Abstract
Purpose
This study aimed to investigate the clinical characteristics of patients with recurrent intraocular lens (IOL) dislocation after scleral-fixated sutured IOL implantation and evaluate the long-term outcomes of scleral re-fixation of IOL.
Methods
The medical records of patients who underwent surgery for IOL dislocation between January 2011 and January 2021 were reviewed. The study included 164 patients (male: 131, female: 33) (176 eyes). Patient demographics, preoperative, intraoperative and postoperative data, and the ocular and systemic conditions associated with IOL re-dislocation were analyzed.
Results
The study included 176 consecutive cases of scleral-fixated sutured IOL. Twenty-six eyes (14.8%) showed re-dislocation of IOL after the initial IOL scleral fixation and underwent reoperation (mean 75.5 ± 62.5 months after the first surgery); three (11.5%) of them required a third surgery. Younger adults (aged less than 40 years), and patients who underwent IOL scleral fixation in complicated cataract surgery or aphakic state had a higher risk of re-dislocation. Diabetes mellitus (DM) was the only statistically significantly higher risk factor in the re-dislocated group (p = 0.041). The complication rate with scleral re-fixation was higher than that in the non-re-dislocated group. No statistically significant differences were observed, except for vitreous hemorrhage (p = 0.024).
Conclusions
Caution should be exercised when performing sutured scleral fixation of IOL in younger patients, cases of complicated cataract surgery and aphakia, and patients with DM to prevent IOL re-dislocation. Scleral-fixated sutured IOL in eyes with recurrent IOL dislocation seems to be a safe and effective procedure with a relatively low complication rate.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.

Introduction
Advancements in cataract surgery techniques and technologies over the last few decades have led to significant changes in the frequency of cataract surgery [1]. Klein et al. reported that the incidence of cataract surgery increased 6.5-fold between 1988–1990 and 2008–2010 [2]. The demand for surgery is expected to increase further as a result of increased life expectancy and changing indications for surgery, especially in terms of correction of refractive errors or lowering of the intraocular pressure (IOP) [3,4,5]. Late in-the-bag intraocular lens (IOL) dislocation is a serious long-term complication of cataract surgery, which usually requires surgical management. In recent years, an increase in the number of surgeries for late IOL dislocations has been noted, with a reported incidence rate of 0.05–3.00% [6,7,8], and an increasing trend for the occurrence of in-the-bag IOL dislocation has been reported [9, 10].
There are several techniques for secondary IOL implantation, including anterior chamber IOL, iris-claw IOL, iris-sutured posterior chamber (PC) IOL, scleral-sutured PCIOL, and intrascleral haptic fixation, all of which are known as safe and effective [11]. Since Malbran first introduced a sutured scleral-fixated IOLs for the management of aphakia following intracapsular cataract extraction in the 1980s [12], it has been widely adopted and modified and has become one of the most useful methods available to fix IOL when there is limited or no capsular support. However, subluxation or luxation of IOL may occur even after sutured scleral fixation of IOL [11, 13], and there is little information on whether sutured scleral re-fixation of the IOL is safe and effective.
In this study, we retrospectively reviewed the medical records of consecutive patients with IOL dislocation, and the clinical characteristics of patients with recurrent IOL dislocation after scleral-sutured IOL implantation were demonstrated and analyzed. Moreover, we investigated the long-term outcomes of the scleral re-fixation of the IOL.
Methods
This study adhered to the tenets of the Declaration of Helsinki, and the requirement to obtain informed consent was waived by the Institutional Review Board (IRB 4–2021-1522). We retrospectively reviewed 243 consecutive cases of 229 patients who underwent a scleral-fixated sutured IOL implantation performed between January 2011 and January 2021 at the Severance Hospital. All patients with a follow-up period of less than 6 months were excluded. Among the patients with IOL re-dislocation after a scleral-fixated sutured IOL implantation, IOL re-dislocation less than 3 months after the initial sutured scleral fixation of IOL surgery was excluded. In addition, the patients who underwent the second surgery other than the sutured scleral fixation of IOL, such as sutured iris fixated IOL, iris-claw IOL, or intrascleral haptic fixation were excluded. After exclusion, 176 eyes of 164 patients were included in the analysis.
