Abstract
Cutaneous temperature sensitivity was tested in 13 male subjects prior to, during and after they breathed either a hypocapnic hypoxic (HH), or a normocapnic hypoxic (NH) breathing mixture containing 10% oxygen in nitrogen. Normocapnia was maintained by adding carbon dioxide to the inspired gas mixture. Cutaneous thresholds for thermal sensation were determined by a thermosensitivity testing device positioned on the plantar side of the first two toes on one leg. Heart rate, haemoglobin saturation, skin temperature at four sites (arm, chest, thigh, calf) and adapting temperature of the skin (T ad; degrees centigrade), i.e. the temperature of the toe skin preceding a thermosensitivity test, were measured at minute intervals. Tympanic temperature (T ty; degrees centigrade) was measured prior to the initial normoxic thermosensitivity test, during the hypoxic exposure and after the completion of the final normoxic thermosensitivity test. End-tidal carbon dioxide fraction and minute inspiratory volume were measured continuously during the hypoxic exposure. Ambient temperature, T ty, T ad and mean skin temperature remained similar in both experimental conditions. Cutaneous sensitivity to cold decreased during both HH (P<0.001) and NH conditions (P<0.001) as compared with the tests undertaken pre- and post-hypoxia. No similar effect was observed for cutaneous sensitivity to warmth. The results of the present study suggest that sensitivity to cold decreases during the hypoxic exposure due to the effects associated with hypoxia rather than hypocapnia. Such alteration in thermal perception may affect the individual’s perception of thermal comfort and consequently attenuate thermoregulatory behaviour during cold exposure at altitude.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypoxia has been shown to significantly alter the thermoregulatory behaviour in animals. During exposure to hypoxia animals prefer a cooler environment than during normoxia, as reflected in their selection of preferred ambient temperature (Hicks and Wood 1985; Gordon and Fogelson 1991; Wood 1991; Malvin and Wood 1992; Gordon 1997). The preference for a cooler environment results in a hypoxia-induced behavioural hypothermia (Hicks and Wood 1985; Gordon and Fogelson 1991). Thus, the fall in deep body temperature towards hypothermic levels is not defended behaviourally in the same manner during hypoxia as during normoxia (Wood 1991).
Information seems to be lacking with respect to the effect of hypoxia on thermal perception in humans. That moderate to severe hypoxia may substantially diminish neural function in humans is implicated by observations of hypoxia-induced decrements in visual (Fowler et al. 1982, 1993) and auditory perception (Fowler et al. 1994), cognitive function (Kennedy et al. 1989) and increments in reaction time (Fowler et al. 1987a, 1994). Assuming that hypoxia affects processes within the thermoregulatory system in the same manner as it has been shown to affect other sensory systems, this may consequently diminish thermal sensitivity, which would be manifested as an increase in cutaneous threshold for thermal sensation.
The perception of thermal stimuli is fundamental in formulating a judgement of thermal (dis)comfort. The latter is defined as a subjective indifference to the thermal environment (Mercer 2001). Skin and core temperature sensors transduce thermal energy into neural coded information, which is subsequently integrated in central thermoregulatory neural foci and conveyed to higher cortical centres, giving rise to a sensation of either cold or warmth, and to a perception of either pleasure or displeasure. The perception of thermal (dis)comfort thus results from the cortical integration of thermoafferent information (Cabanac 1969, 1981; Hensel 1976). The perception of thermal discomfort provides the basis for the initiation of behavioural thermoregulatory responses, which constitute the first defence against displacements of body temperature.
The perception of a temperature stimulus depends on the size (Kenshalo 1976) and site (Nadel et al. 1973; Crawshaw et al. 1975; Tipton and Golden 1987; Burke and Mekjavic 1991) of the thermally stimulated area, the rate of temperature change (Kenshalo 1976) and the adapting temperature of the skin (i.e. the steady-state temperature of the skin obtained prior to the application of a thermal stimulus) (Kenshalo 1976). Furthermore, several non-thermal factors, which interfere with neural information at one or more levels of the thermoregulatory system, have also been shown to influence the efficiency of temperature regulation. Namely, it has been demonstrated that non-thermal factors such as ageing (Collins et al. 1977, 1981, 1985; Collins and Exton-Smith 1983), inert-gas narcosis (Pertwee et al. 1986; Mekjavic and Sundberg 1992; Mekjavic et al. 1994, 1995; Cheung and Mekjavic 1995) and hypoglycaemia (Passias et al. 1996) all induce a change in thermal comfort and affect the regulation of deep body temperature. Usually, non-thermal factors widen the zone of thermal comfort (Collins et al. 1981; Mekjavic et al. 1994; Passias et al. 1996; Gordon 1997) by increasing the interval of ambient temperatures perceived as thermally comfortable (Mercer 2001). Such non-thermal factors may act either upon the transduction of thermal energy into neural coded temperature information, the transmission of sensory information from thermoreceptors to thermoregulatory foci, and/or upon its central integration. Furthermore, the efferent neuraxis and/or thermoregulatory effectors may also be affected.
