Abstract
Prolonged exercise is associated with increased plasma levels of the cytokine interleukin-6 (IL-6). Both circulating catecholamine levels and exercise intensity have been related to the exercise-derived IL-6. During hypoxia and acclimatization, changes in sympathetic activity is seen, and also a given workload becomes more intense in hypoxia. Therefore, hypoxia offers a unique opportunity to study the effect of catecholamines and intensity on exercise-derived IL-6. In the present study, eight Danish sea-level residents performed 60 min of cycle ergometer exercise at sea level (SL) (154 W, 45% maximal O2 consumption, V̇O2max), in acute (AH) and chronic hypoxia (CH), at the same absolute (abs) (AHabs=154 W, 54% V̇O2max; CHabs=154 W, 59% V̇O2max) and same relative (rel) (AHrel=130 W, 46% V̇O2max; CHrel=120 W, 44% V̇O2max) workload. We hypothesized that the IL-6 response to exercise at the same absolute workload would be augmented during hypoxia compared with sea level, and that these changes would not correlate with changes in catecholamines. In AHabs (2.35 pg·ml−1) and CHabs (3.34 pg·ml−1) the IL-6 response to exercise was augmented (p<0.05) compared with that at sea level (0.78·ml−1). In addition, after 60 min of bicycling at sea level, AHrel (1.02 pg·ml−1) and CHrel (1.31 pg·ml−1) resulted in similar IL-6 responses. The augmented IL-6 response during AHabs and CHabs did not match changes in circulating catecholamine levels when comparing all trials. We conclude that the plasma IL-6 concentration during exercise in hypoxia is intensity dependent, and that factors other than catecholamine levels are more important for its regulation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prolonged exercise is associated with increased plasma levels of the cytokine interleukin-6 (IL-6) (Pedersen et al. 2001). It has been demonstrated that contracting skeletal muscle releases IL-6, and that this release can account for the systemic IL-6 increase observed during exercise (Steensberg et al. 2000). In addition, brain (Nybo et al. 2002) and peritendon tissue (Langberg et al. 2002) release small amounts of IL-6 during exercise. At rest fat tissue is responsible for up to 30% of the plasma IL-6 (Mohamed-Ali et al. 1997), and it was recently demonstrated that this release was augmented post-exercise, whereas it was not increased during exercise (Lyngsø et al. 2002). The plasma IL-6 concentration during exercise has previously been correlated with the circulating catecholamine concentration (DeRijk et al. 1994; Mazzeo et al. 2000b; Papanicolaou et al. 1996; van Gool el al. 1990), but a recent publication demonstrated that epinephrine infusion, reaching exercise epinephrine levels, only resulted in a fivefold increase in plasma IL-6 compared with a 29-fold induction during exercise (Steensberg et al. 2001a). In another study (Steensberg et al. 2000b) IL-6 differences across an exercising and a resting leg were measured, and only the exercising leg released IL-6 in spite of the fact that both legs experienced the same catecholamine concentration. In contrast, one recent study found that an α-adrenergic blocker blunted the plasma IL-6 response to exercise at sea level and during hypoxia (Mazzeo et al. 2000b). Humans exposed to hypoxia experience changes in sympathetic activity with acclimatization (Mazzeo et al. 1991, 1995) and the influence of catecholamines on IL-6 concentrations can thus favourably be investigated in a hypoxic environment. Moreover, resting epinephrine is elevated after 2–3 days of hypoxic exposure, and thereafter gradually decreases towards sea level values, whereas a rise in norepinephrine is reported to occur more gradually, and not to return to sea level values with acclimatization (Mazzeo et al. 1991, 1995, 1998, 2000a, 2000b). When using hypoxia to study the role of catecholamines in exercise-induced changes in plasma IL-6, it must be taken into account that maximal O2 consumption (V̇O2max) decreases with increasing altitude, and therefore a workload performed at sea level will be relatively more intense when performed at altitude (Dill et al. 1931). This is important because studies have demonstrated that the IL-6 response to exercise is dependent on the exercise intensity. Moreover, during a marathon race a correlation between the intensity of exercise and the increase in plasma IL-6 was found (Ostrowsky et al. 2000). In support, an increase in plasma-IL-6 was demonstrated after only 6 min of intense rowing exercise (Nielsen et al. 1996), whereas exercise protocols using less intense exercise did not find an increase until 30 min of exercise (Starkie et al. 2001a, 2001b).
