Abstract
Purpose
This study tested the hypothesis that blood pressure responses would increase relative to force production in response to prolonged bouts of muscular work.
Methods
Fifteen individuals performed two minutes of static handgrip (SHG; 35% MVC), followed by three minutes of post-exercise-cuff-occlusion (PECO), before and after thirty minutes of rest (control), or rhythmic handgrip exercise (RHG) of the contralateral and ipsilateral forearms. Beat-by-beat recordings of mean arterial pressure (MAP), heart rate (HR), and handgrip force (kg) were averaged across one-minute periods at baseline, and minutes 5, 10, 15, 20, 25, and 30 of RHG. MAP was also normalized to handgrip force, providing a relative measure of exercise pressor responses (mmHg/kg). Hemodynamic responses to SHG and PECO were also compared before and after contralateral RHG, ipsilateral RHG, and control, respectively. Similar to the RHG trial, areas under the curve were calculated for MAP (blood pressure index; BPI) and normalized to the time tension index (BPInorm).
Results
HR and MAP significantly increased during RHG (15.3 ± 1.4% and 20.4 ± 3.2%, respectively, both p < 0.01), while force output decreased by up to 36.6 ± 8.0% (p < 0.01). This resulted in a 51.6 ± 9.4% increase in BPInorm during 30 min of RHG (p < 0.01). In contrast, blood pressure responses to SHG and PECO were unchanged following RHG (all p ≥ 0.07), and only the mean HR (4.2 ± 1.5%, p = 0.01) and ΔHR (67.2 ± 18.1%, p < 0.01) response to SHG were exaggerated following ipsilateral RHG.
Conclusions
The magnitude of exercise pressor responses relative to force production progressively increases during, but not following, prolonged bouts of muscular work.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As humans exercise, blood pressure increases via a combination of efferent and afferent neural pathways. The feed-forward pathway, referred to as “central command,” directly stimulates sympathetic premotor neurons within the ventrolateral medulla (VLM), eliciting robust increases in sympathetic outflow, blood pressure, and heart rate (Padley et al. 2007). In contrast, group III and IV afferent neurons originating at the skeletal muscle are sensitized by metabolic perturbations and mechanical distortions of the exercising muscle, leading to inhibition of baroreflex control at the nucleus of the solitary tract (NTS; Boscan and Paton 2005; Chen et al. 2009; Potts 2006; Potts et al. 1999), resetting the baroreflex upwards and further augmenting sympathetic outflow. The combination of these neural pathways, collectively termed the exercise pressor response, has been extensively studied as a primary contributor to the regulation of blood flow and oxygen transport during exercise in both animals and humans.
While the contribution of these pathways to blood pressure regulation during exercise is well understood, whether exercise pressor responses change across prolonged bouts of muscular work is less clear. A recent study by Dillon et al. (2020) reported a high degree of repeatability in the blood pressure responses to successive bouts of handgrip exercise (a common assessment of exercise pressor responses), as well as repeated bouts of post-exercise cuff occlusion (PECO; a common assessment of metaboreflex activation), which supports the notion that these responses would remain consistent across repeated trials. However, previous research has also demonstrated progressive increases in peripheral fatigue during muscular work (Alway et al. 1987; Decorte et al. 2012), eliciting compensatory increases in central motor drive and central command (Decorte et al. 2012; Mitchell et al. 1981; Seals and Enoka 1989), which would presumably augment blood pressure responses relative to force production. Thus, it would be reasonable to assume that the magnitude of the exercise pressor response would increase relative to muscular work during prolonged bouts of exercise. However, to the authors’ knowledge, no studies have directly evaluated the time-course of this response during prolonged bouts of rhythmic exercise in humans.
To that end, this study tested the hypothesis that blood pressure responses to handgrip exercise would be significantly augmented relative to force production during thirty-minute bouts of rhythmic handgrip exercise (RHG). If true, this would indicate that exercise blood pressure responses are prone to progressive increases during extended bouts of exercise, which would be an important consideration for prescribing exercise durations in individuals susceptible to acute bouts of extreme hypertension (i.e., individuals with essential hypertension or peripheral artery disease). Secondarily, we also aimed to determine the time-course of any potential alterations in these blood pressure responses by comparing exercise pressor and metaboreflex responses before and after thirty-minutes of ipsilateral RHG, contralateral RHG, and control (rest). The contralateral and ipsilateral RHG conditions were used as a method of partitioning the centrally mediated contributions to the blood pressure responses (i.e., central command and relay of afferent input through the central nervous system) from the combined effects of centrally- and peripherally mediated influences (i.e., metabolic perturbations and peripheral fatigue), as described previously (Stavres et al. 2020). We expected exercise pressor and metaboreflex responses to be exaggerated following ipsilateral RHG, but not contralateral RHG or control, indicating that prolonged muscular work exaggerates exercise pressor responses primarily via peripherally mediated mechanisms.
Methods
Study design and participants
This study followed a within-subjects, repeated measures design and required three total visits to the University of Southern Mississippi campus. A total of seventeen individuals were recruited for participation in this study, two of whom were excluded for medical reasons. All remaining participants arrived at each visit at least three hours postprandial, and having abstained from caffeine for eight hours, alcohol for twelve hours, and intense physical activity and over-the-counter medications for twenty-four hours. All subjects were apparently healthy, defined as having no known cardiovascular, metabolic, neurological, or renal disease, and reported taking no medications. Of note, this study included a multi-racial sample of subjects, with five White females (33%), six Black/African American (B/AA) females (40%), one White Hispanic female (7%), two White males (13%), and one B/AA male (7%). This sample closely represents the demographics of the surrounding Hattiesburg, MS region (39% White, 55% B/AA, and 4% Hispanic or Latino). The mean age of the sample was 21 ± 2 years, with a BMI of 25.2 ± 5.3 kg/m2, a resting blood pressure of 123 ± 9 mmHg / 77 ± 9 mmHg (systolic and diastolic, respectively), and a resting heart rate of 70 ± 10 bpm. The protocols used in this study were approved by the University of Southern Mississippi Institutional Review Board (IRB # 21–339), and all subjects provided written informed consent prior to participation. Of note, phase of menstrual cycle was not controlled in this study, but was recorded in ten female participants. Of the twelve female participants included in this study, the contralateral condition occurred during the luteal phase in six and follicular phase in three participants, the control condition occurred during the luteal phase in four and the follicular phase in five participants, and the ipsilateral condition occurred during the luteal phase in six and the follicular phase in three participants. One participant reported a non-occurring menstrual cycle.
