Abstract
Purpose
Infectious complications, particularly post-transplant sepsis, have a critical impact on postoperative outcomes. This study examined the effects of perioperative synbiotic treatment on postoperative outcomes in patients receiving early enteral nutrition.
Methods
We reviewed 210 living-donor liver transplantation procedures and retrospectively analyzed the postoperative outcomes with and without perioperative synbiotic treatment (live lactic acid bacteria, bifidobacteria, and oligosaccharides) 5 days before and after living-donor liver transplantation.
Results
The synbiotic group (n = 34) had significantly fewer male donors (38.2% vs. 61.9%, p = 0.011) and a higher proportion of ABO-incompatible grafts (52.9% vs. 25.6%, p = 0.021) than the non-synbiotic group (n = 176). The incidence of sepsis was significantly lower in the synbiotic group than in the non-synbiotic group (0% vs. 7.4%, p = 0.029), with a lower incidence rate of sepsis due to bacteremia with intestinal bacteria (0% vs. 4.6%, p = 0.089). There were no significant differences in the proportions of acute rejection, small-for-size graft syndrome, or postoperative liver function between the two groups. Furthermore, there was no significant difference in the graft survival rates after LDLT between two groups. (p = 0.24).
Conclusion
Perioperative synbiotic treatment prevents post-transplant sepsis, even with early enteral nutrition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bacterial infections after liver transplantation (LT) occur in 70% of recipients [1]. Bacterial sepsis after LT is a significant problem that must be addressed because it is associated with mortality in almost 50% of cases [2]. To improve postoperative outcomes after living-donor LT (LDLT), we attempted to reduce the incidence of postoperative bacterial infection through two strategies: early enteral nutrition after LDLT [3] and preemptive thoracic drainage [4]. Early enteral nutrition reduced the occurrence rate of postoperative sepsis, and preemptive thoracic drainage reduced post-LDLT pulmonary complications, resulting in an improved graft survival rate compared with previous years. However, despite these successes, further efforts are needed to improve the postoperative outcomes.
Synbiotics, named by Gibson and Roberfroid in 1995 [5], are a combination of probiotics and prebiotics. Probiotics are beneficial bacteria such as Bifidobacterium and Lactobacillus that increase intestinal motility and stabilize the intestinal barrier against bacterial translocation [6, 7]. Prebiotics are non-digestible food ingredients (fiber) that stimulate the proliferation of beneficial bacteria such as Bifidobacterium in the large bowel and also serve as nutritional sources for probiotic organisms in the colon. Recent literature has shown that synbiotic treatment has positive effects in abdominal surgery, including LT, as well as in liver disease [6,7,8,9,10,11,12]. In our examination of LDLT, we found only two previous reports that revealed a reduction in infectious complications with a combination of 2 days of pre-transplant and 2 weeks of post-transplant synbiotic treatment [8, 9].
In this study, we evaluated the impact of perioperative synbiotic treatment administered 5 days before and after LDLT on reducing the occurrence of infectious complications, especially postoperative sepsis, as well as the current status of sepsis-causing organisms after the introduction of both early enteral nutrition and preemptive thoracic drainage.
Methods
Study design and patients
This retrospective cohort study assessed the impact of perioperative synbiotic treatment on postoperative outcomes of adult-to-adult LDLT. We retrospectively reviewed 210 patients who underwent adult-to-adult LDLT at Kyushu University Hospital between January 2018 and October 2023. The study protocol was approved by the Institutional Review Board of Kyushu University Hospital (2022-146) and conducted in accordance with the Declaration of Helsinki and Istanbul. Written informed consent was obtained from all patients using an opt-out method.
The synbiotic treatment protocol started with eligible recipients on oral administration of Super synbiotics LBG-P™ or Synprotec™ (Yakult Honsha, Tokyo, Japan), which contained 1 g of live lactic acid bacteria and bifidobacteria (1 × 108 living Lacticaseibacillus paracasei strain Shirota and 1 × 108 living Bifidobacterium breve strain Yakult), and a sachet of 6.8 g oligosaccharides, taken three times per day starting 5 days before LDLT and continuing 5 days after LDLT either orally or through a transnasal feeding tube placed intraoperatively in the proximal jejunum. We enrolled recipients who could receive preoperative administration as per the protocol and desired perioperative synbiotic treatment at their own expense into the synbiotic group. A flowchart of the study design is shown in Fig. 1.
