Abstract
Purpose
To study the retinal capillary microvasculature and the choriocapillaris (CC) in myopic eyes using swept-source optical coherence tomography angiography (SS-OCTA).
Methods
Patients with high myopia (≥ − 6D; axial length ≥ 26.5 mm), moderate myopia (≥ − 3D, < − 6D), and age-matched healthy subjects presenting to the Shanghai General Hospital and Doheny-UCLA Eye Centers were enrolled in this prospective, multicenter study. Any subjects with evidence of macular abnormalities suggestive of pathologic myopia were excluded. SS-OCTA at both sites was performed using a Zeiss PLEX Elite instrument with a 6 × 6 mm scan pattern centered on the fovea. Two repeated volume scans were acquired for image averaging. The instrument pre-defined en face slab of the superficial and deep retinal capillary microvasculature was used to isolate and display the superficial and deep retinal capillaries. A slab spanning from 21 to 31 μm deep to the RPE fit line was used to isolate and display the CC. The OCTA images were exported for averaging using Image J. Littmann’s method and the Bennett formula were applied to adjust for the impact of magnification in the high and moderate myopia groups. The resultant images were then binarized. Though projection artifact removal software was used, regions below the large superficial retinal vessels were excluded for quantitative analyses of the deep retinal capillary plexus and the CC. Vessel density (VD) and vessel length density (VLD) of the superficial and deep retinal capillary plexus (SCP, DCP) and CC flow deficit (FD) were analyzed, quantified, and compared between different groups.
Results
Twenty-five eyes of 25 patients with high myopia, 25 eyes of 25 patients with moderate myopia, and 25 eyes of 25 normal age-matched controls were included in this study. The VD of the SCP was lower in the high myopia group compared with the emmetropic control groups (p < 0.05), but the VD of the DCP demonstrated no significant difference among the three groups (p > 0.05). The VLDs of the SCP were lower in the high and moderate myopia groups compared with the control group (p < 0.05), while the VLD of the DCP was lower in the high myopia group compared with the moderate myopia and emmetropic control group (p < 0.05). The CC FD% in the high myopia group was significantly greater than both the control and moderate myopia subjects (p < 0.05). Of note, the severity of the CC flow deficit was not correlated with choroidal thickness (p > 0.05).
Conclusion
The retinal microvasculature may demonstrate alterations in highly myopia eyes. The CC in macular regions shows greater impairment in eyes with high myopia compared with eyes with lesser degrees of myopia, and these deficits are already present in the absence of features of pathologic or degenerative myopia. The threshold of CC FD leading to myopic maculopathy remains to be defined.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Myopia is a major cause of vision loss worldwide and has increased significantly in prevalence [1]. There is an epidemic of myopia in East and Southeast Asia, with the prevalence of myopia and high myopia in young adults ranging from 80 to 90% and 10 to 20%, respectively [2]. Myopia is a risk factor for several macular pathologies, such as lacquer crack formation, chorioretinal atrophy, and choroidal neovascularization (CNV), which are associated with retinal and choroidal vascular alterations.
Optical coherence tomography angiography (OCTA) is an important breakthrough imaging technology of the past decade. OCTA has provided unprecedented three-dimensional detail of not only the retinal microcirculation but also the choriocapillaris [3,4,5]. Alterations of the retinal and choroidal circulation are relevant to many macular diseases including myopic maculopathy, and OCTA has provided new insights into the pathophysiology of various retinal diseases.
Using spectral-domain OCT angiography (SD-OCTA) devices, previous studies have demonstrated evidence of various alterations in the retinal microcirculation in highly myopic eyes [6,7,8,9,10]. Al-Sheikh observed that the density of the superficial and deep retinal capillary microvasculature was reduced in the macula of eyes with high myopia [6]. He and colleagues found that both the radial peripapillary and deep parafoveal vessel densities were reduced in eyes with high myopia, but did not find any change in the superficial parafoveal vessel density [7]. Li observed that both the superficial and deep microvascular plexuses were decreased in high myopia eyes, but the retinal microvessel blood flow velocity remained unchanged (as assessed using the Retinal Function Imager) [8]. Milani reported reduced superficial vascular density and increased outer retina flow in eyes with myopia [9]. Although there has been some inconsistency in the relative changes to the superficial vs deep retinal circulations, overall these various investigations have highlighted that the retinal circulation may be impacted by high levels of myopia.
