Abstract
Arm elevation induces diastolic retrograde flow in the brachial artery and an incremental rise in arterial compliance in healthy subjects with no modifications in vascular resistance. In contrast, changes in resistance have been observed after handgrip exercise. Our objective was to investigate if the resistance change induced by isometric handgrip exercise is able to reverse diastolic retrograde flow induced by arm elevation in a healthy population and to explore these adaptive changes in hypertensive subjects. Arterial flow velocity Doppler measurements were obtained including: (a) a baseline measurement, (b) measurement 30 s after arm elevation, (c) measurement during handgrip maneuver with the arm elevated, (d) measurement during handgrip release with the arm elevated. Our findings showed that diastolic retrograde flow is induced by arm elevation, partially increased by arm-up handgrip and completely reversed during arm-up handgrip release both in healthy and hypertensive subjects. As compared with normal subjects, deceleration time was longer in the hypertensive subjects during baseline but not during the arm-up stage, handgrip contraction and handgrip release stages. An important increase in deceleration time values from baseline to arm-up and handgrip contraction stages was observed in normal subjects but not in the hypertensive group. We believe that the highly significant difference in reactivity to postural changes observed in deceleration time values constitutes a promising hemodynamic index to investigate. Also, our observation of complete reversal of the retrograde flow during arm-up handgrip release provides a new approach to postural and exercise-induced vasomotor responses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since Celermajer et al. (1992) introduced flow-mediated dilation (FMD) assessment to determine arterial dilator capacity, this technique has become a well-established diagnostic method for predicting cardiovascular events in patients with cardiovascular disease (Thijssen et al. 2011). Moreover, over the past few years, there has been an increased interest in novel approaches to the brachial artery flow study, such as, retrograde flow and shear rate assessment (Thijssen et al. 2009; Padilla et al. 2010; Tinken et al. 2009). In this line of work, Thijssen and Green (Thijssen et al. 2009) demonstrated that retrograde flow can acutely impair endothelial function in humans. Furthermore, increased brachial and femoral retrograde flow was associated with aging (Credeur et al. 2009; Young et al. 2010) and a recent investigation demonstrated the influence of arterial stiffness on Doppler wave patterns in the femoral artery (Hashimoto and Ito 2010). Nevertheless, many aspects of retrograde flow and their relation with cardiovascular risk factors are still unknown. Brachial artery compliance is increased during arm elevation in healthy subjects with little or no modifications in vascular resistance. This response has been attributed to a reduced intravascular pressure that may trigger smooth vascular muscle relaxation (Bochmann et al. 2005) decreasing the vasomotor tone without modifying the vessel diameter (Zamir et al. 2007). Likewise, previous investigations reported increased diastolic retrograde flow components during arm elevation (Mc Loughlin et al. 2011) In contrast, handgrip exercise activates vasodilatory mechanisms (Clifford and Hellsten 2004) reducing arterial resistance and increasing brachial antegrade blood flow (Pyke et al. 2008; Wray et al. 2011; Humphreys and Lind 1963; Kirby et al. 2009). We hypothesized that diastolic retrograde flow could be reversed by changes in arterial resistance induced by isometric handgrip exercise. We further hypothesized that postural and exercise-induced adaptation might be impaired in hypertensive patients due to the reduction in arterial compliance (London et al. 1989) and endothelial dysfunction (Panza et al. 1990; Perticone et al. 2001; Plavnik et al. 2007). The purpose of this study was to investigate arm elevation and handgrip exercise influence on arterial flow velocities and retrograde flow in a healthy population and in hypertensive subjects.
Methods
Subjects
Eleven healthy volunteers (7 women) and seven hypertensive patients (3 women) matched by age and body mass index participated in the study (Table 1). Other than hypertension, no subjects reported having been diagnosed with cardiovascular risk factors, myocardial infarction or stroke. Measurements were carried out in a quiet laboratory at a temperature between 21 and 24°C. Caffeine and exercise were avoided for 24 h before testing (Urbina et al. 2009; Corretti et al. 2002). All patients in the hypertensive group were under drug treatment to normalize blood pressure and have been diagnosed with mild hypertension 5–10 years before participating in the study. The study procedures were approved by the ethics committee of the ININCA (UBA-CONICET) and adhered to the Declaration of Helsinki. All of the subjects gave previous written consent.
