Abstract
Aim
Exercise training with blood flow restriction (BFR) increases muscle size and strength. However, there is limited investigation into the effects of BFR on cardiovascular health, particularly central hemodynamic load.
Purpose
To determine the effects of BFR exercise on central hemodynamic load (heart rate—HR, central pressures, arterial wave reflection, and aortic stiffness).
Methods
Fifteen males (age = 25 ± 2 years; BMI = 27 ± 2 kg/m2, handgrip max voluntary contraction-MVC = 50 ± 2 kg) underwent 5-min bouts (counter-balanced, 10 min rest between) of rhythmic unilateral handgrip (1 s squeeze, 2 s relax) performed with a moderate-load (60% MVC) with and without BFR (i.e., 71 ± 5% arterial inflow flow reduction, assessed via Doppler ultrasound), and also with a low-load (40% MVC) with BFR. Outcomes included HR, central mean arterial pressure (cMAP), arterial wave reflection (augmentation index, AIx; wave reflection magnitude, RM%), aortic arterial stiffness (pulse wave velocity, aPWV), and peripheral (vastus lateralis) microcirculatory response (tissue saturation index, TSI%).
Results
HR increased above baseline and time control for all handgrip bouts, but was similar between the moderate load with and without BFR conditions (moderate-load with BFR = + 9 ± 2; moderate-load without BFR = + 8 ± 2 bpm, p < 0.001). A similar finding was noted for central pressure (e.g., moderate load with BFR, cMAP = + 14 ± 1 mmHg, p < 0.001). No change occurred for RM% or AIx (p > 0.05) for any testing stage. TSI% increased during the moderate-load conditions (p = 0.01), and aPWV increased above baseline following moderate-load handgrip with BFR only (p = 0.012).
Conclusions
Combined with BFR, moderate load handgrip training with BFR does not significantly augment central hemodynamic load during handgrip exercise in young healthy men.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The traditional recommendation for increasing muscle size and strength is resistance training two or more times per week with a load ≥ 60% of maximum voluntary contraction (MVC) (ACSM's Guidelines for Exercise Testing and Prescription 2018). However, combining traditional exercise with blood flow restriction (BFR) appears to enhance musculoskeletal adaptations (Abe et al. 2006; Dankel et al. 2016). For instance, in healthy participants, adding BFR to handgrip training increased muscle size similarly to a load-equated non-restriction condition (Credeur et al. 2010; Hunt et al. 2012), which also appeared to amplify improvements in muscle strength (Credeur et al. 2010). Similarly, in a population of individuals with spinal cord injury, adding BFR to an electrical stimulation protocol augmented the increase in muscle size and strength of the muscles controlling the wrist, which also led to functional improvements (Gorgey et al. 2016). Thus, it seems that handgrip training combined with BFR provides a potential therapeutic modality to restore or increase muscle function associated with activities of daily living in a range of populations. However, there is limited investigation into the acute effects of BFR handgrip exercise on the cardiovascular system. If BFR handgrip exercise could acutely increase central hemodynamic load, then this may preclude its prescription in ‘at risk’ populations.
Recently, concerns were raised that argue BFR could increase the risk of an adverse cardiovascular event via augmentation of the exercise pressor reflex (Spranger et al. 2015; Sprick and Rickards 2017). The exercise pressor reflex is a mechanism by which the cardiovascular system responds to physical stress by increasing heart rate, blood pressure, and total peripheral resistance to match delivery demands of metabolically active skeletal muscle (Smith et al. 2006). Of importance, mechanical and metabolic stimuli elicit the pressor effect (Kaur et al. 2015); presumably, these stimuli are enhanced during BFR (Loenneke et al. 2010; Spranger et al. 2015; Sugaya et al. 2011). However, it is unclear whether an additive effect of metabolic accumulation and mechanical stimulation during exercise with BFR actually exaggerates the cardiovascular response.