Despite the extensive evaluation of the retinal circulation, there have been relatively few studies evaluating the choriocapillaris (CC) in myopic eyes. Al Sheikh et al. did show an increase in CC flow deficits in highly myopic eyes and also speculated that progressive ectasia and stretching of inter-capillary spaces may have contributed to the findings. As the study did not include subjects with lower levels of myopia, it was not possible to determine if there was a threshold at which quantitative CC alterations became apparent. In addition, the CC assessments were performed using exclusively a SD-OCTA device. SD-OCT may be associated with significant signal sensitivity roll-off with depth, and given that OCTA-based vessel quantification is highly sensitive to signal, this phenomenon could potentially impact quantitative measurement of the CC, particularly in myopic eyes which may feature tilted or off-axis scans. OCTA capability, however, has also been extended to swept source (SS) – OCT devices. These SS-OCT devices feature a longer deeper penetrating wavelength (1050 nm), reduced sensitivity roll-off, and faster scanning speeds which offer some advantages for reliable visualization and quantification of the CC [11, 12].
In the present study, we quantitatively assess the retinal and CC microvasculature in a cohort of eyes with moderate myopia, high myopia, and age-matched emmetropic normal controls using SS-OCTA.
Methods
Setting and participants
This prospective, multicenter study was approved by the Institutional Review Board of the University of California Los Angeles and the ethics committee of Shanghai General Hospital, Shanghai Jiao Tong University, Shanghai, China, and was conducted in accordance with the ethical standards stated in the Declaration of Helsinki. Written informed consent was obtained from all subjects before OCTA imaging.
All participants underwent comprehensive ophthalmic examinations, including refractive error assessment using an autorefractor machine (model KR-8900; Topcon, Tokyo, Japan), intraocular pressure measurement (Full Auto Tonometer TX-F; Topcon), and slit-lamp biomicroscopy. The axial length was measured using the IOL Master (Zeiss 500, Carl Zeiss Meditec, Inc., Dublin, CA).
Subjects were recruited and divided into three groups: the high myopia group was defined by spherical equivalent (SE) refractive error ≥ − 6.0 diopters (D) or axial length ≥ 26.5 mm [13]; moderate myopia group, SE < − 6.0D, but ≥ − 3.0D; and control group, SE < − 3.0D or emmetropia (no hyperopia was allowed). Individuals with any evidence of retinal or choroidal disorders or a history of prior vitreous or retinal surgery which could affect the retinal or choroidal vasculature were excluded from the study. Eyes with lacquer cracks or chorioretinal atrophy due to high myopia or any structural changes, including myopic CNV that could cause shadowing or interfere with assessment of the CC, were excluded from this study. For all three groups, subjects were also required to have no history of previous ocular or systemic diseases or any visual symptoms. Eyes with a history of surgery (including refractive surgery) were excluded from the study.
Image acquisition and scanning protocols
SS-OCTA images were captured using the PLEX Elite 9000 device (Carl Zeiss Meditec Inc., Dublin, CA) and the technical aspects of which have been previously described in detail [14, 15]. This device provides a full-width at half-maximum (FWHM) resolution of approximately 5 μm (axial) in tissue and 14 μm (lateral) on the retinal surface. All subjects were dilated prior to OCTA scanning. Two 6 × 6 mm (500 × 500 A-scans) OCTA scans were acquired centered on the fovea with tracking software engaged to limit motion artifact. This OCT instrument uses the complex optical microangiopathy algorithm (OMAG), which depends on detection of variation in both the amplitude and the phase between successive B-scans acquired at the same location to achieve motion contrast to generate the OCTA image. OCTA scans were repeated until two sufficient quality scans (signal strength ≥ 7, no evidence of motion artifact) were obtained. If both eyes were eligible for the study, only one eye was randomly selected for inclusion in these analyses.