The following data were collected: age, sex, indication for initial IOL fixation surgery, preoperative, and postoperative best-corrected visual acuities (BCVAs) using a Snellen chart, IOP by non-contact tonometry, refractive data using an auto kerato-refractometer (KR-1, Topcon Medical Systems, Inc.; Oakland, NJ, USA), endothelial cell count (ECC) assessed automatically using specular microscopy (CellChek XL, Konan Medical USA Inc.; Irvine, CA, USA), axial length measurement obtained using a ZEISS IOLMaster 500 (Carl Zeiss AG; Heidenheim, Germany), complications, medical history, ocular history, surgical technique, and suture material used to fix the IOL. Complicated cataract surgery was defined as cataract surgery with an unexpected posterior capsule rupture or zonular weakness, mostly accompanied by vitreous loss during routine cataract surgery. We also investigated the presence of known systemic and ophthalmic risk factors, including diabetes mellitus (DM), pseudoexfoliation, atopic dermatitis, retinitis pigmentosa, and connective tissue disorders, before the date of the first IOL fixation surgery for IOL dislocation.
Surgical technique
All cases of scleral fixation of IOL in this study were performed under general or local anesthesia by one of the multiple surgeons at the Severance Hospital. A double-armed polypropylene suture with curved needles was inserted 2 mm posteriorly from the limbus using an ab externo technique. The sutures used to fixate the IOL were either 10–0, 9–0, or 8–0 polypropylene (Prolene®, Ethicon Inc., Somerville. NJ, USA). The suture was retracted using a 27-gauge needle, which was entered at the opposite side of the sclera in a similar fashion. The suture was then drawn out of the eye through a corneoscleral incision, cut, and tied to each haptic of the IOL. The procedure was performed using Rayner 920H (Rayner Intraocular Lenses Ltd., Hove, East Sussex, UK), Tecnis® ZCB00 (Johnson & Johnson Vision, Santa Ana, CA, USA), CZ70BD® (Alcon Laboratories, Inc., Ft Worth, TX, USA), Sensar® AR40e (Pharamacia and Upjohn LLC, North Peapack, NJ), or ARTIS® PL E (Cristalens Industrie, Lannion, France). In cases of using a single-piece IOL with 4 haptics (e.g., ARTIS® PL E), the modified single-loop suture technique [14] was used for scleral fixation of IOL. The dislocated IOL was repositioned when possible or, otherwise, removed and exchanged for a new IOL. Each end of the polypropylene suture was used to create a knot beneath the scleral flap. In cases without scleral flaps, the suture knots were buried under the conjunctiva. The conjunctiva was sutured with 8–0 polyglactin (Vicryl; Ethicon, Inc., Somerville, NJ). Postoperatively, moxifloxacin and prednisolone eyedrops were administered every 6 to 4 hours and then tapered for 4 to 6 weeks.
Statistical analysis
Data are presented as mean or median with standard deviation or interquartile range for quantitative variables and with absolute and relative frequencies for qualitative variables. Inferential analyses to compare patients who required a secondary procedure due to IOL re-dislocation with those who did not require such procedures were performed using the non-parametric Mann–Whitney U test for quantitative variables and Fisher’s exact test for qualitative variables. The Snellen chart BCVA was converted to the logarithm of the minimum angle of resolution (logMAR). A Wilcoxon signed-rank test for non-parametric data was used to compare the preoperative and postoperative BCVA (logMAR) and IOP. All data were analyzed using statistical analysis software (Statistical Package for the Social Sciences version 25, Armonk, NY, USA; IBM Corp), and the level of statistical significance was set at the two-sided 5% level.