Experimental protocol
As noted previously, this study required three total research visits, each of which represented a separate experimental condition. Each visit began with the assessment of maximal voluntary isometric handgrip force (MVC) of the non-dominant arm. Once the highest MVC was recorded (the highest value achieved across three attempts), participants performed a baseline assessment of exercise pressor and metaboreflex responses. This assessment began with a two-minute rest period, followed by two minutes of static handgrip exercise (SHG; assigned at 35% MVC) and three minutes of post exercise cuff occlusion (PECO; occlusion pressures ~ 200 mmHg). For the PECO trials, a 12 cm cuff was placed over the proximal portion of the upper arm. Beat by beat blood pressure and heart rate (HR) were collected continuously throughout the assessment period (described in more detail in the following section). Following baseline assessments, subjects then performed thirty minutes of either contralateral or ipsilateral RHG or rested quietly for thirty minutes (control). As referenced previously, the contralateral and ipsilateral RHG conditions were used as a method of partitioning centrally vs. peripherally mediated influences on exercise pressor responses. This method is based on the assumption that any changes in the magnitude of exercise pressor or metaboreflex responses would be influenced by a combination of peripheral factors, such as the accumulation of metabolic byproducts and peripheral fatigue within the active skeletal muscle, as well as central factors, such as changes in central command and the relay of afferent input through the central nervous system. Thus, any changes in exercise pressor or metaboreflex responses following contralateral RHG would be subject to these centrally mediated factors, but would be largely unaffected by localized metabolite accumulation or development of peripheral fatigue. The contralateral and ipsilateral conditions were performed in a counterbalanced order, with the control condition always occurring during the second visit. This counterbalancing procedure assured that the ipsilateral and contralateral condition were appropriately counterbalanced, and also assured that the control condition was appropriately counterbalanced with respect to the two experimental conditions (i.e., occurred before the ipsilateral condition in one participant but after the ipsilateral condition in the next). In both trials, RHG exercise was assigned at 35% of the participant’s MVC (assessed independently for the contralateral arm) and was performed at a 3:1 work-rest ratio controlled via a metronome (60 bpm). Lastly, after a ten-minute washout period (allowing brachial blood pressure to return to baseline), participants performed a final assessment of exercise pressor and metaboreflex activation of the non-dominant arm.
Instrumentation and data collection
Pressor responses were quantified by the absolute and relative blood pressure and HR responses during RHG, SHG and PECO. HR responses were recorded using a one-lead electrocardiogram and were calculated for each individual R-R interval. Blood pressure was recorded from the non-exercising arm via finger photoplethysmography (Finapres Nano, AD Instruments, Colorado Springs, CO) and was calibrated to brachial blood pressure collected prior to each baseline timepoint (Tango M2, SunTech Medical, Morrisville, NC). Mean arterial pressure (MAP) was calculated as the average of all samples recorded across each individual cardiac (R-R) interval, while systolic (SBP) and diastolic (DBP) blood pressures were calculated as the maximum and minimum values within each individual cardiac interval, respectively. Handgrip force was recorded using a standard handgrip dynamometer (Smedley Hand Dynamometer, Stoelting, Wood Dale, IL), which provided visual force-feedback to subjects via a video display. This video display included a visual guideline (assigned at the 35% MVC value for each participant), and participants were instructed to grip with enough force for the real-time force tracing to touch the established guideline, as illustrated in Fig. 1. All data were sampled at 600–2000 Hz using a multi-channel data acquisition system (PowerLab 8/35, AD Instruments, Colorado Springs, CO) and stored for offline data analysis using LabChart Version 8 Pro Software (AD Instruments, Colorado Springs, CO). All testing was performed in the supine position with the exercising arm resting in a neutral position with the hand at hip level.
Continuous recordings of heart rate (HR), beat-by-beat blood pressure (BP), and handgrip force (HG) during a period of rhythmic handgrip exercise (RHG). RHG was assigned at 35% of the maximal voluntary contraction, indicated by the green line on top of the shaded area. Participants contracted at a 3:1 work-to-rest ratio, which was maintained via a metronome
The magnitude of exercise pressor responses across a prolonged bout of muscular work were calculated using the following approach. First, MAP, SBP, DBP, HR, and mean handgrip force (kg) were each averaged across one-minute bins at baseline (immediately prior to RHG), and again at minutes 5, 10, 15, 20, 25, and 30 of each RHG trial. Delta scores were then calculated as the changes in blood pressure, HR, and handgrip force relative to the pre-exercise baseline, and the ipsilateral and contralateral RHG trials were combined to provide a single mean value for each time point. MAP was also normalized to the mean handgrip force at each time point (excluding baseline), providing a relative measure of exercise pressor response magnitude (MAPnorm; mmHg/kg).
To examine the recovery of exercise pressor responses following this prolonged bout of RHG, MAP, SBP, DBP, HR, and handgrip force were averaged across the SHG and PECO trials performed before (pre) and after (post) contralateral RHG, ipsilateral RHG, and control. As in the RHG trials, delta scores were calculated as the relative changes in blood pressure and HR from the two-minute period preceding SHG in both trials. Furthermore, a blood pressure index (BPI; mmHg*s) was calculated as areas under the curve for both the SHG and PECO periods, providing an overall index of the blood pressure response to each stimulus (the stimulus being defined as the force output during handgrip exercise). BPI responses during SHG were then normalized to the area under the curve for handgrip force (time-tension index; TTI), providing a relative index of exercise pressor response magnitude for SHG (BPInorm; mmHg/kg). This approach of normalizing blood pressure responses to force production has been employed in previous studies of exercise pressor responses (Stavres et al. 2022, 2023), and is supported by recent data describing the moderating role of absolute force output on the hemodynamic response to handgrip exercise and PECO (Lee et al. 2021a, b). Of note, one participant did not complete the ipsilateral trial (due to time-constraints), resulting in 14 participants’ data being included in the ipsilateral condition.
Statistical approach
To test the hypothesis that exercise pressor and metaboreflex responses would be potentiated during a thirty-minute bout of handgrip exercise, one-level repeated measures analyses of variance (RMANOVA) were used to examine changes in blood pressure and HR from baseline through minute 30 of RHG. Changes in handgrip force and MAPnorm were also compared between minutes 5, 10, 15, 20, 25, and 30 of RHG using one-way ANOVA. Any significant effects of time were examined further using post-hoc analyses employing a Sidak correction for multiple comparisons.
