Abstract
Purpose
This study investigated the association between geographic region and blood lead levels (BLLs) in US children, as well as trends in this relationship, using data from the National Health and Nutrition Examination Survey (NHANES).
Methods
SAS® and SUDAAN® software programs were utilized to develop linear regression models adjusted for several factors associated with BLLs.
Results
The largest decline in BLLs was observed in Northeastern children, while the percentage of children with elevated blood lead levels decreased the most for the West and Northeast. Lead levels of Northeastern children were still higher than those of children living in the West. However, levels were not different among children residing in the Northeast, Midwest, and South, and the blood lead concentrations were less than 5 μg/dL for all but one subgroup of children and less than 2 μg/dL for >70% of the subgroups. More importantly, the effects of different risk factors for higher blood lead levels varied by region even after adjusting for all other covariates.
Conclusions
The results of this study not only provide relevant and current blood lead levels for US children that can be used as reference values to evaluate biomonitoring data, but can also be used to help direct prevention and surveillance strategies to reduce lead in the environment of at-risk children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For more than a 100 years, the malleable and ductile nature of lead has resulted in the extensive inclusion of this metal and its alloys in numerous products, including building construction materials, casting products, noise control materials, ammunition, electronics, jewelry, and pigments used in glass making, ceramic glazes, and paints, thereby creating abundant exposure sources (ATSDR 2007). With the relatively recent efforts in the United States to remove lead from gasoline, paint, plumbing materials, and caulking and solder products (ATSDR 2007), however, exposure of children has declined substantially over the last 20 years as evidenced by the dramatic decrease in the percentage of 1- to 5-year-olds with blood lead levels (BLLs) ≥10 μg/dL (Anderson 1995; CDC 1994, 1997a, 2000, 2005a; Kaufmann et al. 2000; Meyer et al. 2003; Pirkle et al. 1994). Yet, even with these considerable reductions in exposure, other studies have shown that BLLs tend to be higher for minority children, children from low-income families, and children living in older housing (Bernard and McGeehin 2003; Brody et al. 1994; CDC 1997a, 2005a; Meyer et al. 2003; Pirkle et al. 1994, 1998).
Although latex paints began to replace lead-based paints in the US market as early as the 1950s (CEH/CAPP 1987; Sargent et al. 1999), older homes, which are primarily found in the Northeast and Midwest regions of the United States (Diamond 2001), may still present lead hazards to children. In the present study, we evaluated the relationship between geographic region and blood lead levels in children ages 1 to 5 years using data from the National Health and Nutrition Examination Survey (NHANES). Additionally, we assessed the effect of various risk factors on blood lead levels for each region, as well as trends in blood lead levels by geographic region over time.
Materials and methods
NHANES is a series of cross-sectional surveys conducted by the National Center for Health Statistics (NCHS) and the Centers for Disease Control and Prevention (CDC) to assess the health and nutritional status of civilian, non-institutionalized adults and children in the United States. Each survey is based on a complex, multistage probability design that is used to select a nationally representative sample. The NHANES program combines both interviews and physical examinations at a mobile examination center (MEC) creating a comprehensive set of analytical data (NCHS 2005).
To date, there are blood lead and geographic residence data available for NHANES III (1988–1994) and the three subsequent continuous cycles: NHANES 1999–2000, NHANES 2001–2002, and NHANES 2003–2004 (NCHS 2005). During the physical examination, whole blood samples were collected from participants one year and older via venipuncture. Blood lead was measured by graphite furnace atomic absorption spectrophotometry (GFAAS) at the CDC’s Environmental Health Laboratory (CDC 2005b). Region information was collected during the interview and categorized using the Census Bureau definitions of “Northeast,” “Midwest,” “South,” and “West.”
Covariates
In these analyses, poverty index was evaluated using poverty-to-income ratio (PIR), a ratio of family income to poverty threshold. The sample populations were stratified as follows: poor was defined as PIR less than 1.24; low income as PIR 1.25–1.99; middle income as PIR 2.00–3.99; and high income as PIR greater than or equal to 4.00. Year of housing construction was based on the cycle of NHANES data used. For example, in NHANES III the year a home was built was reported as a three-level variable (built before 1946, 1946–1973, after 1973); however, age of housing was reported as a six-level variable (built before 1940, 1940–1949, 1950–1959, 1960–1977, 1978–1989, 1990 and later) in the continuous cycles. For consistency, in our analysis, we established a two-level categorical variable for both the NHANES III (built before 1946 and built in 1946 and later) and continuous cycles (built before 1950 and built in 1950 and later). Race/ethnicity was categorized as Hispanic, non-Hispanic black, and non-Hispanic white. Children with a reported race/ethnicity of “Other Hispanic” and Mexican–American were combined into one group (Hispanic) to provide reliable BLL estimates when stratified by region. Country of birth was categorized as born in the United States, born in Mexico, and born in other countries. Age was stratified into three categories: 1–2, 3–4, and 5 years.