Results
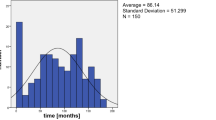
A total of 164 patients (male: 131, female: 33) (176 eyes, 12 patients had bilateral IOL dislocations) were included in this study, with a mean age of 58.1 ± 13.6 (range, 16–83) years. The included patients had a mean follow-up period of 39.3 ± 31.9 (range, 6–156) months. A second scleral-fixated sutured IOL operation was performed in 26 eyes (14.8%) (re-dislocated group). Three (11.5%) of these cases required a third operation at 4, 44, and 116 months after the second scleral-sutured IOL implantation, respectively. Among the 12 patients (male: 11, female: 1) with bilateral IOL dislocation, the mean age was 59.3 ± 17.1 (range, 16–83) years, with a mean follow-up period of 51.6 ± 33.1 (range, 11.2–127.6) months. Of the 24 eyes of 12 patients, five were included in the re-dislocated group, and 19 were included in the non-re-dislocated group.
Table 1 shows the preoperative characteristics of all patients. In the re-dislocated group, 21 patients were men (14.8% of the total male sample). There was a male preponderance, with no statistically significant difference between the non-re-dislocated and re-dislocated groups (p = 0.990). The mean age of the re-dislocated group was statistically significantly younger (52.0 ± 16.1 years) than that of the non-re-dislocated group (59.1 ± 12.9 years; Mann–Whitney U test, p = 0.032). Age was then divided into three groups: group 1, 39 years old or younger; group 2, from 40 to 59 years old, and group 3, 60 years old or older. In the re-dislocated group, six eyes were included in group 1 (40% of this age group), 10 eyes in group 2 (13.3% of this age group), and 10 eyes in group 3 (11.6% of this age group). Younger patients had a significantly higher rate of reoperation (p = 0.015).
The indications for primary scleral-fixated sutured IOL were luxation or subluxation of the IOL (84.1%), complicated cataract surgery (6.8%), aphakia (6.3%), and luxation or subluxation of the crystalline lens (2.8%) (Table 1). In the re-dislocated group, primary fixation with luxation or subluxation of the IOL (9.5% of all luxations and subluxations of the IOL cases) was the most common primary indication, followed by previous aphakia (54.6% of this subgroup), complicated cataract surgery (41.7% of this subgroup), and luxation or subluxation of the crystalline lens (20% of this subgroup). Primary scleral-sutured IOL implantation in complicated cataract surgery and in the aphakic state had a significantly higher rate of reoperation (p < 0.001).
The mean axial length of all eyes was 24.86 ± 2.02 (range, 21.54–34.57) mm. There was no statistically significant difference in the axial length between the non-re-dislocated and re-dislocated groups (24.8 ± 2.01 mm and 25.3 ± 2.07 mm, respectively; Mann–Whitney U test, p = 0.068). Among the prespecified risk factors, the previous vitrectomy was the most common (21.0%), followed by trauma (11.4%) and DM (10.8%). DM was the only statistically significantly higher risk factor in the re-dislocated group (p = 0.041).
Table 2 presents the intraoperative data of the non-re-dislocated and re-dislocated groups. In the re-dislocated group, 24 eyes (92.3%) were previously sutured with 10–0 polypropylene, one (3.8%) with 9–0 polypropylene, and one (3.8%) with 8–0 polypropylene. Of the 148 eyes which underwent IOL reposition or exchange at the initial scleral fixation surgery, 14 eyes underwent reoperation, with eight cases of IOL reposition (57.1%) and six cases of IOL exchange (42.9%). There were no significant differences between the two groups with regard to the suture material, explanation or reposition of IOL, and the incision site for IOL exchange (Fisher’s exact test, p > 0.05; Table 2).