Data from animal studies suggest that not only hypoxia, but also the hypoxia-induced hypocapnia may interfere with the thermoregulatory function (Gautier et al. 1987, 1989; Bonora and Gautier 1989; Rautenberg 1990; Barnas and Rautenberg 1990). The aim of the present study was therefore twofold: to test the hypothesis that hypoxia alters the perception of cold and warm cutaneous stimuli, and to discriminate between the possible effects of a hypoxic and a hypoxia-induced hypocapnic stimulus on thermal sensation. For this reason, cutaneous thermal sensitivity was evaluated during conditions of both hypocapnic hypoxia (HH) and normocapnic hypoxia (NH). We further hypothesised that any such hypoxia-induced decrement in thermal sensation, particularly the sensation of cold, may enhance the risk of cold injury. As cold injury is prevalent in the extremities and occurs primarily on toes (Foray 1992), we examined the effect of hypoxia on cutaneous thresholds for thermal sensation on the toes.
Methods
Thirteen male subjects volunteered for the study. Their average (SD) age was 22 (3) years, height 180 (4) cm and mass 74 (7) kg. The protocol of the study was approved by the National Ethics Committee of the Republic of Slovenia. All subjects were medically examined and their participation in the study was subject to physician’s approval. Subjects were familiarised with the protocol and gave their written consent to participate in the study.
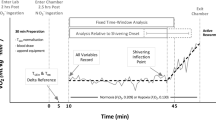
Cutaneous thresholds for thermal sensation were determined on several separate occasions. Initially, each subject participated in a training session to become acquainted with the test procedure and to minimise the effect of learning (Golja et al. 2003). Thereafter, they participated in two experimental trials, hypocapnic hypoxia (HH) and normocapnic hypoxia (NH), separated by a minimum of 7 days. In both trials subjects began by breathing room air (initial normoxic phase) and were then switched to breathing a humidified gas mixture containing 10% oxygen and 90% nitrogen for approximately 20 min (hypoxic phase). Thereafter, they were switched back to breathing room air (final normoxic phase). During the trials, the breathing mixture was directed to the inspiratory side of a Hans Rudolf respiratory valve (Hans Rudolph, Kansas City, Mo.) via corrugated respiratory hoses. Minute inspiratory volume (V I; litres per minute) was monitored with a turbine flow transducer (K 520, KL Engineering, Calif.) throughout the hypoxic phase in both trials. In the NH trial, the hypoxia-induced hypocapnia was prevented by regulating the flow of a gas mixture containing 12% carbon dioxide, 10% oxygen and 78% nitrogen to the inspired mixture, so that the end-tidal carbon dioxide (F ETCO2; per cent) was similar to that observed during the initial normoxic phase. The F ETCO2 was determined by continuously analysing the carbon dioxide content of expired air with a carbon dioxide analyser (Servomex 1400D O2/CO2, UK). In the HH trial, subjects inspired a gas mixture containing 10% oxygen and 90% nitrogen only. No attempt was made to maintain end-tidal carbon dioxide at a normocapnic level. The order of the two conditions was counterbalanced and the subjects were kept naive regarding the condition. The subjects were aware that they could terminate the trial or switch to breathing pure oxygen at any time during the hypoxic exposure.
Each subject conducted both experimental trials at the same time of day in a laboratory kept at 29°C. During the tests of thermal sensitivity subjects wore a short-sleeved T-shirt and long gym trousers. Skin temperature was measured with copper/constantan (T-type) thermocouples (Concept Engineering, Old Saybrook, Conn.) attached to four sites (arm, chest, thigh, calf). Mean skin temperature (T sk; degrees centigrade) was calculated as an non-weighted average from the four skin sites. A pulse oximeter (BCI International, Waukesha, Wis.) was attached to the second toe of the foot that was not involved in the thermosensitivity testing. Once instrumented, subjects rested in a semi-supine position on a chaise lounge chair for 15 min, to allow their skin temperatures to stabilise.