Graft selection criteria, surgical procedure, and postoperative management
Our graft selection criteria for adult-to-adult LDLT have been described previously [13, 14]. The surgical procedures for both donors and recipients have been previously described [15,16,17,18], similar to the postoperative management protocol [17, 18]. Recipients were administered cefazolin and cefotaxime as prophylactic antibiotics for 2 days after LDLT. The central venous catheter is usually removed within 5 days unless continuous hemodiafiltration is introduced or a peripheral catheter is difficult to place. Immunosuppression was initiated with a protocol based on corticosteroids, mycophenolate mofetil, and either tacrolimus or cyclosporine A. Everolimus treatment was initiated 1 to 3 months after LDLT. In ABO-incompatible recipients, rituximab (anti-CD20 antibody) was administered 3 weeks before transplantation, and mycophenolate mofetil was started 1 week before transplantation. Double blood cultures were obtained when the patient had a high fever or shivering chills.
Early enteral nutrition and preemptive thoracic drainage
To prevent postoperative infectious complications, we provided early enteral nutrition after LDLT [3, 19] and inserted preemptive thoracic drainage tubes [4] for all recipients in this cohort. Enteral nutrition (polymeric formula) was provided through a transnasal feeding tube placed intraoperatively in the proximal jejunum on the first postoperative day after LDLT. When the recipient could eat 50% of their regular diet, enteral feeding was discontinued. A thoracic drainage tube was inserted intraoperatively under direct visualization to prevent postoperative bleeding. Continuous drainage of pleural effusions reduces the risk of atelectasis and postoperative pneumonia.
Definitions
Sepsis was defined as the isolation of bacteria from simultaneously positive double blood cultures, excluding contamination within the post-transplant hospitalization period, along with clinical symptoms, including a high fever, shivering, dyspnea, altered mental status, tachycardia, and hypotension [3]. Sepsis due to bacteremia with intestinal bacteria was defined as sepsis resulting from pathogenic organisms in the intestinal tract without other sources of fever (cholangitis, urinary tract infection, aspiration pneumonia, etc.), which was diagnosed by a routine examination for a high fever consisting of a blood examination, urinalysis, radiography, and computed tomography (CT) if necessary.
Statistical analyses
All statistical analyses were performed using SAS software (JMP 16.0.0; SAS Institute Inc., Cary, NC, USA). Our methods for identifying possible predictors and choosing variables are based on both our previous studies and global research. Categorical variables were compared using the χ2 test or Fisher’s exact test; continuous variables were compared using the parametric t test or Mann–Whitney U test, and expressed as mean ± standard deviation. Logistic regression analysis was conducted to determine the independent risk factors for sepsis occurrence after LDLT with univariate and multivariate analyses. The graft survival rate was analyzed using the Kaplan–Meier method and compared using the log-rank test. Differences were considered statistically significant at p < 0.05.
Results
Clinical characteristics of recipients who received perioperative synbiotic treatment
We reviewed 210 recipients, 34 (16.2%) of whom were enrolled in the synbiotic group. One recipient was excluded from the analysis owing to failure to administer synbiotics as per the protocol. The clinical characteristics of the synbiotic (n = 34) and non-synbiotic (n = 176) groups are summarized in Table 1. The synbiotic group had a significantly lower proportion of male donors (38.2% vs. 61.9%, p = 0.011) and a higher proportion of ABO-incompatible grafts (52.9% vs. 25.6%, p = 0.021) than the non-synbiotic group. There were no significant differences between the two groups in any other recipient, donor, or operative factor, including the biliary reconstruction method. Regarding postoperative biliary complications, all patients in this cohort had an RTBD tube that left over each biliary anastomosis site during the post-transplant hospitalization period; therefore, we could not detect biliary stricture. In contrast, the proportion of bile leakage was 2.9% in the synbiotic group and 5.1% in the non-synbiotic group (p = 0.56).
