Abstract
Purpose
The purpose of our study was to assess the changes in ocular parameters for different accommodative demands using a new optical biometer based on swept-source optical coherence tomography (SS-OCT).
Methods
Seven subjects were included in this pilot study, and only one eye per participant was analyzed. Each eye was measured six times with the optical biometer IOLMaster 700 (Carl Zeiss Meditec, Jena, Germany). As this instrument is not able to change the vergence of the stimulus, to enable measurements at different accommodative states, a tilted first-surface mirror attached to the optical biometer was used to place the fixation stimulus at different vergences. Measurements were taken on the right eye of the subject while the left eye was looking through the mirror. Central corneal thickness (CCT), anterior chamber depth (ACD), lens thickness (LT), axial length (AL), white-to-white (WTW) distance and keratometric readings were evaluated for three different accommodative states: 0.0 diopters (D), 1.5 D, and 3.0 D.
Results
No statistically significant differences were found for CCT, AL, WTW, K1 and K2 between the three accommodative states. As expected, changing the accommodative condition did not change CCT, AL, WTW, and keratometric outcomes. Nevertheless, statistically significant differences between the accommodative states were found for ACD and LT measurements. In addition, variations in ACD correlated linearly with variations in LT (R2 ≥ 0.99) when changing the vergence of the optotype.
Conclusion
A practical methodology to assess the changes in ocular parameters for different accommodative demands using the IOLMaster 700 based on SS-OCT has been described. Statistically significant changes that have been found that agree well with previous reports.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The measurement and characterization of ocular anatomic parameters has become increasingly important in ophthalmic practice. The diagnosis and treatment of ocular diseases need reliable descriptions of these parameters, such as central corneal thickness (CCT), anterior chamber depth (ACD), crystalline lens thickness (LT), and eye axial length (AL). In addition to these axial measurements, other ocular parameters like keratometry readings (K1-K2) and white-to-white (WTW) distances are sometimes needed. Some of these parameters are important in clinical settings, for instance for calculating phakic or pseudophakic intraocular lens (IOL) power and diameter, or for research purposes such as studying myopia progression control, among others.
Although in the past ultrasound biometry was the main technology used for obtaining these parameters, optical biometers based on infrared interferometry have replaced ultrasound techniques. In this sense, infrared optical biometry is nowadays a widespread non-contact technology for measuring and characterizing ocular parameters in-vivo [1]. Different types of optical biometers based on different optical technologies for ocular biometry measurement may be found in the market. Recently, the novel optical biometer IOLMaster 700, developed by Carl Zeiss Meditec, has been released. The IOLMaster 700 uses swept-source optical coherence tomography (SS-OCT) to generate several optical B-scans (cross-sections) to determine the biometric data of the eye. This device has recently shown an excellent repeatability and reproducibility results [2,3,4].
Some of the ocular anatomic parameters change depending on the accommodation state of the patient, and these changes have been measured and reported in previous studies [5,6,7,8,9]. The crystalline lens is the main optical structure involved in the accommodation process, as it is able to modify its shape as a response to a near stimulus to focus a clear image on the retina.
The IOLMaster 700 optical biometer measures ocular parameters while the patient is fixating a light point source inside the instrument. In those patients with active accommodation, this non-accommodative target used to facilitate fixation may affect their accommodation state. In these cases, it might be interesting to know the accommodative state of the patient to be able to correlate it with the measured ocular parameters. Besides, the possibility of modifying at will the accommodative demand of the patient being measured with this device could be interesting for research purposes.
The aim of the present study is to describe a methodology to assess the changes in ocular parameters for different accommodative demands using the IOLMaster 700. Changes in ocular parameters are measured for different accommodative states when an accommodative stimulus is presented to the eye at different vergences. This will make it possible to observe in a non-invasive way the main changes in the eye parameters during accommodation by means of SS-OCT technology.