Also hypoxia per se is associated with an increase in plasma IL-6 in most studies (Hartmann et al. 2000; Klausen et al. 1997; Mazzeo et al. 2000b), whereas one study did not find an effect (Pavlicek et al. 2000). The increased sympathetic activity during hypoxia has been associated with the increase in plasma IL-6 (Mazzeo et al. 2000b). In addition, the development of high altitude pulmonary edema (HAPE) seems to further elevate plasma IL-6 (Maggiorini et al. 2000).
The purpose of the present study was to examine the effect of catecholamines and exercise intensity on plasma IL-6 concentrations during exercise using hypoxia as a model. We hypothesized that exercising at the same relative workload at sea level and during acute and chronic hypoxia would result in the same increases in plasma IL-6, whereas exercise at the same absolute workload would result in an increased IL-6 response during acute and chronic hypoxia compared with sea level. Furthermore, we hypothesized that the IL-6 response to exercise would be unaffected by differences in catecholamines.
Methods
Subjects
Eight trained (physical education college students) sea-level residents (six males and two females) [V̇O2max=4.2 (0.3) l·min−1, height=186 (2) cm, weight=78 (3) kg, age=25 (1) year, mean (SD)] took part in this study. All subjects gave their informed consent before participation. The research protocol was approved by the Ethical Committee of Copenhagen and Frederiksberg communities (KF11–050/01), and in accordance with the declaration of Helsinki II. This study was part of a large high altitude expedition to the Andes mountains of Bolivia, and the methods are described in detail elsewhere (Lundby and van Hall 2002).
Acclimatization
The subjects were flown from Copenhagen (sea level) to La Paz (Bolivia), and spent two nights at 3800 m (Fig. 1). Hereafter they lived in the higher part of La Paz at 4100 m during the remaining time of the study. To keep a similar activity level as in Denmark, subjects were encouraged to perform outdoor activities such as cycling, soccer, basketball, hiking, and rock climbing. Food supplies were ample. All testing was performed in a nearby hospital.
Preliminary testing of subjects
V̇O2max was determined by the use of a progressive exercise protocol on a cycle ergometer (Monark 824E, Sweden). Exercise started with a 15-min warm-up period of 100 W at 80 rpm, after which the workload was increased by 40 W every 2 min 30 s until exhaustion. V̇O2max was defined as the value obtained when an increase in exercise intensity of 40 W did not result in any further increase in V̇O2 uptake (V̇O2max; i.e. a decrease, no change, or an increase <150 ml·min−1). This procedure resulted in a plateau in V̇O2 in seven out of eight subjects; the last subject indicated that the exercise protocol elicited maximal exercise in secondary parameters, i.e. high heart rate, lactate, and respiratory exchange ratio (RER) values. Measurements were done on three separate occasions: (1) at sea level, (2) at sea level while inducing acute hypoxia by breathing 12.4% O2 in N2 (equivalent to 4100 m) from a Douglas bag (the subjects started to breath the hypoxic gas mixture 10 min before the start of exercise) and (3) after approximately 4 weeks at 4100 m. To accustom the subjects to the exercise protocol, each subject completed the exercise protocol at sea level and in acute hypoxia before the actual maximal exercise test.
