Abstract
Objective
The aim of this study was to determine whether long-standing racial disparities in lead exposure still exists for children age 1–5 years old. We examined if blood lead levels were higher among non-Hispanic Black children and others compared to non-Hispanic White children.
Methods
Data from the National Health and Nutrition Examination Survey (NHANES) from 1999-2016 were used. Geometric mean blood lead levels (BLLs) were compared by race/ethnicity using log-transformed simple linear regression. Associations between race and elevated BLL were assessed using weighted Chi-square tests. Log-transformed multiple weighted linear regression was used to assess what factors affected BLLs.
Results
A total of 6772 children were included in this study. In 1999–2000, the geometric mean BLL for non-Hispanic Black children was 3.08 μg/dL, compared to 2.03 μg/dL for non-Hispanic White children (p = 0.01). The difference in geometric mean BLL between non-Hispanic Black children and non-Hispanic White children continued to be statistically significant in later years (all p < 0.05) until 2015-2016 (0.89 μg/dL vs 0.74 μg/dL, p = 0.17). Log-transformed linear regression showed that being non-Hispanic Black and having low family income were independently associated with higher BLL.
Conclusion
Although lead exposure in the general population continued to decline for all racial/ethnic groups, non-Hispanic Black children still had higher BLL than non-Hispanic White children. In more recent years, the racial/ethnic gap was lesser but persisted. Racial/ethnic disparity in childhood BLL could be partially explained by socio-economic factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lead is a toxic heavy metal that has affected individuals in various parts of the world (World Health Organization 2010). Historically, lead exposure has come from several sources including manufacturing, lead-based paint, leaded gasoline, and leaded pipes used for drinking water (Latha Chandran 2010). Compared with adults, children are disproportionately affected by exposure to lead because of their physiology, thumb-sucking and hand-to-mouth behaviors (ATSDR 2017). In children, lead-based paint and contaminated dust and/or soil in and around the home are the main sources of exposure. There has been a steady decline in lead exposure in the United States, yet there are still many children with elevated blood lead levels (BLLs). According to the Centers for Disease Control and Prevention (CDC), the definition for elevated BLL is a single blood lead test at or above the CDC blood lead reference value of 5 μg/dL established in 2012 (CDC 2019f). Until 2012, a blood lead “level of concern” was a child having 10 μg/dL or more of lead in blood (CDC 2019c). Based on survey data, there was a decrease from 77.8% in 1976–1980 to 4.4% in 1991–1994 in the overall prevalence of elevated BLLs among children aged 1–5 years in the United States population (CDC 2005). During the period 1999–2002, the CDC reported the overall prevalence of elevated BLLs for the U.S. population was 0.7% (CDC 2005) which could translate to about 2 million people. The CDC reported an estimated 70,680 children aged 1–4 years with blood lead levels 5–9 μg/dL which was above the elevated blood level of 5 μg/dL (Raymond and Brown 2017). Various health effects of lead exposure are known to occur in children even at low-lead levels. These adverse effects include decreased IQ levels and declines in cognitive abilities (Brown and Margolis 2012; Miranda et al. 2007). Deficits in cognitive and academic skills are associated with blood lead even lower than 5 μg/dL (Lanphear et al. 2000). Lead exposure at low levels has been hypothesized to be a cause of ADHD (Nigg et al. 2008). According to the CDC, no safe BLL in children has been identified (CDC 2019e).
It has been consistently documented in the scientific literature that Black children have higher lead exposure than White children (Lanphear et al. 1996; Scott and Nguyen 2011). In a study that analyzed National Health and Nutritional Examination Survey (NHANES) III and NHANES 1999–2004 data, non-Hispanic Black race/ethnicity was associated with higher blood lead levels (Scott and Nguyen 2011). A study that included 205 children, aged 12–31 months, discovered that Black children had higher lead exposure than White children (Lanphear et al. 1996). In another study in the US, childhood lead poisoning was disproportionately found in those who were African–Americans, had Medicaid, and lived in lower socio-economic neighborhoods or urban areas (Latha Chandran 2010). Low-income individuals are more likely to experience lead exposure and to be at risk of several exposure sources (CDC 2019b). These individuals are more likely to live near polluted areas and to live in aging substandard housing with deteriorating lead-based paint. Furthermore, low-income individuals are more likely to live where there is heavy traffic or near lead-related industries, or to work there (Tong et al. 2000).
