Abstract
Purpose
The purpose of this study was to evaluate systemic endothelial function in elderly hypertension patients with non-arteritic anterior ischaemic optic neuropathy (NAION) by using a noninvasive physiological method: endothelium-dependent, flow-mediated vasodilation (FMD).
Methods
Forty-two systemic hypertension patients with NAION (NAION group), 64 age- and sex-matched patients with systemic hypertension and no other ocular disease (hypertension group), and 100 age- and sex-matched healthy volunteers (normal group) were enrolled. FMD was evaluated using a high-resolution ultrasonography. Traditional cardiovascular risk factors and vascular parameters were measured.
Results
Systolic blood pressure and diastolic blood pressure were significantly higher in patients with NAION compared with the control groups (p < 0.001). The FMD decreased significantly in the NAION group (6.02 ± 1.87 %) compared to in the hypertension group (7.86 ± 2.94 %, p < 0.001) and the normal group (8.99 ± 2.44 %, p < 0.001). By multivariable logistic regression analysis, FMD was significantly associated with NAION (OR, 1.79; 95%CI, 1.67–2.01).
Conclusions
NAION may be associated with systemic vascular endothelial dysfunction. FMD might be useful in the treatment monitoring of NAION.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nonarteritic anterior ischemic optic neuropathy (NAION) is the most common type of optic neuropathy in elder individuals, caused by vascular insufficiency leading to optic nerve head ischemia, and characterized by acute and painless visual loss or visual field defect [1, 2]. The pathogenic mechanisms of NAION enclose various cardiovascular risk factors, such as systemic hypertension, hyperlipidemia and diabetes mellitus [3–5]. However, the exact mechanism of NAION is unclear, especially the relationship between NAION and systemic diseases.
The vascular endothelium is the inner surface of all blood vessels and the common ground on which cardiovascular risk factors act to initiate the atherosclerotic process. Furthermore, the endothelium is a highly active autocrine and paracrine organ that regulates vascular tone through the effects of locally synthesized mediators, predominantly nitric oxide (NO), where NO acts as a vasodilator, inhibits inflammation [6]. Dysfunctional endothelium may promote adhesion of monocyte and leukocyte, vasoconstriction, activation of platelets and thrombos formation [6, 7]. Although endothelial function has been assessed by a variety of invasive and noninvasive methods in clinical practice, the brachial artery endothelium-dependent flow-mediated, vasodilation (FMD) is a validated, widely used, noninvasive physiological measure to evaluate generalized endothelial function. Ultrasound assessment of endothelial-dependent FMD of the brachial artery was first performed using a modification of the method described by Celermajer about 20 years ago [8, 9]. Shear stress is increased on the vessel wall of the brachial artery through forearm pressure by cuff inflation, which induces endothelial NO release and subsequent vasodilation. FMD is calculated as the percentage change in diameter before and after cuff inflation. This method has good accuracy and repeatability, and can be offered as early noninvasive monitoring in systemic endothelial function [10, 11]. Impairement of FMD was related to elder age, sex difference, smoking, alcohol abuse, hypertension, dyslipidemia and hyperglycemia [12–14].
FMD is diminished in patients with endothelial dysfunction, and it has also been used to evaluate the peripheral endothelial alterations in patients with cardiovascular disease [15, 16], ischemic stroke [17] and ocular diseases such as glaucoma [18, 19] and diabetic retinopathy [20]. Associations with impaired brachial artery FMD and branch retinal vein occlusion have also been reported, suggesting systemic endothelial dysfunction in the retinal microvasculature in patients with retinal vascular disorders [21]. However, the relationship between systemic endothelial function and NAION remains unclear.
The present study is, to our best knowledge, the first time that the brachial artery FMD in patients with NAION is evaluated to determine whether systemic vascular endothelial dysfunction is associated with the pathogenesis of NAION.