Testing protocol
All subjects were investigated on five separate occasions and performed 60 min of ergometer cycle exercise at 50% of sea level V̇O2max at sea level (SL), and again at the same absolute workload when acutely exposed to 4100 m (AHabs), and after 3.5–4.5 weeks of exposure to 4100 m (CHabs). Similarly they were investigated at 50% of acute and chronic hypoxic V̇O2max in acute (AHrel) and chronic hypoxia (CHrel), i.e. eliciting the same relative work intensity as at sea level. Acute hypoxia was induced by letting the subjects breath 12.4% O2 in N2 from a Douglas bag, and was initiated 10 min before rest measurements. Chronic hypoxic measurements were completed in hospital settings at 4100 m in La Paz, Bolivia. The sea level and acute hypoxic trials were initiated in March in Copenhagen, starting with the sea level trials. The acute trials were conducted in random order. The chronic hypoxic trials were conducted randomly between days 24 and 32 at altitude, the average being 4 weeks. All trials were at least 4 days apart. Resting samples were also obtained after 8 weeks at 4100 m. On each occasion (except at 8 weeks) the subjects reported to the laboratory 12 h post-absorptive and were fed 0.7 g cornflakes/kg body weight with an unlimited amount of skimmed milk. They were allowed to drink water ad libitum. Exercise started exactly 2 h after finishing the meal. Then, 45 min before the start of exercise, a 20 G catheter was inserted in an antecubital vein, after which the subjects lay down for 15 min before measurements began. Pulmonary gas exchange, arterial oxygen saturation, and blood samples were taken at rest and after 15, 30, 45 and 60 min of exercise.
Measurements
The same equipment was used in all experimental trials. V̇O2, CO2 output (V̇CO2), and minute ventilation (V̇ E) were measured on-line by the use of standard open-circuit techniques (Oxygen Analyzer S-3A/I, Ametek, USA; LB-2, Beckman, USA; VRDC/HC-1, Parvo Medics, USA). Before use, the system was calibrated against two gas mixtures previously measured by the micro Scholander method. Flow was calibrated with a 3 l syringe. Pulmonary gas exchange was measured over a period of 5 min on each measure point.
Blood samples obtained for determination of IL-6 were drawn over 5 s in 5 ml syringes (Becton Dickinson, Spain) and transferred to a 10 ml centrifuge tube containing EDTA and immediately centrifuged at 5000 rpm for 5 min at 4°C. The plasma was transferred to Eppendorf tubes and immediately stored at −50°C for later analysis. IL-6 was determined via commercially available high sensitivity ELISA kit (R and D systems, Minneapolis, Minn., USA) in Denmark. From the same sample also free fatty acids (FFA), glycerol, glucose, and lactate were analysed, and the results are published elsewhere (Lunbdy and van Hall 2002).
Blood samples for analysis of epinephrine (E) and norepinephrine (NE) were obtained and stored in the same manner as above, but transferred to centrifuge tubes containing EGTA instead of EDTA (Lundby and van Hall 2002). The analysis was performed by high performance liquid chromatography (HPLC) (Waters, Millipore, Mass., USA). The 15, 30, 45, and 60 min sample points were averaged. Oxygen saturation was monitored throughout the protocol by a pulse oxymeter (Datex, Instrumentarium, Finland) with the sensor attached to the fingertip of the first or second finger. Blood samples were transported from Bolivia to Denmark in dry-ice-filled containers.
Statistics
All data are expressed as means (SE), except when stated differently. IL-6 data were log transformed to obtain a normal distribution. Statistical difference was tested by one-way ANOVA. Pair-wise differences were identified using Newman-Keuls post hoc procedure. The level of significance was set at p<0.05.
Results
Maximal exercise tests
At SL maximal workload was 356 (23) W and elicited a V̇O2 of 4.2 (0.3) l·min−1 and a heart rate (HR) of 187 (8) beats·min−1. Compared with SL V̇O2max decreased (p<0.05) to 3.5 (0.2) l·min−1 in acute hypoxia. W max and HRmax decreased (p<0.05) accordingly to 281 (19) W and 176 (8) beats·min−1. Compared with acute hypoxia acclimatization had no further effect on the above parameters, the values being 3.2 (0.2) l.min−1, 254 (17) W, and 177 (7) beats·min−1, respectively during chronic hypoxia.
The 60-min cycle exercise test
At sea level the 60 min of cycle exercise elicited on average 45% of V̇O2max (Table 1). In AHabs and CHabs this workload corresponded to 54 and 59% of V̇O2max, respectively. When correcting the workload in AHrel and CHrel for the decrease in V̇O2max, the exercise intensity elicited 46 and 44% of the corresponding V̇O2max. The difference in exercise intensities also elicited a higher plasma lactate and HR during AHabs and CHabs, but not during AHrel and CHrel.