We evaluated multiple housing characteristics, individually and as composite variables, to determine how these may affect blood lead levels in children. Housing traits such as type of home, number of rooms in the home, whether the home was owned or rented, whether the home was painted in the last year, and whether any paint in the home was peeling, flaking, or chipping, had very little impact on predicted log blood lead levels. In contrast, an excellent indicator of potential exposure to lead was home cleanliness, as determined using an interviewer-reported evaluation of the cleanliness of the room in which dust samples were taken. This variable was defined as dirtier than average, average, and cleaner than average. Further information describing interviewer training and dust collection and analytical methods may be found at the following websites: http://www.cdc.gov/nchs/data/nhanes/int2.pdf, http://www.cdc.gov/nchs/nhanes/nhanes2003-2004/L20_C.htm#Component_Description, http://www.cdc.gov/nchs/data/nhanes/nhanes_0304/l20_c_met_lead_dust.pdf.
Statistical analysis
All statistical analyses were completed using SAS 9.2 (SAS Institute, Cary, NC) and SUDAAN 9.0 (Research Triangle Institute, Research Triangle Park, NC) and utilized an alpha level of 0.05. The three continuous NHANES cycles (1999–2000, 2001–2002, 2003–2004) were combined into a single data set for greater precision of estimates. To account for the complex, multistage sampling design, survey non-response, and post-stratification, the necessary sample weights were used in all analyses. Sample weights for NHANES III were utilized as provided in the data file. For the 1999–2004 data, six-year sample weights were calculated using the appropriate two-year and four-year weights included in the data files for these surveys. Use of the appropriate weights allows for the calculation of estimates that are representative of the US civilian, non-institutionalized population. More detailed information describing the NHANES sampling design and weighting scheme can be found at http://www.cdc.gov/nchs/tutorials/Nhanes/SurveyDesign/Weighting/OverviewKey.htm.
An elevated blood lead level was defined as BLL ≥10 μg/dL. Since only a very small percentage of children with measured blood levels in 1999–2004 had elevated concentrations (1.48%), we calculated the prevalence of elevated BLLs by region only because stratification by age, race/ethnicity, gender, poverty index, and year of home construction would result in very low within-strata counts (i.e., due to privacy concerns, analyses resulting in cells with <5 counts could not be conducted).
The association between geographic region and blood lead levels was evaluated using linear regression models. The natural log of lead levels was used as the dependent variable in all linear regressions. Linear models developed to compare the effect of region between survey periods (i.e., NHANES III vs. NHANES 1999–2004) included gender, age, year of home construction, poverty index, and race/ethnicity. For these models, we calculated the least-square geometric means (LSGM) and associated 95% confidence intervals.
Using the 1999–2004 data, we conducted a separate, more in-depth analysis that evaluated the impact of region on blood lead levels in both univariate and multivariate models. This analysis was limited to children aged 1 to 5 years with a measured blood lead level and reported region of residence. Only children with complete data on gender, race/ethnicity, age, year of home construction, poverty index, country of birth, home cleanliness, and floor and window dust measurements were included. Lead concentrations in both floor and window dust samples were included in the same model since these variables were not collinear. This analysis included a final population of 1,085 children.
Results
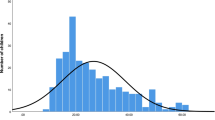
For children 1 to 5 years of age with a blood level measured during the 1999–2004 period, the geometric mean (GM) BLL was 1.9 μg/dL (95% confidence interval (CI): 1.8, 2.0 μg/dL). Children living in the Northeast, regardless of age group, and 1 to 2-year-old children living in the West had the greatest percent decline in blood lead levels during this time period while GM BLLs for children 1 to 2 years of age living in the Midwest decreased the least (data not shown). For both survey periods, geometric mean blood lead levels varied by geographic region with the Northeast and Midwest having the highest concentrations (Table 1).