For the past several decades, BLLs have declined dramatically due to effective laws and regulations aimed at lowering lead exposure (Dignam et al. 2019). The decrease in BLLs for the general population has resulted in a commensurate decrease in BLLs in every racial/ethnic group, and a narrower racial gap in these levels. Based on NHANES II 1976–1980 data, the mean BLL in Black children measured 20.2 μg/dL, which was 6.5 μg/dL higher than that of White children (Pirkle et al. 1994). In the years 1988–1991, based on NHANES III data, the mean BLL in Black children dropped to 5.6 μg/dL, only 2.4 μg/dL higher than that of White children (Pirkle et al. 1994). In 1999–2002, non-Hispanic Black children had higher percentages of elevated BLLs (1.4%) compared to non-Hispanic Whites (0.5%) (Jain 2016). To the best of our knowledge, no published study has examined most recent NHANES data to investigate the current state of racial/ethnic disparity in lead exposure. Despite the continuing decline in BLL in children of all races, we hypothesize that non-Hispanic Black children continue to have higher blood lead levels compared to non-Hispanic White children, due to the persistent socio-economic disparities.
In this study, using data from NHANES 1999–2016, we aim to evaluate whether racial disparities in lead exposure persist despite generally low-lead exposure among children aged 1–5 years. Similar to previous studies, our study looked at the age group 1–5 years, because lead is more likely to cause harm to children in that age group due to their routine hand-to-mouth behavior (CDC 2019d; Roberts et al. 2017). In NHANES, blood was only collected from sample participants aged 1 and above (CDC 2013). Using the most recent years of NHANES data, we will also investigate how socio-economic factors are associated with persistent racial/ethnic disparities in lead exposure, using the poverty–income ratio variable contained in NHANES.
Methods
Data source
The National Center for Health Statistics (NCHS) of the CDC conducts NHANES on nationally represented noninstitutionalized Americans including children and adults to evaluate the health and nutrition of the nation (CDC 2019a). NHANES conducts both interviews and physical examinations on participants to collect detailed health and nutrition information (CDC 2019a). NHANES is cross-sectional survey and has been continuously conducted since 1999; the current study included NHANES 1999 to 2016. The NHANES data are published in a 2-year cycle to increase the sample size of a single cycle, and our data contained nine data cycles: 1999–2000, 2001–2002, and so on up to 2015–2016. NHANES contains blood lead measurements collected from physical examinations in which whole blood is collected. Rigorous procedure is followed to make sure that the blood specimen is collected, stored and analyzed in a reliable manner to ensure data accuracy. This study was limited to persons aged 1–5 years. Excluded from the study were participants with no BLL measurements and participants whose demographic variables of interest such as gender, age, race/ethnicity or income level were missing.
Variables
To measure elevated blood lead levels, we categorized elevated as ≥ 10 μg/dL before 2012, and ≥ 5 μg/dL after 2012, as the CDC lowered its cutoff value for elevated BLL from 10 to 5 μg/dL in 2012 (CDC 2019f). Race/ethnicity was characterized as Hispanic, non-Hispanic Black, non-Hispanic White and Other. Participants with a described race/ethnicity of Mexican–American and Other Hispanic were merged into one group called Hispanic. Poverty index was measured using poverty-to-income ratio (PIR), which was the ratio of family income to federal poverty level. Following the categorization by Scott and Nguyen (2011), participants with PIR less than 1.25 was defined as having poor income; participants with PIR 1.26–1.99 were defined as having low income; participants with PIR 2.00–3.99 were defined as having middle income; participants with PIR 4.00 and higher were defined as having high income. The variable country of birth was categorized into (1) born in 50 U.S. states or Washington, DC; (2) born in other countries, including U.S territories. NHANES does not contain information for a child’s parent, but the household reference person, who is the adult household member owning or renting the residence. We used the household reference person’s educational level as a proxy for parent/guardian’s educational level (CDC 2020).