Plasma IL-6 and catecholamines
The resting plasma IL-6 at sea level was 0.96 (0.09) pg·ml−1 (Fig. 2A). The resting plasma IL-6 at acute hypoxia was not significantly different from that at sea level, being respectively 1.8 (0.72) and 1.18 (0.16) pg·ml−1 before the two exercise trials. In contrast, the plasma IL-6 was augmented (p<0.05) at rest in the subjects before performing the relative workload exercise test at chronic hypoxia, but not before performing the absolute workload test, being 3.2 (0.98) and 1.5 (0.3) pg·ml−1 respectively. This was the case even though the two trials were performed in a randomized order. After 8 weeks at high altitude the plasma IL-6 was significantly elevated (p<0.05) compared to sea level, being 2.57 (0.54) pg·ml−1.
A Plasma interleukin-6 (IL-6) at rest at sea level, acute and chronic hypoxia. B Delta plasma IL-6 in response to 60 min of exercise at sea level, acute and chronic hypoxia. Values are mean (SE); n=8 in each trial. Significant differences: * p<0.05 compared with the other experimental trials, # p<0.05 compared with rest
In order to present the exercise data as simply as possible, the plasma-derived parameters obtained after 15, 30, 45, and 60 min of exercise are all averaged to one exercise value, i.e. one exercise value for each experimental setting. Plasma IL-6 increased in response to exercise in all trials (Fig. 2B). The exercise-induced change in plasma IL-6 was 2.35 (0.28) and 3.34 (0.76) pg·ml−1 during AHabs and CHabs respectively, this increase being augmented (p<0.05) compared to exercise at sea level, AHrel, and CHrel. There were no differences between changes in plasma IL-6 during exercise at sea level, AHrel and CHrel, the increases being 0.78 (0.13), 1.02 (0.39) and 1.31 (0.29) pg·ml−1 respectively.
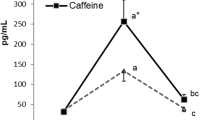
Plasma epinephrine increased (p<0.05) approximately twofold during exercise in AHabs compared with all other trials (Fig. 3). Norepinephrine was elevated (p<0.05) during exercise at AHabs, CHabs and CHrel by 186–263% compared to exercise in SL and AHrel.
A Average plasma epinephrine concentrations (nmol·l−1), and B average plasma norepinephrine concentrations (nmol·l−1) during 60 min of exercise at sea level, acute and chronic hypoxia. Values are mean (SE); n=8 in each trial. Significant differences: * p<0.05 compared with the other experimental trials
Discussion
The major findings in this study are that: (1) submaximal exercise performed at the same relative percent of V̇O2max in acute and chronic hypoxia, as compared to sea level, induces similar increases in plasma IL-6 concentrations; and (2) exercise in acute and chronic hypoxia at the same absolute workload as at sea level further increased the plasma IL-6 concentration compared to sea level. In addition, the results support the idea that catecholamines do not play a major role in the induction of the IL-6 release during exercise.
The limitations of the present study include the use of males and females as subjects, and the use of two different approaches to induce hypoxia in the acute and chronic situation. Firstly, there seems to be no difference in the exercise-induced increase in IL-6 between males and females (B.K. Pedersen, personal communication). Secondly, in acute hypoxia the low O2 saturation was achieved by reducing FIO2 and keeping barometric pressure constant, whereas the same degree of hypoxia was achieved in the chronic situation by reducing barometric pressure and keeping FIO2 constant. This hypoxia model has been applied on numerous high altitude research expeditions. However, recently the use of normobaric hypoxia against hypobaric hypoxia showed different physiological responses in ventilatory parameters (Savourey et al. 2003). Whether metabolic parameters are affected as well is at present unknown.
The finding that exercise at the same absolute workload during hypoxia, as compared with sea level, augments the plasma IL-6 response is in line with the recent study by Mazzeo et al. (2000b), and supports the theory that exercise intensity as such influences the IL-6 response to exercise. Of note, in the present study a difference in exercise intensity of only 45% versus 55% of V̇O2max resulted in an approximately threefold difference in the IL-6 response.