Experimental design
The entire hemodynamic study was performed in one session. Arterial blood pressure was measured in a supine position in the left arm before Doppler assessment. After blood pressure assessment, Doppler measurements were obtained in the right arm while the patients were lying supine and included (a) a baseline measurement, (b) measurement 30 s after arm elevation, (c) measurement during handgrip maneuver with the arm elevated, (d) measurement during handgrip release with the arm elevated. After obtaining the baseline measurement, the patient arm was passively elevated until a vertical position of 90° perpendicular to the stretcher. Once elevated, the arm was not descended at any moment during the rest of the hemodynamic study. The assessment in the arm-elevated handgrip position was performed during a 15-s constant muscle contraction. Fifty percent of the previously determined maximum voluntary contraction was used in all subjects and the last five Doppler waves before handgrip release were used for measurements. For the handgrip release state, measurements were made at the fifth Doppler wave after ending muscle contraction.
To facilitate the article comprehension, the arm-up handgrip contraction stage and the arm-up handgrip release stage will be mentioned only as handgrip contraction and handgrip release.
Doppler assessment
The brachial artery was imaged approximately 5 cm proximal to the antecubital fossa in a longitudinal plane using a commercially available ultrasound scanner with a 12-MHz transducer. Doppler velocity tracings were obtained with an insonation angle inferior to 60°. The wall filter was set at the lowest possible level (50 Hz). Sample volume was widely spaced to encompass the near and far walls of the artery, and simultaneous duplex B-mode -Doppler technique was used to certify venous signals were not included in the tracing.
Doppler measurements
Calculations were made with the ultrasound equipment built-in software and included peak systolic velocity (PSV), minimum diastolic velocity (MDV), pulsatility index (PI) and deceleration time (DT). Deceleration was calculated as peak systolic velocity−minimum diastolic velocity/deceleration time and deceleration time was assessed using the built-in software of the ultrasound equipment measuring the time from peak systolic velocity up to minimum diastolic velocity. (Hashimoto and Ito 2010) (Fig. 1, left). The ultrasound scanner built-in modified resistivity index (MRI = PSV−MDV/PSV) that considers minimum diastolic velocity instead of end diastolic velocity was used. Peak-to-peak difference (PSV−MDV) was calculated for all cases. Mean flow velocity was calculated as (PSV−MDV/PI). Retrograde flow time (ms) was measured and then divided by total cycle time to establish the retrograde time/total time ratio. DT% change was the percent of change during each stage of the study compared with baseline.
Left Peak systolic velocity (PSV) and deceleration time (DT). DT time was measured from peak systolic velocity up to minimum diastolic velocity. Middle Doppler wave patterns in a normal subject. (A) Baseline, (B) arm-up, (C) arm-up handgrip contraction and (D) arm-up handgrip release Right Doppler wave patterns in a hypertensive subject. (A) Baseline, (B) arm-up, (C) arm-up handgrip contraction and (D) arm-up handgrip release
Statistics
Statistical analysis was performed using SPSS for Windows (version 17.0) software. Continuous variables were expressed as mean ± one standard deviation. A one-way repeated measures ANOVA was used to evaluate the four hemodynamic stages. When a significant change was found, Bonferroni’s post hoc procedure was used for pairwise comparisons. Unpaired two-sample t test was used to compare normal subjects with the hypertensive population. A p < 0.05 was considered significant.
Results
Effects of arm elevation and handgrip maneuver in healthy patients
Peak systolic velocity was similar during the four stages (see Table 2). During the arm-up stage, minimum diastolic velocity was reduced as compared with baseline results (p = 0.023). On the contrary, modified resistivity index (p = 0.045), retrograde flow time (p = 0.003) and retrograde flow time/total time (p = 0.002) were increased. Deceleration time and pulsatility index were also increased, however, statistical significance was not reached (p = 0.06, p = 0.1). Deceleration and mean velocity presented a decline trend as compared with baseline, however, these reductions were not statistically significant.
During the handgrip contraction stage, an accentuation of the already observed arm-up changes was noticed. Minimum diastolic velocity was, again, reduced as compared with baseline results (p < 0.008). Deceleration time (p < 0.034), modified resistivity index (p = 0.003), retrograde flow time (p < 0.0001), retrograde time/total time (p < 0.0001) and pulsatility index were increased when compared to baseline (p < 0.002). Mean velocity was reduced during the handgrip contraction stage as compared with baseline (p < 0.001). Deceleration was also reduced when compared with baseline; however, statistical significance was not reached (p = 0.3).
