Abstract
Purpose
To evaluate macular structural changes during the active and remission periods in patients with Behçet uveitis and to further assess the factors affecting final visual acuity.
Methods
Clinical records and spectral domain-optical coherence tomography (SD-OCT) findings of patients with Behçet uveitis were retrospectively reviewed.
Results
Sixty-nine eyes of 35 patients were included in the study. SD-OCT findings in the active uveitis period included epiretinal membrane (ERM) in 26 (37.1%) eyes, ellipsoid zone (EZ) damage in 11 (15.7%), external limiting membrane (ELM) damage in 10 (14.3%), macular atrophy in 6 (8.6%), disruption of retinal pigment epithelium (RPE) in 11 (15.7%), a macular scar in 1 (1.4%), and loss of normal foveal contour appearance in 15 (21.4%). There was macular edema in 23 eyes (32.9%) in the active uveitis period (11 (15.7%) cystoid macular edema, 10 (14.3%) diffuse macular edema, and 7 (10.0%) serous retinal detachment). In the remission period, SD-OCT findings included ERM in 37 (52.9%) eyes, EZ damage in 14 (20%), ELM damage in 14 (20%), macular atrophy in 7 (10%), disruption of RPE in 14 (20.0%), macular scar in 1 (1.4%), and loss of normal foveal contour appearance in 17 (24.3%). The mean central macular thickness in the remission period was significantly lower than in the active uveitis period (p < 0.001). The presence of EZ damage and loss of normal foveal contour appearance in active uveitis period were the independent factors associated with final visual acuity (logMAR) (β = 0.736, p = 0.003; β = 0.682, p = 0.002, respectively).
Conclusion
Ellipsoid zone damage and loss of normal foveal contour appearance are important factors affecting visual acuity in Behçet uveitis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.

Introduction
Behçet disease (BD) is a chronic multisystemic disorder characterized by relapsing-remitting inflammation. Behçet disease mostly affects young adults. It affects both male and female equally with the male gender having a risk factor for more severe involvement [1].
Ocular involvement is responsible for most frequent morbidity of BD by causing nongranulomatous panuveitis and retinal vasculitis [2]. Relapsing course of ocular inflammation leads to permanent damage of intraocular structures such as maculopathy, retinal vessel occlusions, and optic atrophy [2, 3]. Therefore, screening of patients with Behçet uveitis is important to prevent sight-threatening complications.
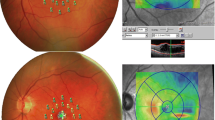
Fluorescein angiography (FA) is the standard imaging tool for the diagnosis and treatment monitoring of the patients with Behçet uveitis [4]. Leakage from retinal capillaries, vascular wall staining, retinal vein occlusion, cystoid macular edema (CME), capillary non-perfusion, and retinal and/or disk neovascularization is well documented by fluorescein angiography [4].
Spectral domain-optical coherence tomography (SD-OCT) is a non-invasive technique that provides high-resolution images of retinal structure. It is now used widely to detect changes in the retinal architecture in eyes with uveitis and to measure quantitatively the retinal thickness. Structural changes such as cystoid or diffuse macular edema (DME), vitreomacular interface diseases, the integrity of the outer retinal structures, the photoreceptor layer, and the retinal pigment epithelium (RPE) can be evaluated with this imaging method [5]. SD-OCT also allows us to evaluate the ellipsoid zone (EZ), which has been reported to have a close relationship with visual function. Two cross-sectional studies using SD-OCT described the disruption of EZ in Behçet disease during the remission phase. These studies reported that the disruption of the EZ is strongly related to the loss of visual acuity [6, 7].
The aims of our study are to evaluate macular changes during the active and remission periods in patients with Behçet uveitis and to further assess the risk factors associated with final visual acuity.
Materials and methods
This is a retrospective, longitudinal study performed at Ankara University Faculty of Medicine, Department of Ophthalmology, a tertiary referral center for uveitis patients. All procedures performed in the study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. The consecutive patients who fulfilled the diagnostic criteria of the International Study Group for Behcet’s disease and were in an active phase of posterior or panuveitis were included in the study. The patients who were lost to follow-up or did not achieve remission were not enrolled. The records of the patients, who were followed over time, were also evaluated after achieving remission. Posterior uveitis and panuveitis were defined according to the criteria of the Standardization of Uveitis Nomenclature Working Group [8]. Exclusion criteria included the presence of substantial media opacities precluding SD-OCT imaging, concomitant retinal vascular diseases such as diabetic retinopathy and uveitis due to causes other than Behçet disease.
