Abstract
Interval training (IT) may induce physiological adaptations superior to those achieved with conventional moderate-intensity continuous training (MCT) in patients with coronary artery disease (CAD). Our objectives were (1) to systematically review studies which have prescribed IT in CAD, (2) to summarize the findings of this research including the safety and physiological benefits of IT, and (3) to identify areas for further investigation. A systematic review of the literature using computerized databases was performed. The search yielded two controlled trials and five randomized controlled trials (RCTs) enrolling 213 participants. IT prescribed in isolation or in combination with resistance training was shown to induce significant and clinically important physiological adaptations in cardiac patients. IT was also shown to improve cardiorespiratory fitness (e.g. VO2max, VO2AT), endothelial function, left ventricle morphology and function (e.g. ejection fraction) to a significantly greater extent when compared with conventional MCT. No adverse cardiac or other life-threatening events occurred secondary to exercise participation in these studies. However, these findings must be interpreted with caution, as methodological limitations were present in all trials reviewed. In conclusion, robustly designed RCTs with thorough and standardized reporting are required to determine the risk and benefits of IT in the broader cardiac patient population. Further research is required to determine optimal IT protocols for the use in cardiac rehabilitation programmes, potentially contributing to novel exercise prescription guidelines for this patient population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular diseases, such as coronary artery disease (CAD), account for over 17 million deaths worldwide each year, representing nearly one-third of the annual death toll (WHO 2008). It is well established that physical activity reduces the cardiovascular disease risk. Data collected over the past 40 years have shown that exercise training is safe, and can induce many health-related adaptations in individuals medically treated for cardiac disease (Jolliffe et al. 2001). The effectiveness of cardiac rehabilitation programs for the secondary prevention of CAD has also been well documented (Jolliffe et al. 2001). However, such rehabilitation programs remain drastically underutilized (Leon et al. 2005), and must continue to be improved to enhance patient uptake, optimize recovery, and more effectively reduce mortality risk profile.
The most recent position statement on exercise prescription for patients with CAD was published by the American College of Sports Medicine in the 2010 Guidelines for Exercise Testing and Prescription (ACSM 2010). The evidence-based recommendation for aerobic training within the guidelines specifies supervised, large-muscle group continuous exercise (e.g. walking, jogging, cycling, swimming, group aerobics and rowing) performed at an intensity of generally 40-85% of heart rate reserve. The guidelines also indicate that rating of perceived exertion (RPE) may be used to monitor exercise intensity, with the goal of keeping the intensity at a moderate level (ACSM, 2010).
The efficacy of moderate-intensity continuous training (MCT) for patients with CAD has been systematically reviewed by Jolliffe et al. (2000) in a meta-analysis involving 8,440 patients in 32 randomized controlled trials (RCTs). The authors concluded that MCT is safe and physiologically beneficial, and reduces all-cause mortality in cardiac patients by approximately 27%.
Interval training (IT), which involves alternating brief (2–5 min) higher intensity (≥75% VO2max/peak or RPE >15) and moderate-intensity workloads throughout an exercise session, has traditionally been used to train athletes requiring high levels of both aerobic and anaerobic fitness (e.g. track and team sport athletes). Recently, several RCTs have demonstrated the safety and effectiveness of IT in cardiac patients (Nilsson et al. 2008; Rognmo et al. 2004; Warburton et al. 2005; Wisløff et al. 2007). Interestingly, some of the data suggest that IT can induce significantly greater improvements in VO2max, and other physiological parameters, versus MCT (Rognmo et al. 2004; Warburton et al. 2005; Wisløff et al. 2007). Such findings are important for many reasons. For example, VO2max has recently been noted as the single best predictor of death among cardiac patients (Kavanagh et al. 2002), and the enhancement of this outcome measure may therefore be associated with risk reduction.
There is currently a need to more thoroughly investigate and elucidate the modalities and dosages of exercise that can be prescribed to elicit safe, expeditious and peak recovery in patients with CAD (Fletcher et al. 2001; Guiraud et al. 2009). To our knowledge, the evidence-base for IT in cardiac patients has not been systematically reviewed to date. A greater understanding of these data, as well as the caveats of this research, is required to formulate novel research questions and advance exercise prescription guidelines in this patient population, which may contribute to enhanced evidence-based practice involving the prescription of IT.