The instrument software’s automatic segmentation was used to generate en face projection images of the superficial retinal capillary plexus (SCP), deep retinal capillary plexus (DCP), and the CC. All segmentation boundaries (all B-scans) were inspected, and manual correction was performed on any B-scans demonstrating segmentation errors. Of note, the CC en face OCTA image was obtained from a 10-μm slab offset, 21μm deep to the RPE fit line, using the maximum projection setting. The manufacturer’s projection removal software was engaged to remove residual artifact from the overlying retinal circulation.
Image processing
After confirmation of proper segmentation, the en face images from the SCP, DCP, and CC were exported from the PLEX Elite software and then imported into the freely available FIJI software (an expanded version of ImageJ version 1.51a; fiji.sc).
As the image magnification would expect to be impacted in these myopic eyes, we adjusted the image size in the high and moderate myopia groups according to each individual axial length using Littmann’s method and the Bennett formula [16, 17]. To optimize visualization of the CC, the en face images from two acquisitions were registered and averaged using the approach previously reported by Uji et al. [18, 19].
After correction of magnification and averaging, the DCP, SCP, and CC images were binarized using a modified version of the previously reported method [20]. Briefly, the images were duplicated in order to apply two binarization methods. One image was processed first by a Hessian filter, followed by global thresholding using Huang’s fuzzy thresholding method. The other (duplicate) image was binarized using median local thresholding. Finally, the two different binarized images were combined to generate the final binarized image in which only pixels that existed on both binarized images were included.
Although projection artifact removal was applied, the DCP and CC directly under superficial large retinal vessels were excluded from quantitative analysis to avoid the confounding effect from residual projection artifact in accordance with the approach reported by Borrelli et al. [20]. Using the binarized SCP images, the MaxEntropy threshold was applied to visualize only the large superficial retinal vessels. The obtained thresholded images were then merged with binarized DCP and CC images using FIJI software for identification and removal of the superficial retinal large vessels.
Vessel density (VD) was assessed on this final resultant image (after averaging and masking of superficial large vessels) and defined as the ratio of the area occupied by vessels divided by the total assessable (i.e., no overlying superficial large retinal vessels) area. After skeletonization of the image, vessel length density (VLD), which represents the vessel length per unit area, was evaluated as described previously [18,19,20,21,22].
In the CC analysis, CC flow deficits were measured using the Phansalkar method (radius, 23.44 μm) as described previously [18, 23, 24]. The percentage of flow deficits (FD %) was calculated as percentage of the resulting area using the “Analyze Particles” command. Analysis was completed by two certified, independent Doheny Image Reading Center OCTA graders (LS, NTT), and inter-grader analysis was performed to validate the measurements.
Choroidal thickness (in microns) was analyzed using the cross-sectional OCT B-scan of the Plex Elite instrument and measured from Bruch’s membrane to the choroid-sclera interface at the foveal center using the caliper tool in the instrument software. The measurement was carried out by two certified, independent Doheny Image Reading Center OCTA graders (LS, NTT), and inter-grader analysis was performed.
Statistical analysis
Statistical analyses were performed using SPSS Statistics version 20 (IBM, Armonk, NY). To detect differences in VD, VLD for the SCP and DCP, flow deficit in CC, axial length, spherical equivalent, and choroidal thickness among the three groups, one-way ANOVA was performed. Post hoc tests with Bonferroni correction were used to determine the presence of pairwise differences between different groups. The inter-grader reproducibility was assessed using intraclass correlation coefficient. A p value < 0.05 was considered statistically significant.
Results
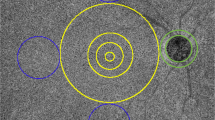
The study cohort consisted of 25 high myopic eyes (25 subjects), 25 moderate myopic eyes (25 subjects), and 25 healthy control eyes (25 subjects). The demographic data for the various groups in this cohort is shown in Table 1. There were no significant differences in age or gender among these groups (p > 0.05). There were significant differences in axial length and spherical equivalent among these groups (p < 0.05). The mean subfoveal choroidal thickness was 174.48 ± 75.19 μm (range 45–387 μm) in the high myopia group, 256.32 ± 95.01 μm (range 108–482 μm) in the moderate myopia group, and 360.76 ± 110.16 μm (range 216–662 μm) in the control group. The subfoveal choroidal thickness was statistically significantly different among the three groups (p < 0.05). As noted in the Methods, to overcome the magnification bias, the en face images in the high and moderate myopia groups were corrected with Littmann’s method and the Bennett formula (Fig. 1).