The postoperative changes at 6 months in mean BCVA, IOP, endothelial cell density, and refractive errors are revealed in Table 3. BCVA improved significantly in both groups postoperatively (p < 0.001, non-re-dislocated group; p = 0.031, re-dislocated group). There was no statistically significant change in median IOP in the 6-month follow-up period compared with the preoperative baseline in either group (p = 0.729, non-re-dislocated group; p = 0.447, re-dislocated group). The mean ECC values before and 6 months after surgery were 2224.5 ± 567.9 and 1635.6 ± 747.8 and 2099.9 ± 606.5 and 1482.7 ± 677.1 in the non-re-dislocated and re-dislocated groups, respectively. A significant reduction in ECC was observed in both groups (p < 0.001 in both groups).
The complications after scleral-sutured IOL implantation are summarized in Table 4. Postoperative complications were categorized as IOP elevation (26.7%), cystoid macular edema (16.5%), uveitis (8.5%), bullous keratopathy (3.4%), vitreous hemorrhage (2.8%), suture exposure (1.7%), and retinal detachment (1.1%). Overall complications tended to be higher in the re-dislocated group than that in the non-re-dislocated group, but the difference was not statistically significant, except for vitreous hemorrhage (p = 0.024).
Discussion
Long-term IOL dislocation rates in scleral-sutured IOLs have been reported to range from 0 to 28% in previous studies [11]. In our study, 14.8% of cases of scleral-sutured IOLs were re-dislocated, which is consistent with those of previous reports. The mean interval between IOL suture and suture breakage was reported from 29.5 months to 50 months [15, 16], while the mean interval between the suturing of the IOL and the dislocation was 75.5 ± 62.5 (4.0–244.6) months in this study, which appears to be longer.
Patient age has been considered one of the possible risk factors for suture breakage in scleral-sutured IOLs. Younger patients were reported to be more likely to have broken sutures [15], and patients aged < 65 years were reported to have a higher tendency of suture breakage than those aged ≥ 65 years [17]. Furthermore, the odds ratio of suture breakage in younger patients aged < 39 years was 4.4 [13]. The reason for the higher incidence of recurrent IOL dislocation in younger patients has rarely been discussed. It may be due to the continuous micro-trauma related to the “active lifestyle” of younger patients [15]. To prevent suture breakage, the use of multiple sutures on each haptic, thicker suture, or different suture materials has been suggested. Buckley et al. [18] noted that caution should be exercised when using a 10–0 polypropylene suture in children, and an alternative thicker suture (such as 9–0 polypropylene) should be considered. There may be advantages to using large-diameter 8–0 or 9–0 polypropylene or CV-8 polytetrafluoroethylene. Since 10–0 polypropylene is known to degrade faster, it would be reasonable to expect that a thicker suture would be more resistant to damage and breakdown and that it would be associated with decreased rates of IOL dislocation [11]. Since younger patients have a longer life expectancy, the high risk of recurrent IOL dislocation could be a burden for surgeons. Further studies are needed to identify the best suture material and technique for long-term IOL stability. In addition, recent sutureless techniques, such as retropupillary iris-claw lens or intrascleral haptic fixation of IOL, can be attempted, once long-term stability and safety are confirmed.
Among the primary indications for scleral-sutured IOL implantation, recurrent IOL dislocation occurred more frequently in cases of aphakia and complicated cataract surgery (23.1% and 19.2%, respectively) than in pseudophakic or phakic luxation/subluxation cases. In aphakia cases, aphakic state after complicated cataract surgery or pars plana lensectomy with vitrectomy was included. In complicated cataract surgeries, vitreous loss typically occurs when the integrity of the posterior capsule or lens zonules is compromised, allowing the vitreous to prolapse into the anterior chamber, requiring anterior vitrectomy and/or vitrectomy in most cases. Scleral-sutured IOL surgery in such situations implies an unplanned procedure. Anterior vitrectomy, especially unplanned, has been a major risk factor for IOL dislocation [19]. However, in a previous report [13], the number of cases that required a reoperation was 14 with previous aphakia (6.73% of all cases with aphakia), followed by six with luxation and subluxation of the IOL (9.09% of this subgroup), and three with luxation and subluxation of the lens (11.54% of this subgroup), which was different from our study.