The purpose of this study was to evaluate the central cardiovascular hemodynamic response to unilateral handgrip exercise with BFR. This was performed in a randomized within-subject study by comparing central cardiovascular hemodynamic (i.e., heart rate—HR, central pressures, arterial wave reflection, and arterial stiffness) responses to moderate-load training (60% MVC) with and without BFR, during a low-load condition (40% MVC) with BFR, and during a time control with BFR only (no exercise). Prior to assessing ‘at risk’ people, young-healthy men were studied to ascertain the ‘normal’ central cardiovascular health response to BFR handgrip training at both a low and moderate exercise intensity. We tested two hypotheses: (1) moderate-load (60% MVC) handgrip training with BFR would augment the central hemodynamic response to exercise compared to a load-equated non-BFR condition and (2) lower-load (40% MVC) BFR handgrip would induce a lessor central hemodynamic response (i.e., lower HR, central pressures, augmentation index, and aortic stiffness) in comparison to moderate-load BFR handgrip.
Methods
Participants
Fifteen healthy males (age = 25 ± 2 years; BMI = 27 ± 2 kg/m2) were recruited from the University of Southern Mississippi and surrounding area. Participants were recreationally active, i.e., performed resistance and or aerobic training, and free of any diagnosed cardiovascular, metabolic or neurological disease (assessed via detailed health history questionnaire), were non-medicated, and non-smokers. All participants provided written informed consent prior to data collection, and all experimental protocols and procedures were reviewed and approved by the University of Southern Mississippi Institutional Review Board (Protocol Approval # 16041401).
All participants were studied in a quiet, dimly lit, humidity (50%) and temperature (21–23 °C) controlled laboratory. Prior to arrival, participants were euhydrated and instructed to refrain from caffeine intake for 12 h, alcohol and strenuous physical activity for 24 h, and be at least 2 h fasted (low-fat, low-glycemic meal recommended). Following the consent and screening process, height and weight were obtained with standard measures, and participants were positioned semi-recumbent on an examination table and instrumented for experimental measurements.
Experimental protocol
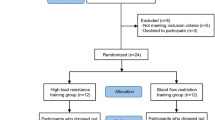
The experimental protocol was conducted in a single visit. After baseline assessments, participants underwent a time-control (BFR, no exercise), followed by three stages of exercise: (i) handgrip at 40% MVC with BFR; (ii) 60% MVC with BFR; and (iii) 60% MVC without BFR, in a randomized order (Fig. 1). During exercise, participants were instructed to squeeze the dynamometer at a constant cadence (20 contractions per minute; 1 s squeeze, 2 s relax, for 5 min) set by metronome. Visual acquisition was provided for the participant on a monitor (Powerlab, AD Instruments) to ensure that the target percentage was achieved. Measurements of radial artery blood flow were recorded from the right arm at minute two, with HR, central hemodynamics, and leg muscle oxygenation (i.e., marker of peripheral vasoconstriction) measured at minute three, and aortic arterial stiffness measured immediately following completion of each stage with the BFR cuff still inflated. Following exercise, the BFR cuff was deflated and participants were allowed 10 min of rest before commencing the next stage of testing.
Experimental protocol timeline. With the exception of baseline (BL) and time control (TC), the order of the remaining experimental testing stages were randomized. Pulse wave analysis (PWA) measurements were performed twice at BL and once at minute three of each 5-min testing stage. Radial artery blood flow (BF) measures were recorded for 1-min intervals starting at minute two of each stage, while leg microvascular responses were recorded via near-infrared spectroscopy (NIRS) at minute three, and aortic arterial stiffness (aPWV) measured immediately following the completion of each stage
Experimental measurements and procedures
Handgrip strength testing A handgrip dynamometer (Stoelting chart recorder) was placed in the participant’s right hand and supported with positioning pads. MVCs were determined prior to the experimental protocol by performing 5 maximal handgrip squeezes (3 s contraction, 30 s rest between trials), and the average of the greatest 3 was considered MVC 100% (50 ± 2 kg MVC on average).
Blood flow restriction procedure Following MVC testing, a cuff was positioned around the lower portion of the right upper-arm and inflated 80–100 mmHg (Hokanson® cuff size-10 cm via E20-Rapid Cuff Inflator) to reduce radial artery blood flow by 71 ± 5% on average (see Fig. 2 for example), validated by Doppler-ultrasound (Logiq P5; GE® Medical systems, Milwaukee, WI, USA). This reduction in blood flow corresponded to the typical reduction seen when applying 40–80% arterial occlusion pressure, which is the recommended range for BFR exercise (Dankel et al. 2016). Once identified, this pressure was used during the experimental protocol (see Fig. 2, protocol timeline).