Examples of magnification correction using Littmann’s method and the Bennett formula, F = 3.48 × 0.01306 × (AL – 1.82). F represents the magnification factor, and AL represents axial length. a En face image of superficial vasculature of an eye with AL of 26.71 mm in the high myopia group. b En face image of superficial vasculature of an eye with AL of 26.07 mm in the moderate myopia group. The yellow square represents the actual image size that corresponds to 6 × 6 mm
The mean VD and VLD in the SCP and DCP in the total 6 × 6 mm scan are shown in Table 2. The VD of the SCP was lower in the high myopia group compared with the emmetropic control groups (p < 0.05), but the VD of the DCP demonstrated no significant difference among the three groups (p > 0.05). The VLDs of the SCP were lower in the high and moderate myopia groups compared with the control group (p < 0.05), while the VLD of the DCP was lower in the high myopia group compared with the moderate myopia and emmetropic control group (p < 0.05).
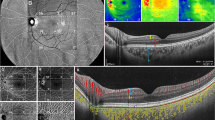
For the CC, the percentage of flow deficits (FD %) was 25.98 ± 2.24 in the high myopia group, 24.09 ± 2.88 in the moderate myopia group, and 23.98 ± 2.26 in the control group (Table 3, Fig. 2), which was significantly different (p < 0.05). In particular, the CC FD in the high myopia group was significantly higher compared to both the control group and the moderate myopia group (p < 0.05). However, there was no significant difference in the CC FD between the normal and moderate myopia eyes (p > 0.05). Of note, although there was a trend for a more extensive CC FD to be associated with a thinner choroid, CC FD was not significantly correlated with choroidal thickness (p = 0.172).
Three cases (one from each group) illustrating the final masked choriocapillaris en face image, after magnification correction, averaging, and binarization, used to calculate the area of choriocapillaris (CC) flow deficit percentage. a The final CC en face image of a 38-year-old male subject with high myopia. Axial length was 26.71 mm, and area of flow deficit was 29.18%. b The final CC en face image of a 32-year-old female subject with moderate myopia. Axial length was 26.07 mm, and area of flow deficit was 22.29%. c The final CC en face image of a 35-year-old male subject without myopia. Axial length was 23.13 mm, and area of flow deficit was 21.13%
The intraclass correlation coefficient (ICC) between the two graders was 0.95 (95% confidence interval (CI), 0.85–0.98) for choroidal thickness and 0.99 (95% CI, 0.98–0.99) for CC FD.
Discussion
In this study, using swept-source OCT angiography, we observed that the severity of CC flow deficits in eyes with high myopia was significantly greater compared to both normal eyes and eyes with moderate myopia. The VLDs of SCP were also lower in both high and moderate myopia groups compared with the emmetropic control group, and the VLD of the DCP was lower in the high myopia group compared to both the other groups. The VD of the SCP was also lower in the high myopia group, but the VD of the DCP demonstrated no significant difference among the three groups.