It is well documented that, as exercise intensity increases, there is a gradual shift from fat towards carbohydrate oxidation in the contracting skeletal muscle (Christensen and Hansen 1939), ultimately providing almost all of the substrate at V̇O2max. The increase in carbohydrate oxidation during exercise has been shown to result mostly from an increase in muscle glycogen utilization compared to a less increased blood glucose uptake (Febbrario et al. 2000). In the present study, no muscle glycogen measurement was obtained; however, it is reasonable to assume that, during AHabs and CHabs, the breakdown of glycogen must be higher than during the SL, AHrel and CHrel trials, due to the relatively higher exercise intensity, ultimately resulting in a lower intra muscular glycogen content. Also, as published in our accompanying paper (Lundby and van Hall 2002), the oxidation of carbohydrates during AHabs and CHabs is significantly higher than during AHrel and CHrel. Interestingly, it was recently shown that a contracting leg with low glycogen released IL-6 1 h before the control leg (Steensberg et al. 2001b). Furthermore, the leg with the lowest glycogen content at the end of exercise expressed the highest level of IL-6 mRNA regardless of pre-exercise glycogen levels. Although no measurements of glycogen, IL-6 expression or IL-6 release in the exercising muscle were performed in this study, it is tempting to speculate that the higher carbohydrate utilization in the working muscle during AHabs and CHabs presumably resulting in lower glycogen levels would cause the augmented plasma IL-6 concentrations during these trials.
As previously mentioned, catecholamines have been hypothesized to be involved in the IL-6 response to exercise (DeRijk et al. 1994; Mazzeo et al. 2000b; Papanicolaou et al. 1996; van Gool el al. 1990). In contrast, other recent studies (Steensberg et al. 2000, 2001a) have not found support for catecholamines to play a major role in the exercise-induced IL-6 response. In the present study, the IL-6 response to exercise was augmented in AHabs and CHabs when compared to exercise at SL, AHrel and CHrel. However, epinephrine was only augmented during exercise at AHabs. In addition, plasma norepinephrine was similarly elevated during exercise at AHabs, CHrel and CHabs compared to exercise at SL and AHrel, despite the demonstration that only exercise at AHabs and CHabs resulted in increased plasma IL-6 levels compared to exercise at SL, AHrel and CHrel. Therefore, these results suggest that catecholamines are not the main regulators of the IL-6 response during exercise.
Most studies have reported augmented resting plasma levels of IL-6 at high altitude; however, the elevations are not uniform. One study has reported an effect after 4 h of hypoxic conditions (Mazzeo et al. 2000b). In the present study the resting plasma IL-6 level after ~10 min of hypoxic conditions was unchanged compared with sea level. Regarding chronic hypoxia, the present study did not demonstrate a clear picture. Thus, after 3–4 weeks of high altitude plasma IL-6 was either augmented or unchanged in the same subjects measured on two different occasions. After 8 weeks of high altitude exposure IL-6 was elevated in all subjects compared with sea level. Plasma IL-6 has not been measured after such a long period of high altitude exposure before, but the finding is in line with the observed effect of 2–12 days of high altitude exposure (Klausen et al. 1997; Mazzeo et al 2000b). The plasma IL-6 concentrations reported in these studies were between 2.5 and 10 pg ml−1, and thus not as high as the levels seen during infections (Bruunsgaard et al. 1999). In contrast, one study found that individuals with high-altitude pulmonary edema (HAPE) after exposure to high altitude had plasma levels of IL-6 >20 pg ml−1, whereas non-HAPE individuals did not develop an increase in plasma IL-6 (Kleger et al. 1996; Maggiorini et al. 2000). Also, the bronchoalveolar fluid of patients with HAPE contains elevated levels of IL-6 (Kubo et al. 1996). The literature therefore suggests that hypoxia is associated with non-pathophysiological elevations in plasma IL-6, whereas development of HAPE results in further elevated plasma IL-6, possible related to inflammation.
In conclusion, this study suggests that catecholamines are not key regulators of the IL-6 response to exercise. In contrast, during exercise, the IL-6 response depends heavily on exercise intensity. Furthermore, this study confirms the observation that chronic hypoxia results in elevated plasma IL-6.