Impact of perioperative synbiotic treatment on post-LDLT outcomes
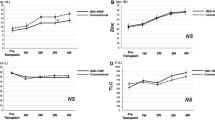
To clarify the impact of perioperative synbiotic treatment, we compared post-LDLT outcomes between synbiotic and non-synbiotic groups. The incidence of sepsis was significantly lower in the synbiotic group than in the non-synbiotic group (0% vs. 7.4%, p = 0.029), with a lower incidence rate of sepsis due to bacteremia with intestinal bacteria (0% vs. 4.6%, p = 0.089) (Fig. 2A). Regarding other infectious complications, the rate of pneumonia was significantly lower proportion in the synbiotics group than in the non-synbiotics group (0% vs. 6.8%, p = 0.036), and two cases in the non-synbiotics group led to sepsis. There were no significant differences in the occurrence of intra-abdominal (2.9% vs. 13.1%, p = 0.052) or urinary tract infections (0% vs. 3.4%, p = 0.14) between the groups. There were no significant differences in the occurrence rates of acute rejection or small-for-size graft syndrome between the groups (8.3% vs. 4.6%, p = 0.34 and 17.7% vs. 10.8%, p = 0.29, respectively) (Fig. 2B and C). With respect to short-term outcomes, there were no significant differences in the total bilirubin level (4.6 ± 2.8 vs. 4.8 ± 3.4 mg/dl, p = 0.81 and 4.7 ± 5.0 vs. 4.3 ± 5.6 mg/dl, p = 0.68, respectively) or prothrombin time/international normalized ratio (1.10 ± 0.12 vs. 1.10 ± 0.13 mg/dl, p = 0.97 and 1.08 ± 0.11 vs. 1.07 ± 0.11 mg/dl, p = 0.62, respectively) on postoperative days (PODs) 7 and 14 between the synbiotic and non-synbiotic groups (Fig. 2D). There were also no significant differences in the duration of central venous catheter placement (4.0 ± 3.4 days vs. 6.5 ± 19.5 days, p = 0.47) and postoperative hospital stay (32.6 ± 10.0 days vs. 41.3 ± 57.3 days, p = 0.39) between the synbiotic and non-synbiotic groups. The graft survival rates at 1 and 6 months after LDLT were 100.0% and 100.0%, respectively, in the synbiotic group, and 97.7% and 95.9%, respectively, in the non-synbiotic group (p = 0.24) (Fig. 2E). Re-transplantation was not performed in this cohort, and the graft survival rate coincided with the overall survival rate.
Postoperative outcomes of perioperative synbiotic treatment in LDLT. A The incidence of sepsis was significantly lower in the synbiotics group than in the non-synbiotics group (p = 0.029) with a lower incident rate of sepsis due to bacteremia with intestinal bacteria (p = 0.089). B, C There were no significant differences in the occurrence rate of acute rejection or small-for-size graft syndrome between the groups (p = 0.34 and p = 0.29, respectively). D There were no significant differences between the groups in the total bilirubin level or prothrombin time/international normalized ratio on PODs 7 and 14. E The graft survival rates of the two groups were not significantly different (p = 0.24). LDLT living-donor liver transplantation; POD postoperative day; T.Bil total bilirubin; PT-INR prothrombin time/international normalized ratio
Impact of perioperative synbiotic treatment on postoperative sepsis occurrence
To identify independent risk factors for postoperative sepsis occurrence after LDLT under early enteral nutrition, we performed univariate and multivariate analyses that revealed that a recipient age of ≥ 65 years old and a lack of synbiotic treatment were independent risk factors (Table 2).
Status of sepsis-causing organisms after the introduction of early enteral nutrition and preemptive thoracic drainage
In this study, 13 recipients developed sepsis after LDLT. Blood culture tests identified 37 causative organisms belonging to 21 species that caused post-LDLT sepsis under early enteral nutrition and preemptive thoracic drainage. The details of sepsis-causing organisms are summarized in Fig. 3. Enterococcus spp. (n = 8; faecium [n = 5], faecalis [n = 2], and raffinosus), Staphylococcus spp. (n = 8; epidermidis [n = 3], aureus [methicillin-resistant staphylococcus aureus: n = 2], capitis [n = 2], and haemolyticus), Klebsiella spp. (n = 7; pneumonia [extended-spectrum β-lactamase (ESBL): n = 3], oxytoca [n = 2: ESBL and metallo β-lactamase], and aerogenes [n = 2]), Stenotrophomonas maltophilia (n = 3), Candida spp. (n = 2; albicans and krusei), Escherichia coli (ESBL: n = 2), Pseudomonas spp. (n = 2; aeruginosa and luteola), Serratia spp. (n = 2; marcescens and plymuthica), Acinetobactor baumannii, Cutibacterium acnes, and Lactobacillus spp. (all n = 1) were identified.