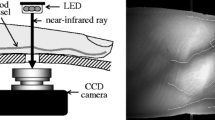
Cutaneous thresholds for thermal sensation were assessed with a Middlesex Thermal Testing System (MTTS, Howe Institute, Canvey Island, Essex, UK; see Fowler et al. 1987b). The MTTS consists of a thermode (Peltier element) with a surface area of 24 cm2 and mass of 165 g, and a controlling unit connected to a computer (Compaq Presario, Series CM 2060, Taiwan). The adapting temperature of the skin, i.e. the temperature of the toe skin preceding a thermosensitivity test, and the temperature of the stimulating thermode were continuously measured with NiCr/NiAl (K-type) thermocouple, connected to an Almemo data acquisition system (Almemo 2290-8 V5, Ahlborn, Holzkirchen, Germany).
The difference in thermosensitivity between the contralateral toes has not been investigated systematically. We therefore decided to test the thermosensitivity on the contralateral toes as opposed to right- or left-handedness, to control for the body site in case such differences existed. The thermosensitivity assessment was thus performed on the left-leg toes in right-handed subjects, and on the right-leg toes in left-handed subjects.
During the trials, subjects rested their feet on an inclined (45°) wooden board covered with a cotton towel. The stimulating thermode was attached to the plantar side of the first two toes with medical adhesive tape (Transpore, Tosama Domzale, Slovenia). The exact area of the thermally stimulated skin was determined after the completion of the trial by pressing a piece of Plexiglas with similar dimensions as the stimulating thermode against the two toes and outlining the area in contact. The outlined area was then copied to graph paper and the surface area was determined by counting the squares bound by the margins of the outlined area.
Subjects’ thermal thresholds for cold/warm sensation were determined by applying cooling/warming stimuli to the toes with the attached thermode. The rate of temperature change (1°C s−1) was identical for all stimuli, and the intensity of each thermal stimulus depended on the duration of the applied stimulus. The tests of temperature sensitivity were performed during the initial normoxic condition, 10 min into breathing the hypoxic mixture and 10 min after switching back to breathing the normoxic mixture. The order of the tests for cold and warm sensitivity was counterbalanced in the initial normoxic phase of each trial. In the hypoxic and in the final normoxic phases of the trials, the test of cold sensitivity always preceded the test of warm sensitivity to control for the dose-effect of hypoxia.
Tympanic temperature (T ty; degrees centigrade) was measured with an infrared tympanic thermometer (ThermoScan IRT 3020, Braun, Kronberg, Germany) prior to the initial normoxic thermosensitivity test, during the hypoxic exposure and after completion of the final normoxic thermosensitivity test.
Data analyses
Cutaneous thresholds for thermal sensation, ambient air temperature (T a; degrees centigrade) and T ty obtained in each trial were analysed with a one-way ANOVA for correlates samples. A paired t-test was used to compare T a, T ty, T sk, heart rate (HR), haemoglobin saturation (S aO2; per cent), V I and F ETCO2 between the HH and NH trials and the values obtained at the beginning of the hypoxic phase and those in minute 15 of the hypoxic phase for both, HH and NH trials.
Results
All subjects were able to complete at least 15 min of the hypoxic exposure with only mild signs or symptoms of hypoxia (lethargy, loss of concentration, hyperventilation). Three subjects did not observe any difference between NH and HH trials and ten subjects reported that the symptoms were milder during NH.
The average (SD) T a and humidity in the laboratory were 28.6 (0.6)°C and 24 (3)%, respectively, in the HH, and 28.8 (0.6)°C and 28 (6)%, respectively, in the NH trial. The size of the thermally stimulated area, i.e. the skin area on the first and second toe in contact with the stimulating thermode, was 7.3 (1.3) cm2 in both, the cold and warm sensitivity tests.
The average (SD) cutaneous threshold for the sensation of cold (n=13) obtained prior to (initial normoxic phase), during (hypoxic phase), and following (final normoxic phase) the hypoxic exposure was 4.7 (3.2)°C, 6.3 (3.5)°C and 4.6 (2.8)°C, respectively, during HH, and 4.7 (3.2)°C, 6.2 (3.2)°C and 5.3 (3.0)°C, respectively, during NH (Fig. 1A). The increase in the cutaneous threshold for the sensation of cold during the hypoxic phase was significant (P<0.001) in both the HH and NH trials. There were no significant differences (P>0.22) in the cutaneous threshold for the sensation of cold between the HH and NH trials in any of the three phases.