Finally, during the handgrip release stage a partial reversion of the arm-up induced changes was observed. When the handgrip release stage was compared with the arm-up stage, a significant decrease in modified resistivity index (p = 0.001), retrograde flow time (p = 0.001) and retrograde time/total time (p = 0.002) was observed. Minimum diastolic velocity was increased from the arm-up stage to the handgrip release stage (p = 0.001). In conclusion, handgrip contraction increased the hemodynamic changes produced by arm elevation. On the other hand, handgrip release produced a reversion of the changes observed during the arm-up and the handgrip contraction stages. In fact, handgrip release results were similar to baseline results (See Table 2; Fig. 1, middle).
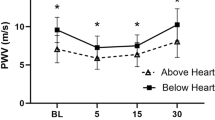
Normal versus hypertensive
Peak systolic velocity was higher in healthy subjects during all the stages with the arm elevated (p = 0.004; p = 0.005 and p = 0.008). However, statistical significance in the difference between groups was not reached during baseline (p = 0.06). Deceleration time was higher in the hypertensive subjects during baseline (p = 0.002) but not during the arm-up, handgrip contraction and handgrip release stages of the hemodynamic study (p = 0.97; p = 0.27 and p = 0.41). Interestingly, DT% change demonstrated an important increase in DT values from baseline to arm-up and handgrip contraction stages in normal subjects but not in the hypertensive group. Statistical significance of the different DT% change between healthy versus hypertensive subjective was p = 0.007 during arm-up and during handgrip contraction p = 0.001. During handgrip release, normal subjects presented a tendency for returning to DT baseline values resulting in a reduction of the described difference between the groups in the DT% change values (p = 0.32). Statistical data are presented in Table 2.
Discussion
Previous investigations have reported the presence of increased brachial retrograde flow in elderly patients with one or more cardiovascular risk factors (Credeur et al. 2009). A significant role of NO in the generation of arterial reflux (Padilla et al. 2011) was recently communicated. Moreover, an increase in blood flow after handgrip exercise (Pyke et al. 2008; Wray et al. 2011; Humphreys and Lind 1963) and the role of both NO and acetylcholine in the observed reactive hyperemia (Casey et al. 2010; Shoemaker et al. 1997) have been demonstrated. In the present paper, we introduce a novel method for assessing Doppler velocities and retrograde flow in the brachial artery. During the first stage of our study, we evaluated the hemodynamic impact of gravity (arm-up stage). We then added to gravity force an increase in forearm impedance produced by isometric handgrip contraction (arm-up handgrip contraction stage), and we investigated if post exercise vasodilation was able to reverse the previously observed changes induced by gravity and handgrip contraction (arm-up handgrip release stage).
Effects of arm elevation and handgrip maneuver in healthy patients
Peak systolic velocity was similar during the four stages of the experimental design. Our results, demonstrate that gravity and arm-up handgrip exercise induce changes in Doppler parameters only after the peak systolic velocity is reached. In contrast, after peak systolic velocity was reached we observed that retrograde flow was induced by arm elevation. Specifically, our findings showed that retrograde flow is induced by arm elevation, partially increased by arm-up handgrip and completely reversed during arm-up handgrip release. Moreover, our results suggest that the impedance augmentation caused by the restriction of the large vessels at the fascia level as they enter and leave the muscle (Gray et al. 1967) and/or by the local compression of intramuscular blood vessels during the muscle contraction (Barcroft and Dornhorst 1949; Sadamoto et al. 1983) causes an incremental rise in gravity-induced reflux (Green et al. 2005; Lutjemeier et al. 2005). This finding occurs despite the described systemic pressure increase observed during handgrip exercise (Eklund et al. 1974; Hunyor and Nyberg 1978) that might facilitate antegrade flow. Given that conduit artery blood flow profiles are markedly affected by downstream vascular resistance (Baccelli et al. 1985; Halliwill and Minson 2010), and the observed retrograde flow reversion during handgrip release suggests an adaptive response in the forearm microvasculature after exercise that results in a monophasic Doppler wave where no retrograde flow is observed. Diastolic retrograde flow reversion observed in the brachial artery after handgrip might be useful for studying microvasculature relaxation after isometric exercise.