Our CC findings are consistent with previous studies using SD-OCT angiography and other techniques. Al-Sheikh reported the area of flow deficit in the CC was increased in eyes with pathologic high myopia by using spectral-domain OCT angiography [6]. Using scanning electron microscopy, Hirata noted that the density of CC decreased in myopic chick eyes [25]. Shih reported that choroidal blood flow was reduced in chicks with goggle-induced myopia using laser Doppler velocimetry [26]. Interestingly, our study would appear to suggest that changes in the CC are only observed after a certain level of ectasia or progressive myopia is achieved, as individuals with only moderate myopia did not manifest changes to the macular CC. There was a trend for a decrease in macular CC in the moderate myopic group however that may not have been significant due to the power of the study. Importantly, we observed that more CC flow deficits were observed in these high myopic eyes without any other pathologic alterations (e.g., atrophy, CNV) present. Assuming CC flow deficits would be worse in eyes with findings of degenerative myopia such as chorioretinal atrophy, one might speculate that progressive CC flow deficit may be a key feature in the evolution and pathophysiology of pathologic myopia. Although the CC flow deficit appears to be greater in these more myopic eyes, we cannot exclude that these CC abnormalities may be a result of simple ectasia or stretching of the CC rather than a true loss of atrophy of the CC. Regardless of the mechanisms, one might anticipate that greater spacing between the CC capillaries may mean less surface area for metabolic exchange with the overlying RPE and photoreceptors. However, it is important to emphasize that this is only a hypothesis at this stage that requires prospective longitudinal studies for validation. Nonetheless, this concept would appear to be consistent with the central role of the CC established in other macular diseases. For example, it is now well established that the central macular CC shows progressive increase in flow deficits with age [27, 28]. These CC flow deficits have been also shown to predict the future development of drusen, nascent geographic atrophy, and the enlargement rate of atrophy [20, 29,30,31]. As CC flow deficits are also noted adjacent to CNV lesions, CNV has been proposed as a potential pathologic response attempting to compensate for progressive CC dysfunction [4, 14, 32]. Progressive CC dysfunction may play a similar role in myopia, stimulating the development of CNV and contributing to the eventual development of atrophy. Partially supporting this hypothesis is the observation that the choroid is thinner in myopic eyes that develop CNV compared to those which do not [33]. Sayanagi et al. found that the CC features appeared to differ depending on the specific manifestation of myopic maculopathy. For example, in the lacquer crack formation process, breaks in Bruch’s membrane and the RPE were suggested to precede the diminution of the CC [34]. Lacquer cracks, however, may represent an acute and localized process which may be distinct from a global diffuse worsening of the CC FD which may occur with progressive ectasia. Regardless, prospective longitudinal studies will be required to further clarify the pathophysiology and progression on CC impairment in myopia and myopic maculopathy.
In our study, there was no statistically significant correlation between choroidal thickness and CC flow deficit despite the presence of a correlative trend. Although our study may have been underpowered to find a weak correlation, this finding suggests that the choroidal thickness alone cannot serve as a surrogate for the CC FD. This finding may also explain why some subjects with myopia can tolerate an extremely thin choroid without significant functional compromise [35]. It may be that if the CC can stay relatively intact despite overall choroidal thinning, the overlying RPE and retina can be adequately supported.
The threshold of posterior pole ectasia and choroidal thinning before CC alterations become apparent, and the tipping point at which these CC alterations result in pathologic alterations to the outer retina remains to be defined. In our study, quantitative CC alterations could not be observed in eyes with moderate myopia suggesting that these eyes are positioned below this threshold. Future studies with larger, longitudinal data will be required to provide further clarity on this issue. Of note, similar to previous studies, we did confirm a thinner choroid in myopic eyes compared to emmetropic eyes [36, 37].
Although it was not the main objective of our study, we were also able to evaluate the superficial and deep retinal vasculature. Using the 6 × 6 mm scan pattern, we observed that the VLD’s of the SCP decreased in both the high and moderate myopia groups compared with the control group. And the VLD of DCP was decreased in the high myopia group compared to the other two groups. The VD of the SCP decreased in the high myopia group, but the VD of the DCP demonstrated no significant difference among the three groups. Using a 3 × 3 scan pattern, Al Sheik et al. also found a reduced retinal capillary density in both the superficial and deep retinal capillary plexus [6]. He et al. found no difference in the superficial plexus in high myopic eyes using a similar 6 × 6 scan pattern (albeit with a different OCTA instrument); however, they found a reduction in vessel density in the deep plexus [7]. While the reason for the apparent discrepancies among these studies cannot be established definitely, it may be related to different instruments (SS vs SD-OCTA), different OCTA algorithms, different segmentation, and differences in processing (e.g., use of averaging). Garrity et al. found that 3 × 3 mm scans were more repeatable and likely more accurate than the 6 × 6 mm scans and the SCP was more accurate than the DCP in healthy eyes using the RTVue SD-OCTA [38, 39]. Future studies in myopic eyes with different devices and scan patterns may more precisely elucidate the cause for these differences. Regardless, taken as a whole, these studies would suggest that the retinal microvasculature may be impacted by myopia which is not surprising given the progressive ectasia evident in these eyes.