Central cardiovascular hemodynamics and arterial stiffness Heart rate (HR) and heart rate variability (HRV) were monitored using surface electrocardiography (Powerlab Bioamp, AD-Instruments, Dunedin, Otago). Central pulse wave analysis was measured via the oscillometric method (SphygmoCor XCEL, AtCor Medical, Itasca, Illinois). The XCEL system performs a standard blood pressure measure, followed by determination of a brachial pressure waveform. Waveform decomposition is then performed using internalized software (details outlined in “Data analysis” below). Two pulse wave analyses were taken at baseline (values averaged), and one was taken during the other stages of testing. Aortic arterial stiffness was measured using the same XCEL device. To do this, carotid-femoral artery pulse transit time (Δt in sec) was determined via application tonometry performed on the left common carotid artery, coupled with the oscillometric method performed over the left upper thigh. Prior to this, distance measurements between the carotid pulse site and sternal notch (L1), and sternal notch to proximal edge of thigh cuff (L2) were obtained using a specialized calliper. Along with Δt, distance was applied to the following equation: aortic pulse wave velocity (aPWV in m/s) = Length (L2 – L1)/Δt. One aPWV measure was performed for each stage of testing.
Vastus lateralis muscle oxygenation The rationale for examining NIRS estimates of muscle oxygenation stems from evidence supporting that changes in tissue oxygenation assessed via NIRS can reliably determine sympathetically induced vasoconstriction, and have been previously validated in human and animal models (Fadel et al. 2004; Horiuchi et al. 2014). To do this, a continuous-wave, near-infrared spectroscopy (NIRS) device (PortaLite; Artinis Medical Systems BV, Elst, The Netherlands) emitted wavelengths (760 and 850 nm) to detect relative concentrations of oxygenated and deoxygenated hemoglobin and myoglobin, as well as total hemoglobin (Barstow 2019). The NIRS probe was secured about two-thirds from the top of the vastus lateralis over the muscle belly, as previously performed (Lucero et al. 2018). A custom-made cover was secured over the probe to shield ambient light.
Forearm blood flow and venous pooling Blood flow through the right radial artery was measured at rest and during exercise using a duplex-Doppler ultrasound system (Logiq P5; GE® Medical systems, Milwaukee, WI, USA) (Credeur et al. 2010, 2014). The artery was imaged along the forearm, ~ 5 cm distal to antecubital fossa using an 11-MHz linear array transducer. Blood velocity signals were obtained using the same probe in pulse wave mode (5-MHz) and insonation angle of 60°. The velocity cursor was maintained mid-vessel and a large sample volume was used to encompass the entire vessel lumen. To ensure consistency and stability in measurement, probe placement was marked on the skin, and the transducer was stabilized using a customized clamp. To provide a simple index of venous pooling, forearm circumference measures were obtained immediately following each stage using a measuring tape. Marks were placed over the largest part of the forearm to ensure consistency between measurements.
Data analysis
Central cardiovascular hemodynamics For pulse wave analysis, oscillometric pressure waveforms were analyzed through the SphygmoCor XCEL device. An aortic pressure waveform was generated by the device using a validated transfer function, from which the following central hemodynamic indices were derived: central systolic BP, central diastolic BP, pulse pressure (PP), augmentation pressure (AP), augmentation index (AIx%), and reflection magnitude (RM%). AP is the maximum systolic pressure, minus the pressure at the inflection point. This value, expressed as a percentage of total pulse pressure, is considered AIx%. The generalized aortic pressure waveform was also decomposed into its forward (Pf) and backward (Pb) wave components. The RM% is then calculated as Pb/Pf*100.
HR and HRV data were analysed using Powerlab and LabChart software (AD-Instruments, Colorado Spring, CO). For HRV, both time (standard deviation of normal R–R intervals—SDNN, and square root of mean squared differences of normal R–R intervals—RMSSD) and frequency domain indices (power spectral analysis to determine low frequency—LF, high frequency—HF and the LF/HF component ratio) were examined in accordance with guidelines (Camm et al. 1996) and provided an index of autonomic balance (i.e., sympathetic and vagal input to heart rate). Along with central systolic BP, the rate pressure product (RPP), an estimate of myocardial demand (Dursteine and Moore 2003), was also calculated: RPP (bpm*mmHg) = HR*central systolic BP.