Statistical analysis
All statistical analyses have applied sampling weights to account for the complex survey design of NHANES, a multistage probability sampling design which oversamples minorities. Since both geometric mean BLL and arithmetic mean BLL have been used in the literature to measure blood exposure (Scott and Nguyen 2011; Pirkle et al. 1994), racial/ethnic differences in geometric mean BLL were presented, as well as the arithmetic mean. Box-and-whisker plots were drawn to visually present the minimum, maximum, medium, 1st quartile (i.e., 25th percentile) and 3rd quartile (75th percentile) of BLL. Chi-square test was conducted to explore the associations between race/ethnicity and BLL elevation status. In addition, log-linear regression model was used to test if there existed racial/ethnic disparity in lead exposure, with log-transformed BLL as the dependent variable. Log-transformation was used because the test for normality showed that BLL was not normally distributed. Confounders in the model included PIR, education level, where or not born in the U.S., as defined above, as well as age and gender. Statistical analyses for this study were conducted using SAS 9.4.
Results
This study included 6772 participants aged 1–5 years. After applying the sampling weights, this sample consisted of 53.45% non-Hispanic Whites, 14.54% non-Hispanic Blacks, 24.61% Hispanics and 7.39% others. As seen in Table 1, in 1999–2016, non-Hispanic Black children had the highest geometric mean BLL at 1.75 μg/dL, compared to 1.23 μg/dL for non-Hispanic White children, and 1.20 μg/dL for Hispanic children. Non-Hispanic Black children had higher BLL, with higher percentages in subcategories of higher BLLs. For instance, for BLL between 2.5 μg/dL and 5 μg/dL, 21.28% of non-Hispanic Black children were in that subcategory, compared with only 11.71% of non-Hispanic White children, or 11.94% of Hispanic children and 12.00% of Other children. For BLL as high as at least 40 μg/dL, all corresponding participants were non-Hispanic Black children. Two separate periods were analyzed in regards to BLL elevation status because the standard changed after the year 2012. In 1999–2012, 2.05% of non-Hispanic Black children had an elevated BLL while only 0.86% of non-Hispanic White children had elevated BLL. In 2013–2016, 1.20% of non-Hispanic Black children had an elevated BLL, still higher than the 0.80% for non-Hispanic White children.
Childhood lead exposure is a more pronounced problem in younger children. We further explored the racial disparity in lead exposure for different age groups: age 1, age 2, and ages 3–5. Figure 1 presents the box plots by racial/ethnic group within a given age group; the dot denotes the arithmetic mean, the center line being the median, and the upper and lower line of the box representing the third and first quartile, respectively. As shown in panel A of Fig. 1, for all ages combined, non-Hispanic Black children had much larger maximum, visibly higher third quartile in the box plot, and higher mean as compared to other racial/ethnic groups. Panel B shows data for 1-year-old participants, among whom non-Hispanic Black children had much larger maximum, larger third quartile, and mean as compared to other racial/ethnic groups. A similar pattern was found for children aged 2 years (Fig. 1c). For children 3–5 years old (Fig. 1d), though their BLLs were generally lower than those for age 1 for all racial/ethnic groups, the racial disparity still persisted with non-Hispanic Blacks having higher BLL as compared to other racial/ethnic groups.