Methods
Subjects
This pilot study included seven emmetropic subjects with healthy and phakic eyes. Only one eye per participant was included in order not to artificially reduce the confidence interval around the limits of agreement [10]. All the subjects underwent a complete eye examination, including refraction, screening for ocular and systemic diseases, and slit-lamp biomicroscopy. All the subjects were free of any ocular pathologic conditions, showed a photopic pupil diameter greater than 3.0 mm and had best-corrected monocular decimal visual acuity of 20/20 (0.0 logMAR). Exclusion criteria included tear film abnormality, amblyopia and/or strabismus, history of ocular surgery or inflammation. All patients provided written informed consent after the nature and possible consequences of the study were explained fully in accordance with the Declaration of Helsinki. Institutional review board approval was obtained.
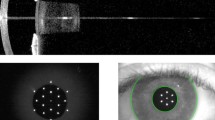
Optical biometer
The IOLMaster 700 is an optical biometry device, based on SS-OCT technology, for measuring different distances in the eye along the visual axis. It obtains measurements of the AL, ACD, CCT, LT, WTW, and K1 and K2 readings. The device acquires six measurements for each of the various eye parameters and presents an average value per triggered measurement. The device enables a 44 mm scan depth with 22 μm resolution in tissue. The speed of the length measurement system allows acquisition of full-eye length tomograms at 2000 A-scans/s.
Experimental procedure
One skilled operator was involved in the experimental procedure, which took place at the Grupo de Investigación en Optometría Laboratory (University of Valencia, Valencia, Spain).
This SS-OCT instrument uses a red light point source inside the equipment as a fixation stimulus, and there is no option for changing the vergence of the stimulus. To enable measurements at different accommodative states, a tilted first-surface mirror (5 cm diameter) was used to place the fixation stimulus at different vergences. The tilted mirror was attached to the optical biometer, and placed in front of the left eye of the patient while the right eye was viewing normally through the IOLMaster 700 (see Fig. 1). Measurements were taken on the right eye of the subject while the left eye was looking through the mirror. The tilting angle of the mirror was adjusted for every patient depending on the particular interpupillary distance. To facilitate this task, the mirror was attached to the optical biometer by means of a reusable putty-like pressure-sensitive adhesive (Blu Tack, Bostik smart adhesives, Milwaukee, WI, USA). Subjects were instructed to look through the mirror at an optotype that was placed at the required distance depending on the vergence tested. This optotype was mounted on an optical rail to allow its repositioning at the appropriate distance. Optical alignment of the displacement axis for changing the vergence of the stimulus was initially performed. The optotype consisted of standard Sloan letters of different size. To ensure that patients where accommodating to the right distance, they were asked to clearly focus those letters of the optotype requiring decimal visual acuity of 1.0 during data acquisition. Subjects were also instructed to look at the target during the measurements and to relax between measurements. Figure 2 shows some pictures of the experimental setup, including the optical rail used to place the optotype at the required distance depending on the vergence tested, and the first surface mirror attached to the optical biometer.
Measurements were taken for three different conditions. In each of them, the left eye of the patient was always looking through the tilted mirror at the optotype placed at different distances: infinity, 67 cm, and 33 cm. These distances correspond, respectively, to the following vergences measured in diopters (D): 0.0 D, 1.5 D, 3.0 D (note that for the sake of simplicity all vergences were taken as positive values). Figure 3 shows SS-OCT images obtained for one of the subjects for the 0.0 D (upper part) and 3.0 D (lower part) vergence conditions. For each subject and each of the three accommodative conditions, six consecutive measurements were taken. Each measurement was taken 4 s after the subject’s last blink to allow the tear film to spread over the cornea [11], and blinking was not permitted during the image acquisition. No other examinations or measurements of the eye involving contact were conducted on the same day prior to the start of measurements with the optical biometer.
Statistical analysis
The results were evaluated using SPSS software v.22 (IBM Corp., Armonk, NY, USA). A repeated measures analysis of variance (rANOVA) was performed to reveal significant differences among conditions for each of the parameters taken with the device. The normality of all data sets was evaluated by means of the Shapiro-Wilk test. The ANOVA procedure based on the F statistic is robust under the breach of the normality assumption, provided that the data samples have no important asymmetries or similar distribution shapes [12]. Prior to the rANOVA the sphericity assumption was checked using the Mauchly’s sphericity test. The Greenhouse-Geisser correction was applied in those cases in which the sphericity test was not statistically significant [13]. The Bonferroni procedure was used as a post hoc test for comparisons between data groups when the rANOVA revealed significant differences between measurements. This method allows for obtaining the significance level for paired differences between the individual conditions. The statistical significance limit was set to p < 0.05 in all cases.