Average cutaneous threshold (SD) for the sensation of cold (A) and warmth (B), i.e. the absolute temperature change of the thermode upon sensation of cold and warmth, obtained prior to, during and following the hypoxic exposure in the hypocapnic hypoxia (HH; open bars) and the normocapnic hypoxia condition (NH; filled bars)
In contrast to cold stimulation, several subjects did not perceive warm stimuli on the toes. It was therefore only possible to determine the cutaneous threshold for the sensation of warmth in five subjects. The average (SD) cutaneous threshold for the sensation of warmth (n=5) obtained prior to (initial normoxia phase), during (hypoxic phase), and following (final normoxia phase) the hypoxic exposure was 11.3 (3.1)°C, 8.9 (2.9)°C and 8.0 (3.5)°C, respectively, in the HH, and 10.1 (3.0)°C, 9.2 (4.1)°C and 8.4 (3.9)°C, respectively, in the NH (Fig. 1B). In both trials, the cutaneous threshold for the sensation of warmth did not differ significantly between the normoxic and hypoxic phases.
There was no significant difference in the mean T sk between the two trials. At the onset of the initial normoxic thermosensitivity test, T sk was 34.0 (0.7)°C in the HH, and 34.2 (0.7)°C in the NH trial. Although the average T sk rose slightly during the course of experiment in both conditions, the change in T sk was not greater than 0.5°C (0.3)°C during the HH, and 0.5°C (0.4)°C during the NH trial.
T ty was also similar (P>0.10) in the two experimental conditions. During the initial normoxic phase, T ty was 37.0 (0.4)°C in the HH, and 36.8 (0.4)°C in the NH trial.
The adapting temperature of the skin (T ad; °C) during the cold sensitivity tests in HH was 31.2 (1.3)°C in the initial normoxic phase, 31.9 (1.8)°C during the hypoxic phase, and 32.8 (1.7)°C in the final normoxic phase. In NH, T ad was 32.1 (2.3)°C in the initial normoxic phase, 32.5 (1.9)°C in the hypoxic phase, and 32.9 (1.6)°C during the final normoxic phase. During all cold sensitivity tests T ad did not differ significantly (P>0.20) between the HH and NH trial. During the warm sensitivity tests in the HH, T ad was 32.9 (1.4)°C, 35.5 (1.7)°C and 35.6 (1.6)°C for initial normoxic, hypoxic and final normoxic phases, respectively. In the NH, T ad was 34.2 (0.8)°C, 36.7 (1.3)°C and 37.0 (1.3)°C in the initial normoxic, the hypoxic, and the final normoxic phase, respectively. During all warm sensitivity tests T ad did not differ significantly between the HH and NH trial (P>0.09).
The length of the hypoxic exposure was not the same for all subjects, as it depended upon the time required for the assessment of thermal sensitivity, which varied between subjects. As all subjects completed at least 15 min of hypoxia, the values for HR, S aO2, V I and F ETCO2 are reported for the beginning of the hypoxic exposure and for min 15 of the hypoxic exposure.
As seen in Table 1, HR (beats per minute) increased significantly (P<0.01) from average (SD) values of 80 (8) beats min−1 and 81 (12) beats min−1 at the beginning of the hypoxic phase in the HH and NH trials, respectively, to 91 (12) beats min−1 and 84 (10) beats min−1 by min 15 of the hypoxic phase in the HH and NH, respectively. The difference in HR between the HH and NH was not statistically significant (P>0.30).
Average (SD) S aO2at the toe decreased significantly (P<0.001) from resting values of 97 (1)% and 96 (1)% immediately prior to the hypoxic phase, to 72 (13)% and 80 (7)% by min 15 of the hypoxic phase in the HH and NH trials, respectively (Table 1). During the hypoxic phase, S aO2 was significantly higher (P<0.02) in the NH than in the HH trial.