Forearm blood flow Radial artery diameters and blood velocities were analyzed on the Doppler ultrasound (1-min recordings performed at the 2-min time point of each stage). Blood flow analysis occurred offline by one operator separates from the sonographer. Time-averaged mean velocity (Vmean) values were calculated using internal software (Logiq P5). Arterial diameter was measured at a perpendicular angle to the anterior and posterior walls of the vessel (example provided in Fig. 1). Using diameter and Vmean, radial artery blood flow was calculated as: blood flow (mL/min) = Vmean * π(diameter/2)2 × 60.
Vastus lateralis muscle oxygenation The tissue saturation index (TSI%) was determined using the spatially resolved spectroscopy approach (Lucero et al. 2018). Importantly, this approach can provide accurate absolute estimates of total hemoglobin (Thavasothy et al. 2002). TSI% was monitored continuously but averaged for 1-min recordings during the last minute of each bout. The NIRS signals were observed following completion of each testing stage to ensure basal levels were comparable to the original baseline level before commencing the next testing stage.
Statistical analysis
Statistical analyses were performed using SigmaPlot software (version 12.0) and SPSS (version 23). Data are presented as mean ± standard error, and statistical significance was set a priori at p < 0.05. For hypothesis 1, the impact of moderate load (i.e., 60% MVC) handgrip with and without BFR on dependent variables was evaluated using a two-way repeated measures ANOVA. For hypothesis 2, the impact of low (i.e., 40% MVC) and moderate load handgrip with BFR on dependent variables was determined using a one-way repeated measures ANOVA. All post hoc testing was performed using a Bonferroni test. To account for changes in MAP and HR on aPWV and AIx, respectively, covariate analyses were performed using a mixed linear model. The following parameters were selected; testing stage (i.e., Baseline and 60% HG) and condition (with or without BFR) were set as fixed factors, and subjects were randomized. Interactions between fixed factors (testing stage*condition) were examined first, and if significant, post hoc testing for repeated measures were performed.
Results
Central cardiovascular hemodynamics
Wave decomposition analysis was not performed on the first three participants due to a software update that was performed at the beginning of the study. All dependent central cardiovascular hemodynamic data are summarized in Table 1. There were no differences observed for any central hemodynamic parameter between the baseline and time control conditions (p > 0.05). Compared to time control, HR increased in an intensity dependent manner (Fig. 3), but was similar in magnitude for moderate-load handgrip with and without BFR (p < 0.001), but did not significantly differ during the low-load BFR condition (p > 0.05). A similar finding was noted for central systolic, diastolic, and cMAP (Fig. 4). All central pressures increased from baseline and time control during each handgrip bout (p < 0.001), a response that was comparable between the moderate-load handgrip conditions (p < 0.001). RPP also increased above baseline and time control during each handgrip bout, a response that was greater during the moderate-load stages (p < 0.001). Compared to time control, no significant differences were noted for the PP, AP, AIx, and RM% (p > 0.05). For aortic arterial stiffness, aPWV increased from baseline during moderate load handgrip with BFR only (p = 0.02) (Fig. 5).
Mean summary data for central blood pressure [systolic (cSBP), diastolic (cDBP), and mean arterial pressure (cMAP)] response to each testing stage. a Depicts the results from Hypothesis 1 testing with b showing results from Hypothesis 2 testing. *p < 0.05 vs. baseline (BL); #p < 0.05 vs. time control (TC); †p < 0.05 vs. 40% MVC with BFR
Two participants were considered outliers for HRV and were excluded from this analysis. For time domain analyses, SDNN decreased similarly from baseline during the moderate intensity handgrip bouts (p = 0.004). The RMSSD, decreased from baseline only during moderate intensity handgrip without BFR (p = 0.013). For frequency domain, LF component was lower than baseline only during the moderate load handgrip bouts (p = 0.018), whereas the HF tended to decrease only during moderate-load handgrip without BFR (p = 0.05). There was no difference in the LF/HF component ratio for any stage of testing (p > 0.05).
Forearm blood flow, circumference, and vastus lateralis tissue oxygenation
Two participants were excluded from the NIRS analysis due to technical issues (i.e., poor signal quality during testing stages). Compared to baseline, forearm BF decreased during time control (p < 0.001), but increased during the moderate load handgrip bouts (p < 0.001), a response that was greater for the non-BFR conditions (p < 0.001). Compared to baseline, forearm circumference increased during time control (p = 0.008) and each handgrip bout (p < 0.05), and response that was greatest during moderate load with BFR (p < 0.001). TSI% increased from rest only during the moderate-load handgrip bouts (p < 0.05).