Results
A total of seven eyes of seven subjects (six male and one female) were included in the study. Average age of the sample was 34.9 ± 5.9 years (range: 26 to 41 years). All subjects completed the whole experiment, and all ocular measurements were taken correctly.
Anterior chamber depth and lens thickness
The ACD boxplots for each accommodative condition (optotype placed at 0.0 D, 1.5 D and 3.0 D of vergence) are shown in Fig. 4a (note that the drawn whiskers in the boxplots display the full range of variation, i.e., from the minimum to the maximum values in the distribution). The rANOVA procedure revealed statistically significant differences in ACD between the three data groups (p < 0.001). Post hoc tests for multiple comparisons using the Bonferroni procedure revealed statistical significant differences for all paired comparisons. Therefore, ACD changed with statistical significance when focusing the optotype at the three different vergences. Mean ACD was reduced 60 μm, when the accommodation changed between 0.0 D and 1.5 D, while the reduction was around 100 μm when changing from 1.5 D to 3.0 D.
(a) ACD boxplots for each accommodative condition: optotype placed at 0.0 D, 1.5 D and 3.0 D of vergence. (b) LT measurements for each vergence condition. Note that the drawn whiskers in the boxplots display the full range of variation, i.e., from the minimum to the maximum values in the distribution
Figure 4b shows the results obtained for the LT measurements and for the three conditions. The rANOVA procedure revealed statistically significant differences between the three data groups corresponding to LT results (p < 0.001). Bonferroni post hoc tests revealed statistical significant differences for all the LT paired comparisons. Mean LT was increased 66 μm, when changing the accommodation from 0.0 D to 1.5 D, while the increase was around 106 μm, when accommodating from 1.5 D to 3.0 D.
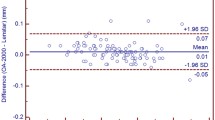
Figure 5 shows the correlation obtained between ACD and LT for all subjects enrolled in the study. Variations in ACD correlated linearly with variations in LT (R2 ≥ 0.99) when changing the vergence of the optotype. The rate of variation was different for each subject, with values ranging from −0.774 to −1.167 mm change in ACD per mm change in LT.
Central corneal thickness and axial length
CCT outcomes for each vergence condition are shown in Fig. 6a. In this case, the rANOVA procedure did not reveal statistically significant differences between the three data groups (p > 0.05). Figure 6b shows the results obtained for AL variations at the three different vergence conditions. As with CCT, differences found between the three different accommodative conditions were not statistically significant (p > 0.2). Therefore, changing the accommodative condition did not change, as expected, the CCT and the AL outcomes.
(a) CCT boxplots for each accommodative condition: optotype placed at 0.0 D, 1.5 D and 3.0 D of vergence. (b) AL measurements for each vergence condition. Note that the drawn whiskers in the boxplots display the full range of variation, i.e., from the minimum to the maximum values in the distribution
White-to-white distance and Keratometric readings
Figure 7a shows the changes measured in WTW distance for the three accommodative conditions. No statistically significant differences were found between the three data groups (p > 0.5). The mean keratometric readings (K1 and K2) for the three vergence conditions are shown in Fig. 7b. There were not statistically significant changes between the three conditions, either for K1 or for K2, as rANOVA showed (p > 0.05). As expected, changes in the accommodation state did not alter WTW and keratometric outcomes.
(a) WTW boxplots for each accommodative condition: optotype placed at 0.0 D, 1.5 D and 3.0 D of vergence. Note that the drawn whiskers in the boxplot display the full range of variation, i.e., from the minimum to the maximum values in the distribution. (b) Keratometric readings K1 and K2 (mean ± standard deviation) for each vergence condition
Discussion
The aim of the present study was to describe a methodology to assess the changes in ocular parameters for different accommodative demands using the IOLMaster 700 based on SS-OCT technology. Changes in ocular parameters (CCT, ACD, LT, AL, WTW and keratometric readings) were measured for different accommodative states, when an accommodative stimulus was presented to the eye at different vergences. The IOLMaster 700 was not designed to measure ocular parameters at different accommodative demands. Therefore, the instrument has no possibility of changing the vergence of the stimulus presented to the eye. Nevertheless, the simple methodology described here may help clinicians to use this optical device to assess the changes in ocular parameters for different accommodative demands. OCT image acquisition is also fast and noninvasive, which is a practical advantage for patients and clinicians.