Current status of sepsis-causing organisms after LDLT. The pie chart reveals the sepsis-causing organisms found in 13 recipients. Enterococcus spp. and Staphylococcus spp. were the most common (21.6%), followed by Klebsiella spp. (18.9%) and Stenotrophomonas maltophilia (8.1%). Candida spp., Escherichia coli, Pseudomonas spp., and Serratia spp. each accounted for 5.4% of the abundance, and Acinetobactor baumannii, Cutibacterium acnes, and Lactobacillus spp. each accounted for 2.7%. LDLT living-donor liver transplantation
Discussion
In this study, perioperative synbiotic treatment significantly reduced the occurrence rate of post-LDLT sepsis (0% vs. 7.4%, p = 0.029) when the incidence of sepsis had already been reduced through the use of early enteral nutrition and preemptive thoracic drainage. There were no significant differences in the post-LDLT liver function or the occurrence rate of post-LDLT critical complications such as acute rejection and small-for-size graft syndrome (p = 0.34 and p = 0.29, respectively) between the synbiotic and non-synbiotic groups. Although the graft survival rate as a long-term postoperative outcome was not significantly different (p = 0.24) between the groups, the non-synbiotic group had longer postoperative hospital stays, suggesting that it is possible to complete the treatment of postoperative sepsis solely with postoperative management, although it requires a longer treatment period. Univariate and multivariate analyses revealed that lack of synbiotic treatment was an independent risk factor for post-LDLT sepsis occurrence.
This study also identified the sepsis-causing organisms found after LDLT without synbiotic treatment. Bacteria from the intestinal tract accounted for the majority of the identified organisms, suggesting that post-LDLT sepsis is often caused by bacterial translocation. A previous study [9] revealed an increase in the proportion of Enterococcus spp. in fecal cultures after LDLT, and the majority of their sepsis-causing organisms were microorganisms from the intestinal tract, such as Enterococcus spp. and Candida spp., in a slightly smaller control group (n = 25) than in this study. In LT, intraoperative ischemia or congestion of the intestinal tract related to the surgical technique, portal hypertension, and usage of antibiotics contribute to disruption of normal flora, resulting in increased bacterial translocation due to intestinal immune system dysregulation [20].
The main functions of synbiotic treatment are the implementation of colonization resistance in pathogenic germs, improvement of bowel motility and splanchnic blood flow, stimulation of enterocyte growth and mucus formation, modulation of intestinal inflammation, stabilization of the intestinal barrier, and stimulation of immune and non-immune mechanisms through competition with potential pathogens [7]. As a result, synbiotic treatment has been shown to significantly reduce the risk of postoperative infectious complications in patients undergoing elective abdominal surgery [21].
Regarding the duration of synbiotic administration, in most previous studies of LT, administration of synbiotics began postoperatively; in two studies, administration began on the second preoperative day [8, 20]. In contrast, administration in this study was initiated on the fifth preoperative day. Sugawara et al. examined the importance of preoperative synbiotic treatment [22], showing that preoperative treatment enhanced immune responses, attenuated systemic postoperative inflammatory responses, and improved the intestinal microbial environment, resulting in a significant reduction in postoperative infectious complications compared to patients who did not receive preoperative intervention (12.1% vs. 30.0%, p < 0.05). Another study revealed that synbiotic treatment for 1 week significantly increased the number of Bifidobacterium and Lactobacillus, and the abundance of these organisms in fecal microflora compared to before administration; however, there was no significant difference at 1 week and 2 weeks of administration [23]. These results suggest the importance of preoperative synbiotic treatment for a precise duration. The 5-day preoperative administration used in this study could be a strength over the 2-day administration used in previous LDLT studies. In addition, the gut microbiome varies by background disease, ethnicity, etc. [24]; therefore, this study can add value regarding the usefulness of synbiotic treatment in LDLT.