To test the hypothesis that ipsilateral RHG would augment pressor responses to SHG and PECO, two-level RMANOVA were used to examine changes in blood pressure (including BPI and BPInorm) and HR across time (baseline vs. post exercise) and conditions (contralateral vs. ipsilateral vs. control) during both handgrip and PECO. Similar to the 30-min RHG trials, any significant interactions or main effects of time or condition were further examined using post-hoc analyses employing a Sidak correction for multiple comparisons.
Lastly, to examine the potential influences of biological sex and race, each of the aforementioned ANOVA and RMANOVA procedures were repeated with sex and race included as independent between-factors grouping variables. Moreover, considering previous evidence describing the moderating role of absolute contractile forces in explaining sex differences in exercise pressor and metaboreflex responses (Lee et al. 2021a, b), the mean MVC (across both arms) was included as a covariate in the models examining sex as a between-factors comparison. Similar to the previous statistical analyses, any significant main effects of condition, time, or interactions were examined further using post-hoc comparisons employing a Sidak correction. All data are presented as means ± standard deviation (SD), and significance was accepted at p < 0.05. All statistical tests were performed using SPSS version 28.0 software (SPSS Statistics, IBM Corp., Armonk, NY).
Results
Responses to fatiguing rhythmic handgrip exercise
When blood pressure and HR responses were compared across time during RHG, results indicated significant main effects of time for the mean and ΔHR (both F = 18.88, p < 0.01; Fig. 2a, e), mean and ΔMAP (both F = 5.08, p < 0.01; Fig. 2b, f), mean and ΔSBP (both F = 2.91, p = 0.01; Fig. 2c, g), and mean and ΔDBP (both F = 6.02, p < 0.01; Fig. 2d, h) responses. Post-hoc comparisons revealed significant increases in MAP (20.4 ± 3.2%, p < 0.01), SBP (17.5 ± 3.2%, p < 0.01), and DBP (20.8 ± 2.6%, p < 0.01) during the first 5 min of exercise (all p < 0.01), which did not differ significantly from baseline or minute 5 thereafter (Fig. 2). HR also significantly increased at minute 5 (15.3 ± 1.4%, p < 0.01), and remained elevated through minutes 10, 15, 25, and 30 (all p < 0.01; Fig. 2a). In contrast to HR and blood pressure, handgrip force progressively decreased through thirty minutes of RHG (F = 10.18, p < 0.01; Fig. 2i, k), with maximum decreases occurring at minutes 25 (-36.6 ± 8.0%, p < 0.01) and 30 (-28.2 ± 5.9%, p < 0.01). This decrease in handgrip force, coupled with the increase in MAP, resulted in a progressively increasing MAPnorm response (F = 13.99, p < 0.01), reaching maximum increases of 51.6 ± 9.4% at minute 25 and 32.2 ± 7.2% at minute 30 (both p < 0.01; Fig. 2 j, l).
Panels a–d Heart rate (HR; a), mean arterial pressure (MAP; b), systolic blood pressure (SBP; c), and diastolic blood pressure (DBP; d) compared from baseline (BL) through thirty minutes of rhythmic handgrip exercise (RHG). Panels e–h represent delta scores (Δ) for the same variables. Panels i, j represent handgrip force (HG; i) and mean arterial pressure normalized to handgrip force (MAPnorm; j), and panels k, l represent ΔHG force and ΔMAPnorm, respectively. *, significantly different from BL; †, significantly different from the 5-min time point; ‡, significantly different from the 10-min time point. Significance accepted at p < 0.05. Data presented as mean ± standard deviation
Responses to static handgrip and metaboreflex activation
When the mean pressor responses to SHG were compared across time and between conditions, results indicated no significant main effect of time or condition for any mean or relative blood pressure response (all p ≥ 0.09, Fig. 3a, d). In contrast, significant time by condition interactions were observed for the mean HR (F = 4.81, p = 0.01) and ΔHR (F = 3.46, p = 0.04) responses during handgrip. These interactions can be explained by a 4.2 ± 1.5% increase in the mean HR response (p = 0.01; Fig. 3b) and a 67.2 ± 18.1% increase in the ΔHR response (p < 0.01; Fig. 3e) following ipsilateral handgrip exercise, which were not observed in the contralateral or control conditions (all p ≥ 0.09). When the total BPI and BPInorm responses were compared across time and between trials, results indicated no significant main effects of time, condition, or interactions (all p ≥ 0.07; Fig. 3c, f).
Mean arterial pressure (MAP; a) and heart rate (HR; b) responses to static handgrip (SHG), as well as the delta scores (Δ) for MAP (d) and HR (e), compared before and after thirty minutes of contralateral (Contra) forearm exercise, ipsilateral (Ipsi) forearm exercise, and control. Panel c illustrates the total blood pressure index (BPI), while panel f illustrates the normalized BPI (BPInorm). *, significantly different from pre-exercise (p < 0.05)
When the responses to PECO were compared across time and between conditions, results indicated significant main effects of condition (F = 3.65, p = 0.04) and time (F = 6.04, p = 0.02) for the mean HR response, and a condition by time interaction for the ΔHR response (F = 3.80, p = 0.03). These effects can be explained by a significantly attenuated mean HR response following the ipsilateral trial (− 3.9 ± 0.8%, p < 0.01; Fig. 4b), which was not observed in the contralateral or control trials (both p ≥ 0.15), as well as a reversal of the ΔHR response following the contralateral trial (p = 0.01; Fig. 4e) which was not observed in the ipsilateral or control trials (both p ≥ 0.84). In contrast, no significant main effects of time or condition were observed for any of the mean or Δ blood pressure responses (all p ≥ 0.27; Fig. 4a, d) or BPI responses (all p ≥ 0.23; Fig. 4c) during PECO. To examine if changes in contraction intensity may have influenced differences (or lack thereof) in PECO responses across time and between conditions, a separate condition (3) by time (2) RMANOVA was performed on HG and TTI responses during SHG. Results indicated no significant main effects of time (p ≥ 0.07) or condition by time interactions (p ≥ 0.07) for HG or TTI. However, a main effect of condition was observed for both HG (F = 3.53, p = 0.04) and TTI (F = 3.39, p = 0.04), explained by a significantly lower mean HG force (9.4 ± 3.8 kg vs. 8.4 ± 3.4 kg, pre vs. post, respectively, p = 0.01) and TTI (1145.4 ± 452.4 kg*s vs. 1009.6 vs. 404.6 kg*s, pre vs. post, respectively, p = 0.01) following ipsilateral RHG only.