Therefore, our objectives are threefold:
-
1.
To systematically review studies which have prescribed IT in patients with CAD,
-
2.
To summarize the findings of this research including the safety and physiological benefits of IT, and
-
3.
To identify areas for further investigation.
Methods
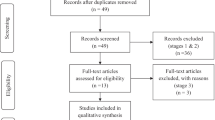
A systematic review of all published literature, regardless of study design was conducted. Given the paucity of RCTs, and the heterogeneity of interventions and outcome measures across investigations, the pooling of effect sizes across studies in a meta-analysis was not considered appropriate at this stage.
Criteria for considering studies
Study designs
RCTs, non-RCTs and uncontrolled trials published in peer-reviewed journals were included. Abstracts, case reports and unpublished trials were excluded.
Participants
Trials involving adults (>18 years) diagnosed with and/or surgically treated for CAD were included.
Interventions
Trials prescribing IT in isolation, or in combination with other exercise modalities (e.g. resistance training), were included. Studies investigating the effect of single bouts of IT or interventions that were <8 weeks in duration were not included. IT was defined as an exercise program alternating higher intensity (≥75% VO2max/peak or RPE of >15) (Borg 1998) and lower intensity workloads.
Outcome measures
Trials evaluating physiological outcome measures potentially responsive to chronic exercise exposure, based on the empirical evidence of exercise in CAD and other clinical and healthy cohorts, were included.
Search method
We conducted a literature review in January 2010, from the earliest date available to December 31, 2009, limited to the English language, using computerized databases including PubMed, Medline, CINAHL, Google Scholar, SportDiscus, Embase, and Web of Science. The search combined key words related to CAD (i.e. heart disease, cardiac disease, myocardial infarction), cardiac rehabilitation (i.e. exercise rehabilitation, training, sports, physical activity) and IT (i.e. interval training, aerobic interval training, anaerobic interval training, high-intensity interval training). Articles retrieved were examined for further relevant references.
Data extraction and analyses
Outcome measures significantly adapted by the intervention were extracted for the assessment of study and intervention quality. Relative ES (mean changeTreatment − mean changeControl) ÷ SDPooled baseline and 95% confidence intervals (SDPooled baseline × bias correction factor (Hedges) ± z value × standard error of ES estimate) were calculated for controlled trials and RCTs (Becker 2000).
Results
Studies retrieved and quality assessment
The search resulted in seven peer-reviewed articles, including two non-RCTs (Ehsani et al. 1981, 1982) and five RCTs (Munk et al. 2009; Nilsson et al. 2008; Rognmo et al. 2004; Warburton et al. 2005; Wisløff et al. 2007). All non-RCTs involved an IT group and a non-exercising control group, both consisting of CAD patients but without randomization of participants to these two groups (Ehsani et al. 1981, 1982). The control group in these trials consisted of participants who could not make the time commitment to the IT group or lived too far away from the exercise venue (Ehsani et al. 1981, 1982). Statistical analyses performed in the controlled trials involved repeated measures comparisons within groups over time only, and did not involve statistical comparisons between groups over time (i.e. group × time effect).
Four of the five RCTs involved randomization of subjects to an IT group and a MCT group (Nilsson et al. 2008; Rognmo et al. 2004; Warburton et al. 2005; Wisløff et al. 2007). Two RCTs included a non-exercising control group (Munk et al. 2009; Nilsson et al. 2008). All RCTs performed statistical comparisons between groups. Only one RCT specifically stated when the randomization of participants occurred (i.e. after baseline testing) (Nilsson et al. 2008). No RCT reported that collection of outcome measures were performed by blinded assessors, nor did any RCT involve an intention-to-treat strategy of analysis.