Discussion
The primary purpose of this study was to determine the effects of BFR on the central cardiovascular hemodynamic response to unilateral handgrip exercise. Interestingly, moderate load handgrip exercise with BFR did not significantly augment central hemodynamic load over the load equated non-BFR conditions. Low-load handgrip with BFR produced the lowest pressor response overall. A non-BFR comparison for the low-load condition was not investigated but it could be assumed that there would no effect based on the results of the moderate-load conditions with and without BFR. Nevertheless, this remains an assumption. The underlying mechanisms mediating the pressor response to handgrip exercise with BFR are unclear and discussed below to provide insight but may likely be more cardiac driven as the TSI%, an index of sympathetically induced vasoconstriction, did not significantly decrease during any stage of testing.
Recently, concerns were raised regarding BFR training that argued this modality, while effective for enhancing muscle strength and size, could exaggerate the pressor response to exercise, thus making it potentially unsafe for certain patient groups (Spranger et al. 2015). Indeed, early work demonstrates that pressor responses are exaggerated when blood flow is restricted to exercising skeletal muscle (Alam and Smirk 1937). Furthermore, performing isometric handgrip with post-exercise ischemia—a standard approach for assessing the muscle metaboreflex—results in marked elevations in muscle sympathetic nerve activity, total peripheral resistance, and subsequently, arterial pressure (Kaur et al. 2015; Smith et al. 2006). It is important to emphasize, these assessments typically utilize isometric (static) exercise with complete arterial occlusion (i.e., 250 mmHg occlusion cuff pressures) during post-exercise ischemia (Kaur et al. 2015; Smith et al. 2006). Considering this, our study used rhythmic exercise and a lower cuff inflation pressure (i.e., 80–100 mmHg) to limit possible muscle metaboreflex engagement. This approach resulted in ~ 70% arterial inflow reduction, which is similar to the reduction observed within the recommended application range for BFR, i.e., 40–80% of arterial occlusion pressure (Mouser et al. 2017). Our data demonstrate an intensity-dependent increase in BP during unilateral handgrip exercise with BFR, albeit this response was comparable to the load equated non-BFR condition. These results are consistent with some other BFR reports utilizing a variety of other exercise modalities (Domingos and Polito 2018).
The underlying mechanisms mediating the pressor response to BFR exercise in the current study are unclear, but may likely be due to stimulation of the afferent limb of the exercise pressor reflex. A bevy of research supports that muscle afferents are sensitive to both mechanical (i.e., muscle distortion during contraction) and metabolic stimuli (i.e., lactate, H+ , adenosine, phosphate, etc.) (Smith et al. 2006, 2010). During exercise, muscle contractions and the resultant metabolite accumulation can stimulate mechanically and metabolically sensitive afferent fibers (i.e., groups III and IV), which in turn, facilitate efferent parasympathetic withdrawal and increased sympathetic nervous system outflow to the heart and peripheral vasculature, respectively (Smith et al. 2010). We postulate that moderate-load handgrip with BFR would result in greater venous pooling and accumulation of metabolites. Though, metabolite levels were not measured presently, we did examine limb circumference changes (a marker of venous pooling) and BFR conditions produced a greater forearm circumference following exercise. Though, we cannot definitively state whether the acute increase in forearm circumference during BFR exercise is related to venous pooling or overall tissue hypervolemia per se. Nevertheless, the changes seen in forearm circumference during BFR exercise did not correspond with a greater pressor response compared to the non-BFR condition.
To explore potential efferent limb contributors (e.g., cardiac vs. peripheral vascular) of the pressor response, we examined autonomic nervous system input to the heart (i.e., HRV), and indicators of peripheral vasoconstriction and vascular resistance, including TSI% changes via NIRS (Fadel et al. 2004; Horiuchi et al. 2014) and arterial wave reflection via RM% (Butlin et al. 2012; Qasem and Avolio 2008). For HRV, parasympathetic input to HR was estimated through the SDNN, RMSSD, and the HF component from power spectral analysis (Camm et al. 1996). Though debatable, the LF/HF component ratio reflects autonomic balance and provided a marker of sympathetic input to the heart (Camm et al. 1996). Considering this, our data demonstrated that overall autonomic balance (LF/HF) was not significantly impacted by handgrip exercise, with or without BFR; whereas, time domain indices, namely a decrease in SDNN, was suggestive of greater parasympathetic withdrawal during exercise, a response that was comparable between stages.