Accommodation occurs through changes in the shape and thickness of the crystalline lens. According to the classic theory of accommodation from Helmholtz and Fincham and other experimental findings [14], during near vision these changes are induced by the contraction of the ciliary muscle, which causes the release of the zonular fibers anchored to the equator of the crystalline lens [15]. The thickness and the curvature of the lens increase, causing an increase in the eye’s refractive power. Because it is a muscle-induced activity, accommodation is a highly fluctuant and dynamic process.
The resolution of various techniques available for imaging and measuring ocular parameters varies widely, with the best having a value of approximately 5 to 15 μm [16]. Regarding OCT, over the past years this technique has found a wide range of biomedical applications, including imaging of the human cornea in healthy and diseased patients [17]. Time-domain OCT has been used to perform biometry of the anterior segment for different static degrees of accommodation and in eyes of patients of different ages [15] using low image resolution and limited axial range. The imaging speed of time-domain OCT technology is relatively low. The more recent Fourier-domain OCT technology, including spectral-domain OCT and SS-OCT implementations, provides higher acquisition speeds. In addition, new developments of broad-bandwidth light sources and high-speed, large pixel-number cameras have resulted in development of spectral-domain and full-field ultrahigh-resolution OCT technology with axial resolution close to or below 1 μm, suitable for imaging the cellular and subcellular structure of biological tissue [18].
Our results revealed that there are no statistically significant differences in CCT, AL, WTW, K1 and K2, when the eye changes its accommodative state to clearly focus the optotype presented at the three different vergences.
In the case of the cornea, this is in agreement with previous results from other researchers that found that different parameters in various zones of the cornea as well as corneal aberrations were stable during accommodation. Sisó-Fuertes et al. [19] assessed whether corneal parameters and aberrations are affected by accommodation using a dual Scheimpflug device. They obtained data on the anterior and posterior corneal axial curvatures, total corneal power, and corneal pachymetry from three corneal zones (central: 0.0 up to 4.0 mm; paracentral or mid: 4.0 up to 7.0 mm; peripheral: 7.0 up to 10.0 mm) in young emmetropic eyes in the unaccommodated and four accommodated states (from 1.0 to 4.0 D, in 1.0 D steps). They found no significant changes in any measured parameter during accommodation for any corneal zone (p > 0.05), concluding that different parameters measured in various zones of the cornea as well as corneal aberrations were stable during accommodation. Bayramlar et al. [20] investigated the effect of accommodation on corneal topography in healthy subjects. Using an aberrometer and a corneal topographer, corneal topographic images, images of the iris, and the refraction of the subjects were simultaneously obtained before and during fixation of a near target. They obtained no apparent differences in corneal topography and no statistical differences in mean keratometry values.
Regarding the AL outcomes, we obtained no statistically significant differences between the three accommodative conditions, concluding that AL did not change with statistical significance when focusing the optotype at the three different vergences. Woodman et al. [21] indicated that, although studies have consistently noted small increases in AL during accommodation, the exact cause of this axial elongation is unknown. They found a significant axial elongation (about 5 and 15 μm) immediately following the commencement of an accommodation task (4 D). This was sustained for the duration of the task, and was also evident to a lesser extent immediately following task cessation. They indicated that AL returned to baseline levels 10 min after the accommodation task. Zhong et al. [22], using ultra-long scan depth OCT, also obtained an averaged elongated AL of 26.1 ± 13.4 μm, when the subjects accommodated from the relaxed state to a stimulus placed at 6.0 D of vergence. In our case, mean AL increased by around 7 μm when the subjects accommodated from the relaxed state to the 3.0 D condition, which could be in agreement with previous reports, although this change was not statistically significant probably due to the intersubject variability.