V I increased significantly (P<0.002) in both conditions during the hypoxic phase. Immediately prior to the hypoxic exposure, V I was 9.5 (1.3) l min−1 in the HH and 10.0 (1.0) l min−1 in the NH trial. By min 15 of the hypoxic exposure V I increased to 12.6 (4.1) l min−1 (P<0.03) in the HH, and to 13.4 (1.7) l min−1 (P<0.001) in the NH trial (Table 1). V I was significantly higher in the NH than in the HH trial (P<0.05).
In HH, the F ETCO2 decreased significantly (P<0.001) from pre-hypoxic values of 4.2 (0.6)%, to 3.4 (0.9)% by min 15 of the hypoxia phase (Table 1). In the hypoxic phase of the NH, F ETCO2 stabilised at 4.4 (0.4)%, which was approximately the level observed during the initial normoxic phase.
Discussion
The results of the present study demonstrate that inspiring a breathing mixture containing 10% oxygen significantly decreases the sensation of cold in humans. No similar effect of hypoxia on the sensation of warmth was observed in the present study. The effect of hypoxia on the sensation of cold seems to be associated with hypoxia rather than with hypoxia-induced hypocapnia, as the thresholds for thermal sensation obtained in the hypoxic phase of the HH and NH conditions did not differ. The observed hypoxia-induced alteration in thermal sensitivity may predispose individuals to cold injury in cold hypoxic environment.
The absence of any significant difference in the temperature sensation thresholds between the NH and HH trials suggests that hypoxia-induced hypocapnia does not contribute to the observed alteration of cold sensation threshold during the hypoxic exposure. The hypoxia-induced hypocapnia does, however, affect the subjective assessment of the severity of hypoxic exposure. In HH, the minute ventilation was lower than in NH, which resulted in lower S aO2, and consequently more pronounced symptoms of hypoxia.
It is unlikely that hypoxia preferentially affected the cold receptors before the warm receptors. The fact that there was no significant effect of hypoxia on the sensation of warmth may be attributable to other mechanisms, such as: regional differences in cutaneous temperature sensitivity, variable density of temperature receptors and/or the effect of adapting temperature on the sensitivity of temperature receptors. However, it is possible that no significant effects of hypoxia on warm sensation were observed in the present study due to a small number of subjects involved in warm sensitivity testing.
It is well established that in humans, the skin is much more sensitive to cold stimulation, and the core region to warm stimulation. This is most likely associated with the greater cutaneous cold receptor density compared with warm receptor density. In the present study, toes were chosen as the region of interest for practical reasons as the majority of freezing and non-freezing cold injuries occur in this region (Foray 1992). We hypothesised that hypoxia may compromise thermal sensitivity and hence predispose individuals to cold injury.
The rate of temperature change used in the present study (1°C s−1) was higher than the rate of skin cooling normally anticipated during real-life conditions. However, based on the available neurophysiological evidence (Kenshalo 1976), the rate of temperature change will not affect either cold or warm thresholds, thus will not alter the temperature sensitivity, as long as the rate of temperature change is greater than 0.1°C s−1. At slower rates the threshold systematically increases and such effect is ascribed to the adaptation of thermoreceptors. If anything, with a smaller rate of skin cooling experienced in real-life conditions, the adaptation of thermoreceptors would occur faster, which would increase the possibility that the applied thermal stimulus would pass unnoticed, and would thus potentiate the effects of hypoxia upon the thermal sensation.
The static firing rate of cold and warm receptors as a function of adapting temperature describes a bell-shaped curve with peak frequencies occurring between 25 and 30°C for the former, and between 40 and 47°C for the latter (Pierau and Wurster 1981). A cooling stimulus initiated at a temperature of maximal activity of cold receptors will elicit a greater dynamic response than one initiated at a temperature at which the sensors are less sensitive (Kenshalo 1976). Similarly, a warming stimulus initiated at the temperature of the maximal response of warm receptors will elicit the greatest dynamic response. In the present study, our subjects’ perception of cooling or warming was a consequence of the dynamic response of the receptors within an approximately 7 cm2 stimulated region, to a corresponding 1°C s−1 cooling or warming stimulus. The adapting temperature during the cold sensitivity tests was much closer to the temperature of the maximal activity of the cold receptors, than was the adapting temperature during the warm sensitivity tests to the temperature of the maximal response of the warm receptors. A given cooling stimulus would therefore have elicited a much greater dynamic response from the cold receptors, than would a warming stimulus of a corresponding magnitude have elicited from the warm receptors. Consequently, the cooling stimulus would more likely be detected than the warming stimulus.