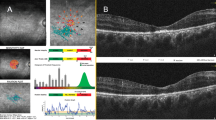
Demographic data, Snellen best-corrected visual acuity (BCVA), intraocular pressure, slit-lamp examination, dilated fundus examination, and laser flare meter (Kowa FC 600; Acculas, San Jose, CA, USA) records of the patients were retrospectively evaluated. BCVA values were converted to the logarithm of the minimum angle of resolution (logMAR) for statistical analysis. Visual acuity by eye was used for statistical analysis. Therapeutic regimes were also reviewed. Additionally, fluorescein angiography and SD-OCT images (Optovue Inc., Fremont, CA, USA) were evaluated. Structural SD-OCT findings, evaluated during both active and remission periods in each patients, included macular edema, RPE damage, EZ damage (Fig. 1), external limiting membrane (ELM) damage (Fig. 1), presence of epiretinal membrane (ERM), presence of atrophy, the structure of foveal contour, and macular thickness. We defined the remission phase as no inflammatory findings in clinical examination and also no leakage in FA.
Macular edema were classified as CME, DME, and serous retinal detachment. DME is characterized by disturbance of the layered retinal structure or spongelike low reflective areas and increased retinal thickness. CME is characterized by the formation of clearly defined intraretinal cystoid spaces (Fig. 1). Serous retinal detachment is characterized by a separation of the neurosensory retina from the underlying retinal pigment epithelium and fluid accumulation between these layers.
The EZ was identified as a distinct band just above the RPE-choriocapillaris line, and the line corresponding to the ELM was detected just above the EZ line. EZ and ELM integrity were also examined. We described the “EZ damage” as “discontinuity or irregularity or absence of the EZ”. Also, we described the “ELM damage” as “discontinuity or irregularity or absence of the ELM”. The term “macular damage” was defined as the presence of one of the following: ELM damage, EZ damage, disruption of RPE, or the combination of these findings.
The central macular thickness (CMT) was obtained by measuring the distance from the surface of the fovea to the RPE-choriocapillaris complex.
Statistical analysis
We used statistical models that took into account the dependency among right and left eyes to evaluate the data from 69 eyes of 35 patients. Data were summarized as the mean ± standard deviation and median (minimum-maximum) for continuous variables and frequencies (percentiles) for the categorical variables. In order to account for the clustered structure of the data, linear mixed effects models (random intercept model) were used to explain the variation in BCVA (logMAR) in the remission period throughout the left and right eyes, with regard to disruption of RPE, EZ damage, ELM damage, ERM formation, and loss of normal foveal contour appearance. In the comparison of BCVA, flare, and CMT in active and remission periods, linear mixed-effects model (random intercept model) was employed. Random intercept was used to introduce the dependency between the right and left eyes of the same patient. Generalized estimating equations were used to compare SD-OCT findings in active and remission periods. Correlations were assessed using the repeated measures correlation coefficient along with related P values. Statistical significance was set at a value of p < 0.05. The data were analyzed using SPSS 11.5 for Windows (SPSS Inc., Chicago, IL, USA) and R programming language. The “gee” package was used for generalized estimation equations, “lme4” package was used for mixed effect models, and “rmcorr” package was used for repeated measures correlation coefficient in R.
Results
Sixty-nine eyes of 35 patients (24 male and 11 female) with Behçet disease were included in the study. The mean age of the patients at the onset of uveitis and at the time of presentation to our institution were 28.3 ± 7.4 (range: 13–40) and 30.0 ± 9.0 (range: 13–51) years, respectively.
Bilateral involvement was detected in 34 patients (97.1%). Forty-four eyes had panuveitis and 25 had posterior uveitis. The mean disease duration was 72.2 ± 68.2 (range 5–236) months. Patients were followed up for a mean of 57.6 ± 49.5 (range: 4–208) months. The demographic characteristics of patients are shown in Table 1.
At the time of presentation, 24 (68.6%) patients were treatment-naive, 9 were on conventional immunosuppressive treatment and 1 was on interferon-alpha-2a, and 1 was on systemic corticosteroid. During the follow-up period, all patients received systemic immunosuppressive treatment which included interferon-alpha-2a in 14 (40%), azathioprine in 12 (34.3%), cyclosporine in 6 (17.1%), short-term oral prednisolone in 6 (17.1%), and infliximab + azathioprine in 3 (8.6%) patients.