Regarding the ACD and LT measurements, our results evidenced that there are statistically significant differences for both axial outcomes when the eye changes its accommodative state to clearly focus the optotype presented at the three different vergences.
The crystalline lens is established to be the ocular structure that suffers the principal anatomical changes during accommodation. Accordingly, the differences in ACD and LT outcomes comparing the three accommodative conditions were statistically significant (p < 0.001). Specifically, ACD decreased and LT increased when the subject was looking at the optotype placed at closer distances (higher vergences in D). Mean ACD was reduced by around 160 μm when the accommodation changed from the relaxed state to the 3.0 D condition, while mean LT increased by around 170 μm for the same change in the accommodation state. Our findings agree with the consideration that, when accommodation is active, there is a decrease in ACD and an increase in LT. This is in agreement with the classic theory of accommodation from Helmholtz and Fincham [14], which states that, during accommodation, the anterior surface of the crystalline lens becomes steeper and moves forward, increasing its thickness and causing a decrease in the ACD. The changes in ACD and LT measurements were linearly correlated for all subjects enrolled in the study, as previously shown in Fig. 5. In addition, the R2 value was greater or equal to 0.99 for all included subjects. These results agree with the classic theory of accommodation from Helmholtz and Fincham, as the ACD decreases when the anterior surface of the crystalline lens moves forward with increasing accommodation.
Previously there have been reports of the per diopter changes in ACD and LT. Ostrin et al. [23] obtained on average, and by means of A-scan biometry measuring in 22 human subjects between the ages of 21 and 30 years, a per diopter change in ACD and LT of −0.051 ± 0.008 mm/D and 0.067 ± 0.008 mm/D, respectively. Bolz et al. [24] obtained, using partial coherence interferometry over ten emmetropic and 3ten myopic subjects, a per diopter change in ACD of −0.047 mm/D in emmetropic eyes and −0.057 mm/D in myopic eyes, and a per diopter change in LT of 0.063 mm/D in emmetropic eyes and 0.072 mm/D in myopic eyes. Meanwhile, Richdale et al. [9] obtained on average, by means of time-domain OCT and measuring on 22 subjects between the ages of 36 and 50 years, a per diopter change in LT of 0.051 ± 0.019 mm/D. Neri et al. [15], by means of anterior segment SS-OCT imaging on 14 eyes changing the accommodative stimulus from 0.0 D to 9.0 D with 3.0 D steps, obtained a per diopter ACD reduction of −0.027 ± 0.012 mm/D, and a per diopter LT increase of 0.036 ± 0.013 mm/D. Laughton and colleagues [25], using optical low coherence reflectometry on 20 individuals aged between 34 and 41 years, measured an ACD change per diopter of −0.063 ± 0.020 mm/D in the case of myopic subjects, and of −0.101 ± 0.078 mm/D for emmetropes. And the measured per diopter LT change was 0.066 ± 0.023 mm/D for myopes, and 0.104 ± 0.079 mm/D for emmetropes. Lastly, ultrasound biomicroscopy has been used to measure per diopter ACD and LT changes [26, 27]. In a first study [26], they enrolled 26 subjects aged 21 to 36 years, and obtained an ACD decrease rate of −0.049 mm/D and an LT increase rate of 0.065 mm/D. In a second study [27], they included 25 subjects aged 36 to 46 years, and obtained a per diopter ACD decrease of −0.053 mm/D, and a per diopter LT increase of 0.073 mm/D.
The findings obtained in our study by means of SS-OCT technology are in agreement with the previously reported results. Thus, we obtained a per diopter change for ACD of −0.052 ± 0.011 mm/D, and a per diopter change for LT of 0.057 ± 0.011 mm/D. Nevertheless, a direct comparison of all the reported per diopter outcomes can not be done directly, because of several factors. For instance, differences in the accommodative stimulus presentation, subject populations, sample size, lack of accurate recording of the accommodative response, and variation of resolution of the different techniques may influence the results [9, 25,26,27,28]. In particular, many of the studies, including this one, did not record accommodative response, but only assumed that the subject was accommodating accurately to the target (an optotype with Sloan letters corresponding to decimal visual acuity of 1.0 was used at each distance in order to assure that the subject accommodative response was close enough to the accommodative demand). In any case, depending on the amount of accommodative lag for each subject, the calculation of per diopter changes could be artificially influenced. Therefore, per diopter changes in biometry calculated from stimulus amplitudes rather than from objectively measured accommodative optical response amplitudes underestimate the actual per diopter biometry changes because the actual accommodative response lags behind the stimulus amplitude [26].