In the present study, the adapting temperature of the skin slightly increased from the pre-hypoxic to the post-hypoxic test in both HH and HN trials for both cold and warm sensitivity assessment. Should the change in adapting temperature cause the observed change in thermal thresholds, one would then expect, that the thresholds would be even more affected during the last post-hypoxic test where the adapting temperature was highest. However, in the post-hypoxic test, the thresholds have returned towards the pre-hypoxic value, which precludes any effect of the adapting temperature on the thermosensitivity in the present experiment.
Our findings of a reduced sensation to cold during hypoxia are in accordance with the results of Iggo and Paintal (1977), who demonstrated a diminished rate of firing of cutaneous cold receptors in primates resulting from a reduced oxygen supply to the region. Regardless of whether they reduced either the arterial blood flow to the skin (mechanical pressure, low blood pressure), or blood oxygenation (nitrogen ventilation), the result was a fall in cutaneous cold sensor responsiveness in that region.
That the cooling stimulus needs to be greater to be perceived during hypoxia, is most likely due to an attenuation of thermal information, as a consequence of an effect of hypoxia on neural membrane function. A nerve cell consumes energy for its metabolism, which consists of the basal and the activation part (Astrup 1982). The former supports basic cellular processes that function even when synaptic transmission is blocked, and maintains the membrane function. The latter supports synaptic transmission and is more susceptible to oxygen or glucose deprivation than the basal part (Astrup 1982). As the oxygen supply diminishes below the metabolic demands of the nerve tissue, the energy-requiring cell functions are sequentially switched off, with synaptic transmission failing first (Astrup 1982). The prompt abolishment of synaptic function reveals its high dependability on oxygen. When the oxygen supply is reduced even further, the membranes of nerve cells can no longer maintain their function. Finally, as the cellular ATP stores become depleted, the Na+/K+ ATP-ase transport fails and the net ion current through the membrane results in membrane depolarisation and complete loss of neural cell function. The membrane failure is the final step in the loss of neural function as it is closely associated with irreversible structural cell damage (Astrup 1982). These observations suggest that synaptic function is the first neural process to become affected during oxygen depletion.
Although only speculative, the results of the present study may be explained by the manner in which hypoxia affects resting membrane and synaptic function. The resting membrane potential in anoxia is not immediately diminished (Hansen et al. 1982). Instead, the membrane of neural cells firstly becomes hyperpolarized, which decreases the excitability of the cells. Although the precise mechanism remains unknown, hyperpolarization results from an increase in the outward K+ current, as a consequence of an anoxia-induced increase in the conductance of transmembrane K+ channels (Hansen et al. 1982; Krnjevic and Leblond 1989; Martin et al. 1994).
Findlater et al. (1987) reported that slowly adapting type I cutaneous mechanoreceptors (Merkel cells) reduced their activity in a hypoxic environment. During hypoxia, the number of dense-cored vesicles that were most probably involved in the release of neurotransmitter in the synaptic cleft significantly decreased. The intensity of electrical stimulation sufficient to initiate an action potential in the afferent fibre, however, remained unchanged during hypoxia. This suggests that the resting potential of nerve cells did not change during hypoxia, but that synaptic function abated, and consequently diminished the afferent nervous activity. This observation is consistent with the findings of Nelson and Frank (1963) who studied the resting potential of cat motoneurons during oxygen depletion. They reported that even exposure to several minutes of anoxia did not produce more than negligible changes in motoneurons’ resting potential. Thus, for several minutes during anoxia the activity of Na+/K+ ATP-ase seems to remain relatively unaffected. Compared to anoxia, the effect of oxygen depletion on Na+/K+ ATP-ase activity must be even smaller during hypoxia, as the oxygen supply is limited, but not completely abolished.
The cutaneous thresholds for thermal sensation obtained in the present study were greater than those obtained in other thermosensitivity studies (Bravenboer et al. 1992). The difference may be due to either different methods by which thermosensitivity is assessed, various thermal sensitivity of skin areas, or both. Thermosensitivity has been often determined on other body sites (Jamal et al. 1985; Meh and Denislic 1994), but data on thermal sensitivity of the toes is lacking. Regional differences in thermosensitivity (Nadel et al. 1973; Crawshaw et al. 1975; Tipton and Golden 1987; Burke and Mekjavic 1991) may also contribute to the observed difference in thresholds between studies.