Normal versus hypertensive subjects
A similar response in retrograde flow to postural changes and exercise in hypertensive subjects was observed (see Table 2). However, special considerations must be addressed concerning peak systolic velocity, deceleration time, deceleration and mean velocity. As previously reported (Safar et al. 1981), our results demonstrate that normal subjects present higher velocities and lower deceleration time than hypertensive subjects during baseline and these findings might reflect an increased arterial stiffness in the hypertensive group (Hashimoto and Ito 2010). Moreover, in normal subjects, deceleration time was increased during arm-up position and handgrip contraction resulting in a reduction in the deceleration slope from peak systolic velocity to minimum diastolic velocity. Although not significant, a tendency for returning to baseline values was observed in deceleration time and deceleration during handgrip release. Interestingly, the change in deceleration time observed in normal subjects between baseline and arm-up position was absent in hypertensive patients. Prolonged deceleration slopes are caused by the deprivation of pressure energy (Abela 2004). When post-stenotic arterial segments are studied using the Doppler technique, prolonged deceleration slopes are observed due to the deprivation of pressure energy caused by the upstream stenosis (Fronek et al. 1976). As mentioned, we observed a similar response when healthy subjects elevated the arm. These results suggest that healthy subjects compensate retrograde flow components induced by arm elevation by increasing the deceleration time enabling a prolonged antegrade flow. Likewise, it has been demonstrated that normal subjects increase the brachial arterial compliance during arm elevation (Zamir et al. 2007). Our observation of deceleration time increment in normal subjects might reflect the arterial compliance modification. The absence of prolongation of the deceleration slope in hypertensive subjects during arm elevation suggests an impaired response to postural changes that might represent an early marker of altered brachial hemodynamics. The understanding of this mechanism may be addressed in future investigations.
Study limitations
Some limitations of the present study need to be noted. Although the sample size was relatively modest, it is in keeping with physiological studies of this nature and the results were consistent between and within individuals. We believe that the highly significant difference observed between the four stages of the experimental design provides powerful evidence that our findings are robust. Moreover, all subjects in our cohort were white, so generalization to other ethnicities is not possible. Hypertensive subjects in our experiment were studied without suspending antihypertensive therapy. As in previous investigations evaluating hemodynamic modifications in the brachial artery in similar patients (Benjamin et al. 2004), we considered that since the study was performed with community-based volunteers, it would have been inappropriate to withhold antihypertensive medication. Previous communications demonstrated that the administration of vasoactive medications not containing nitrates does not significantly influence hemodynamic variables in the brachial artery such as FMD% (Gokce et al. 2002). Other studies have shown that chronic treatment with ACE inhibitors actually improves FMD (Anderson et al. 2000; Hornig et al. 2001). Nevertheless, it is important to mention that antihypertensive therapy may have influenced the differences observed between the studied groups.
Perspectives
Sustained retrograde flow can be induced by arm elevation in a population where normal triphasic flow is observed during baseline measurements. Our findings, encourage further studies of the impact of retrograde flow. Also, our observation of complete reversion of the retrograde flow during arm-up handgrip release is, to our knowledge, a previously unknown physiological phenomenon that provides a new approach to postural and exercise-induced vasomotor responses. Frequent associations of hypertensive disease, such as dysautonomia, might be the future targets for the study of retrograde flow reversion. Finally, we demonstrate that deceleration time is significantly lower in normal subjects as compared with hypertensive subjects during baseline and that hypertensive patients lack the adaptive deceleration time increase observed in normal subjects. The highly significant difference in reactivity to postural changes observed in deceleration time values constitutes a promising hemodynamic index to explore.