Increased IOP is a well-documented complication after scleral-fixated IOL implantation, affecting up to 44% of eyes [20, 21]. Increased IOP was the most common complication in our study, accounting for 26.7% of all cases. Overall complications including ocular hypertension tended to be higher in the re-dislocated group than in the non-re-dislocated group, but the difference was not statistically significant, except for vitreous hemorrhage (p = 0.024). Complications such as uveitis-glaucoma-hyphema (UGH) syndrome, iris capture, and reverse pupillary block were not observed in our series. However, among patients with increased IOP, subclinical reverse pupillary block and pigment dispersion syndrome cannot be completely ruled out.
The limitations of this study include its retrospective design, small sample size, and a single-center multi-surgeon data. Because of the retrospective design of the study, many surgical factors including the tension of the sutures could not be investigated. Because of the small sample size, comparisons between each surgeon with different experiences or each technique were not possible. The preferences and proficiency of each surgeon also could be significant confounders in this study.
In conclusion, recurrent dislocation of the scleral-sutured IOL is not a common complication during long-term follow-up. The risk factors of IOL re-dislocation after sutured scleral fixation of IOL included younger adults, complicated cataract surgery and aphakia, and DM. Caution should be exercised when performing sutured scleral fixation of IOL in younger patients, cases of complicated cataract surgery and aphakia, and patients with DM to prevent IOL re-dislocation. Recurrent sutured IOL dislocation can be managed with IOL exchange or repositioning with a safe and effective scleral-sutured IOL technique.
References
Erie JC (2014) Rising cataract surgery rates: demand and supply. Ophthalmology 121:2–4. https://doi.org/10.1016/j.ophtha.2013.10.002
Klein BE, Howard KP, Lee KE, Klein R (2014) Changing incidence of lens extraction over 20 years: the Beaver Dam eye study. Ophthalmology 121:5–9
Alio JL, Grzybowski A, El Aswad A, Romaniuk D (2014) Refractive lens exchange. Surv Ophthalmol 59:579–598. https://doi.org/10.1016/j.survophthal.2014.04.004
Azuara-Blanco A, Burr J, Ramsay C, Cooper D, Foster PJ, Friedman DS, Scotland G, Javanbakht M, Cochrane C, Norrie J, group Es (2016) Effectiveness of early lens extraction for the treatment of primary angle-closure glaucoma (EAGLE): a randomised controlled trial. Lancet 388:1389–1397. https://doi.org/10.1016/S0140-6736(16)30956-4
Lee CM, Afshari NA (2017) The global state of cataract blindness. Curr Opin Ophthalmol 28:98–103. https://doi.org/10.1097/ICU.0000000000000340
Jakobsson G, Zetterberg M, Lundstrom M, Stenevi U, Grenmark R, Sundelin K (2010) Late dislocation of in-the-bag and out-of-the bag intraocular lenses: ocular and surgical characteristics and time to lens repositioning. J Cataract Refract Surg 36:1637–1644. https://doi.org/10.1016/j.jcrs.2010.04.042
Gimbel HV, Condon GP, Kohnen T, Olson RJ, Halkiadakis I (2005) Late in-the-bag intraocular lens dislocation: incidence, prevention, and management. J Cataract Refract Surg 31:2193–2204. https://doi.org/10.1016/j.jcrs.2005.06.053
Stark WJ Jr, Maumenee AE, Datiles M, Fagadau W, Baker CC, Worthen D, Auer C, Klein P, McGhee E, Jacobs ME et al (1983) Intraocular lenses: complications and visual results. Trans Am Ophthalmol Soc 81:280–309
Kim SS, Smiddy WE, Feuer W, Shi W (2008) Management of dislocated intraocular lenses. Ophthalmology 115:1699–1704. https://doi.org/10.1016/j.ophtha.2008.04.016