Overview of the participants
Sample size, gender and age
Two hundred and thirteen (n = 213) participants were enrolled in the seven trials reviewed (Table 1). Four trials enrolled fewer than 21 participants (Ehsani et al. 1981, 1982; Rognmo et al. 2004; Warburton et al. 2005), while the other trials enrolled 27 (Wisløff et al. 2007), 40 (Munk et al. 2009) and 80 participants (Nilsson et al. 2008).
All trials provided a gender breakdown. A total of 33 women and 180 men were enrolled. Three trials limited enrolment to men only (Ehsani et al. 1981, 1982; Warburton et al. 2005) with no explanations as to why women were excluded.
Mean age according to group assignment is presented in Table 1. In the two trials that provided an age range the youngest and eldest patient enrolled were 31 and 69 years (Ehsani et al. 1981, 1982).
Diagnosis of CAD, cardiac surgery, and comorbidities
Diagnosis of CAD was described in all trials but only three trials described the number of diseased vessels (Munk et al. 2009; Rognmo et al. 2004; Warburton et al. 2005). The percentage of participants who experienced a myocardial infarction was provided in five trials: 100% (Wisløff et al. 2007), 90% (Ehsani et al. 1981), 75% (Ehsani et al. 1982), 38% (Rognmo et al. 2004), and 35% (Warburton et al. 2005) while the participants in the RCT by Nilsson et al. (2008) had angiographically confirmed CAD or chronic heart failure (CHF).
Three trials described the surgical procedure received by participants prior to enrolment (Munk et al. 2009; Rognmo et al. 2004; Warburton et al. 2005; Wisløff et al. 2007), with 16 coronary artery bypass surgeries and 50 percutaneous coronary interventions reported. The remaining participants received medications as their medical intervention. The remaining trials did not provide data on surgery received prior to enrolment.
Medication
All trials provided a description of the medications received by the participants. The most common medications were beta-blockers (55%), statins (45%), anticoagulant and antiplatelet agents (35%), ACE inhibitors (38%), and nitrates (28%). In two of the trials, the use of propranolol in four exercising participants was reduced or ceased during the intervention period (Ehsani et al. 1981, 1982).
Comorbidities of the enrolled participants were not presented in six of the trials, while Munk et al. (2009) presented the prevalence of diabetes (23%), hypertension (53%) and hyperlipidemia (73%) in their cohort.
Overview of the exercise interventions
Details of the exercise interventions prescribed have been provided in Table 1. Overall, the interventions were heterogeneous with respect to duration of intervention, session duration, specific training modalities, and intensity ranges.
Length of exercise intervention
Four trials (Nilsson et al. 2008; Rognmo et al. 2004; Warburton et al. 2005; Wisløff et al. 2007) prescribed 10–16 weeks of training. Munk et al. (2009) prescribed 26 weeks of training and Ehsani et al. (1981, 1982) prescribed 52 weeks. Follow-up assessments beyond the completion of the prescribed exercise training were completed in two trials (Nilsson et al. 2008; Munk et al. 2009). IT was prescribed throughout the intervention period in five trials (Munk et al. 2009; Nilsson et al. 2008; Rognmo et al. 2004; Warburton et al. 2005; Wisløff et al. 2007), whereas Ehsani et al. (1981, 1982) prescribed continuous training for the initial 12 weeks, and IT for the remaining 40 weeks, of their 52-week intervention.
Phase of rehabilitation/exercise history
None of the seven trials outlined the phase of the cardiac rehabilitation or detailed the exercise training history of the participants (i.e. completed phases of cardiac rehabilitation). Only one trial detailed the exercise training history of the participants (Ehsani et al. 1982).
Timing of intervention
Time of enrolment relative to myocardial infarction and/or cardiac intervention was reported as an entry criterion in all trials (Table 1).
Modalities
All trials prescribed aerobic and anaerobic exercise training modalities and one trial also included resistance training (Rognmo et al. 2004). Of the five RCTs, three compared IT to MCT (Rognmo et al. 2004; Warburton et al. 2005; Wisløff et al. 2007) and one of these studies also included a non-exercising control group (Wisløff et al. 2007). Both Nilsson et al. (2008) and Munk et al. (2009) compared IT to a non-exercise control group, and did not involve a MCT group. The trials by Ehsani et al. (1981, 1982) included an exercise group (prescribed a combination of MCT and IT) and a non-exercising control group.