Mean arterial pressure (MAP; a) and heart rate (HR; b) responses to post-exercise cuff occlusion (PECO), as well as the delta scores (Δ) for MAP (d) and HR (e), compared before and after thirty minutes of contralateral (Contra) forearm exercise, ipsilateral (Ipsi) forearm exercise, and control. Panel c illustrates the total blood pressure index (BPI). *, significantly different from pre-exercise (p < 0.05)
Influence of biological sex and race
When race was included as a between-factors comparison during the 30-min RHG comparisons, results indicated no significant main effects of group, nor any significant time by race interactions for any dependent variable (all p ≥ 0.27). In contrast, a significant three-way (condition by time by race) interaction was observed for the HR (F = 5.01, p = 0.01) and ΔHR (F = 3.74, p = 0.03) responses during SHG compared before and after RHG. When examined further, this could be explained by significant decreases in the absolute HR response to SHG following the contralateral condition in B/AA participants (85 ± 8 bpm vs. 80 ± 8 bpm, pre vs. post, respectively, p = 0.02) that was not observed in White participants (p = 0.62), a significant increase in the absolute HR response to SHG following the ipsilateral condition in White participants (83 ± 10 bpm vs. 87 ± 13 bpm, pre vs. post, respectively, p < 0.01) that was not observed in B/AA participants (p = 0.39), and significant increases in the ΔHR response following the contralateral (11 ± 6 bpm vs. 16 ± 5, pre vs. post, respectively, p = 0.04), control (10 ± 6 bpm vs. 15 ± 5 bpm, pre vs. post, respectively, p = 0.2), and ipsilateral (10 ± 7 bpm vs. 18 ± 9 bpm, pre vs. post, respectively, p < 0.01) conditions in White participants that were not observed in B/AA participants (all p ≥ 0.12). Likewise, a significant three-way interaction was also observed for the absolute HR response to PECO (F = 7.59, p = 0.01), explained by a significant decrease in the absolute HR response to PECO following the control condition in B/AA participants (80 ± 10 bpm vs. 75 ± 9 bpm, pre vs. post, respectively, p < 0.01) that was not observed in White participants (p = 0.22), and a significant decrease in the absolute HR response to PECO in the ipsilateral condition in White participants (71 ± 9 bpm vs. 68 ± 7 bpm, pre vs. post, respectively, p < 0.01) that was not observed in B/AA participants (p = 0.056).
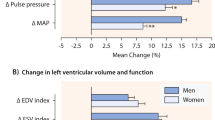
When sex was included as a between-factors comparison for the 30-min RHG comparisons, results indicated significant time by sex interactions for absolute and ΔHG force (both F = 8.47, p < 0.01), absolute and ΔMAP (both F = 3.93, p < 0.01), absolute and ΔSBP (both F = 4.81, p < 0.01), and absolute and ΔDBP (both F = 3.64, p < 0.02). However, covarying for mean MVC abolished each of these time by sex interactions (all p ≥ 0.24). Likewise, when sex was included as a between-factors grouping variable in the comparisons of pressor responses to SHG and PECO before and after RHG, results indicated significant three-way (condition by time by sex) interactions for the absolute DBP (F = 3.61, p = 0.04) and ΔHR (F = 4.21, p = 0.02) response to SHG, as well as the ΔHR response to PECO (F = 3.45, p = 0.04). However, as was the case for the 30-min handgrip trials, these interactions were completely abolished after covarying for mean MVC (all p ≥ 0.09).
Discussion
This study tested the overall hypothesis that prolonged muscular work would exaggerate exercise pressor responses evoked from the same muscles, both during and after exercise. Our results partially support this hypothesis. As illustrated in Fig. 2, blood pressure significantly increased during 30 min of handgrip, and did not significantly decrease, despite significant decreases in force production. This resulted in a significant increase in exercise pressor response magnitude (mmHg/kg; Fig. 2j, l), which progressively increased throughout the RHG period. However, in contrast to the changes observed during exercise, no significant differences were observed for the blood pressure responses to SHG or PECO following RHG. Collectively, these data would suggest that the magnitude of exercise pressor responses increases during prolonged bouts of muscular work, but quickly recovers thereafter. These findings extend our understanding of blood pressure regulation during exercise and expand on previous works describing the interactions between acute bouts of exercise and the blood pressure regulation. This will be discussed further in the following sections.
Changes in exercise pressor response magnitude during exercise
The observation that the magnitude of blood pressure responses increases relative to force production during prolonged bouts of exercise expands on prior studies within this field, and there are a few key factors that may contribute to this effect. The first, and most likely, is an increase in central command occurring secondary to an accumulation of peripheral muscular fatigue. As noted previously, it is well-documented that intense exercise contributes to inhibition of excitation–contraction coupling mechanisms (Allen et al. 2002; Potma et al. 1995; Rockenfeller et al. 2020), which leads to an increase in the central motor drive (and thus, central command) required to achieve the same absolute force production (Decorte et al. 2012; Mitchell et al. 1981; Seals and Enoka 1989). Seals et al. (Seals and Enoka 1989) demonstrated this convincingly by reporting concomitant increases in electromyographic activity of the forearm muscles, muscle sympathetic nerve activity, and mean arterial pressure across acute bouts of fatiguing isometric handgrip exercise. Considering this evidence, it is most plausible that the increase in MAPnorm observed in the present study can be explained by muscle fatigue related increases in central command that persist across repeated contractions.
Another potential factor could be an accelerated accumulation of metabolic byproducts, thus increasing activation of metabo-sensitive afferents. Handgrip intensities of ≥ 30% MVC have been shown to significantly decrease skeletal muscle oxygenation during exercise (Celie et al. 2012; Nell et al. 2020), resulting from a combination of increased metabolic demand and increased intramuscular pressure (Barnes 1980; Wigmore et al. 2004). The 3:1 work-rest ratio used in the present study is also likely to maximize this time-under-tension stimulus and limited washout periods, thus promoting the accumulation of metabolic byproducts. In such case, an increase in the excitation of metabosensitive afferents would presumably lead to an increase in excitatory input at the medulla (Potts 2006; Potts et al. 1999), further increasing sympathetic outflow.