References
Bruunsgaard H, Skinhøj P, Quist J, Pedersen BK (1999) Elderly humans show prolonged in vivo inflammatory activity during pneumococcal infections. J Infect Dis 180:551–554
Christensen EH, Hansen O (1939) Respiratorische quotient – Bestimmungen in Ruhe und bei Arbeit. Skand Arch Physiol 81:137–151
DeRijk RH, Boelen A, Tilders FJ, Berkenbosch F (1994) Induction of plasma interleukin-6 by circulating adrenalin in the rat. Psychoneuroendocrinology 19:155–163
Dill DB, Edwards HT, Fölling A, Oberg SA, Pappenheimer AM, Talbott JH (1931) Adaptations of the organism to changes in oxygen pressure. J Physiol (Lond) 71:47–63
Febbrario MA, Keenan J, Angus DJ, Campbel SE, Garovoy MR (2000) Preexercise carbohydrate ingestion, glucose kinetics, and muscle glycogen use: effect of the glycemic index. J Appl Physiol 89(5):1845–1851
Hartmann G, Tschöp M, Fischer R, Bidlingmaier C, Riepl R, Tschöp K, Hautmann H, Enders S, Toepfer M (2000) High altitude increases circulating interleukin-6, interleukin-1 receptor antagonist and c-reactive protein. Cytokine 12:246–252
Klausen T, Olsen NV, Poulsen TD, Richalet JP, Pedersen BK (1997) Hypoxemia increases serum interleukin-6 in humans. Eur J Appl Physiol 76:480–482
Kleger GR, Bartsch P, Vock P HB, Roberts LJ 2nd, Balsamo V (1996) Evidence against an increase in capillary permeability in subjects exposed to high altitude. J Appl Physiol 81(5):1917–1923
Kubo K, Hanaoka M, Yamaguchi S, Hayona T, Hayasaka M, Koizumi T, Fujimoto K, Kobayashi T, Honda T (1996) Cytokines in bronchoalveolar lavage fluid in patients with high altitude pulmonary oedema at moderate altitude in Japan. Thorax 51:739–742
Langberg H, Olesen JL, Gemmer C, Kjaer M (2002) Substantial elevation of interleukin-6 concentrations in peritendinous, but not muscle, following prolonged exercise. J Physiol (Lond) 542:985–990
Lundby C, van Hall G (2002) Submaximal substrate utilization is unaffected by acute and chronic hypoxia when expressed relatively to maximal oxygen uptake. Acta Physiol Scand 176:195–201
Lyngsø D, Simonsen L, Bülow J (2002) Interleukin-6 production in human subcutaneous abdominal adipose tissue: effect of exercise. J Physiol (Lond) 543:1033–1046
Maggiorini M, Swenson E, Mairbaurl H, Joller-Jemelka H, Gibbs S, Bärtsch P (2000) Plasma interleukin-6 a marker of injury to the blood-gas barrier in high altitude pulmonary edema. Abstract 117 at the IV World Congress on Mountain Medicine and High Altitude Physiology, Arica, Chile
Mazzeo RS, Bender PR, Brooks GA, Butterfield GE, Groves BM, Sutton JR, Wolfel EE, Reeves JT (1991) Arterial catecholamine responses during exercise with acute and chronic high-altitude exposure. Am J Physiol 261:E419–E424
Mazzeo RS, Brooks GA, Butterfield GE, Podolin DA, Wolfel EE, Reeves JT (1995) Acclimatization to high altitude increases muscle sympathetic activity both at rest and during exercise. Am J Physiol 269:R201–R207
Mazzeo RS, Child A, Butterfield GE, Mawson JT, Zamundio S, Moore LG (1998) Catecholamine response during 12 days of high-altitude exposure (4,300 m) in women. J Appl Physiol 84:1151–1115
Mazzeo RS, Child A, Butterfield GE, Braun B, Rock PB, Wolfel EE, Zamudio S, Moore LG (2000a) Sympathoadrenal responses to submaximal exercise in women after acclimatization to 4,300 Meters. Metabolism 49:1036–1042
Mazzeo RS, Donovan D, Fleshner M, Butterfield GE, Zamudio S, Wolfel EE, Moore LG (2000b) Interleukin-6 response to exercise and high-altitude exposure: influence of α-adrenergic blockade. J Appl Physiol 91:2143–2149