To explore the time trend of declining BLL, we calculated geometric mean BLLs by year and by race/ethnicity as shown in Table 2. We found that lead exposure continued to decrease over this time period for every race/ethnicity category. From 1999 to 2016, the geometric mean BLL decreased from 2.10 to 0.74 μg/dL in non-Hispanic White children, from 3.08 to 0.89 μg/dL in non-Hispanic Black children, from 2.03 to 0.67 μg/dL in Hispanic children and from 1.86 to 0.81 μg/dL in Other children. Non-Hispanic Black children had statistically significantly higher geometric mean BLL in all years except for the last data cycle, 2015–2016, compared to non-Hispanic White children. With the continued decline of BLL, the racial/ethnic difference in BLLs had been reduced regarding geometric mean BLLs. In 2015–2016, the difference in geometric mean BLL between non-Hispanic Black children and non-Hispanic White children was no longer statistically significant (0.89 μg/dL vs. 0.74 μg/dL, p = 0.17). Throughout the years, no statistical difference existed between non-Hispanic White children and Hispanic children or Other children.
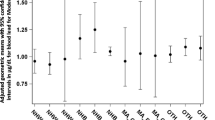
Table 3 presents results from linear regression models with natural log-transformed BLL as the dependent variable. The test for normality showed that the blood lead level was not normality distributed (p < 0.01). The unadjusted analysis was from simple linear regression models with only one variable of interest being included, whereas the adjusted analysis included all covariates simultaneously. As shown in the unadjusted analysis, non-Hispanic Black children had significantly higher BLL (p < 0.0001), however, there was no statistical significance for Hispanic children (p = 0.49) and Other children (p = 0.37) compared to non-Hispanic White children. In the unadjusted analysis, higher income and higher education level were associated with lower BLLs.
In the adjusted analysis, after controlling for other covariates, income and education level remain significant factors. After controlling for other covariates, non-Hispanic Black children still had statistically significantly higher BLL (p < 0.0001) as compared to non-Hispanic Whites. Interestingly, Hispanic children who previously did not differ from non-Hispanic White children in BLL in unadjusted analyses, had statistically significantly lower exposure in adjusted analysis (p = 0.002).
Discussion
This study showed persistent racial disparity between non-Hispanic Blacks and non-Hispanic Whites in childhood lead exposure, despite the continuing decline of BLL for each racial/ethnic group. Although both non-Hispanic Black children and non-Hispanic White children are exposed to lead, non-Hispanic Black children are more likely to have higher blood lead levels. The finding in this study is consistent with other studies that have established the racial disparity in blood lead levels (Joseph et al. 2005; Lanphear et al. 1996; Ngueta 2014; Pugh Smith and Nriagu 2011; Smith et al. 2010). In particular, our study showed that the racial disparity still existed amid current low BLLs for non-Hispanic Black children compared to non-Hispanic White children. We hope, however, the gap will close completely soon, as the racial difference in the mean BLL was not statistically significant in the most recent data cycle 2015–2016. To the best of our knowledge, this study signifies the first study to use the most recent NHANES data to comprehensively explore persistent racial disparity in lead exposure in young children despite overall low-lead exposure. The NHANES data are the largest continuous national survey that contains blood lead levels for children to accurately study racial disparity in lead exposure.
As noted in the results, non-Hispanic Black children tended to have higher outlier BLLs, especially for younger children. A total of 0.05% of non-Hispanic Black children had BLL of at least 40 μg/dL, whereas no child from any other racial/ethnical group had such high BLL. Those outlier numbers, though a very small percentage, could mean that as many as thousands of non-Hispanic Black children in the U.S. have such high BLLs. The Flint, Michigan water crisis example could be the tip of the iceberg reflecting the existence of a large number of non-Hispanic Black children with extremely high BLLs (Kennedy et al. 2016).
According to Table 3, participants born outside of the United States were more likely to be exposed to lead. This could be because the United States has developed initiatives to eliminate the risk of lead poisoning in American children (Apostolou et al. 2012). Analysis for the education level showed that children living with individuals who did not have a college education or higher had more lead exposure. The reason for this could be because more education leads to greater awareness of lead exposure and environmental issues. In addition, individuals who are educated may be able to afford resources that would prevent lead exposure, such as newer homes without lead paint. A study using NHANES 2007–2010 data observed that those with better education had less lead exposure (Obeng-Gyasi 2018).