Lastly, we are also not able to discount any potential influence of anticipatory responses, which can independently elicit increases in blood pressure (Green et al. 2007). It is interesting that force production does seem to recover slightly from minute 25 to minute 30 of RHG, and this corresponds to a reciprocal decrease in MAPnorm (Fig. 2). It is also interesting that similar responses are observed for power output at the end of a 5k time trial (Hureau et al. 2019; Paradis-Deschênes et al. 2020). Therefore, while speculative, it may also be possible that the participant’s perception of the exercise also contributes to changes in the magnitude of exercise pressor responses.
Another interesting question posed by these findings is whether this response is beneficial, detrimental, or irrelevant to exercise performance. It is generally understood that the exercise pressor response is necessary for maintaining adequate blood flow to working muscles, and without an in-tact pressor response, working muscle are prone to accelerated peripheral fatigue responses (Amann et al. 2010, 2011, 2015; Hureau et al. 2019). Therefore, it would be reasonable to suspect this increase in exercise pressor response magnitude to facilitate oxygen transport to the active muscle during exercise, thus promoting exercise tolerance and performance. However, we must also consider two other factors that run counter to this argument. First, prior evidence has demonstrated that the vascular beds of the active skeletal muscle, which typically experience net vasodilation via functional sympatholysis (Dinenno and Joyner 2004; Moynes et al. 2013; Tschakovsky and Hughson 2003), are still subject to the influences of sympathetic vasoconstriction. Therefore, it would also be reasonable to suspect that an over-exaggeration of sympathetic responses (leading to exaggerated blood pressure responses) would restrict active muscle blood flow, thus accelerating peripheral fatigue and impairing exercise tolerance. Second, feedback from group III and IV muscle afferents have been shown to inhibit central motor drive to active muscles (Amann and Dempsey 2008; Amann and Dempsey 2008; Amann et al. 2009), thus limiting force production (relative to motor drive). Thus, if the exaggeration of exercise pressor response magnitude is explained by an increased activation of metabosensitive afferents, this may also contribute to a concurrent decrease in force production. How these three potential factors interact with one another to influence exercise performance during prolonged muscular work is worthy of further investigation.
Post-exercise responses
In contrast to the changes observed during exercise, no changes in exercise pressor or metaboreflex responses were observed following ipsilateral or contralateral RHG. This generally agrees with previous work from our group reporting a preservation of exercise pressor responses following non-fatiguing locomotor exercise (Stavres et al. 2020), and the work of others demonstrating highly repeatable blood pressure responses during successive bouts of SHG (Dillon et al. 2020). Likewise, a recent study from Zambolin et al. (2023) reported no significant differences in cardiovascular responses to isometric knee extension or PECO two days following exercise induced muscle damage (via eccentric exercise), but did report significant associations between indices of pain and effort (i.e., rating of perceived exertion and subject pain responses) and the change in MAP during exercise. The authors postulate that the association between indices of pain and MAP changes are indicative of a positive relationship between afferent activity and blood pressure responses to exercise in the presence of exercise induced hyperalgesia (a.k.a. delayed onset muscle soreness, or DOMS). This would also be supported by other works reporting an upregulation of P2X4 gene expression following eccentric exercise (Zambolin et al. 2022), as well as a mechanosensory role of acid sensing ion channels (particularly ASIC3 subunits) in mediating DOMS (Matsubara et al. 2019). On the other hand, other studies have demonstrated no changes in blood pressure responses to acute capsaicin infusion following EIMD (Queme et al. 2013). Collectively, this may indicate that exercise induced muscle damage elicits acute increases in the activity of ASICs and purinergic signaling pathways, which may contribute to increases and mechanical nociception. Indeed, recent studies have supported a role of ASICs in contributing to both the mechanoreflex (Butenas et al. 2022) and baroreflex function (Lu et al. 2009). In contrast, the lack of change in capsaicin responses reported by Queme et al. (2013) likely reflects no significant influence of exercise induced muscle damage on metaboreflex responses. While the RHG protocol in the present study was likely not sufficient to elicit muscle damage, the lack of changes in metaboreflex responses would nevertheless agree with the present findings.
In contrast to the lack of change in blood pressure responses, the absolute and ΔHR responses to SHG were significantly exaggerated following ipsilateral RHG only (Fig. 3a, c). Considering prior evidence indicating that central command influences HR responses to a greater degree than changes in vascular tone (Nobrega et al. 1994), this exaggerated heart rate response may represent a compensatory increase in central command secondary to a residual level of peripheral fatigue. It is also worth noting that ΔHR responses were significantly elevated following the ipsilateral RHG condition in White, but not B/AA participants. This may indicate differences in the influence of acute exercise on the relative contributions of HR and peripheral vasoconstriction to blood pressure regulation between B/AA and White individuals, with White individuals relying more heavily on increases in HR to reach target blood pressure values following prolonged ipsilateral limb exercise. This would agree with prior evidence indicating that sympathetic vasoconstriction is more pronounced in B/AA individuals compared to White individuals (Barbosa et al. 2018; Ray and Monahan 2002).
Regarding metaboreflex responses, a recent study by Lee et al. (2023) demonstrated significantly attenuated metaboreflex responses 24-h following high-volume eccentric exercise. In this study, muscular weakness was implicated as the primary contributor to attenuated PECO responses (confirmed via reduced MVC and potentiated twitch), which, at first glance, would run counter to our findings. However, there is a key distinction that supports the findings of both studies. In the study by Lee et al. (2023), eccentric exercise was used as a method of eliciting muscle weakness, which the authors hypothesized would translate to reduction in peak force output, thus reducing the absolute workload of the relative exercise stimulus preceding PECO. By reducing the absolute intensity of the muscular stimulus, the metabolic stimulus during PECO was also reduced, which supports an uncoupling of relative intensities and metabolic perturbations. In other words, assigning 35% MVC may not always elicit the same metaboreflex response, particularly if the absolute workload differs considerably across trials. This notion is also supported by other work from the same authors, in which differences in PECO responses between males and females are abolished by covarying for MVC (Lee et al. 2021b). This same argument could be inverted in support of our findings. In the present study, force production was assigned as 35% of the pre-exercise MVC, and therefore, the same absolute intensity was assigned pre- and post-RHG. If the absolute workload preceding PECO is, in fact, the primary contributor the magnitude of metaboreflex responses (at least compared relative workloads), we should expect to see similar PECO responses before and after RHG.