The present study measured only healthy eyes, and therefore, the conclusions cannot be applied to pathological eyes, or postoperatively altered corneas, and in addition in older patients with or without cataract. Further studies should assess this effect in those excluded eye groups. Another limitation of our study is the small sample size, which limits the accurate description of the whole population. Thus, the extrapolation to the rest of the population should be treated carefully.
All the ocular parameters measured by non-contact optical biometry might help researchers to know real values for the anatomical dimensions of the human eye on a defined sample. These values could be used to assess, for instance, some of the elastic properties of the eye structures, like Young’s modulus and Poisson’s ratio, by means of the definition and analysis of computational human eye models [29]. These elastic material properties of the human eye might help quantify details of symptoms of the diseases in the near future. In addition, we outline that one promising research line where the obtained measurements are of interest is the feedback between the mechanical response of the eye to the accommodation and the actual mechanism of accommodation.
In conclusion, a methodology to assess the changes in ocular parameters for different accommodative demands using the IOLMaster 700 has been described. This allows for measuring changes in ocular parameters when an accommodative stimulus is presented to the eye at different vergences. This methodology makes possible observing in a non-invasive way the main changes in the eye parameters during accommodation by means of SS-OCT technology.
References
Montés-Micó R, Carones F, Buttacchio A, Ferrer-Blasco T, Madrid-Costa D (2011) Comparison of immersion ultrasound, partial coherence interferometry, and low coherence reflectometry for ocular biometry in cataract patients. J Refract Surg 27:665–671
Srivannaboon S, Chirapapaisan C, Chonpimai P, Loket S (2015) Clinical comparison of a new swept-source optical coherence tomography-based optical biometer and a time-domain optical coherence tomography-based optical biometer. J Cataract Refract Surg 41:2224–2232
Kunert KS, Peter M, Blum M, Haigis W, Sekundo W, Schütze J, Büehren T (2016) Repeatability and agreement in optical biometry of a new swept-source optical coherence tomography–based biometer versus partial coherence interferometry and optical low-coherence reflectometry. J Cataract Refract Surg 42:76–83
Akman A, Asena L, Güngör SG (2016) Evaluation and comparison of the new swept source OCT-based IOLMaster 700 with the IOLMaster 500. Br J Ophthalmol 100:1201–1205
Lehman BM, Berntsen DA, Bailey MD, Zadnik K (2009) Validation of OCT-based crystalline lens thickness measurements in children. Optometry and vision science: official publication of the American Academy of Optometry 86:181
Baikoff G, Lutun E, Ferraz C, Wei J (2004) Static and dynamic analysis of the anterior segment with optical coherence tomography. J Cataract Refract Surg 30:1843–1850
Tsorbatzoglou A, Nemeth G, Szell N, Biro Z, Berta A (2007) Anterior segment changes with age and during accommodation measured with partial coherence interferometry. J Cataract Refract Surg 33:1597–1601
Leng L, Yuan Y, Chen Q, Shen M, Ma Q, Lin B et al (2014) Biometry of anterior segment of human eye on both horizontal and vertical meridians during accommodation imaged with extended scan depth optical coherence tomography. PLoS One 9:e104775
Richdale K, Bullimore MA, Zadnik K (2008) Lens thickness with age and accommodation by optical coherence tomography. Ophthalmic Physiol Opt 28:441–447
McAlinden C, Khadka J, Pesudovs K (2011) Statistical methods for conducting agreement (comparison of clinical tests) and precision (repeatability or reproducibility) studies in optometry and ophthalmology. Ophthal Physiol Opt 31:330–338