Patients and methods
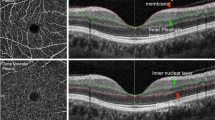
This study was approved by the Ethics Committee of the Sun Yat-sen University. Written consent was obtained from all study participants according to the Declaration of Helsinki. The study included age- and sex-matched systemic hypertension patients with NAION (NAION group), patients with systemic hypertension and no history of acute visual loss or impaired visual function at patient recruiting period (hypertension group), and healthy volunteers (normal group). Hypertension was defined as systolic blood pressure (SBP) more than140 mm Hg, diastolic blood pressure (DBP) more than 90 mm Hg, or current use of antihypertensive medications. All subjects were aged from 50 to 80 years old and enrolled in the study between March 2011 and April 2015. Subjects with pregnancy, cardiovascular or cerebrovascular diseases, diabetes mellitus, dyslipidemia and those who were current or past smokers (previous 5 years), or patients with alcohol abuse history, were excluded. Inclusion criteria for the normal group included no acute visual loss history or impaired visual function at the same period of patient recruitment, no hypertension, no use of antihypertensive medications, and no family history of vascular disease. The hypertension group and normal group were recruited from the health screening center in our hospital. Patients from the NAION group who visited the First Affiliated Hospital of Sun Yat-sen University had not been admitted to other medical facilities. All patients with NAION presented acute painless loss of visual acuity, relative afferent pupillary defect, optic disc edema, field defect on computerized perimetry, and early filling defect of the disc (by FFA) in the affected eye without evidence of other neurological, systemic or ocular disease. Patients with a high erythrocyte sedimentation rate or a positive history for clinical features of giant cell arteritis were excluded from this study. Fasting (> 8 hours) blood samples were drawn from participants, and blood chemistry was performed in the Clinical Testing Center of our hospital. All subjects had a complete ophthalmological examination (slit-lamp biomicroscopy, and funduscopic examination using a 78-diopter lens).
Blood pressure was determined by sphygmomanometry in a sitting position after a rest of 10 min. The endothelial function was evaluated by measurement of the FMD in the brachial artery in response to hyperemia, according to previously described ultrasound studies, and acquired according to a standard protocol [16, 17]. All subjects fasted for at least 8 hours and stopped taking coffee for at least 2 h before the ultrasound examination. After 15 min of rest in quiet conditions, FMD was evaluated in the right brachial artery using a high-resolution ultrasound machine equipped with a high-frequency and linear array ultrasound probe (5–12 MHz, GE VIVID7, USA). The probe was positioned approximately 2–5 cm proximal to the elbow. Diameter and blood flow velocity of brachial artery were recorded by R-wave gating of the synchronic electrocardiogram (ECG). Baseline parameters were obtained before reactive hyperemia, and then an arterial occlusion cuff was placed around the arm, which was inflated above 250 mmHg for 5 min before deflating. After cuff deflation, the greatest diameter and maximal velocity were recorded at end diastole (tip of ECG R-wave). FMD is expressed as the percentage change in diameter before and after cuff inflation [18]. All measurements were performed by the same experienced operator, who was unaware of the subject’s condition.
Statistical analysis
Data were expressed as mean ± standard error. Continuous variables were compared among the NAION group, hypertension group and normal group by one-way ANOVA with Bonferroni correction. Multivariable logistic regression analysis was performed to identify significant risk factors for NAION. All statistical analysis was performed in SPSS (Version19.0, Chicago, USA), and p < 0.05 was considered statistically significant. The sample size analysis was performed in power analysis and sample size system (PASS) 2011.
Results
In a one-way ANOVA study, assuming that the power is 0.9 and significance level 0.05, the calculated sample size is 40 NAION subjects, 40 hypertension subjects, and 90 healthy subjects. To allow higher power in our study, the NAION group comprised 42 patients, 19 men and 23 women, with a mean age of 63.2 ± 3.6 years. The hypertension group comprised 64 age- and sex-matched subjects (28 male and 36 female; mean age 62.8 ± 1.2 years), and the normal group consisted of 100 age- and sex-matched subjects (44 male and 56 female; mean age 63.4 ± 2.3 years). The clinical characteristics of the participants are shown in Table 1. The average interval between onset of NAION and measurement was 10.6 ± 5.2 days. Thirty-two (75 %) of 42 patients in the NAION group and 48 (75 %) of 64 subjects in the hypertension group were taking antihypertensive drug, and the distribution of taking antihypertensive drugs was matching in the two groups (p > 0.999).