Mean BCVA (logMAR) was 0.647 ± 0.9 (range: 0–3.2) in the active uveitis period and 0.355 ± 0.7 (range: 0–3.3) in the remission period. BCVA (logMAR) of the eyes with an active uveitis period was significantly lower than that in the remission period (p = 0.005). Mean flare values were 15.7 ± 11.2 (range: 1.4–38.4) ph/ms in the active uveitis period and 3.7 ± 1.4 (range: 1.1–20) ph/ms in the remission period. Mean flare values in the remission period were significantly lower than the flare values in the active uveitis period (p < 0.001).
In the active uveitis period, 26 (37.7%) eyes had normal SD-OCT findings and 43 (62.3%) eyes had any kind of macular pathology. In the active uveitis group, macular damage was also detected by SD-OCT, because some patients had already had uveitis attacks earlier than presentation to our institution. SD-OCT findings in the active uveitis period included ERM in 26 (37.7%) eyes, EZ damage in 11 (15.9%), ELM damage in 10 (14.5%), macular atrophy in 6 (8.7%), disruption of RPE in 11 (15.9%), a macular scar in 1 (1.4%), and loss of normal foveal contour appearance in 15 (21.7%). There was macular edema in 23 (33.3 %) eyes in the active uveitis period (CME in 11 (15.9%), DME in 10 (14.5%), serous retinal detachment in 7 (10.1%), and the combination of all patterns in 5 (7.2%)).
Mean CMT was 253.9 ± 156.4 (range: 53–841) μm in the active uveitis period and 163.1 ± 37.6 (range: 55–215) μm in the remission period. The mean CMT in the remission period was significantly lower than in the active uveitis period (p < 0.001). There is not a statistically significant relationship between macular thickness and high flare values in the active uveitis period (r = 0.549, p = 0.052). In terms of flare values in the remission period, there is not a statistically significant difference between the presence or absence of diffuse macular edema in the active uveitis period (p = 0.195). In the remission period, 32 (46.3%) eyes had normal SD-OCT findings and 37 (53.6%) eyes had any kind of macular pathology. In the remission period, SD-OCT findings included ERM in 37 (53.6%) eyes, EZ damage in 14 (20.3%), ELM damage in 14 (20.3%), macular atrophy in 7 (10.1%), disruption of RPE in 14 (20.3%), and loss of normal foveal contour appearance in 17 (24.6%). In the remission period, macular edema was not detected in any of the eyes. A comparison of SD-OCT findings in active and remission periods are given in Table 2.
ERM, ELM damage, EZ damage, disruption of RPE, and loss of normal foveal contour appearance have been identified as risk factors for decreased final visual acuity. Univariate linear mixed effects model for factors predicted to affect final BCVA is given in Table 3. Univariate linear mixed effects model was applied for these variables and variables with a p value below 0.20 were included in the multiple linear mixed effects model. However, ERM, ELM damage, EZ damage, and disruption of RPE were found to be statistically highly related to each other. While EZ damage, which is thought to have more clinical impact, was included in the model, others were excluded from the model. In this case, the final model was established with the remaining two variables.
Linear mixed effects model was carried out to investigate whether the presence of EZ damage and loss of normal foveal contour appearance could significantly predict patients’ final BCVA. The presence of EZ damage and loss of normal foveal contour appearance in active uveitis period were the statistically significant independent factors associated with final BCVA (logMAR) (β = 0.736, p = 0.003; β = 0.682, p = 0.002, respectively). The occurrence of BCVA in the EZ damage (+) group was 0.736 units higher than in the EZ damage (−) group and 0.682 units higher in those with loss of normal foveal contour appearance compared with the others (Table 4).
Discussion
Repeated ocular inflammatory attacks of BD can result in significant ocular damage leading to irreversible alterations and severe vision loss [9, 10]. In this study, we evaluated macular structural changes detected by SD-OCT during active and remission periods in patients with Behçet uveitis and investigated the influence of these variables on final visual acuity.
SD-OCT has been widely used in the diagnosis, treatment, and complications of uveitic patients [11]. A number of articles have described the advantages of SD-OCT in Behçet disease [6]. In our series, macular involvement was detected in 61.4% of eyes with active uveitis. We found that CMT in the remission period was significantly lower in comparison with the CMT in active uveitis period. Similarly to our results, Kang et al. showed that the mean CMT and the mean macular volume were significantly reduced after treatment compared with baseline in patients with Behçet uveitis [12]. Macular edema often appears as a complication that reduces vision in patients with Behçet uveitis. It is the result of the breakdown of the blood-retinal barrier, which is composed of tight junctions between the endothelium of non-fenestrated capillaries and RPE cells. Pro-inflammatory cytokines and vascular endothelial growth factors are involved in the breakdown of the blood-retinal barrier [13, 14]. SD-OCT examination is an important diagnostic method in the quantitative and qualitative evaluation of macular edema allowing identification of different patterns of macular edema in Behçet uveitis [15, 16]. Macular edema has been reported in 11.3 to 62% of patients with Behçet’s uveitis [2, 17]. In our study, macular edema was detected in 32.9%, CME in 15.7%, DME in 14.3%, serous retinal detachment in 10.0% of eyes.