To further evaluate the effect of region between survey periods, linear regression models were utilized to adjust log-transformed blood lead levels for selected characteristics available in both data sets. For the 1988–1994 period, least-square geometric mean blood lead levels of children living in the various regions ranged from ~2.5 to 3.9 μg/dL after adjusting for gender, race/ethnicity, age of child, year of housing construction, and poverty index (Table 1). Adjusted LSGM blood lead levels measured during the 1999–2004 period were <2 μg/dL for each region (Table 1), considerably lower than the previous period. Specifically, adjusted LSGM BLLs declined by ~50% for the Northeast, ~43% for the Midwest and West, and ~40% for the South from the 1988–1994 period to the 1999–2004 period.
The percentage of children with measured blood lead levels ≥10 μg/dL for the 1988–1994 period was 6.3% and 1.5% for the 1999–2004 period, a 76% decrease overall. By region, the percentage of children with elevated BLLs declined from 2.0 to 0.3% for the West (88% decrease), from 3.8 to 0.9% for the South (77% decrease), from 12.8 to 1.9% for the Northeast (85% decrease), and from 9.9 to 3.5% for the Midwest (65% decrease) (Table 2). Interestingly, among children with blood lead levels ≥10 μg/dL, the percentage of children living in each region noticeably changed between survey periods (Table 2). For example, of the 401 children with elevated blood lead levels in 1988–1994, 33% lived in the Northeast and 38% lived in the Midwest. However, for the 1999–2004 period, only 21% of the 53 children with BLLs ≥10 μg/dL lived in the Northeast whereas 52% of these children resided in the Midwest (Table 2), suggesting that factors affecting the prevalence of elevated blood lead levels in US children may be changing over time.
In separate analysis of the 1999–2004 data (Table 3), the study population included slightly more males and was predominantly non-Hispanic white. The majority of children lived in housing built in 1950 or later (76.9%) and had a poverty index less than four (78.4%). Only a small percentage of children were born outside of the United States (1.1%) whereas 27.8% of the children sampled lived in a home considered to be dirtier than average. Generally, children were exposed to 0.5 and 7.0 μg of lead in dust per square foot of flooring and window trimming, respectively.
Factors associated with higher log blood lead levels in the unadjusted regression models included living in the Northeast, Midwest, or South; non-Hispanic black race/ethnicity; living in a home built before 1950; a PIR < 4.0; being born outside the United States; living in an average or dirty home, and increasing concentrations of lead in floor and window dust samples. As expected, older age was associated with a decrease in log blood lead levels. In the multivariate model, these same characteristics were associated with Ln[BLL], not including a birth country of “Other.” Geometric mean blood lead levels of children living in the Northeast were approximately 30% higher (95% CI: 12, 51%) than children living in the West, while children in the Midwest and South had levels ~25 and 16% higher (95% CI: 6, 45%; 6, 27%), respectively, after adjusting for all other factors (Table 4). However, adjusted GM blood lead levels did not vary significantly between the Northeast and Midwest, the Northeast and South, or the Midwest and South. As noted previously, adjusted least-square geometric mean concentrations of lead for each region were all less than two micrograms per deciliter (Table 4). Models that included different levels of housing construction (before 1978 and 1978 and later; before 1950, 1950–1978, and 1978 and later) did not change these estimates (data not shown).
Table 5 presents least-square geometric mean estimates stratified by region. Although children residing in the Northeast and Midwest typically had higher BLLs than children living in the South and the West, blood lead levels in almost all subgroups of children were still less than 5 μg/dL—half the CDC’s action level for children. Southern children born in Mexico were the only children in which BLLs were greater than 5 μg/dL.
More importantly, the effect of various factors on blood lead levels differed considerably by region (Table 6). For example, the Northeast was the only region in which BLLs were significantly different between males and females, while the Midwest was the only region in which children’s blood lead levels varied significantly based on year of housing construction. Interestingly, blood lead levels of children living in the Northeast were dependent on lead concentrations in window and floor dust, yet did not vary significantly between children living in clean and average and clean and dirty homes. Just as notable was the lack of an association between race/ethnicity and blood lead levels for each region, except the South in which non-Hispanic black children had significantly higher levels than non-Hispanic whites.
Discussion
Based on these data, blood lead levels of children 1 to 5 years of age in the United States appear to be associated with geographic region of residence. Although children living in the Western states have significantly lower blood lead levels than those in other regions, no significant differences were observed among children living in the South, Midwest, and Northeast regions.