Our study does have some limitations which should be considered in assessing our results. First, our sample size is relatively small. As a result, we may have been underpowered to detect smaller differences in CC flow deficit between the control and moderate myopia groups. On the other hand, the clinical significance of such small differences in CC flow deficit are uncertain. Second, while we did include patients with high myopia, we excluded patients with clinical evidence of myopic maculopathy or pathologic myopia. Thus, we were not able to assess and compare the CC in these patients with more advanced disease. Third, although we used the instrument projection removal function and took the extra precaution of excluding regions underlying large superficial vessels (a method reported by Borrelli et al. [20]), there may be other artifacts specific to myopic eyes which may be difficult to fully account for. For example, Dolz-Marco and colleagues demonstrated that directional changes in Henle fiber reflectivity might impact flow detection on OCTA, which may be particularly problematic in elongated eyes where retina may be tilted or non-perpendicular to the OCT scan beam in some locations [40]. Methods to compensate for such tilting effects are still forthcoming. Our study also has several strengths including its prospective design, the use of deeper penetrating SS-OCTA which may have some advantages for visualization and quantification of the CC, standardized imaging protocols, image averaging, magnification correction for high and moderate groups, and use of certified image reading center graders.
In summary, using SS-OCTA, we observed retinal microvascular network alterations and increased CC flow deficits in highly myopic eyes compared to eyes with moderate myopia or normal controls. The relevance of the CC to the pathophysiology of high myopia warrants further study.
References
Fricke TR, Jong M, Naidoo KS, Sankaridurg P, Naduvilath TJ, Ho SM, Wong TY, Resnikoff S (2018) Global prevalence of visual impairment associated with myopic macular degeneration and temporal trends from 2000 through 2050: systematic review, meta-analysis and modelling. Br J Ophthalmol 102:855–862
Morgan IG, French AN, Ashby RS, Guo X, Ding X, He M, Rose KA (2018) The epidemics of myopia: aetiology and prevention. Prog Retin Eye Res 62:134–149
Spaide RF, Fujimoto JG, Waheed NK, Sadda SR, Staurenghi G (2018) Optical coherence tomography angiography. Prog Retin Eye Res 64:1–55
Borrelli E, Sarraf D, Freund KB, Sadda SR (2018) OCT angiography and evaluation of the choroid and choroidal vascular disorders. Prog Retin Eye Res 67:30–55
Kashani AH, Chen CL, Gahm JK, Zheng F, Richter GM, Rosenfeld PJ, Shi Y, Wang RK (2017) Optical coherence tomography angiography: a comprehensive review of current methods and clinical applications. Prog Retin Eye Res 60:66–100
Al-Sheikh M, Phasukkijwatana N, Dolz-Marco R, Rahimi M, Iafe NA, Freund KB, Sadda SR, Sarraf D (2017) Quantitative OCT angiography of the retinal microvasculature and the choriocapillaris in myopic eyes. Invest Ophthalmol Vis Sci 58:2063–2069
He J, Chen Q, Yin Y, Zhou H, Fan Y, Zhu J, Zou H, Xu X (2019) Association between retinal microvasculature and optic disc alterations in high myopia. Eye (Lond) 33:1494–1503
Li M, Yang Y, Jiang H, Gregori G, Roisman L, Zheng F, Ke B, Qu D, Wang J (2017) Retinal microvascular network and microcirculation assessments in high myopia. Am J Ophthalmol 174:56–67