All trials reviewed described the exercise training equipment used. Six trials involved the use of treadmills and/or bicycle ergometers (Ehsani et al. 1981, 1982; Munk et al. 2009; Rognmo et al. 2004; Warburton et al. 2005; Wisløff et al. 2007), while one study also utilized arm ergometers and stair climbers (Warburton et al. 2005). Further, Ehsani et al. (1982) also provided patients with the option of exercising without equipment, by walking or jogging on an indoor track. Nilsson et al. (2008) prescribed aerobic dance exercise and movements but no exercise equipment.
Training intensity
All trials provided details regarding training intensity (Table 1).
IT
Low intensity intervals were prescribed at 40% of reserve oxygen consumption (VO2reserve) (Warburton et al. 2005), 50–60% of peak oxygen consumption (VO2peak) (Rognmo et al. 2004), 50–60% of peak heart rate (Wisløff et al. 2007), 60–70% of peak heart rate (Munk et al. 2009), and 70–80% of VO2max (Ehsani et al. 1981, 1982). High intensity intervals were prescribed at 90% of VO2reserve (Warburton et al. 2005), 80–90% of peak heart rate (Munk et al. 2009), 80–95% of VO2max/peak (Ehsani et al. 1981, 1982; Rognmo et al. 2004) and 90–95% of peak heart rate (Wisløff et al. 2007). The RCT by Nilsson et al. (2008) prescribed high intensity intervals at RPE = 15–18 but did not describe the intensity of the lower intensity intervals.
MCT
In three trials that included MCT, the prescribed intensities were 50–60% of VO2peak (Rognmo et al. 2004), 65% of VO2reserve (Warburton et al. 2005), and 70% of peak heart rate (Wisløff et al. 2007).
Session duration
All trials outlined the length of each session (Table 1). Two trials matched the total work performed by the IT and MCT groups by adjusting session length to equal the same training load (Rognmo et al. 2004; Wisløff et al. 2007). Aerobic training was prescribed two to five times per week in all trials (Table 1).
Compliance, attrition and adverse events
Attendance to exercise sessions was reported to be >90% by Munk et al. (2009), and 92% (IT group) and 95% (MCT group) by Wisløff et al. (2007). In trials by Ehsani et al. (1981, 1982) compliance was reported to range from 4.2 to 4.7 sessions per week. Three trials did not provide any information about compliance (Nilsson et al. 2008; Rognmo et al. 2004; Warburton et al. 2005). None of the reviewed trials presented a priori definition of “compliance” within their methodology.
Participant attrition of approximately 4% occurred in three trials (Rognmo et al. 2004; Warburton et al. 2005; Nilsson et al. 2008). Reasons for attrition included: discontinuing training because of knee/ankle injuries; stroke; poor motivation; unwillingness to attend follow-up testing; orthostatic intolerance; one death due to cardiovascular disease. These participants were removed from the statistical analysis. None of the adverse events contributing to participant attrition were attributed to the exercise training. Only one trial reported an adverse event during training (orthostatic collapse), which was not considered serious and did not require hospitalization (Munk et al. 2009). No trial reported adverse cardiac symptoms (angina, syncope, fibrillation) or complications due to exercise training. Notably, none of the reviewed trials presented an a priori definition of adverse event within their methodology.
Physiological adaptations to IT
Significant physiological adaptations to exercise training are presented in Table 2 for non-randomized trials and Table 3 for RCTs. Non-randomized trials by Ehsani et al. (1981, 1982) have shown that participants who engaged in 12 weeks of MCT followed by 40 weeks of IT significantly improved health-related outcome measures including VO2peak, exercise capacity, hemodynamic measures during maximal exercise, left ventricular (LV) morphology and function, body mass, and high-density lipoprotein cholesterol (Table 2). No improvements were noted in the control groups (Ehsani et al. 1981, 1982).