While these data are, overall, consistent with previous studies that have demonstrated the substantial decline in blood lead levels and in the percentage of children with elevated BLLs (Anderson 1995; Brody et al. 1994; CDC 1994, 1997a, 2000, 2005a; Kaufmann et al. 2000; Meyer et al. 2003; Pirkle et al. 1994, 1998), they also highlight unexpected trends and associations such as the considerably large decline in the percentage of children in the Northeast with elevated BLLs and the potential association between birth country and blood lead levels of children living in the Midwest, South, and West regions. While the latter result was statistically significant, the small numbers of children born outside the United States do not allow us to generalize these findings at this time and must be evaluated further.
As suggested by the decrease in BLLs with increasing age (i.e., decreasing hand-to-mouth activity) and the increased lead levels in children in the Northeast and Midwest relative to children in the West, some exposure to lead from lead-based paint in older homes still appears to be possible. Nonetheless, the results presented here also suggest that lead in children’s blood can be markedly affected by other exposure sources. Lead-based paint is considered one of the most common high-dose sources of lead (CDC 2007; CEH/CAPP 1987); however, very few children with measured blood lead levels in the 1999–2004 survey period had BLLs ≥10 μg/dL (N = 53) and of these children only eight had blood lead levels above 20 μg/dL, indicating that lead-based paint may no longer be as significant an exposure source for young children as it once was. This is supported by the observation that among children with elevated BLLs, a slightly smaller percentage lives in the Northeast than in the South—a region shown to have housing with about half the prevalence of lead-based paint hazards compared to housing in the Northeast (Jacobs et al. 2002). Additionally, no association was observed for year of housing construction when blood lead levels of children living in the Northeast were evaluated separately despite the fact that older age of housing, another marker for the presence of lead-based paint, has been strongly associated with higher blood lead levels in children (Bernard and McGeehin 2003; Kaufmann et al. 2000; Mannino et al. 2003; Pirkle et al. 1998; Rabito et al. 2007; Sargent et al. 1997).
Furthermore, lead concentrations in window dust samples had a very minor effect on BLLs for Midwestern children, but significantly impacted BLLs of children living in the South and West. Given these findings, it is possible that lead dust measured in homes originated from multiple sources and was not simply due to the presence of lead-based paint. As reported by Jacobs et al. (2002), approximately 2.7 million homes have dust lead hazards but no lead-based paint in the home. Transfer of lead dust from an occupational source to the home, second-hand smoke, hobbies involving ceramics, ammunition or glass making, and lead emissions from local industries have been shown to result in lead-contaminated dust (Bates et al. 1997; Dorevitch and Babin 2001; Friedman et al. 2005; Gulson et al. 1996; Kawai et al. 1983; Maharachpong et al. 2006; Mannino et al. 2003; Rahbar et al. 2002; Whelan et al. 1997). Indeed, a study of lead house dust in 64 residences in a Northeastern urban city demonstrated that exterior proximate sources such as crustal materials and deposited airborne particulates were responsible for ~66% of lead house dust mass (Adgate et al. 1998). Just as notable, a review by Laidlaw and Filippelli (2008) of several studies evaluating the resuspension and contribution of lead-contaminated soil to interior household lead loading has suggested that the source of outdoor lead loading penetrating homes is likely a combination of lead from past use of leaded gasoline with lesser amounts from lead-based paint.
In light of the numerous recalls of children’s products, such as toys, jewelry, and lunchboxes, it is likely that exposure to lead may have also occurred from contact with these types of goods. Nevertheless, it is important to note that the trends and differences in blood lead levels observed in this study may be the result of multifaceted public health efforts, including primary and secondary lead-poisoning prevention programs, to reduce lead in children’s environment.
The results presented here are conditional on a number of limitations. First, we were unable to adjust for exposure to environmental tobacco smoke, which has been shown to be associated with increased blood lead levels in children (Berglund et al. 2000; Friedman et al. 2005; Mannino et al. 2003; Willers et al. 1988), as cotinine was measured only in children three years and older. Nevertheless, blood lead concentrations described in the current study are within the range of levels presented by Mannino et al. (2003) across strata of cotinine concentrations.
Second, we cannot rule out the effect of selection bias since not all children that participated in the surveys had measured blood lead levels and because we excluded children who were missing data for several other covariates. In spite of this, the similar LSGM regional concentrations reported in Tables 1 and 4 for the 1999–2004 survey period suggest that our estimates are quite robust. Finally, because such a low percentage of children with measured BLLs had concentrations ≥10 μg/dL, we were only able to calculate the prevalence of elevated BLLs by region and could not adjust these estimates for other important factors such as age, race/ethnicity, and year of housing construction.