References
Abela GS (2004) Peripheral vascular disease: basic diagnostic and therapeutic approaches. Lippincott Publisher, Inc, New York
Anderson TJ, Elstein E, Haber H, Charbonneau F (2000) Comparative study of ACE-inhibition, angiotensin II antagonism, and calcium channel blockade on flow-mediated vasodilation in patients with coronary disease (BANFF study). J Am Coll Cardiol 35:60–66
Baccelli G, Pignoli P, Corbellini E, Pizzolati PL, Bassini M, Longo T, Zanchetti A (1985) Hemodynamic factors changing blood flow velocity waveform and profile in normal human brachial artery. Angiology 36:1–8
Barcroft H, Dornhorst AC (1949) The blood flow through the human calf during rhythmic exercise. J Physiol 109:402–411
Benjamin EJ, Larson MG, Keyes MJ, Mitchell GF, Vasan RS, Keaney JF Jr, Lehman BT, Fan S, Osypiuk E, Vita JA (2004) Clinical correlates and heritability of flow-mediated dilation in the community: the Framingham HEART Study. Circulation 109(5):613–9 (Erratum in: Circulation 2004 Jun 29; 109(25):3256)
Bochmann RP, Seibel W, Haase E, Hietschold V, Rödel H, Deussen A (2005) External compression increases forearm perfusion. J Appl Physiol 99(6):2337–2344 (Epub 2005 Aug 4)
Casey DP, Madery BD, Curry TB, Eisenach JH, Wilkins BW, Joyner MJ (2010) Nitric oxide contributes to the augmented vasodilatation during hypoxic exercise. J Physiol 588:373–385
Celermajer DS, Sorensen KE, Gooch VM, Spiegelhalter DJ, Miller OI, Sullivan ID, Lloyd JK, Deanfield JE (1992) Noninvasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet 340:1111–1115
Clifford PS, Hellsten Y (2004) Vasodilatory mechanisms in contracting skeletal muscle. J Appl Physiol 97:393–403
Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA et al (2002) International brachial artery reactivity task Force. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the international brachial artery reactivity task force. J Am Coll Cardiol 39(2):257–265
Credeur DP, Dobrosielski DA, Arce-Esquivel AA, Welsch MA (2009) Brachial artery retrograde flow increases with age: relationship to physical function. Eur J Appl Physiol 107(2):219–225 (Epub 2009 Jun 30)
Eklund B, Kaijser L, Knutsson E (1974) Blood flow in resting (contralateral) arm and leg during isometric contraction. J Physiol 240(1):111–124
Fronek A, Coel M, Berstein EF (1976) Quantitative ultrasonographic studies of lower extremity flow velocities in health and disease. Circulation 53(6):957–960
Gokce N, Holbrook M, Hunter LM, Palmisano J, Vigalok E, Keaney JF Jr, Vita JA (2002) Acute effects of vasoactive drug treatment on brachial artery reactivity. J Am Coll Cardiol 40(4):761–765
Gray SD, Carlsson E, Staub NC (1967) Site of increased vascular resistance during isometric muscle contraction. Am J Physiol 213:683–689
Green DJ, Bilsborough W, Naylor LH, Reed C, Wright J, O’Driscoll G, Walsh JH (2005) Comparison of forearm blood flow responses to incremental handgrip and cycle ergometer exercise. J Physiol 562:617–628
Halliwill JR, Minson CT (2010) Retrograde shear: backwards into the future? Am J Physiol Heart Circ Physiol 298:H1126–H1127
Hashimoto J, Ito S (2010) Pulse pressure amplification, arterial stiffness, and peripheral wave reflection determine pulsatile flow waveform of the femoral artery. Hypertension 56(5):926–933 (Epub 2010 Sep 27)
Hornig B, Landmesser U, Kohler C, Ahlersmann D, Spiekermann S, Christoph A, Tatge H, Drexler H (2001) Comparative effect of ACE inhibition and angiotensin II type 1 receptor antagonism on bioavailability of nitric oxide in patients with coronary artery disease: role of superoxide dismutase. Circulation 103:799–805
Humphreys PW, Lind AR (1963) The blood flow through active and inactive muscles of the forearm during sustained hand-grip contractions. J Physiol 166:120–135
Hunyor S, Nyberg G (1978) Comparison of intra-arterial and indirect blood pressures at rest and during isometric exercise in hypertensive patients before and after metoprolol. Br J Clin Pharmacol 6(2):109–114
Kirby BS, Voyles WF, Simpson CB, Carlson RE, Schrage WG, Dinenno FA (2009) Endothelium-dependent vasodilatation and exercise hyperaemia in ageing humans: impact of acute ascorbic acid administration. J Physiol 587(Pt 9):1989–2003 (Epub 2009 Mar 23)
London GM, Marchais SJ, Safar ME (1989) Arterial compliance in hypertension. J Hum Hypertens 3 Suppl 1:53–6 (Review)