Milani P, Montesano G, Rossetti L, Bergamini F, Pece A (2018) Vessel density, retinal thickness, and choriocapillaris vascular flow in myopic eyes on OCT angiography. Graefes Arch Clin Exp Ophthalmol 256:1419–1427
Yang Y, Wang J, Jiang H, Yang X, Feng L, Hu L, Wang L, Lu F, Shen M (2016) Retinal microvasculature alteration in high myopia. Invest Ophthalmol Vis Sci 57:6020–6030
Al-Sheikh M, Falavarjani KG, Tepelus TC, Sadda SR (2017) Quantitative comparison of swept-source and spectral-domain OCT angiography in healthy eyes. Ophthalmic Surg Lasers Imaging Retina 48:385–391
Miller AR, Roisman L, Zhang Q, Zheng F, Rafael de Oliveira Dias J, Yehoshua Z, Schaal KB, Feuer W, Gregori G, Chu Z, Chen CL, Kubach S, An L, Stetson PF, Durbin MK, Wang RK, Rosenfeld PJ (2017) Comparison between spectral-domain and swept-source optical coherence tomography angiographic imaging of choroidal neovascularization. Invest Ophthalmol Vis Sci 58:1499–1505
Ohno-Matsui K (2017) What is the fundamental nature of pathologic myopia. Retina 37:1043–1048
Alagorie AR, Verma A, Nassisi M, Sadda SR (2019) Quantitative assessment of choriocapillaris flow deficits in eyes with advanced age-related macular degeneration versus healthy eyes. Am J Ophthalmol 205:132–139
Bo Q, Yan Q, Shen M, Song M, Sun M, Yu Y, Rosenfeld PJ, Wang F, Sun X (2019) Appearance of polypoidal lesions in patients with polypoidal choroidal vasculopathy using swept-source optical coherence tomographic angiography. JAMA Ophthalmol 137:642–650
Wen C, Pei C, Xu X, Lei J (2019) Influence of axial length on parafoveal and peripapillary metrics from swept source optical coherence tomography angiography. Curr Eye Res 44:980–986
Bennett AG, Rudnicka AR, Edgar DF (1994) Improvements on Littmann’s method of determining the size of retinal features by fundus photography. Graefes Arch Clin Exp Ophthalmol 232:361–367
Uji A, Balasubramanian S, Lei J, Baghdasaryan E, Al-Sheikh M, Sadda SR (2017) Choriocapillaris imaging using multiple en face optical coherence tomography angiography image averaging. JAMA Ophthalmol 135:1197–1204
Uji A, Balasubramanian S, Lei J, Baghdasaryan E, Al-Sheikh M, Sadda SR (2017) Impact of multiple en face image averaging on quantitative assessment from optical coherence tomography angiography images. Ophthalmology 124:944–952
Borrelli E, Uji A, Sarraf D, Sadda SR (2017) Alteration in the choriocapillaris in intermediate age-related macular degeneration. Invest Ophthalmol Vis Sci 58:4792–4798
Kim AY, Chu Z, Shahidzadeh A, Wang RK, Puliafito CA, Kashani AH (2016) Quantifying microvascular density and morphology in diabetic retinopathy using spectral-domain optical coherence tomography angiography. Invest Ophthalmol Vis Sci 57:OCT362–OCT370
Reif R, Qin J, An L, Zhi Z, Dziennis S, Wang R (2012) Quantifying optical microangiography images obtained from a spectral domain optical coherence tomography system. Int J Biomed Imaging 2012:509783
Spaide RF (2017) Choriocapillaris signal voids in maternally inherited diabetes and deafness and in pseudoxanthoma elasticum. Retina 37:2008–2014
Spaide RF (2016) Choriocapillaris flow features follow a power law distribution: implications for characterization and mechanisms of disease progression. Am J Ophthalmol 170:58–67
Hirata A, Negi A (1998) Morphological changes of choriocapillaris in experimentally induced chick myopia. Graefes Arch Clin Exp Ophthalmol 236:132–137
Shih YF, Fitzgerald ME, Reiner A (1993) Choroidal blood flow is reduced in chicks with ocular enlargement induced by corneal incisions. Curr Eye Res 12:229–237