The main limitation of this study is its retrospective, small-cohort, and single-center design. The number of patients who could be administered treatment 5 days prior to surgery was limited, and it took time to enroll patients. In addition, it should be noted that the definition of sepsis in this study is based on our previous report [3]. We were also unable to investigate changes in the gut microbiota after synbiotic treatment. A prospective randomized control study will be performed in the near future to validate the results of this study and investigate the changes in the abundance of these organisms in the fecal microflora.
In conclusion, perioperative synbiotic treatment significantly reduced the occurrence of post-LDLT sepsis without adverse effects on postoperative outcomes, even with early enteral nutrition and preemptive thoracic drainage.
Abbreviations
- BMI:
-
Body mass index
- GV:
-
Graft volume
- LDLT:
-
Living-donor liver transplantation
- LT:
-
Liver transplantation
- POD:
-
Postoperative day
- RTBD:
-
Retrograde transhepatic biliary drainage
- SLV:
-
Standard liver volume
References
Fishman JA. Infection in solid-organ transplant recipients. N Engl J Med. 2007;357:2601–14.
Oliveira RA, Turrini RNT, Poveda VB. Risk factors for development of surgical site infections among liver transplantation recipients: an integrative literature review. Am J Infect Control. 2018;46:88–93.
Ikegami T, Shirabe K, Yoshiya S, Yoshizumi T, Ninomiya M, Uchiyama H, et al. Bacterial sepsis after living donor liver transplantation: the impact of early enteral nutrition. J Am Coll Surg. 2012;214:288–95.
Imai D, Ikegami T, Toshima T, Yoshizumi T, Yamashita Y, Ninomiya M, et al. Preemptive thoracic drainage to eradicate postoperative pulmonary complications after living donor liver transplantation. J Am Coll Surg. 2014;219:1134-42.e2.
Gibson GR, Roberfroid MB. Dietary modulation of the human colonic microbiota: introducing the concept of prebiotics. J Nutr. 1995;125:1401–12.
Rayes N, Seehofer D, Theruvath T, Mogl M, Langrehr JM, Nüssler NC, et al. Effect of enteral nutrition and synbiotics on bacterial infection rates after pylorus-preserving pancreatoduodenectomy: a randomized, double-blind trial. Ann Surg. 2007;246:36–41.
Zhang Y, Chen J, Wu J, Chalson H, Merigan L, Mitchell A. Probiotic use in preventing postoperative infection in liver transplant patients. Hepatobiliary Surg Nutr. 2013;2:142–7.
Mallick S, Kathirvel M, Nair K, Durairaj MS, Varghese CT, SivasankaraPillaiThankamonyAmma B, et al. A randomized, double-blinded, placebo-controlled trial analyzing the effect of synbiotics on infectious complications following living donor liver transplant-PREPRO trial. J Hepatobiliary Pancreat Sci. 2022;29:1264–73.
Eguchi S, Takatsuki M, Hidaka M, Soyama A, Ichikawa T, Kanematsu T. Perioperative synbiotic treatment to prevent infectious complications in patients after elective living donor liver transplantation: a prospective randomized study. Am J Surg. 2011;201:498–502.
Trone K, Rahman S, Green CH, Venegas C, Martindale R, Stroud A. Synbiotics and surgery: can prebiotics and probiotics affect inflammatory surgical outcomes? Curr Nutr Rep. 2023;12:238–46.
Rong L, Ch’ng D, Jia P, Tsoi KKF, Wong SH, Sung JJY. Use of probiotics, prebiotics, and synbiotics in non-alcoholic fatty liver disease: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2023;38:1682–94.
Rayes N, Seehofer D, Theruvath T, Schiller RA, Langrehr JM, Jonas S, et al. Supply of pre- and probiotics reduces bacterial infection rates after liver transplantation–a randomized, double-blind trial. Am J Transpl. 2005;5:125–30.