If macular edema persists for several months, it gives rise to chronic macular changes leading to permanent visual impairment [18]. In our study, no statistically significant correlation was found between macular edema in the active uveitis period and macular damage in the remission period. The reason for this situation may be explained either by the relatively small number of cases or by the effective treatment of the patients in our study.
ERM formation is a pathology caused by a fibrocellular proliferation on the inner surface of the internal limiting membrane. ERM can be either idiopathic or secondary to intraocular inflammation and vitreoretinal disorders. On SD-OCT scans, ERM appears as hyper-reflective line lying on the retinal surface. This complication has been reported in 10 to 30% of patients with Behçet uveitis [19, 20]. In our series, ERM was detected by SD-OCT in 37.1% of eyes in the active period and in 52.9% of eyes in the remission period.
The EZ is at the junction between the photoreceptor outer and inner segments. Disturbed EZ integrity is associated with low visual acuity in retinal diseases. The underlying mechanisms for EZ disturbance in patients with Behçet disease have not been fully elucidated. Ocular Behçet patients suffer from recurrent macular edema attacks due to recurrent uveitis attacks, which may lead to photoreceptor damage. We found EZ damage in 11 of eyes (15.7%) in the active period and in 14 of eyes (20%) in the remission period. Unoki et al. reported that nine eyes (37.5%) with ocular Behçet disease had an absent or an indefinite EZ [6]. They also found a negative correlation between EZ damage and visual acuity. Similarly, in our study, there was a negative correlation between BCVA and EZ damage in both active and remission periods. Yüksel et al. showed that EZ and ELM integrity are impaired in 25% of inactive ocular Behçet patients, and also that EZ integrity was an independent variable factor affecting visual acuity [7]. In a study by Unoki et al., the effect of EZ zone damage and ELM damage on visual acuity was evaluated in Behçet patients in the remission period [6]. They demonstrated a relationship between EZ damage and decreased visual acuity, whereas ELM damage was not associated with visual acuity [6]. All these data have proven that EZ damage negatively affects visual acuity.
Cheng et al. examined the thickness of specific retinal layers and their relationship with visual acuity in patients with Behçet uveitis in remission [21]. They showed that thinning of the outer retinal layers and RPE was observed in long-term Behçet patients [21]. According to our results, in the remission period, SD-OCT findings included ELM damage in 14 (20%) of eyes. Thus, these results have been proven that recurrent attacks of Behçet uveitis affect both inner and outer retinal layers.
Patients with severe vitritis were excluded because of inability to obtain clear SD-OCT images. Although these exclusion criteria might be assumed as a limitation of the study, it was not possible to include these patients due to the design of the study. Also, patients who were lost to follow-up or did not achieve remission were not enrolled due to the design of the study. Excluding the patients who respond poorly to treatment might have the potential to bias the results. However, most of the enrolled patients had already severe uveitis because of the nature of our institution, which is a tertiary referral center. In addition, to avoid biases from enrolling both eyes of a given patient, the linear mixed-effects model (random intercept model) was used to introduce the dependency between the right and left eyes of the same patient [22].
In conclusion, SD-OCT is a very useful diagnostic technique for the evaluation of macular pathologies related to intraocular inflammation in Behçet uveitis. Visual potential and prognostic factors can also be determined by this imaging method. Our findings demonstrate that EZ damage and loss of normal foveal contour appearance were significantly more likely to have adverse effects on visual acuity in Behçet uveitis.
Data availability
Available.