The RCTs showed that IT induced significantly greater increases in VO2max/peak (Munk et al. 2009; Nilsson et al. 2008; Rognmo et al. 2004; Warburton et al. 2005; Wisløff et al. 2007), VO2 at ventilatory threshold (Munk et al. 2009), time to fatigue (Nilsson et al. 2008; Wisløff et al. 2007), anaerobic threshold (Munk et al. 2009; Warburton et al. 2005; Wisløff et al. 2007), exercise/work economy (Wisløff et al. 2007), workload (Munk et al. 2009), improved 6-min walk distance (Nilsson et al. 2008), and improved LV size and function (Wisløff et al. 2007) as compared to the MCT group and the control groups (Table 3). Nilsson et al. (2008) showed that IT significantly improved 6-min walk test distance compared to the control group only.
LV function and hemodynamics were improved in three controlled trials (Ehsani et al. 1981, 1982; Wisløff et al. 2007), with significant increases during exercise in LV diastolic diameter diastolic volume, posterior wall thickness, surface area, fractional shortening, ejection fraction and rate pressure product (RPP). Ehsani et al. (1981, 1982) and Wisløff et al. (2007) conducted resting echocardiograms to assess LV function, but not exercise echocardiograms. Wisløff et al. (2007) reported that resting LV diastolic diameter and volume, both indicators of a reversal in post-infarct remodeling, significantly decreased in both the MCT and IT groups, while resting stroke volume, cardiac output and ejection fraction, indicators of improved myocardial contractile function, increased in the IT group only.
There were some differences in reported LV remodeling between authors. Ehsani et al. (1981, 1982) ascribed increased LV wall thickness to exercise-induced cardiac hypertrophy, whereas Wisløff et al. (2007) suggested that decreased LV wall thickness and end-diastolic/end-systolic volumes were due to an exercise-induced halt in post-myocardial infarction cardiac remodeling. Wisløff et al. (2007) also suggested that IT plus medications improved ejection fraction and myocardial contractile function.
Discussion
To our knowledge, this is the first systematic review of IT for CAD patients. Overall, this review suggests that IT prescribed in isolation or in combination with resistance training can induce significant and clinically important physiological adaptations in cardiac patients (Table 3). Further, IT has been noted to improve cardiorespiratory fitness (e.g. VO2max, VO2AT), endothelial function, left ventricle morphology and function (e.g. ejection fraction) to a significantly greater extent than conventional MCT (Rognmo et al. 2004; Warburton et al. 2005; Wisløff et al. 2007; Table 3). Notably, these physiological adaptations were achieved without significant cardiovascular or other life-threatening events. Training compliance was high according to four trials presenting these data (Ehsani et al. 1981, 1982; Munk et al. 2009; Wisløff et al. 2007).
Although this review provides support for the prescription of IT in cardiac patients, the findings must be interpreted with caution. All trials reviewed suffered from methodological limitations according to the current standards of reporting (Moher et al. 2001). These limitations were evident with respect to: statistical analyses where no studies to date have mentioned the use of intention-to-treat strategy; lack of involvement of blinded outcomes assessors; inadequate reporting of pertinent participant characteristics such as comorbidities and previous participation in cardiac rehabilitation; considerable variation in the intensities of exercise intervals used, and in the duration of study lengths; and insufficient reporting about safety and compliance including a priori definitions of terms and statistical comparison of adverse events between groups.
Moreover, exercise intervention studies conducted in chronically diseases cohorts commonly involve a self-selected (relatively fit and motivated) sample of participants, and none of the trials reviewed has described a standardized recruitment and screening process to enrol a more heterogeneous, representative sample of CAD patients according to current guidelines (Moher et al. 2001). Thus, the combined sample size of our review (n = 213) may be a limitation as it reflects only a minority of patients referred for cardiac rehabilitation who are motivated to exercise, perhaps indicating limited generalizability of these data to the larger cardiac patient population. Future RCTs must address these limitations.