We conclude that hypoxia diminishes cold sensitivity of the toes, a region, which is the most susceptible to freezing and non-freezing cold injury. As a consequence, the perception of cold and ultimately behavioural thermoregulatory actions may be compromised, thus augmenting the risk of cold injury to the region.
References
Astrup J (1982) Energy-requiring cell functions in the ischemic brain. Their critical supply and possible inhibition in protective therapy. J Neurosurg 56:482–497
Barnas GM, Rautenberg W (1990) Shivering and cardiorespiratory responses during normocapnic hypoxia in the pigeon. J Appl Physiol 68:84–87
Bonora M, Gautier H (1989) Effects of hypoxia on thermal polypnea in intact and carotid body-denervated conscious cats. J Appl Physiol 67:578–583
Bravenboer B, van Dam PS, Hop J, vd SJ, Erkelens DW (1992) Thermal threshold testing for the assessment of small fibre dysfunction: normal values and reproducibility. Diabet Med 9:546–549
Burke WE, Mekjavic IB (1991) Estimation of regional cutaneous cold sensitivity by analysis of the gasping response. J Appl Physiol 71:1933–1940
Cabanac M (1969) Plaisir ou Déplaisir de la Sensation Thermique et Homothermique. Physiol Behav 4:359–364
Cabanac M (1981) Physiological signals for thermal comfort. In: Cena K, Clark JA (eds) Bioengineering, thermal physiology and comfort. Elsevier, Amsterdam, pp 181–192
Cheung SS, Mekjavic IB (1995) Human temperature regulation during subanesthetic levels of nitrous oxide-induced narcosis. J Appl Physiol 78:2301–2308
Collins KJ, Exton-Smith AN (1983) Thermal homeostasis in old age. J Am Geriatr Soc 31:519–524
Collins KJ, Dore C, Exton-Smith AN, Fox RH, MacDonald IC, Woodward PM (1977) Accidental hypothermia and impaired temperature homoeostasis in the elderly. Br Med J 1:353–356
Collins KJ, Exton-Smith AN, Dore C (1981) Urban hypothermia: preferred temperature and thermal perception in old age. Br Med J (Clin Res Ed) 282:175–177
Collins KJ, Easton JC, Belfield-Smith H, Exton-Smith AN, Pluck RA (1985) Effects of age on body temperature and blood pressure in cold environments. Clin Sci (Lond) 69:465–470
Crawshaw LI, Nadel ER, Stolwijk JA, Stamford BA (1975) Effect of local cooling on sweating rate and cold sensation. Pflugers Arch 354:19–27
Findlater GS, Cooksey EJ, Anand A, Paintal AS, Iggo A (1987) The effects of hypoxia on slowly adapting type I (SAI) cutaneous mechanoreceptors in the cat and rat. Somatosens Res 5:1–17
Foray J (1992) Mountain frostbite. Current trends in prognosis and treatment (from results concerning 1261 cases). Int J Sports Med 13 [Suppl 1]:S193–S196
Fowler B, White PL, Wright GR, Ackles KN (1982) The effects of hypoxia on serial response time. Ergonomics 25:189–201
Fowler B, Taylor M, Porlier G (1987a) The effects of hypoxia on reaction time and movement time components of a perceptual-motor task. Ergonomics 30:1475–1485
Fowler CJ, Carroll MB, Burns D, Howe N, Robinson K (1987b) A portable system for measuring cutaneous thresholds for warming and cooling. J Neurol Neurosurg Psychiatry 50:1211–1215
Fowler B, Banner J, Pogue J (1993) The slowing of visual processing by hypoxia. Ergonomics 36:727–735
Fowler B, Prlic H, Brabant M (1994) Acute hypoxia fails to influence two aspects of short-term memory: implications for the source of cognitive deficits. Aviat Space Environ Med 65:641–645
Gautier H, Bonora M, Remmers JE (1989) Effects of hypoxia on metabolic rate of conscious adult cats during cold exposure. J Appl Physiol 67:32–38
Gautier H, Bonora M, Schultz SA, Remmers JE (1987) Hypoxia-induced changes in shivering and body temperature. J Appl Physiol 62:2477–2484
Golja P, Tipton MJ, Mekjavic IB (2003) Cutaneous thermal thresholds—the reproducibility of their measurements and the effect of gender. J Therm Biol 28:341–346
Gordon CJ (1997) The role of behavioral thermoregulation as a thermoeffector during prolonged hypoxia in the rat. J Therm Biol 22:315–324