References
Tursen U, Gurler A, Boyvat A (2003) Evaluation of clinical findings according to sex in 2313 Turkish patients with Behçet’s disease. Int J Dermatol 42(5):346–351
Tugal-Tutkun I, Onal S, Altan-Yaycioglu R, Huseyin Altunbas H, Urgancioglu M (2004) Uveitis in Behçet disease: an analysis of 880 patients. Am J Ophthalmol 138(3):373–380
Kim JN, Kwak SG, Choe JY, Kim SK (2017) The prevalence of Behçet’s disease in Korea: data from Health Insurance Review and Assessment Service from 2011 to 2015. Clin Exp Rheumatol 108(6):38–42
Atmaca LS, Sonmez PA (2003) Fluorescein and indocyanine green angiography findings in Behçet’s disease. Br J Ophthalmol 87(12):1466–1468
Cunningham ET Jr, van Velthoven ME, Zierhut M (2014) Spectral-domain-optical coherence tomography in uveitis. Ocul Immunol Inflamm 22(6):425–428
Unoki N, Nishijima K, Kita M, Hayashi R, Yoshimura N (2010) Structural changes of fovea during remission of Behcet’s disease as imaged by spectral-domain optical coherence tomography. Eye 24(6):969–975
Yuksel H, Turkcu FM, Sahin M, Cinar Y, Cingü AK, Ozkurt Z, Sahin A, Ari S, Caça I (2014) Inner and outer segment junction (IS/OS line) integrity in ocular Behcet’s disease. Arq Bras Oftalmol 77(4):219–221
Standardization of Uveitis Nomenclature (SUN) Working Group (2005) Standardization of uveitis nomenclature for reporting clinical data. Results of the first international workshop. Am J Ophthalmol 140(3):509–516
Chajek T, Fainaru M (1975) Behçet's disease. Report of 41 cases and a review of the literature. Medicine (Baltimore) 54(3):179–196
Sakane T, Takeno M, Suzuki N, Inaba G (1999) Behçet's disease. N Engl J Med 341(17):1284–1291
Coskun E, Gurler B, Pehlivan Y, Kisacik B, Okumus S, Yayuspayi R, Ozcan E, Onat AM (2013) Enhanced depth imaging optical coherence tomography findings in Behcet disease. Ocul Immunol Inflamm 21(6):440–445
Kang HM, Koh HJ, Lee SC (2018) Spectral domain optical coherence tomography as an adjunctive tool for screening Behçet uveitis. PLoS One 13(12):e0208254
Omri S, Behar-Cohen F, de Kozak Y, Sennlaub F, Verissimo LM, Jonet L, Savoldelli M, Omri B, Crisanti P (2011) Microglia/macrophages migrate through retinal epithelium barrier by a transcellular route in diabetic retinopathy: role of PKCζ in the Goto Kakizaki rat model. Am J Pathol 179(2):942–953
Klaassen I, Van Noorden CJ, Schlingemann RO (2013) Molecular basis of the inner blood-retinal barrier and its breakdown in diabetic macular edema and other pathological conditions. Prog Retin Eye Res 34:19–48
Ossewaarde-van Norel A, Rothova A (2012) Imaging methods for inflammatory macular edema. Int Ophthalmol Clin 52(4):55–66
Gurlu V, Guclu H, Ozal A (2016) Thickness changes in foveal, macular, and ganglion cell complex regions associated with Behcet uveitis during remission. Eur J Ophthalmol 26(4):347–350
Kahloun R, Yahia SB, Mbarek S, Attia S, Zaouali S, Khairallah M (2012) Macular involvement in patients with Behçet’s uveitis. J Ophthalmic Inflamm Infect 2(3):121–124
Biswas J, Annamalai R, Islam M (2017) Update on clinical characteristics and management of uveitic macular edema. Kerala J Ophthalmol 29(1):4
Öztürk HE, Yücel ÖE, Süllü Y (2017) Vitreomacular interface disorders in Behçet’s uveitis. Turk J Ophthalmol 47(5):261
Amer R, Alsughayyar W, Almeida D (2017) Pattern and causes of visual loss in Behçet's uveitis: short-term and long-term outcomes. Graefes Arch Clin Exp Ophthalmol 255(7):1423–1432
Cheng D, Wang Y, Huang S, Wu Q, Chen Q, Shen M, Lu F (2016) Macular inner retinal layer thickening and outer retinal layer damage correlate with visual acuity during remission in Behcet’s disease. Invest Ophthalmol Vis Sci 57(13):5470–5478
Holopigian K, Bach M (2010) A primer on common statistical errors in clinical ophthalmology. Doc Ophthalmol 121:215–222
Funding
SD-OCT device was supported by the Ankara University Scientific Projects (Project number: 15A0230008).
Author information
Authors and Affiliations
Contributions
F.N.Y and E.T. conceived of the presented idea and planned the study. F.N.Y and E.T. carried out the measurements and analysis. I.K. carried out statistical analysis. F.N.Y and E.T. wrote the manuscript with support from M.Z.Ş. All authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
All procedures performed in the study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yalçındağ, F.N., Temel, E., Şekkeli, M.Z. et al. Macular structural changes and factors affecting final visual acuity in patients with Behçet uveitis. Graefes Arch Clin Exp Ophthalmol 259, 715–721 (2021). https://doi.org/10.1007/s00417-020-04958-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04958-4