The phases of rehabilitation and details regarding exercise history were also not adequately presented in the trials to date. These data may be important for establishing the timeline to initiate IT, which may contribute to more systematic and effective rehabilitation. For example, IT may be particularly beneficial for CAD patients who have completed 12 weeks of MCT during phase II cardiac rehabilitation and have reached a physiological plateau (Ehsani et al. 1982). Furthermore, the optimal duration of IT programmes for CAD patients has yet to be defined, as short-term (<8 weeks) IT exercise regimes in healthy individuals have produced significant physiological improvements (e.g. peripheral and skeletal muscle adaptations) which may be applicable for older CAD patients (Gibala et al. 2006; McKay et al. 2009). At present, however, more research is required to determine the optimal modalities and doses of exercise and timecourse to adaptations to provide the greatest health benefits in patients with CAD (Fletcher et al. 2001; Guiraud et al. 2009).
The reviewed trials also did not detail if participants were receiving additional components of cardiac rehabilitation, such as dietary modification, smoking cessation, or physical activity recommendations beyond the structured exercise program, and compliance to medications were not specifically detailed. These are clearly confounding variables, and, accordingly, must be reported in future investigations.
Only three RCTs performed randomization of participants to IT and MCT groups (Rognmo et al. 2004; Warburton et al. 2005; Wisløff et al. 2007), and these trials each enrolled fewer than 30 participants. Accordingly, it may be premature to draw conclusions regarding the effectiveness of IT as compared to MCT. It is likely that both modalities of exercise can be implemented as important components of cardiac rehabilitation, and more robust RCTs involving standardized exercise interventions are required to elucidate the relative importance and contribution of each across a number of physiologically important variables, medication usage, and long-term morbidity and mortality (Haskell 1994; Hedback and Perk 1990; Kavanagh et al. 2002).
There is a need to more adequately determine the risks and benefits of IT in this cohort, the outcomes of which can potentially lead to the development of appropriate exercise prescription guidelines (Fletcher et al. 2001; Giannuzzi et al. 2003; Guiraud et al. 2009; Leon et al. 2005). The safety and efficacy of supervised (in-center) as well as unsupervised (home-based) training are important to investigate. Home-based MCT, for example, has been found to be safe (Ades et al. 2000), but the risks of home-based IT have yet to be determined. Home-based exercise programs have important cost and feasibility implications for enhancing long-term compliance and behavior change. Future investigations should also define and describe target subpopulations of cardiac patients, including women and ethnic minorities who are perhaps less likely to access or enrol in an in-center rehabilitation program.
In summary, the effectiveness of cardiac rehabilitation for patients with CAD has been well established but the optimal intensity and type of exercise protocol to yield the greatest health benefits has yet to be defined (Kavanagh et al. 2002). This review highlights significant physiological improvements from IT compared to conventional MCT or usual care control, but we also highlight variations in, and limitations of, the IT studies conducted to date. Further investigation through larger, more robust studies is required to develop effective training prescription guidelines for cardiac rehabilitation programmes.
References
Ades PA, Pashkow FJ, Fletcher G, Pina IL, Zohman LR, Nestor JR (2000) A controlled trial of cardiac rehabilitation in the home setting using electrocardiographic and voice transtelephonic monitoring. Am Heart J 139(3):543–548
American College of Sports Medicine (2010) Resource manual for guidelines for exercise testing and prescription. Wolters Kluwer: Lippincott Williams and Wilkins, Baltimore MD:559–571
Becker L (2000) Effect size calculators. http://webuccsedu/lbecker/Psy590escalec3htm. Accessed 21 Jan 2010
Borg G (1998) Borg’s perceived exertion and pain scales. Human Kinetics, Champagne, pp 13–16
Ehsani AA, Heath GW, Hagberg JM, Sobel BE, Holloszy JO (1981) Effects of 12 months of intense exercise training on ischemic ST-segment depression in patients with coronary artery disease. Circulation 64(6):1116–1124