Practical implications
From a practical standpoint, the findings from this study may be useful for improving exercise programming, particularly for resistance exercise in individuals in whom acute hypertensive insults are contraindicated. As noted previously, it is generally understood that blood pressure increases during exercise in an intensity-dependent manner. Understanding this, current exercise professionals can modulate blood pressure responses by reducing workloads and increasing overall volume (i.e., sets and repetitions). However, the results from the present study would suggest that the relationship between muscular work and blood pressure is altered during a single bout of exercise, and it may be possible that the blood pressure responses to the same absolute workload (i.e., bench press or squat) become exaggerated as fatigue develops. A possible method of circumventing these issues is to prescribe exercise modalities that allow individuals to adjust workloads in real-time, thus compensating for fatigue and potentially avoiding substantially exaggerated blood pressure responses.
These findings may also have practical implications in clinical settings. Certain clinical populations, such as individuals with peripheral artery disease (Luck et al. 2017; Stavres et al. 2019), diabetes (Regensteiner et al. 2009; Scott et al. 2008), and metabolic syndrome (Dutra-Marques et al. 2021; Stavres et al. 2023) demonstrate significantly exaggerated blood pressure responses to exercise. It may be possible that some of these patient populations demonstrate a steeper incline in the exercise pressor response magnitude during continuous exercise, contributing to the observed exaggeration in blood pressure responses during exercise. If so, it would then be important to know if this exaggerated response facilitates or inhibits exercise tolerance, as described above. Ultimately, it would be important to understand if exercise tolerance can be improved by modulation of exercise pressor responses, particularly in these clinical populations.
Limitations
As is the case with any study, certain limitations must be considered while interpreting these findings. First, the lack of MSNA and peripheral blood flow recordings limit the interpretation of these results. Including peripheral blood flow measures would have permitted the calculation of vascular conductance/resistance, which allow for a deeper examination of the contributors to the reported changes in blood pressure and heart rate. Likewise, MSNA data would have permitted the calculation of sympathetic-blood pressure transduction, providing a more comprehensive description of the overall sympathetic responses to RHG, SHG, and PECO. The lack of neuromuscular assessments is also a limitation to this study. Specifically, peripheral fatigue was not quantified using potentiated twitch techniques or neuromuscular stimulation, nor was voluntary activation quantified or electromyography data collected. Therefore, while we cannot make direct inferences regarding peripheral fatigue, given the ~ 37% decrease in force output during RHG, we can infer that the difficulty of the exercise increased throughout the 30-min trial, whether that be due to psychological discomfort or physiological alterations. Lastly, menstrual cycle was not controlled in this study, and therefore, may have contributed to variations in the pressor responses observed in female participants.
Perspectives and significance
This study tested the overall hypothesis that exercise pressor responses would be exaggerated during and after a prolonged bout of muscular work. Our results indicate that blood pressure responses are exaggerated relative to force production throughout thirty-minutes of RHG, but no differences in blood pressure responses to SHG or PECO are observed following exercise. From these results, we conclude that exercise pressor response magnitude significantly increases during prolonged exercise, but recovers quickly thereafter. This information should be taken into consideration when prescribing exercise to individuals susceptible to acute bouts of severe hypertension.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to data sharing policies of the host institution. However, data may be made available by the corresponding author upon reasonable request, and with the permission of the University of Southern Mississippi.
References
Allen DG, Kabbara AA, Westerblad H (2002) Muscle fatigue: the role of intracellular calcium stores. Can J Appl Physiol 27(1):83–96. https://doi.org/10.1139/h02-006
Alway SE, Hughson RL, Green HJ, Patla AE, Frank JS (1987) Twitch potentiation after fatiguing exercise in man. Eur J Appl Physiol Occup Physiol 56(4):461–466. https://doi.org/10.1007/bf00417776
Amann M, Dempsey JA (2008) Locomotor muscle fatigue modifies central motor drive in healthy humans and imposes a limitation to exercise performance. J Physiol 586(1):161–173. https://doi.org/10.1113/jphysiol.2007.141838
Amann M, Proctor LT, Sebranek JJ, Eldridge MW, Pegelow DF, Dempsey JA (2008) Somatosensory feedback from the limbs exerts inhibitory influences on central neural drive during whole body endurance exercise. J Appl Physiol 105(6):1714–1724. https://doi.org/10.1152/japplphysiol.90456.2008
Amann M, Proctor LT, Sebranek JJ, Pegelow DF, Dempsey JA (2009) Opioid-mediated muscle afferents inhibit central motor drive and limit peripheral muscle fatigue development in humans. J Physiol 587(1):271–283. https://doi.org/10.1113/jphysiol.2008.163303
Amann M, Blain GM, Proctor LT, Sebranek JJ, Pegelow DF, Dempsey JA (2010) Group III and IV muscle afferents contribute to ventilatory and cardiovascular response to rhythmic exercise in humans. J Appl Physiol 109(4):966–976. https://doi.org/10.1152/japplphysiol.00462.2010
Amann M, Blain GM, Proctor LT, Sebranek JJ, Pegelow DF, Dempsey JA (2011) Implications of group III and IV muscle afferents for high-intensity endurance exercise performance in humans. J Physiol 589(Pt 21):5299–5309. https://doi.org/10.1113/jphysiol.2011.213769
