Mada M, Mutai M (1986) Selective agar medium for counting viable cells of bifidobacteria in fermented milk (in Japanese with English abstract). J Food Hyg Soc Jpn 27:238–244
Kitajima H, Sumida Y, Tanaka R, Yuki N, Takayama H, Fujimura M (1997) Early administration of Bifidobacterium breve to preterm infants: randomized controlled trial. Arch Dis Child 76:101–107
Kikuchi H, Yajima T (1992) Correlation between water-holding capacity of different types of cellulose in vitro and gastrointestinal retention time in vivo of rats. J Sci Food Agric 60:139–146
Mochizuki H, Trocki O, Dominioni L, Brackett KA, Joffe SN, Alexander JW (1984) Mechanism of prevention of postburn hypermetabolism and catabolism by early enteral feeding. Ann Surg 200:297–310
Gionotti L, Alexander JW, Nelson JL (1994) Role of early enteral feeding and acute starvation on postburn bacterial translocation and host defense: prospective, randomized trials. Crit Care Med 22:265–272
Kudsk KA, Croce MA, Fabian TC, Minard G, Tolley EA, Poret HA (1992) Enteral versus parenteral feeding: effects on septic morbidity after blunt and penetrating abdominal trauma. Ann Surg 215:503–513
Omura K, Hirano K, Kanehira E, Kaito K, Tamura M, Nishida S, Kawakami K, Watanabe Y (2000) Small amount of low-residue diet with parenteral nutrition can prevent decreases in intestinal mucosal integrity. Ann Surg 231:112–118
Yuki N, Watanabe K, Mike A, Tagami Y, Tanaka R, Ohwaki M, Morotomi M (1999) Survival of a probiotic, Lactobacillus casei Shirota, in the gastrointestinal tract: selective isolation from feces and identification using monoclonal antibodies. Int J Food Microbiol 48:51–57
Welsh FK, Ramsden CW, MacLennan K, Sheridan MB, Barclay GR, Guillou PJ, Reynolds JV (1998) Increased intestinal permeability and altered mucosal immunity in cholestatic jaundice. Ann Surg 227:205–212
Luk G, Bayless TM, Baylin SB (1983) Plasma postheparin diamine oxidase. J Clin Invest 71:1308–1315
Mitsuoka T (2000) Significance of dietary modulation of intestinal flora and intestinal environment. Biosci Microflora 19:15–25
Schneider SM, Le Gall P, Girard-Pipau F, Piche T, Pompei A, Nano JL, Hebuterne X, Rampal P (2000) Total artificial nutrition is associated with major changes in the fecal flora. Eur J Nutr 39:248–255
Guerrant GO, Lambert MA, Moss CW (1982) Analysis of short-chain acids from anaerobic bacteria by high-performance liquid chromatography. J Clin Microbiol 16:355–360
Takagi A, Matsuzaki T, Sato M, Nomoto K, Morotomi M, Yokokura T (1999) Inhibitory effect of oral administration of Lactobacillus casei on 3-methylcholanthrene-induced carcinogenesis in mice. Med Microbiol Immunol 188:111–116
Yasui H, Nagaoka N, Hayakawa K (1994) Augmentation of anti-influenza virus hemagglutinin antibody production by Peyer’s patch cells with Bifidobacterium breve YIT4064. Clin Diagn Lab Immunol 1:244–246
Kato I, Tanaka K, Yokokura T (1999) Lactic acid bacterium potently induces the production of interleukin-12 and interferon-gamma by mouse splenocytes. Int J Immunopharmacol 21:121–131
Yasui H, Nagaoka N, Mike A (1991) Enhancement of immune response in Peyer’s patch cells cultured with Bifidobacterium breve. J Dairy Sci 74:1187–1195
Takagi A, Matsuzaki T, Sato M, Nomoto K, Morotomi M, Yokokura T (2001) Enhancement of natural killer cytotoxicity delayed murine carcinogenesis by a probiotic microorganism. Carcinogenesis 22:599–605
Sakata T (1995) Effect of short-chain fatty acids on the proliferation of gut epithelial cells in vivo. In: Cummings JH, Rombeau JL, Sakata T (eds) Physiological and clinical aspects of short-chain fatty acids. Cambridge University Press, Cambridge, pp 289–305
Cherbut C (1995) Effects of short-chain fatty acids on gastrointestinal motility. In: Cummings JH, Rombeau JL, Sakata T (ed) Physiological and clinical aspects of short-chain fatty acids. Cambridge University Press, Cambridge, pp 191–208
Willemsen LE, Koetsier MA, van Deventer SJH, van Tol EA (2003) Short chain fatty acids stimulate epithelial mucin2 expression through differential effects on prostaglandin E1 and E2 production by intestinal myofibroblasts. Gut 52:1442–1447
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kanazawa, H., Nagino, M., Kamiya, S. et al. Synbiotics reduce postoperative infectious complications: a randomized controlled trial in biliary cancer patients undergoing hepatectomy. Langenbecks Arch Surg 390, 104–113 (2005). https://doi.org/10.1007/s00423-004-0536-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-004-0536-1