While these data confirm that BLLs continue to decline in the United States, they also suggest that blood lead levels in children may vary between specific geographic regions which could be a proxy indicator that historically significant sources of lead exposure, such as lead-based paint, may be less significant now compared to 20–30 years ago. Regardless, this study also illustrates the need to continue considering the effect of geographic region when determining reference levels of lead in the blood of young children as well as the effect of various characteristics on blood lead levels of children within each region. As the CDC has suggested, prevention and surveillance strategies for lead exposure should be designed to target at-risk children (Binder and Falk 1991; CDC 1991, 1997b, 2000, 2002; Meyer et al. 2003). The results presented here should be useful in determining which demographic groups are at an increased risk of having higher BLLs, and our analysis of factors thought to influence blood lead levels should provide insight with regard to lessening future exposures of children in the United States.
References
Adgate JL, Willis RD, Buckley TJ, Chow JC, Watson JG, Rhoads GG, Lioy PJ (1998) Chemical mass balance source apportionment of lead in house dust. Environ Sci Technol 32(1):108–114
Anderson LA Jr (1995) A review of blood lead results from the Third National Health and Nutrition Examination Survey (NHANES III). Am Ind Hyg Assoc J 56(1):7–8
ATSDR (Agency for Toxic Substances and Disease Registry) (2007) Toxicological Profile for Lead. U.S. Department of Health and Human Services, Public Health Service, Atlanta, GA
Bates MN, Wyatt R, Garrett N (1997) Old paint removal and blood lead levels in children. New Zeal Med J 110(1053):373–377
Berglund M, Lind B, Sorensen S, Vahter M (2000) Impact of soil and dust lead on children’s blood lead in contaminated areas of Sweden. Arch Environ Health 55(2):93–97
Bernard SM, McGeehin MA (2003) Prevalence of blood lead levels > or = 5 micro g/dL among US children 1 to 5 years of age and socioeconomic and demographic factors associated with blood of lead levels 5 to 10 micro g/dL, Third National Health and Nutrition Examination Survey, 1988–1994. Pediatrics 112:1308–1313
Binder S, Falk H (1991) Strategic plan for the elimination of childhood lead poisoning. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Public Health Service, Atlanta, GA
Brody DJ, Pirkle JL, Kramer RA, Flegal KM, Matte TD, Gunter EW et al (1994) Blood lead levels in the US population. Phase 1 of the Third National Health and Nutrition Examination Survey (NHANES III, 1988 to 1991). JAMA 272(4):277–283
CDC (Centers for Disease Control and Prevention) (1991) Preventing lead poisoning in young children: a statement by the centers for disease control. U.S. Department of Health and Human Services, Public Health Service, Atlanta, GA
CDC (Centers for Disease Control and Prevention) (1994) Blood lead levels–United States, 1988–1991. MMWR Morb Mortal Wkly Rep 43(30):545–548
CDC (Centers for Disease Control and Prevention) (1997a) Update: blood lead levels–United States, 1991–1994. MMWR Morb Mortal Wkly Rep 46(7):141–146
CDC (Centers for Disease Control and Prevention) (1997b) Screening young children for lead poisoning: guidance for state and local public health officials. U.S. Department of Health and Human Services, Atlanta, GA
CDC (Centers for Disease Control and Prevention) (2000) Blood lead levels in young children–United States and selected states, 1996–1999. MMWR Morb Mortal Wkly Rep 49(50):1133–1137
CDC (Centers for Disease Control and Prevention) (2002) Managing elevated BLLs among young children: recommendations from the advisory committee on childhood lead poisoning prevention. U.S. Department of Health and Human Services, Atlanta, GA
CDC (Centers for Disease Control and Prevention) (2005a) Blood lead levels–United States, 1999–2002. MMWR Morb Mortal Wkly Rep 54(20):513–516
CDC (Centers for Disease Control and Prevention) (2005b) Third national report on human exposure to environmental chemicals. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Environmental Health, Atlanta, GA
CDC (Centers for Disease Control and Prevention) (2007) Interpreting and managing blood lead levels <10 micro g/dL in children and reducing childhood exposures to lead: Recommendations of CDC’s advisory committee on childhood lead poisoning prevention. MMWR Recomm Rep 56(RR-8):1–16