Gordon CJ, Fogelson L (1991) Comparative effects of hypoxia on behavioral thermoregulation in rats, hamsters, and mice. Am J Physiol 260:R120–R125
Hansen AJ, Hounsgaard J, Jahnsen H (1982) Anoxia increases potassium conductance in hippocampal nerve cells. Acta Physiol Scand 115:301–310
Hensel H (1976) In: Zotterman Y (ed) Sensory functions of the skin in primates with special reference to man. Proceedings of the international symposium. Pergamon, Oxford, pp 331–353
Hicks JW, Wood SC (1985) Temperature regulation in lizards: effects of hypoxia. Am J Physiol 248:R595–R600
Iggo A, Paintal AS (1977) The metabolic dependence of primate cutaneous cold receptors [proceedings]. J Physiol (Lond) 272:40P–41P
Jamal GA, Hansen S, Weir AI, Ballantyne JP (1985) An improved automated method for the measurement of thermal thresholds. 1. Normal subjects. J Neurol Neurosurg Psychiatry 48:354–360
Kennedy RS, Dunlap WP, Banderet LE, Smith MG, Houston CS (1989) Cognitive performance deficits in a simulated climb of Mount Everest: Operation Everest II. Aviat Space Environ Med 60:99–104
Kenshalo DR (1976) In: Zotterman Y (ed) Sensory functions of the skin in primates with special reference to man. Proceedings of the international symposium. Pergamon, Oxford, pp 305–330
Krnjevic K, Leblond J (1989) Changes in membrane currents of hippocampal neurons evoked by brief anoxia. J Neurophysiol 62:15–30
Malvin GM, Wood SC (1992) Behavioral hypothermia and survival of hypoxic protozoans Paramecium caudatum. Science 255:1423–1425
Martin RL, Lloyd HG, Cowan AI (1994) The early events of oxygen and glucose deprivation: setting the scene for neuronal death? Trends Neurosci 17:251–257
Meh D, Denislic M (1994) Quantitative assessment of thermal and pain sensitivity. J Neurol Sci 127:164–169
Mekjavic IB, Sundberg CJ (1992) Human temperature regulation during narcosis induced by inhalation of 30% nitrous oxide. J Appl Physiol 73:2246–2254
Mekjavic IB, Passias T, Sundberg CJ, Eiken O (1994) Perception of thermal comfort during narcosis. Undersea Hyperb Med 21:9–19
Mekjavic IB, Savic SA, Eiken O (1995) Nitrogen narcosis attenuates shivering thermogenesis. J Appl Physiol 78:2241–2244
Mercer J (2001) Glossary of terms for thermal physiology. The Commission for Thermal Physiology of the International Union of Physiological Sciences. Jpn J Physiol 51:245–280
Nadel ER, Mitchell JW, Stolwijk JA (1973) Differential thermal sensitivity in the human skin. Pflugers Arch 340:71–76
Nelson PG, Frank K (1963) Intracellularly recorded responses of nerve cells to oxygen deprivation. Am J Physiol 205:208–212
Passias TC, Meneilly GS, Mekjavic IB (1996) Effect of hypoglycemia on thermoregulatory responses. J Appl Physiol 80:1021–1032
Pertwee RG, Marshall NR, Macdonald AG (1986) Effects of subanesthetic doses of inert gases on behavioral thermoregulation in mice. J Appl Physiol 61:1623–1633
Pierau FK, Wurster RD (1981) Primary afferent input from cutaneous thermoreceptors. Fed Proc 40:2819–2824
Rautenberg W (1990) Control of cardiorespiration during shivering thermogenesis in pigeons. In: Bligh J, Voigt K (eds) Thermoreception and temperature regulation. Springer, Berlin Heidelberg New York, pp 200–208
Tipton MJ, Golden FS (1987) The influence of regional insulation on the initial responses to cold immersion. Aviat Space Environ Med 58:1192–1196
Wood SC (1991) Interactions between hypoxia and hypothermia. Annu Rev Physiol 53:71–85
Acknowledgement
This study was supported, in part, by the Ministry of Education, Science and Sport of the Republic of Slovenia.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Golja, P., Kacin, A., Tipton, M.J. et al. Hypoxia increases the cutaneous threshold for the sensation of cold. Eur J Appl Physiol 92, 62–68 (2004). https://doi.org/10.1007/s00421-004-1058-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-004-1058-9