Lutjemeier BJ, Miura A, Scheuermann BW, Koga S, Townsend DK, Barstow TJ (2005) Muscle contraction-blood flow interactions during upright knee extension exercise in humans. J Appl Physiol 98:1575–1583
Mc Loughlin MJ, Mc Loughlin S, Milei J (2011) Diastolic retrograde arterial flow: preliminary report. Radiologia English, Spanish (in press)
Padilla J, Young CN, Simmons GH, Deo SH, Newcomer SC, Sullivan JP, Laughlin MH, Fadel PJ (2010) Increased muscle sympathetic nerve activity acutely alters conduit artery shear rate patterns. Am J Physiol Heart Circ Physiol 298(4):H1128–H1135 (Epub 2010 Feb 12)
Padilla J, Simmons GH, Fadel PJ, Laughlin MH, Joyner MJ, Casey DP (2011) Impact of aging on conduit artery retrograde and oscillatory shear at rest and during exercise: role of nitric oxide. Hypertension 57(3):484–489 (Epub 2011 Jan 24)
Panza JA, Quyyumi AA, Brush JE et al (1990) Abnormal endothelium-dependent vascular relaxation in patients with essential hypertension. N Engl J Med 323:22–27
Perticone F, Ceravolo R, Pujia A, Ventura G, Iacopino S, Scozzafava A, Ferraro A, Chello M, Mastroroberto P, Verdecchia P, Schillaci G (2001) Prognostic significance of endothelial dysfunction in hypertensive patients. Circulation 104(2):191–196
Plavnik FL, Ajzen SA, Christofalo DM, Barbosa CS, Kohlmann O Jr (2007) Endothelial function in normotensive and high-normal hypertensive subjects. J Hum Hypertens 21(6):467–472 (Epub 2007 Feb 8)
Pyke KE, Poitras V, Tschakovsky ME (2008) Brachial artery flow-mediated dilation during handgrip exercise: evidence for endothelial transduction of the mean shear stimulus. Am J Physiol Heart Circ Physiol 294(6):H2669–H2679 (Epub 2008 Apr 11)
Sadamoto T, Bonde-Petersen F, Suzuki Y (1983) Skeletal muscle tension, flow, pressure, and EMG during sustained isometric contractions in humans. Eur J Appl Physiol 51:395–408
Safar ME, Peronneau PA, Levenson JA, Toto-Moukouo JA, Simon AC (1981) Pulsed Doppler: diameter, blood flow velocity and volumic flow of the brachial artery in sustained essential hypertension. Circulation 63(2):393–400
Shoemaker JK, Halliwill JR, Hughson RL, Joyner MJ (1997) Contributions of acetylcholine and nitric oxide to forearm blood flow at exercise onset and recovery. Am J Physiol 273(5 Pt 2):H2388–H2395
Thijssen DH, Dawson EA, Tinken TM, Cable NT, Green DJ (2009) Retrograde flow and shear rate acutely impair endothelial function in humans. Hypertension 53(6):986–992 (Epub 2009 Apr 20)
Thijssen DH, Black MA, Pyke KE, Padilla J, Atkinson G, Harris RA, Parker B, Widlansky ME, Tschakovsky ME, Green DJ (2011) Assessment of flow-mediated dilation in humans: a methodological and physiological guideline. Am J Physiol Heart Circ Physiol 300(1):H2–H12 (Epub 2010 Oct 15. Review)
Tinken TM, Thijssen DH, Hopkins N, Black MA, Dawson EA, Minson CT, Newcomer SC, Laughlin MH, Cable NT, Green DJ (2009) Impact of shear rate modulation on vascular function in humans. Hypertension 54(2):278–285 (Epub 2009 Jun 22)
Urbina EM, Williams RV, Alpert BS, Collins RT, Daniels SR, Hayman L et al (2009) Noninvasive assessment of subclinical atherosclerosis in children and adolescents. Recommendations for standard assessment for clinical research: a scientific statement from the American Heart Association. Hypertension 54(5):919–950 (Epub 2009 Sep 3)
Wray DW, Witman MA, Ives SJ, McDaniel J, Fjeldstad AS, Trinity JD, Conklin JD, Supiano MA, Richardson RS (2011) Progressive handgrip exercise: evidence of nitric oxide-dependent vasodilation and blood flow regulation in humans. Am J Physiol Heart Circ Physiol 300(3):H1101–H1107 (Epub 2011 Jan 7)
Young CN, Deo SH, Padilla J, Laughlin MH, Fadel PJ (2010) Pro-atherogenic shear rate patterns in the femoral artery of healthy older adults. Atherosclerosis 211:390–392
Zamir M, Goswami R, Salzer D, Shoemaker JK (2007) Role of vascular bed compliance in vasomotor control in human skeletal muscle. Exp Physiol 92(5):841–848 (Epub 2007 Jun 1)
Acknowledgments
We acknowledge Liliana Brocca for her help during the investigation.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Dag Linnarsson.
Rights and permissions
About this article
Cite this article
Mc Loughlin, S., Mc Loughlin, M.J., Azzato, F. et al. Retrograde flow components in the brachial artery. A new hemodynamic index. Eur J Appl Physiol 112, 3577–3583 (2012). https://doi.org/10.1007/s00421-012-2347-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-012-2347-3