Amann M, Sidhu SK, Weavil JC, Mangum TS, Venturelli M (2015) Autonomic responses to exercise: group III/IV muscle afferents and fatigue. Auton Neurosci 188:19–23. https://doi.org/10.1016/j.autneu.2014.10.018
Barbosa TC, Kaur J, Stephens BY, Akins JD, Keller DM, Brothers RM, Fadel PJ (2018) Attenuated forearm vascular conductance responses to rhythmic handgrip in young African-American compared with Caucasian-American men. Am J Physiol Heart Circ Physiol 315(5):H1316-h1321. https://doi.org/10.1152/ajpheart.00387.2018
Barnes WS (1980) The relationship between maximum isometric strength and intramuscular circulatory occlusion. Ergonomics 23(4):351–357. https://doi.org/10.1080/00140138008924748
Boscan P, Paton JF (2005) Excitatory convergence of periaqueductal gray and somatic afferents in the solitary tract nucleus: role for neurokinin 1 receptors. Am J Physiol Regul Integr Comp Physiol 288(1):R262-269. https://doi.org/10.1152/ajpregu.00328.2004
Butenas ALE, Rollins KS, Parr SK, Hammond ST, Ade CJ, Hageman KS, Musch TI, Copp SW (2022) Novel mechanosensory role for acid sensing ion channel subtype 1a in evoking the exercise pressor reflex in rats with heart failure. J Physiol 600(9):2105–2125. https://doi.org/10.1113/jp282923
Celie B, Boone J, Van Coster R, Bourgois J (2012) Reliability of near infrared spectroscopy (NIRS) for measuring forearm oxygenation during incremental handgrip exercise. Eur J Appl Physiol 112(6):2369–2374. https://doi.org/10.1007/s00421-011-2183-x
Chen CY, Bechtold AG, Tabor J, Bonham AC (2009) Exercise reduces GABA synaptic input onto nucleus tractus solitarii baroreceptor second-order neurons via NK1 receptor internalization in spontaneously hypertensive rats. J Neurosci 29(9):2754–2761. https://doi.org/10.1523/JNEUROSCI.4413-08.2009
Decorte N, Lafaix PA, Millet GY, Wuyam B, Verges S (2012) Central and peripheral fatigue kinetics during exhaustive constant-load cycling. Scand J Med Sci Sports 22(3):381–391. https://doi.org/10.1111/j.1600-0838.2010.01167.x
Dillon GA, Lichter ZS, Alexander LM, Vianna LC, Wang J, Fadel PJ, Greaney JL (2020) Reproducibility of the neurocardiovascular responses to common laboratory-based sympathoexcitatory stimuli in young adults. J Appl Physiol 129(5):1203–1213. https://doi.org/10.1152/japplphysiol.00210.2020
Dinenno FA, Joyner MJ (2004) Combined NO and PG inhibition augments alpha-adrenergic vasoconstriction in contracting human skeletal muscle. Am J Physiol Heart Circ Physiol 287(6):H2576–H2584
Dutra-Marques AC, Rodrigues S, Cepeda FX, Toschi-Dias E, Rondon E, Carvalho JC, Alves M, Braga A, Rondon M, Trombetta IC (2021) exaggerated exercise blood pressure as a marker of baroreflex dysfunction in normotensive metabolic syndrome patients. Front Neurosci 15:680195. https://doi.org/10.3389/fnins.2021.680195
Green AL, Wang S, Purvis S, Owen SL, Bain PG, Stein JF, Guz A, Aziz TZ, Paterson DJ (2007) Identifying cardiorespiratory neurocircuitry involved in central command during exercise in humans. J Physiol 578(Pt 2):605–612. https://doi.org/10.1113/jphysiol.2006.122549
Hureau TJ, Weavil JC, Thurston TS, Wan HY, Gifford JR, Jessop JE, Buys MJ, Richardson RS (1985) Amann M (2019) Pharmacological attenuation of group III/IV muscle afferents improves endurance performance when oxygen delivery to locomotor muscles is preserved. J Appl Physiol 127(5):1257–1266. https://doi.org/10.1152/japplphysiol.00490.2019
Lee JB, Lutz W, Omazic LJ, Jordan MA, Cacoilo J, Garland M, Power GA, Millar PJ (2021a) Blood pressure responses to static and dynamic knee extensor exercise between sexes: role of absolute contraction intensity. Med Sci Sports Exerc 53(9):1958–1968. https://doi.org/10.1249/mss.0000000000002648
Lee JB, Notay K, Seed JD, Nardone M, Omazic LJ, Millar PJ (2021b) Sex differences in muscle metaboreflex activation after static handgrip exercise. Med Sci Sports Exerc 53(12):2596–2604. https://doi.org/10.1249/mss.0000000000002747
Lee JB, Katerberg C, Bommarito J, Power GA, Millar PJ (2023) Blood pressure responses to post-exercise circulatory occlusion are attenuated following exercise-induced muscle weakness. Med Sci Sports Exerc. https://doi.org/10.1249/mss.0000000000003182
Lu Y, Ma X, Sabharwal R, Snitsarev V, Morgan D, Rahmouni K, Drummond HA, Whiteis CA, Costa V, Price M, Benson C, Welsh MJ, Chapleau MW, Abboud FM (2009) The ion channel ASIC2 is required for baroreceptor and autonomic control of the circulation. Neuron 64(6):885–897. https://doi.org/10.1016/j.neuron.2009.11.007
Luck JC, Miller AJ, Aziz F, Radtka JF 3rd, Proctor DN, Leuenberger UA, Sinoway LI, Muller MD (2017) Blood pressure and calf muscle oxygen extraction during plantar flexion exercise in peripheral artery disease. J Appl Physiol 123(1):2–10. https://doi.org/10.1152/japplphysiol.01110.2016
Matsubara T, Hayashi K, Wakatsuki K, Abe M, Ozaki N, Yamanaka A, Mizumura K, Taguchi T (2019) Thin-fibre receptors expressing acid-sensing ion channel 3 contribute to muscular mechanical hypersensitivity after exercise. Eur J Pain 23(10):1801–1813. https://doi.org/10.1002/ejp.1454
Mitchell JH, Schibye B, Payne FC III, Saltin B (1981) Response of arterial blood pressure to static exercise in relation to muscle mass, force development, and electromyographic activity. Circ Res 48(6, Suppl. I):I70–I75
Moynes J, Bentley RF, Bravo M, Kellawan JM, Tschakovsky ME (2013) Persistence of functional sympatholysis post-exercise in human skeletal muscle. Front Physiol 4:131. https://doi.org/10.3389/fphys.2013.00131
Nell HJ, Castelli LM, Bertani D, Jipson AA, Meagher SF, Melo LT, Zabjek K, Reid WD (2020) The effects of hypoxia on muscle deoxygenation and recruitment in the flexor digitorum superficialis during submaximal intermittent handgrip exercise. BMC Sports Sci Med Rehabil 12(1):16. https://doi.org/10.1186/s13102-020-00163-2
Nobrega AC, Williamson JW, Friedman DB, Araujo CG, Mitchell JH (1994) Cardiovascular responses to active and passive cycling movements. Med Sci Sports Exerc 26(6):709–714