CEH/CAPP Committee on Environmental Hazards and Committee on Accident and Poison Prevention) (1987) Statement on childhood lead poisoning. Pediatrics 79(3):457–465
Diamond RC (2001) An overview of the U.S. building stock. In: Spengler JD, Samet JM, McCarthy JF (eds) Indoor air quality handbook. McGraw-Hill, New York, 2001 pp 6.3–6.17
Dorevitch S, Babin A (2001) Health hazards of ceramic artists. Occup Med 16(4):563–575
Friedman LS, Lukyanova OM, Kundiev YI, Shkiryak-Nizhnyk ZA, Chislovska NV, Mucha A, Zvinchuk AV, Oliynyk I, Hryhorczuk D (2005) Predictors of elevated blood lead levels among 3-year-old Ukrainian children: a nested case-control study. Environ Res 99(2):235–242
Gulson BL, Mizon KJ, Korsch MJ, Howarth D (1996) Importance of monitoring family members in establishing sources and pathways of lead in blood. Sci Total Environ 188(2–3):173–182
Jacobs DE, Clickner RP, Zhou JY, Viet SM, Marker DA, Rogers JW, Zeldin DC, Broene P, Friedman W (2002) The prevalence of lead-based paint hazards in U.S. housing. Environ Health Perspect 110(10):599–606
Kaufmann RB, Clouse TL, Olson DR, Matte TD (2000) Elevated blood lead levels and blood lead screening among U.S. children aged one to five years: 1988–1994. Pediatrics 106(6):1–7
Kawai M, Toriumi H, Katagiri Y, Maruyama Y (1983) Home lead-work as a potential source of lead exposure for children. Int Arch Occup Environ Health 53(1):37–46
Laidlaw MAS, Filippelli GM (2008) Resuspension of urban soils as a persistent source of lead poisoning in children: a review and new directions. Appl Geochem 23(8):2021–2039
Maharachpong N, Geater A, Chongsuvivatwong V (2006) Environmental and childhood lead contamination in the proximity of boat-repair yards in southern Thailand—I: pattern and factors related to soil and household dust lead levels. Environ Res 101(3):294–303
Mannino DM, Albalak R, Grosse S, Repace J (2003) Second-hand smoke exposure and blood lead levels in U.S. children. Epidemiology 14(6):719–727
Meyer PA, Pivetz T, Dignam TA, Homa DM, Schoonover J, Brody D (2003) Surveillance for elevated blood lead levels among children–United States, 1997–2001. MMWR Surveill Summ 52(10):1–21
NCHS (National Center for Health Statistics) (2005) National health and nutrition examination survey data. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Hyattsville, MD
Pirkle JL, Brody DJ, Gunter EW, Kramer RA, Paschal DC, Flegal KM, Matte TD (1994) The decline in blood lead levels in the United States. The national health and nutrition examination surveys (NHANES). JAMA 272(4):284–291
Pirkle JL, Kaufmann RB, Brody DJ, Hickman T, Gunter EW, Paschal DC (1998) Exposure of the U.S. population to lead, 1991–1994. Environ Health Perspect 106(11):745–750
Rabito FA, Iqbal S, Shorter CF, Osman P, Philips PE, Langlois E, White LE (2007) The association between demolition activity and children’s blood lead levels. Environ Res 103:345–351
Rahbar MH, White F, Agboatwalla M, Hozhabri S, Luby S (2002) Factors associated with elevated blood lead concentrations in children in Karachi, Pakistan. Bull World Health Organ 80(10):769–775
Sargent JD, Bailey A, Simon P, Blake M, Dalton MA (1997) Census tract analysis of lead exposure in Rhode Island children. Environ Res 74:159–168
Sargent JD, Dalton M, Demidenko E, Simon P, Klein RZ (1999) The association between state housing policy and lead poisoning in children. Am J Public Health 89(11):1690–1695
Whelan EA, Piacitelli GM, Gerwel B, Schnorr TM, Mueller CA, Gittleman J, Matte TD (1997) Elevated blood lead levels in children of construction workers. Am J Publ Health 87(8):1352–1355
Willers S, Schutz A, Attewell R, Skerfving S (1988) Relation between lead and cadmium in blood and the involuntary smoking of children. Scand J Work Environ Health 14(6):385–389
Conflict of interest
Support for this research was provided by firms involved in the metals industry that, at times, are involved in litigation related to lead in the environment. These sponsors were not involved in any way with the preparation or editing of this manuscript. In addition, none of the authors of this manuscript have ever served as experts in lead-related litigation and have no other connections to the metals industry.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Scott, L.L.F., Nguyen, L.M. Geographic region of residence and blood lead levels in US children: results of the National Health and Nutrition Examination Survey. Int Arch Occup Environ Health 84, 513–522 (2011). https://doi.org/10.1007/s00420-011-0624-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-011-0624-9