Dabrowska-Kloda K, Kloda T, Boudiaf S, Jakobsson G, Stenevi U (2015) Incidence and risk factors of late in-the-bag intraocular lens dislocation: evaluation of 140 eyes between 1992 and 2012. J Cataract Refract Surg 41:1376–1382. https://doi.org/10.1016/j.jcrs.2014.10.040
Shen JF, Deng S, Hammersmith KM, Kuo AN, Li JY, Weikert MP, Shtein RM (2020) Intraocular lens implantation in the absence of zonular support: an outcomes and safety update: a report by the American Academy of Ophthalmology. Ophthalmology 127:1234–1258. https://doi.org/10.1016/j.ophtha.2020.03.005
Malbran ES, Malbran E Jr, Negri I (1986) Lens guide suture for transport and fixation in secondary IOL implantation after intracapsular extraction. Int Ophthalmol 9:151–160. https://doi.org/10.1007/BF00159844
Bausili Portabella MM, Nadal J, Alvarez de Toledo J, Fideliz de la Paz M, Barraquer RI (2020) Long-term outcome of scleral-sutured posterior chamber intraocular lens: a case series. Br J Ophthalmol 104:712–717. https://doi.org/10.1136/bjophthalmol-2019-314054
Oh HS, Chu YK, Kwon OW (2007) Surgical technique for suture fixation of a single-piece hydrophilic acrylic intraocular lens in the absence of capsule support. J Cataract Refract Surg 33:962–965. https://doi.org/10.1016/j.jcrs.2006.09.050
Vote BJ, Tranos P, Bunce C, Charteris DG, Da Cruz L (2006) Long-term outcome of combined pars plana vitrectomy and scleral fixated sutured posterior chamber intraocular lens implantation. Am J Ophthalmol 141:308–312. https://doi.org/10.1016/j.ajo.2005.09.012
Cho BJ, Yu HG (2014) Surgical outcomes according to vitreous management after scleral fixation of posterior chamber intraocular lenses. Retina 34:1977–1984. https://doi.org/10.1097/IAE.0000000000000168
Kawano S, Takeuchi M, Tanaka S, Yamashita T, Sakamoto T, Kawakami K (2019) Current status of late and recurrent intraocular lens dislocation: analysis of real-world data in Japan. Jpn J Ophthalmol 63:65–72. https://doi.org/10.1007/s10384-018-0637-y
Buckley EG (2008) Safety of transscleral-sutured intraocular lenses in children. J AAPOS 12:431–439. https://doi.org/10.1016/j.jaapos.2008.04.016
Clark A, Morlet N, Ng JQ, Preen DB, Semmens JB (2015) Long-term trends and outcomes of anterior vitrectomy in Western Australia. Acta Ophthalmol 93:27–32. https://doi.org/10.1111/aos.12453
Krause L, Bechrakis NE, Heimann H, Salditt S, Foerster MH (2009) Implantation of scleral fixated sutured posterior chamber lenses: a retrospective analysis of 119 cases. Int Ophthalmol 29:207–212. https://doi.org/10.1007/s10792-008-9217-3
McAllister AS, Hirst LW (2011) Visual outcomes and complications of scleral-fixated posterior chamber intraocular lenses. J Cataract Refract Surg 37:1263–1269. https://doi.org/10.1016/j.jcrs.2011.02.023
Funding
This research was supported by grants for the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Science, ICT & Future Planning (grant number: 2019R1A2C2086729). The funding organization had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the Institutional Review Board of Severance Hospital (IRB No. 4–2021-1522) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
According to the IRB standard operating procedures for retrospective clinical study, the Ethics Committee ruled that subject consent was not required for this study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, Y., Choi, E.Y., Lee, C.S. et al. Clinical Characteristics of recurrent intraocular lens dislocation after scleral-fixated sutured intraocular lens and long-term outcomes of intraocular lens re-fixation. Graefes Arch Clin Exp Ophthalmol 260, 3267–3273 (2022). https://doi.org/10.1007/s00417-022-05692-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05692-9