Toshima T, Yoshizumi T, Shimagaki T, Wang H, Kurihara T, Nagao Y, et al. Which is better to use “body weight” or “standard liver weight”, for predicting small-for-size graft syndrome after living donor liver transplantation? Ann Gastroenterol Surg. 2021;5:363–72.
Yonemura Y, Yoshizumi T, Inokuchi S, Kosai-Fujimoto Y, Harada N, Itoh S, et al. Predictor of outcome after living donor liver transplantation for patients with hepatocellular carcinoma beyond the Japan criteria. Ann Gastroenterol Surg. 2020;4:413–21.
Yoshiya S, Harada N, Tomiyama T, Takeishi K, Toshima T, Iguchi T, et al. The significant prognostic factors in prolonged intensive/high care unit stay after living donor liver transplantation. Transpl Proc. 2021;53:1630–8.
Yoshiya S, Shirabe K, Kimura K, Yoshizumi T, Ikegami T, Kayashima H, et al. The causes, risk factors, and outcomes of early relaparotomy after living-donor liver transplantation. Transplantation. 2012;94:947–52.
Yoshiya S, Harada N, Toshima T, Toshida K, Kosai Y, Tomino T, et al. Treatment strategy for hepatocellular carcinoma recurrence in the transplant era: Focusing on the Japan criteria. Surg Today. 2024;54:64–72.
Yoshiya S, Harada N, Toshima T, Toshida K, Kosai Y, Tomino T, et al. Treatment strategy for hepatocellular carcinoma recurrence in the transplant era: Focusing on the Japan criteria. Surg Today. 2024;54:64–72.
Tomino T, Harada N, Toshida K, Tomiyama T, Kosai Y, Kurihara T, et al. Effect of early enteral nutrition on graft loss after living donor liver transplantation: a propensity score matching analysis. Transpl Proc. 2023. https://doi.org/10.1016/j.transproceed.2023.07.029.
Jorgenson MR, Descourouez JL, Siodlak M, Tjugum S, Rice JP, Fernandez LA. Efficacy and safety of probiotics and synbiotics in liver transplantation. Pharmacotherapy. 2018;38:758–68.
Chowdhury AH, Adiamah A, Kushairi A, Varadhan KK, Krznaric Z, Kulkarni AD, et al. Perioperative probiotics or synbiotics in adults undergoing elective abdominal surgery: a systematic review and meta-analysis of randomized controlled trials. Ann Surg. 2020;271:1036–47.
Sugawara G, Nagino M, Nishio H, Ebata T, Takagi K, Asahara T, et al. Perioperative synbiotic treatment to prevent postoperative infectious complications in biliary cancer surgery: a randomized controlled trial. Ann Surg. 2006;244:706–14.
Shioiri T, Yahagi K, Nakayama S, Asahara T, Yuki N, Kawakami K, et al. The Effects of a synbiotic fermented milk beverage containing <i>Lactobacillus casei</i> Strain Shirota and Transgalactosylated Oligosaccharides on defecation frequency, intestinal microflora, organic acid concentrations, and putrefactive metabolites of sub-optimal health state volunteers: a randomized placebo-controlled cross-over study. Biosci Microflora. 2006;25:137–46.
Hsu CL, Schnabl B. The gut-liver axis and gut microbiota in health and liver disease. Nat Rev Microbiol. 2023;21:719–33.
Acknowledgements
We thank Lisa Oberding, MSc, from Edanz (https://jp.edanz.com/ac), for editing the draft of this manuscript.
Funding
This study was supported by JSPS KAKENHI (grant number JP-23K08214). The funding source had no role in the collection, analysis, or interpretation of the data, or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
SY participated in research design, data analysis, and writing of the manuscript. SI, TT, and TY contributed to discussion and reviewed the manuscript. YB and T. Izumi participated in the data analysis and interpretation. YT, NI, KT, YN, and T. Ishikawa participated in data collection.
Corresponding author
Ethics declarations
Conflict of interest
Prof. Tomoharu Yoshizumi is an editorial member of the journal. The other authors declare no conflicts of interest for this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yoshiya, S., Itoh, S., Toshima, T. et al. The impact of perioperative synbiotics treatment in living-donor liver transplantation after induction of early enteral nutrition. Surg Today (2024). https://doi.org/10.1007/s00595-024-02918-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00595-024-02918-7