Although there has been great attention focused on health disparities, it is still difficult to fully identify the factors that create and maintain disparities in health status and health care (Brondolo and Gallo 2009). Income level could be a possible factor that creates disparities. Research suggests that low-income individuals are more likely to live in communities with higher amounts of air pollution and in areas with polluting industries and waste sites subsequently exposing them to increased levels of pollutants (Vrijheid et al. 2012). In our study, as the income level increased, the BLL decreased.
In both unadjusted and adjusted analysis, income and education level were significant factors. In the unadjusted analysis without considering other covariates, Hispanic children had no significantly different BLLs compared to non-Hispanic White children; however, in the adjusted analysis when income, education level and other factors were controlled for, Hispanic children had significantly lower BLLs than non-Hispanic Whites. This observed change in statistical significance from unadjusted analysis to adjusted analysis highlights the role that income and educational level play in affecting lead exposure.
To further explore the effects of income and educational level, subgroup analyses were conducted by income level and educational level separately. In the subgroup analysis by income, non-Hispanic Black children continued to have higher BLLs than non-Hispanic White children in every subgroup with the same level of income. In the subgroup analysis by education level, in each subgroup with the same educational level, non-Hispanic Black children continued to have higher BLLs than non-Hispanic White children. Even in subgroup that had both the highest income and the highest educational level, non-Hispanic Black children had statistically significantly higher BLLs compared to non-Hispanic White children. These subgroup sensitivity analyses suggested that the racial/ethnic disparity in lead exposure also came from other factors in addition to the significant socio-economic factors. Future studies should investigate what additional factors should be addressed to reduce lead exposure for non-Hispanic Black children. Examples of some other factors may include infants’ lead exposure from pregnant mothers and lead-contaminated floor dust, soil and water (Cassidy-Bushrow et al. 2017; Lanphear et al. 2002).
Several limitations exist in this study. First, we were not able to measure sources of lead absorption, such as house paint exposures, behavioral exposures and dietary intake. Second, from the time of exposure to the time the blood lead was taken for assessment, blood lead may have been cleared from the blood, due to a short half-life of 1–2 months (Gambelunghe et al. 2016). The measured lead level may be lower than it originally was. Third, blood lead level value did not exist for a considerable percentage of children who were excluded from the study, which may cause some sample selection bias in the study. Another potential source of sample selection bias might be from the language barriers that immigrant families face, which may make them less likely to participate in the NHANES survey. Lastly, housing characteristics analysis was not performed because this information was not available for some of the data cycles studied. Despite those limitations, one of the strengths of this study is that NHANES is a large national survey that sampled the general population which can make the findings generalizable. Another strength is that a thorough analysis using multi-years of NHANES data including the most recent data allowed the study to observe the time trends of racial/ethnic disparities in blood lead levels.
The findings from this study can inform lead-related health policies. Local counties with higher minorities and low-income individuals should have policies for identifying higher risk properties and detailing safeguards such as environmental testing requirements and protective interventions such as abatement. Additional environmental interventions would include targeted cleaning, repairs, maintenance, soil removal and replacement, and short-term containment of lead hazards (Yeoh et al. 2014). Educational interventions would address parental awareness of lead exposure pathways, such as washing of hands and dust control measures to prevent absorption of dust and soil (Yeoh et al. 2014). It is also important to establish culturally competent interventions that would address challenges that minorities face. For example, a study observed that non-Hispanic Black children were more likely to put their mouths on window sills (Lanphear et al. 1996). Our study highlights the importance of continued efforts to develop interventions that aim to reduce childhood lead exposure, especially in racial/ethnic minority groups.