Microcirculatory responses (TSI%) revealed the moderate-load handgrip results in a significant increase in tissue oxygenation. Initially, we anticipated the opposite response as peripheral vascular resistance would presumably be greater during BFR exercise. The RM%, also did not significantly vary from baseline. Furthermore, the AP and resultant AIx did not significantly change for any level of testing. The AP is partly dependent on RM%, which may explain the lack of change in this measurement during handgrip exercise. While aPWV was elevated above baseline during the moderate-load BFR handgrip, this effect was not significantly different for the other exercise conditions. The underlying mechanism for this response is unclear, as sympathetically induced peripheral vasoconstriction (i.e., a decrease in TSI%) was not affected by moderate-load exercise. It is plausible that sympathetic nervous outflow during exercise is not entirely uniform and could be elevated in some vascular regions and not others. For instance, in animals, for a given perturbation (i.e., limb movement or electrical stimulation of presynaptic neurons) the magnitude of sympathetic outflow may vary between post-synaptic efferent pathways for heart, vertebral and renal nerves (Gebber et al. 2000; Morrison 2001a, b, c). We did not directly assess changes in muscle sympathetic nerve activity, so we cannot state whether sympathetic nerve activity increased during exercise with or without BFR. Nonetheless, the resultant increase in aPWV to moderate-load BFR handgrip was ~ 0.5 m/s, a value that is still well below the clinical threshold for chronic changes (i.e., 1 m/s)23. Collectively, our current data suggest that increases in central hemodynamic load during handgrip training with and without BFR are likely more cardiac driven (i.e., parasympathetic withdrawal), rather than altered by changes in peripheral vascular resistance.
Implications
Our study has important implications regarding the cardiovascular health response to BFR exercise training. The typical pressor response to exercise is characterized by an intensity-dependent increase in HR and arterial BP. In some populations, e.g., hypertension and type-II diabetes, this response could be exaggerated, in part, due to a heightened muscle metaboreflex (Delaney et al. 2010; Holwerda et al. 2016). Thus, professionals seeking to utilize modalities, like BFR, should consider this and pay careful attention to intensity of exercise and procedure to induce BFR. Our data provide support that BFR training, when performed in accordance with published recommendations [i.e., 40–80% arterial occlusion pressure] (Mouser et al. 2017), does not appear to augment the central hemodynamic response to unilateral handgrip over a traditional (non-BFR) moderate load training scheme. Nevertheless, it is important to note that the present findings are applicable only in healthy young men, and prior to implementation, future BFR-related research should confirm that these responses are consistent in other clinical populations.
Limitations
This study is not without limitations. Our protocol utilized unilateral upper-body exercise. Therefore, our results cannot be extrapolated to other bilateral and or lower-body exercise modalities. Our data do provide preliminary evidence to show that BFR applied to low- and moderate-load unilateral handgrip training does not elevate the pressor response over traditional exercise. Our primary comparison to evaluate pressor response to exercise during BFR was a the moderate load condition. A non-BFR comparison was not performed for the low-load intensity, thus, we cannot state if the pressor response would be greater for this condition. Future studies should consider investigating the clinical utility of this unilateral adaptation of BFR. Our study examined acute responses to BFR exercise and was not designed to determine the time course of change (i.e., serial measures post-exercise), or long-term impact of BFR exercise on cardiovascular health. Finally, our data were collected in healthy young men. The rationale for this was to control for the potential influence of sex hormones, and disease status on the cardiovascular response to BFR exercise. Future studies should confirm these results in women, as well as in older subjects, and in those of varying disease states.
Conclusion
In conclusion, these results indicate that moderate load, unilateral handgrip training with BFR does not augment the central pressor response to exercise. Furthermore, low-load BFR handgrip produced the most favorable pressor response. Future BFR research seeking to minimize central cardiovascular load during exercise should consider a low-intensity, unilateral adaptation of BFR during training sessions.