Padley JR, Kumar NN, Li Q, Nguyen TBV, Pilowsky PM, Goodchild AK (2007) Central command regulation of circulatory function mediated by descending pontine cholinergic inputs to sympathoexcitatory rostral ventrolateral medulla neurons. Circ Res 100(2):284–291. https://doi.org/10.1161/01.RES.0000257370.63694.73
Paradis-Deschênes P, Joanisse DR, Mauriège P, Billaut F (2020) Ischemic preconditioning enhances aerobic adaptations to sprint-interval training in athletes without altering systemic hypoxic signaling and immune function. Front Sports Act Living 2:41. https://doi.org/10.3389/fspor.2020.00041
Potma EJ, van Graas IA, Stienen GJ (1995) Influence of inorganic phosphate and pH on ATP utilization in fast and slow skeletal muscle fibers. Biophys J 69(6):2580–2589. https://doi.org/10.1016/s0006-3495(95)80129-3
Potts JT (2006) Inhibitory neurotransmission in the nucleus tractus solitarii: implications for baroreflex resetting during exercise. Exp Physiol 91(1):59–72. https://doi.org/10.1113/expphysiol.2005.032227
Potts JT, Fuchs IE, Li J, Leshnower B, Mitchell JH (1999) Skeletal muscle afferent fibres release substance P in the nucleus tractus solitarii of anaesthetized cats. J Physiol 514:829–841
Queme F, Taguchi T, Mizumura K, Graven-Nielsen T (2013) Muscular heat and mechanical pain sensitivity after lengthening contractions in humans and animals. J Pain 14(11):1425–1436. https://doi.org/10.1016/j.jpain.2013.07.010
Ray CA, Monahan KD (2002) Sympathetic vascular transduction is augmented in young normotensive blacks. J Appl Physiol 92(2):651–656
Regensteiner JG, Bauer TA, Reusch JE, Quaife RA, Chen MY, Smith SC, Miller TM, Groves BM, Wolfel EE (2009) Cardiac dysfunction during exercise in uncomplicated type 2 diabetes. Med Sci Sports Exerc 41(5):977–984. https://doi.org/10.1249/MSS.0b013e3181942051
Rockenfeller R, Günther M, Stutzig N, Haeufle DFB, Siebert T, Schmitt S, Leichsenring K, Böl M, Götz T (2020) Exhaustion of skeletal muscle fibers within seconds: incorporating phosphate kinetics into a hill-type model. Front Physiol 11:306. https://doi.org/10.3389/fphys.2020.00306
Scott JA, Coombes JS, Prins JB, Leano RL, Marwick TH, Sharman JE (2008) Patients with type 2 diabetes have exaggerated brachial and central exercise blood pressure: relation to left ventricular relative wall thickness. Am J Hypertens 21(6):715–721. https://doi.org/10.1038/ajh.2008.166
Seals DR, Enoka RM (1989) Sympathetic activation is associated with increases in EMG during fatiguing exercise. J Appl Physiol 66(1):88–95
Stavres J, Sica CT, Blaha C, Herr M, Wang J, Pai S, Cauffman A, Vesek J, Yang QX, Sinoway LI (2019) The exercise pressor reflex and active O2 transport in peripheral arterial disease. Physiol Rep 7(20):e14243. https://doi.org/10.14814/phy2.14243
Stavres J, Luck JC, Ducrocq GP, Cauffman AE, Pai S, Sinoway LI (2020) Central and peripheral modulation of exercise pressor reflex sensitivity after nonfatiguing work. Am J Physiol Regul Integr Comp Physiol 319(5):R575-r583. https://doi.org/10.1152/ajpregu.00127.2020
Stavres J, Luck JC, Hamaoka T, Blaha C, Cauffman AE, Dalton P, Herr MD, Ruiz-Velasco V, Carr Z, Janicki P, Cui J (2022) A 10mg dose of amiloride increases time to failure during blood-flow-restricted plantar flexion in healthy adults without influencing blood pressure. Am J Physiol Regul Integr Comp Physiol. https://doi.org/10.1152/ajpregu.00190.2022
Stavres J, Aultman RA, Brandner CF, Newsome TQA, Vallecillo-Bustos A, Wise HL, Henderson A, Stanfield D, Mannozzi J, Graybeal AJ (2023) Hemodynamic responses to handgrip and metaboreflex activation are exaggerated in individuals with metabolic syndrome independent of resting blood pressure, waist circumference, and fasting blood glucose. Front Physiol. https://doi.org/10.3389/fphys.2023.1212775
Tschakovsky ME, Hughson RL (2003) Rapid blunting of sympathetic vasoconstriction in the human forearm at the onset of exercise. J Appl Physiol 94(5):1785–1792
Wigmore DM, Damon BM, Pober DM, Kent-Braun JA (2004) MRI measures of perfusion-related changes in human skeletal muscle during progressive contractions. J Appl Physiol 97(6):2385–2394. https://doi.org/10.1152/japplphysiol.01390.2003
Zambolin F, Giuriato G, Laginestra FG, Ottaviani MM, Favaretto T, Calabria E, Duro-Ocana P, Bagley L, Faisal A, Peçanha T, McPhee JS, Venturelli M (2022) Effects of nociceptive and mechanosensitive afferents sensitization on central and peripheral hemodynamics following exercise-induced muscle damage. J Appl Physiol 133(4):945–958. https://doi.org/10.1152/japplphysiol.00302.2022
Zambolin F, Peçanha T, Pinner S, Venturelli M, McPhee JS (2023) Effects of exercise induced muscle damage on cardiovascular responses to isometric muscle contractions and post-exercise circulatory occlusion. Eur J Appl Physiol. https://doi.org/10.1007/s00421-023-05255-8
Acknowledgements
The authors would like to thank Marshall Dearmon, Havens Lane Wise, Anabelle Vallecillo-Bustos, and Diavion Stanfield for their assistance with this study. The authors would also like to thank DeAnna Greer, Anne Speed, and Brandy Lowe for their administrative support. Lastly, the authors would like to thank all the participants who committed their time and effort to the completion of this study.
Funding
Funding was provided by Aubrey Keith and Ella Gin Lucas Endowment for Faculty Excellence and the University of Southern Mississippi.
Author information
Authors and Affiliations
Contributions
JS conceptualized the initial study idea and designed the study protocol. JS, TN, and RA collected, analyzed, and interpreted the raw data. JS prepared figures and drafted the manuscript, and all authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to report.
Additional information
Communicated by I. Mark Olfert.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stavres, J., Aultman, R.S. & Newsome, T.A. Exercise pressor responses are exaggerated relative to force production during, but not following, thirty-minutes of rhythmic handgrip exercise. Eur J Appl Physiol 124, 1547–1559 (2024). https://doi.org/10.1007/s00421-023-05390-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-023-05390-2