References
Apostolou A, Garcia-Esquinas E, Fadrowski JJ, McLain P, Weaver VM, Navas-Acien A (2012) Secondhand tobacco smoke: a source of lead exposure in US children and adolescents. Am J Public Health 102(4):714–722. https://doi.org/10.2105/AJPH.2011.300161
ATSDR (2017) Lead (Pb) toxicity: who is at risk of lead exposure? ATSDR—environmental medicine & environmental health education—CSEM
Brondolo E, Gallo LC (2009) Race, racism and health: disparities, mechanisms, and interventions. J Behav Med. https://doi.org/10.1007/s10865-008-9190-3
Brown MJ, Margolis S (2012) Lead in drinking water and human blood lead levels in the United States. MMWR Suppl 61(4):1–9
Cassidy-Bushrow AE, Sitarik AR, Havstad S, Park SK, Bielak LF, Austin C, Arora M (2017) Burden of higher lead exposure in African–Americans starts in utero and persists into childhood. Environ Int 108:221–227. https://doi.org/10.1016/j.envint.2017.08.021
Centers for Disease Control and Prevention (2005) Blood lead levels–United States, 1999–2002. MMWR Morb Mortal Wkly Rep 54(20):513–516
Centers for Disease Control and Prevention (2013) National Health and Nutrition Examination survey: plan and operations, 1999–2010. Monitoring the Nation’s Health. https://www.cdc.gov/nchs/data/series/sr_01/sr01_056.pdf. Accessed 12 Dec 2019
Centers for Disease Control and Prevention (2019a) National Health and Nutrition Examination Survey. https://wwwn.cdc.gov/nchs/nhanes/Default.aspx. Accessed 12 Dec 2019
Centers for Disease Control and Prevention (2019b) At-risk populations, CDC's lead poisoning prevention. https://www.cdc.gov/nceh/lead/prevention/populations.htm. Accessed 12 Dec 2019
Centers for Disease Control and Prevention (2019c) CDC—Lead-blood lead levels in children. https://www.cdc.gov/nceh/lead/prevention/blood-lead-levels.htm. Accessed 12 Dec 2019
Centers for Disease Control and Prevention (2019d) CDC—Lead-CDC's Childhood Lead Poisoning Prevention Program. https://www.cdc.gov/nceh/lead/about/program.htm. Accessed 12 Dec 2019
Centers for Disease Control and Prevention (2019e) CDC—lead-home page. https://www.cdc.gov/nceh/lead/. Accessed 12 Dec 2019
Centers for Disease Control and Prevention (2019f) CDC—National Childhood Blood Lead Surveillance Data. https://www.cdc.gov/nceh/lead/data/national.htm. Accessed 12 Dec 2019
Centers for Disease Control and Prevention (2020) National Health and Nutrition Examination Survey 2011–2012: data documentation, codebook, and frequencies. https://wwwn.cdc.gov/Nchs/Nhanes/2011-2012/DEMO_G.htm#DMDHREDU. Accessed 30 Nov 2020
Dignam T, Kaufmann RB, LeStourgeon L, Brown MJ (2019) Control of lead sources in the United States, 1970–2017: public health progress and current challenges to eliminating lead exposure. J Public Health Manag Pract 25(Suppl 1 lead poisoning prevention):S13-22. https://doi.org/10.1097/phh.0000000000000889
Gambelunghe A, Sallsten G, Borne Y, Forsgard N, Hedblad B, Nilsson P, Barregard L (2016) Low-level exposure to lead, blood pressure, and hypertension in a population-based cohort. Environ Res 149:157–163. https://doi.org/10.1016/j.envres.2016.05.015
Jain RB (2016) Trends and variability in blood lead concentrations among US children and adolescents. Environ Sci Pollut Res Int 23(8):7880–7889. https://doi.org/10.1007/s11356-016-6039-0
Joseph CL, Havstad S, Ownby DR, Peterson EL, Maliarik M, McCabe MJ Jr, Johnson CC (2005) Blood lead level and risk of asthma. Environ Health Perspect 113(7):900–904. https://doi.org/10.1289/ehp.7453
Kennedy C, Yard E, Dignam T, Buchanan S, Condon S, Brown MJ, Breysse P (2016) Blood lead levels among children aged < 6 years—Flint, Michigan, 2013–2016. MMWR Morb Mortal Wkly Rep 65(25):650–654. https://doi.org/10.15585/mmwr.mm6525e1