Abbreviations
- Aix:
-
Augmentation Index
- AP:
-
Augmentation pressure
- aPWV:
-
Aortic pulse wave velocity
- BFR:
-
Blood flow restriction exercise
- BP:
-
Blood pressure
- cMAP:
-
Central mean arterial pressure
- H+ :
-
Hydrogen ions
- HF:
-
High-frequency component
- HR:
-
Heart rate
- HRV:
-
Heart rate variability
- L1:
-
Distance between sternal notch and carotid pulse site
- L2:
-
Distance between sternal notch and proximal edge of thigh cuff
- LF:
-
Low-frequency component
- LF/HF:
-
Low-frequency-to-high-frequency component ratio
- MHz:
-
Mega-hertz
- MVC:
-
Maximal voluntary contraction
- NIRS:
-
Near-infrared spectroscopy
- Pb:
-
Backward pressure component
- Pf:
-
Forward pressure component
- PP:
-
Pulse pressure
- RM%:
-
Reflection magnitude
- RMSSD:
-
Root mean square of standard deviation of R–R intervals
- RPP:
-
Rate pressure product
- SDNN:
-
Standard deviation of R–R intervals
- TSI%:
-
Tissue Saturation Index
- V mean :
-
Mean blood velocity
References
Abe T, Kearns CF, Sato Y (2006) Muscle size and strength are increased following walk training with restricted venous blood flow from the leg muscle, Kaatsu-walk training. J Appl Physiol 100:1460–1466
Alam M, Smirk FH (1937) Observations in man upon a blood pressure raising reflex arising from the voluntary muscles. J Physiol 89:372–383
Barstow TJ (2019) Understanding near infrared spectroscopy (NIRS) and its application to skeletal muscle research. J Appl Physiol 126:1360–1376
Butlin M, Qasem A, Avolio AP (2012) Estimation of central aortic pressure waveform features derived from the brachial cuff volume displacement waveform. Conf Proc IEEE Eng Med Biol Soc 2012:2591–2594
Camm AJ et al (1996) Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation 93:1043–1065
Credeur DP, Hollis BC, Welsch MA (2010) Effects of handgrip training with venous restriction on brachial artery vasodilation. Med Sci Sports Exer 42:1296–1302
Credeur DP et al (2014) Characterizing rapid onset vasodilation to single muscle contractions in the human leg. J Appl Physiol 118:455–464
Dankel SJ, Jessee MB, Abe T, Loenneke JP (2016) The effects of blood flow restriction on upper-body musculature located distal and proximal to applied pressure. Sports Med 46:23–33
Delaney EP, Greaney JL, Edwards DG, Rose WC, Fadel PJ, Farquhar WB (2010) Exaggerated sympathetic and pressor responses to handgrip exercise in older hypertensive humans: role of the muscle metaboreflex. Am J Physiol Heart Circ Physiol 299:H1318–1327
Domingos E, Polito MD (2018) Blood pressure response between resistance exercise with and without blood flow restriction: A systematic review and meta-analysis. Life Sci 209:122–131
Dursteine JL, Moore GM (2003) ACSM's exercise management for persons with chronic diseases and disabilities, 2nd edn. Human kinetics
Fadel PJ, Keller DM, Watanabe H, Raven PB, Thomas GD (2004) Noninvasive assessment of sympathetic vasoconstriction in human and rodent skeletal muscle using near-infrared spectroscopy and Doppler ultrasound. J Appl Physiol 96:1323–1330
Gebber GL, Zhong S, Lewis C, Barman SM (2000) Defenselike patterns of spinal sympathetic outflow involving the 10-Hz and cardiac-related rhythms. Am J Physiol Regul Integr Comp Physiol 278:R1616–1626
Gorgey AS, Timmons MK, Dolbow DR, Bengel J, Fugate-Laus KC, Michener LA, Gater DR (2016) Electrical stimulation and blood flow restriction increase wrist extensor cross-sectional area and flow meditated dilatation following spinal cord injury. Eur J Appl Physiol 116:1231–1244
Holwerda SW, Restaino RM, Manrique C, Lastra G, Fisher JP, Fadel PJ (2016) Augmented pressor and sympathetic responses to skeletal muscle metaboreflex activation in type 2 diabetes patients. Am J Physiol Heart Circ Physiol 310:H300–309
Horiuchi M, Fadel PJ, Ogoh S (2014) Differential effect of sympathetic activation on tissue oxygenation in gastrocnemius and soleus muscles during exercise in humans. Exp Physiol 99:348–358