Ehsani AA, Martin WH, Heath GW, Coyle EF (1982) Cardiac effects of prolonged and intense exercise training in patients with coronary artery disease. Am J Cardiol 50(2):246–254
Fletcher GF, Balady GJ, Amsterdam EA, Chaitman B, Eckel R (2001) Exercise standards for testing and training: a statement for healthcare professionals from the American Heart Association. Circulation 104:1694–1740
Giannuzzi P, Saner H, Bjornstad H et al (2003) Secondary prevention through cardiac rehabilitation: position paper of the working group on cardiac rehabilitation and exercise physiology of the European Society of Cardiology. Eur Heart J 24(13):1273–1278
Gibala M, Little J, van Essen M, Wilkin G, Burgomaster K, Safdar A, Raha S, Tarnopolsky M (2006) Short-term sprint interval versus traditional endurance training: similar initial adaptations in human skeletal muscle and exercise performance. J Physiol 575:901–911
Guiraud T, Juneau M, Nigram A, Gayda M, Meyer P, Mekary S, Paillard F, Bosquet L (2009) Optimization of high intensity interval exercise in coronary heart disease. Eur J Appl Physiol 108:733–740
Haskell WL (1994) The efficacy and safety of exercise programs in cardiac rehabilitation. Med Sci Sports Exerc 26(7):815–823
Hedback B, Perk J (1990) Can high-risk patients after myocardial infarction participate in comprehensive cardiac rehabilitation? Scand J Rehabil Med 22(1):15–20
Jolliffe JA, Rees K, Taylor RS, Thompson D, Oldridge N, Ebrahim S (2001) Exercise-based rehabilitation for coronary heart disease. Cochrane Database Syst Rev 1:CD001800
Kavanagh T, Mertens DJ, Hamm LF, Beyene J, Kennedy J (2002) Prediction of long-term prognosis in 12169 men referred for cardiac rehabilitation. Circulation 106:666–671
Leon AS, Franklin BA, Costa F et al (2005) Cardiac rehabilitation and secondary prevention of coronary heart disease: an American Heart Association scientific statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity), in collaboration with the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation 111(3):369–376
McKay B, Paterson D, Kowalchuk J (2009) Effect of short-term high-intensity interval training vs. continuous training on O2 uptake kinetics, muscle deoxygenation, and exercise performance. J Appl Physiol 107(1):128–138
Moher D, Schulz K, Altman D (2001) The CONSORT statement: revised recommendations for improving the quality of reports of parallel group randomised trials. Lancet 357:1191–1194
Munk P, Staal E, Butt N, Isaksen K, Larsen A (2009) High-intensity interval training may reduce in-stent restenosis following percutaneous coronary intervention with stent implantation: a randomized controlled trial evaluating the relationship to endothelial function and inflammation. Am Heart J 158:734–741
Nilsson B, Westheim A, Risberg M (2008) Effects of group-based high-intensity aerobic interval training in patients with chronic heart failure. Am J Cardiol 102(10):1361–1365
Rognmo Ø, Hetland E, Helgerud J, Hoff J, Slørdahl SA (2004) High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. Eur J Cardiovasc Prev Rehabil 11:216–222
Warburton D, Mckenzie DC, Haykowsky MJ, Taylor A, Shoemaker P, Ignaszewski A, Chan S (2005) Effectiveness of high-intensity interval training for the rehabilitation of patients with coronary artery disease. Am J Cardiol 95:1080–1084
Wisløff U, Støylen A, Loennechen JP, Bruvold M, Rognmo Ø, Haram P, Tjǿnna A, Helgerud J, Slǿrdahl S, Lee S, Videm V, Bye A, Smith G, Najjar S, Ellingsen Ø, Skjaerpe T (2007) Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation 115:3086–3094
World Health Organisation (2008) The World Health Report: cardiovascular disease. Report of the Director-General. WHO, Geneva
Acknowledgments
This review article complies with Human Ethics guidelines at Victoria University and University of Western Sydney (Australia) and Massey University (New Zealand). The article was not financed by any research group or funding body and the authors have no conflicting interest with any funding or sponsoring organization.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Susan Ward.
Rights and permissions
About this article
Cite this article
Cornish, A.K., Broadbent, S. & Cheema, B.S. Interval training for patients with coronary artery disease: a systematic review. Eur J Appl Physiol 111, 579–589 (2011). https://doi.org/10.1007/s00421-010-1682-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-010-1682-5