Lanphear B, Weitzman M, Eberly S (1996) Racial differences in urban children’s environmental exposures to lead. Am J Public Health 86(10):1460–1463
Lanphear BP, Dietrich K, Auinger P, Cox C (2000) Cognitive deficits associated with blood lead concentrations < 10 microg/dL in US children and adolescents. Public Health Rep 115(6):521–529
Lanphear BP, Hornung R, Ho M, Howard CR, Eberly S, Knauf K (2002) Environmental lead exposure during early childhood. J Pediatr 140(1):40–47. https://doi.org/10.1067/mpd.2002.120513
Latha Chandran TC (2010) Lead poisoning: basic and new developments. Pediatr Rev 31(10):399–407
Miranda ML, Kim D, Galeano MAO, Paul CJ, Hull AP, Morgan SP (2007) The relationship between early childhood blood lead levels and performance on end-of-grade tests. Environ Health Perspect 115(8):1242–1247. https://doi.org/10.1289/ehp.9994
Ngueta G (2014) Racial disparities in children’s blood lead levels: possible implication of divalent metal transporter 1. Med Hypotheses 82(1):71–73. https://doi.org/10.1016/j.mehy.2013.11.008
Nigg JT, Knottnerus GM, Martel MM, Nikolas M, Cavanagh K, Karmaus W, Rappley MD (2008) Low blood lead levels associated with clinically diagnosed attention-deficit/hyperactivity disorder and mediated by weak cognitive control. Biol Psychiatry 63(3):325–331. https://doi.org/10.1016/j.biopsych.2007.07.013
Obeng-Gyasi E (2018) Lead exposure and oxidative stress—a life course approach in US adults. Toxics 6(3):42. https://doi.org/10.3390/toxics6030042
Pirkle JL, Brody DJ, Gunter EW, Kramer RA, Paschal DC, Flegal KM, Matte TD (1994) The decline in blood lead levels in the United States: the National Health and Nutrition Examination Surveys (NHANES). JAMA 272(4):284–291. https://doi.org/10.1001/jama.1994.03520040046039
Pugh Smith P, Nriagu JO (2011) Lead poisoning and asthma among low-income and African American children in Saginaw, Michigan. Environ Res 111(1):81–86. https://doi.org/10.1016/j.envres.2010.11.007
Raymond J, Brown MJ (2017) Childhood blood lead levels in children aged. Morb Mortal Wkly Rep
Roberts EM, Madrigal D, Valle J, King G, Kite L (2017) Assessing child lead poisoning case ascertainment in the US, 1999–2010. Pediatrics 139(5):e20164266. https://doi.org/10.1542/peds.2016-4266
Scott LL, Nguyen LM (2011) Geographic region of residence and blood lead levels in US children: results of the National Health and Nutrition Examination Survey. Int Arch Occup Environ Health. https://doi.org/10.1007/s00420-011-0624-9
Smith M, Grant L, Sors AI (2012) Lead exposure and child development: an international assessment. Kluwer Academic Publishers, Lancaster
Tong S, von Schirnding YE, Prapamontol T (2000) Environmental lead exposure: a public health problem of global dimensions. Bull World Health Organ 78(9):1068–1077
Vrijheid M, Martinez D, Aguilera I, Ballester F, Basterrechea M, Esplugues A, Sunyer J (2012) Socioeconomic status and exposure to multiple environmental pollutants during pregnancy: evidence for environmental inequity? Environ Health. https://doi.org/10.1136/jech.2010.117408
World Health Organization (2010) Childhood lead poisoning. Publication of the World Health Organization, pp 11–69
Yeoh B, Woolfenden S, Lanphear B, Ridley GF, Livingstone N, Jorgensen E (2014) Household interventions for preventing domestic lead exposure in children. Cochrane Database Syst Rev 12:Cd006047. https://doi.org/10.1002/14651858.CD006047.pub4
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Teye, S.O., Yanosky, J.D., Cuffee, Y. et al. Exploring persistent racial/ethnic disparities in lead exposure among American children aged 1–5 years: results from NHANES 1999–2016. Int Arch Occup Environ Health 94, 723–730 (2021). https://doi.org/10.1007/s00420-020-01616-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-020-01616-4