Montés-Micó R, Alió J, Muñoz G, Charman W (2004) Temporal changes in optical quality of air-tear film interface at anterior cornea after blink. Invest Ophthalmol Vis Sci 45:1752–1757
Tan WY (1982) Sampling distributions and robustness of t, F and variance-ratio in two samples and ANOVA models with respect to departure from normality. Communication in statistics – Theory and Methods 11:486–511
Box GEP (1965) Some theorems on quadratic forms applied in the study of analysis of variance problems. II: effects of inequality of variance and of correlation between errors in the two-way classification. Ann Math Stat 25:484–498
Charman WN (2008) The eye in focus: accommodation and presbyopia. Clin Exp Optom 91:207–225
Neri A, Ruggeri M, Protti A, Leaci R, Gandolfi SA, Macaluso C (2015) Dynamic imaging of accommodation by swept-source anterior segment optical coherence tomography. J Cataract Refract Surg 41:501–510
Piñero DP (2015) Technologies for anatomical and geometric characterization of the corneal structure and anterior segment: a review. Semin Ophthalmol 30:161–170
Ramos JL, Li Y, Huang D (2009) Clinical and research applications of anterior segment optical coherence tomography—a review. Clin Experiment Ophthalmol 37:81–89
Bizheva K, Haines L, Mason E, MacLellan B, Tan B, Hileeto D, Sorbara L (2016) In vivo imaging and morphometry of the human pre-Descemet's layer and endothelium with ultrahigh-resolution optical coherence tomography. Invest Ophthalmol Vis Sci 57(1):2782–2787
Sisó-Fuertes I, Domínguez-Vicent A, del Águila-Carrasco A, Ferrer-Blasco T, Montés-Micó R (2015) Corneal changes with accommodation using dual Scheimpflug photography. J Cataract Refract Surg 41:981–989
Bayramlar H, Sadigov F, Yildirim A (2013) Effect of accommodation on corneal topography. Cornea 32:1251–1254
Woodman EC, Read SA, Collins MJ (2012) Axial length and choroidal thickness changes accompanying prolonged accommodation in myopes and emmetropes. Vis Res 72(1):34–41
Zhong J, Tao A, Xu Z, Jiang H, Shao Y, Zhang H, Liu C, Wang J (2014) Whole eye axial biometry during accommodation using ultra-long scan depth optical coherence tomography. Am J Ophthalmol 157:1064–1069
Ostrin L, Kasthurirangan S, Win-Hall D, Glasser A (2006) Simultaneous measurements of refraction and A-scan biometry during accommodation in humans. Optom Vis Sci 83:657–665
Bolz M, Prinz A, Drexler W, Findl O (2007) Linear relationship of refractive and biometric lenticular changes during accommodation in emmetropic and myopic eyes. Br J Ophthalmol 91:360–365
Laughton DS, Sheppard AL, Davies LN (2016) A longitudinal study of accommodative changes in biometry during incipient presbyopia. Ophthalmic Physiol Opt 36:33–42
Ramasubramanian V, Glasser A (2015) Objective measurement of accommodative biometric changes using ultrasound biomicroscopy. J Cataract Refract Surg 41:511–526
Ramasubramanian V, Glasser A (2015) Prediction of accommodative optical response in prepresbyopic subjects using ultrasound biomicroscopy. J Cataract Refract Surg 41:964–980
Farouk MM, Naito T, Shinomiya K, Eguchi H, Sayed KM, Nagasawa T, Katome T, Mitamura Y (2015) Optical coherence tomography reveals new insights into the accommodation mechanism. J Ophthalmol 2015:510459
Aloy MA, Adsuara JE, Cerdá-Durán P, Obergaulinger M, Esteve-Taboada JJ, Ferrer-Blasco T, Montés-Micó R (2017) PLOS One (accepted for publication)
Funding
The Spanish Government provided financial support in the form of research grant funding (Explora project, reference SAF2013–49284-EXP). The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
ESM 1
(DOCX 10 kb)
Rights and permissions
About this article
Cite this article
Esteve-Taboada, J.J., Ferrer-Blasco, T., Aloy, M.A. et al. Ocular anatomic changes for different accommodative demands using swept-source optical coherence tomography: a pilot study. Graefes Arch Clin Exp Ophthalmol 255, 2399–2406 (2017). https://doi.org/10.1007/s00417-017-3801-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-017-3801-z