Hunt JE, Walton LA, Ferguson RA (2012) Brachial artery modifications to blood flow-restricted handgrip training and detraining. J Appl Physiol 112:956–961
Kaur J et al (2015) Muscle metaboreflex activation during dynamic exercise vasoconstricts ischemic active skeletal muscle. Am J Physiol Heart Circ Physiol 309:H2145–2151
American College of Sports Medicine (2018) ACSM's guidelines for exercise testing and prescription, 10th edn. Wolters Kluwer, Alphen aan den Rijn
Loenneke JP, Wilson GJ, Wilson JM (2010) A mechanistic approach to blood flow occlusion. Int J Sports Med 31:1–4
Lucero AA et al (2018) Reliability of muscle blood flow and oxygen consumption response from exercise using near-infrared spectroscopy. Exp Physiol 103:90–100
Morrison SF (2001) Differential control of sympathetic outflow. Am J Physiol Regul Integr Comp Physiol 281:R683–698
Morrison SF (2001) Differential regulation of brown adipose and splanchnic sympathetic outflows in rat: roles of raphe and rostral ventrolateral medulla neurons. Clin Exp Pharmacol Physiol 28:138–143
Morrison SF (2001) Differential regulation of sympathetic outflows to vasoconstrictor and thermoregulatory effectors. Ann N Y Acad Sci 940:286–298
Mouser JG, Dankel SJ, Jessee MB, Mattocks KT, Buckner SL, Counts BR, Loenneke JP (2017) A tale of three cuffs: the hemodynamics of blood flow restriction. Eur J Appl Physiol 117:1493–1499
Qasem A, Avolio A (2008) Determination of aortic pulse wave velocity from waveform decomposition of the central aortic pressure pulse. Hypertension 51:188–195
Smith SA, Mitchell JH, Garry MG (2006) The mammalian exercise pressor reflex in health and disease. Exp Physiol 91:89–102
Smith SA, Leal AK, Young CN, Fadel PJ (2010) Neural mechanisms of cardiovascular control during exercise in health and disease. Recent advances in cardiovascular research: from sleep to exercise. Transworld research network, pp 179–209. http://www.ressign.com/UserBookDetail.aspx?bkid=1029&catid=236#
Spranger MD, Krishnan AC, Levy PD, O'Leary DS, Smith SA (2015) Blood flow restriction training and the exercise pressor reflex: a call for concern. Am J Physiol Heart Circ Physiol 309:H1440–1452
Sprick JD, Rickards CA (2017) Combining remote ischemic preconditioning and aerobic exercise: a novel adaptation of blood flow restriction exercise. Am J Physiol Regul Integr Comp Physiol 313:R497–R506
Sugaya M, Yasuda T, Suga T, Okita K, Abe T (2011) Change in intramuscular inorganic phosphate during multiple sets of blood flow-restricted low-intensity exercise. Clin Physiol Funct Imaging 31:411–413
Thavasothy M, Broadhead M, Elwell C, Peters M, Smith M (2002) A comparison of cerebral oxygenation as measured by the NIRO 300 and the INVOS 5100 Near-Infrared Spectrophotometers. Anaesthesia 57:999–1006
Acknowledgements
The authors would like to thank the participants for their time and dedication towards the study. The authors would also like to thank the students (graduate and undergraduate) from the School of Kinesiology and Nutrition at the University of Southern Mississippi for their support and assistance throughout the various stages of this project.
Author information
Authors and Affiliations
Contributions
DC, LS, and SM conceived, and designed research; DC, RJ, and SM conducted experiments; DC, RJ, DS, LS, and MJ analyzed data; DC and RJ drafted the manuscript. All authors read, edited, and approved the final manuscript for submission.
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest to report for this study.
Additional information
Communicated by Philip D Chilibeck.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Credeur, D.P., Jones, R., Stanford, D. et al. Central cardiovascular hemodynamic response to unilateral handgrip exercise with blood flow restriction. Eur J Appl Physiol 119, 2255–2263 (2019). https://doi.org/10.1007/s00421-019-04209-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-019-04209-3