Mohamed-Ali V, Goodrick S, Rawesh A, Katz DR, Miles JM, Yudkin JS, Klein S, Coppack SW (1997) Subcutaneous adipose tissue releases interleukin-6, but not tumor necrosis factor-alpha, in vivo. J Clin Endocrinol Metab 82:4196–4200
Nielsen HB, Secher N, Perdersen BK (1996) Lymphocytes and NK cell activity during repeated bouts of maximal exercise. Am J Physiol 271:R222–R227
Nybo L, Nielsen B, Pedersen BK, Møller K, Secher NH (2002) Interleukin-6 release from human brain during exercise. J Physiol (Lond) 542:991–995
Ostrowsky K, Schjerling P, Pedersen BK (2000) Physical activity and plasma interleukin-6 in humans-effect of intensity of exercise. Eur J Appl Phys 83:512–515
Papanicolaou DA, Petrides JS, Tsigos C, Bina S, Kalogeras KT, Wilder R (1996) Exercise stimulates interleukin-6 secretion: inhibition by glucocorticoids and correlation with catecholamines. Am J Physiol 271(3 Pt 1):E601–E605
Pavlicek V, Marti HH, Grad S, Gibbs JSR, Kol C, Wenger RH, Gassmann M, Kohl J, Maly FE, Oelz O, Koller EA, Schirlo C (2000) Effects of hypobaric hypoxia on vascular endothelial growth factor and the acute phase response in subjects who are susceptible to high-altitude pulmonary oedema. Eur J Appl Physiol 81:497–503
Pedersen BK, Steensberg A, Schjerling P (2001) Muscle-derived interleukin-6: possible biological effects. J Physiol (Lond) 536:329–339
Savourey G, Launay JC, Besnard Y, Guinet A, Travers S (2003) Normo- and hypobaric hypoxia: are there any physiological differences ? Eur J Appl Physiol 89:122–126
Starkie RL, Rolland J, Angus DJ, Aanderson MJ, Febbraio MA (2001a) Circulating monocytes are not the source of elevations in plasma IL-6 and TNF-alpha levels after prolonged running. Am J Physiol 280:C769–C774
Starkie RL, Arkinstall MJ, Koukoulas I, Hawley JA, Febbraio MA (2001b) Carbohydrate ingestion attenuates the increase in plasma interleukin 6, but not skeletal muscle interleukin 6 mRNA, during exercise in humans. J Physiol (Lond) 533(Pt 2):585–591
Steensberg A, van Hall G, Osada T, Sacchetti M, Saltin B, Pedersen BK (2000) Production of interleukin-6 in contracting human skeletal muscles can account for the exercise-induced increase in plasma interleukin-6. J Physiol (Lond) 529.1:237–242
Steensberg A, Toft AD, Scherling P, Halkjaer-Kristensen J, Pedersen BK (2001a) Plasma interleukin-6 during strenuous exercise: role of epinephrine. Am J Physiol 281:C1001–C1004
Steensberg A, Febbraio MA, Osada T, van Hall G, Schjerling P, Saltin B, Pedersen BK (2001b) Interleukin-6 production in contracting human skeletal muscle is influenced by pre-exercise muscle glycogen content. J Physiol (Lond) 537.2:633–639
van Gool J, van Vugt H, Helle M, Aarden LA (1990) The relation among stress, adrenalin, interleukin 6 and acute phase proteins in the rat. Clin Immunol Immunopathol 57:200–210
Acknowledgements
Lab technician Ruth Rousing performed the IL-6 analysis, and her technical skills are greatly appreciated. Furthermore, the Dutch Hospital in El Alto is thanked for its hospitality. This paper is based on a series of experiments conducted during the Danish research expedition to Bolivia 2001. This study was supported by grants aided by the Danish National Research Foundation 504–14.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lundby, C., Steensberg, A. Interleukin-6 response to exercise during acute and chronic hypoxia. Eur J Appl Physiol 91, 88–93 (2004). https://doi.org/10.1007/s00421-003-0935-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-003-0935-y