Zheng F, Zhang Q, Shi Y, Russell JF, Motulsky EH, Banta JT, Chu Z, Zhou H, Patel NA, de Sisternes L, Durbin MK, Feuer W, Gregori G, Wang R, Rosenfeld PJ (2019) Age-dependent changes in the macular choriocapillaris of normal eyes imaged with swept-source optical coherence tomography angiography. Am J Ophthalmol 200:110–122
Nassisi M, Baghdasaryan E, Tepelus T, Asanad S, Borrelli E, Sadda SR (2018) Topographic distribution of choriocapillaris flow deficits in healthy eyes. PLoS One 13(11):e0207638
Nassisi M, Shi Y, Fan W, Borrelli E, Uji A, Ip MS, Sadda SR (2019) Choriocapillaris impairment around the atrophic lesions in patients with geographic atrophy: a swept-source optical coherence tomography angiography study. Br J Ophthalmol 103:911–917
Nassisi M, Baghdasaryan E, Borrelli E, Ip M, Sadda SR (2019) Choriocapillaris flow impairment surrounding geographic atrophy correlates with disease progression. PLoS One 14(2):e0212563
Nassisi M, Tepelus T, Nittala MG, Sadda SR (2019) Choriocapillaris flow impairment predicts the development and enlargement of drusen. Graefes Arch Clin Exp Ophthalmol 257:2079–2085
Borrelli E, Souied EH, Freund KB, Querques G, Miere A, Gal-Or O, Sacconi R, Sadda SR, Sarraf D (2018) Reduced choriocapillaris flow in eyes with type 3 neovascularization and age-related macular degeneration. Retina. 38:1968–1976
El Matri L, Bouladi M, Chebil A, Kort F, Bouraoui R, Largueche L, Mghaieth F (2012) Choroidal thickness measurement in highly myopic eyes using SD-OCT. Ophthalmic Surg Lasers Imaging 43:S38–S43
Sayanagi K, Ikuno Y, Uematsu S, Nishida K (2017) Features of the choriocapillaris in myopic maculopathy identified by optical coherence tomography angiography. Br J Ophthalmol 101:1524–1529
Pang CE, Sarraf D, Freund KB (2015) Extreme choroidal thinning in high myopia. Retina. 35(3):407–415
Nishida Y, Fujiwara T, Imamura Y, Lima LH, Kurosaka D, Spaide RF (2012) Choroidal thickness and visual acuity in highly myopic eyes. Retina 32:1229–1236
Ho M, Liu DT, Chan VC, Lam DS (2013) Choroidal thickness measurement in myopic eyes by enhanced depth optical coherence tomography. Ophthalmology 120:1909–1914
Garrity ST, Iafe NA, Phasukkijwatana N, Chen X, Sarraf D (2017) Quantitative analysis of three distinct retinal capillary plexuses in healthy eyes using optical coherence tomography angiography. Invest Ophthalmol Vis Sci 58(12):5548–5555
Iafe NA, Phasukkijwatana N, Chen X, Sarraf D (2016) Retinal capillary density and foveal avascular zone area are age-dependent: quantitative analysis using optical coherence tomography angiography. Invest Ophthalmol Vis Sci 57(13):5780–5787
Dolz-Marco R, Freund KB (2018) Directional changes in tissue reflectivity may influence flow detection on optical coherence tomography angiography. Retina. 38:739–747
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Li Su: none, Yong-Sok Ji: none, Nianting Tong: none, David Sarraf: Amgen (C, F), Bayer (C, F), Genentech (C, F), Heidelberg (F), Novartis (C, F), Regeneron (F), Optovue (C, F), Topcon (F)Xiangui He: none, Xiaodong Sun: none, Xun Xu: none, SriniVas R. Sadda: Genentech (C), Allergan (C), Novartis (C), 4DMT (C), Oxurion (C), Optos (C, F), Heidelberg (C, F), Carl Zeiss Meditec (F), Centervue (C,), Topcon (C), Amgen (C).
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Su, L., Ji, YS., Tong, N. et al. Quantitative assessment of the retinal microvasculature and choriocapillaris in myopic patients using swept-source optical coherence tomography angiography. Graefes Arch Clin Exp Ophthalmol 258, 1173–1180 (2020). https://doi.org/10.1007/s00417-020-04639-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04639-2