The SBP and DBP were significantly higher in patients with NAION compared to in the control groups (p < 0.001). The group averaged FMD values were shown in Fig. 1. The mean brachial artery FMD values were decreased significantly in the NAION group (6.02 ± 1.87 %) compared to in the hypertension group (7.86 ± 2.94, p < 0.001) and the normal group (8.99 ± 2.44 %, p < 0.001). There were no marked differences among the three groups, including for the body mass index, cholesterol, high-density lipoprotein, low-density lipoprotein, triglyceride, uric acid and the baseline diameter of the brachial artery (p > 0.05).
The three above-mentioned variables, FMD, SBP and DBP, were put into multivariate logistic regression analysis to determine risk factors for NAION. Their odds ratios were shown in Table 2. Our results showed that the lower FMD value was significantly associated with NAION (OR, 1.79; 95%CI, 1.67–2.01).
Discussion
The major findings of our study demonstrated for the first time that FMD was significantly impaired in elderly hypertension patients with NAION, indicating that NAION may be associated with peripheral vascular endothelial dysfunction.
Hypertension is the most common vasculopathic risk factor for NAION patients, accounting for about 47–49 % [4, 5]. FMD in patients with systemic hypertension significantly decreased compared to in healthy subjects [22]. Consistent with this, our results found that FMD in systemic hypertension patients significantly decreased compared with healthy subjects, indicating endothelial dysfunction. Brachial FMD is associated with various cardiovascular risk factors, and a low level of FMD has been demonstrated to predict future cardiovascular disease events [23]. In the current study of hypertension subjects, we also found that the mean brachial artery FMD value decreased significantly in the NAION group compared to in the hypertension group, with higher SBP and DBP. Furthermore, the lower FMD value was significantly associated with NAION in the study, suggesting endothelial dysfunction may be associated with NAION. Although the pathogenic concept of NAION is poorly understood, Potarazu [24] considered that endothelial defects in the ocular circulation may impair the efficacy of endothelial-derived relaxation factors in NAION. Tsutomu Sakai et al. [25, 26] also found that genetic polymorphisms in enzymes influencing endothelial function, including the endothelial nitric oxide synthase gene, may be an important risk factor in developing NAION in the Japanese population. The pathogenesis of NAION is believed to be multifactorial, and encompass the acute hypoperfusion of short posterior ciliary arteries. [1] Dysfunctional endothelium may promote vascular tone, worsen vasodilation and vasoconstriction, and lead to hypoperfusion of the short posterior ciliary arteries. Furthermore, dysfunctional endothelium may cause the adhesion of monocyte and leukocyte, activation of platelets and thrombos formation, which may change the blood components and blood viscosity. Further studies are needed to determine if endothelial dysfunction may be involved in the pathogenesis of NAION, and to assess whether FMD is a prognostic marker of NAION events.
There are some limitations to the present study. One is that we measured endothelial function of the brachial artery instead of the retrobulbar artery, because no proper method for providing a reliable endothelial function measurement for the retrobulbar artery has been found to date. Secondly, since antihypertensive drugs can improve endothelial dysfunction [27], we could not separate the effects of hypertension and hypertensive medicine from endothelial function, due to the limited sample size. In addition, selection bias might have been present when both SBP and DBP in the NAION group were significantly higher than those in the hypertension group. Larger scale studies with better case–control matching will be helpful in the pathogenic mechanisms of NAION.
In summary, our study demonstrated impaired brachial arteries FMD in elderly hypertension patients with NAION, suggesting endothelial dysfunction may be associated with NAION. FMD could be used as an important noninvasive monitoring technique for NAION prevention.
References
Hayreh SS, Podhajsky P, Zimmerman MB (1999) Role of nocturnal arterial hypotension in optic nerve head ischemic disorders. Ophthalmologica 213:76–96
Newman NJ, Scherer R, Langenberg P et al (2002) The fellow eye in NAION: report from the ischemic optic neuropathy decompression trial follow-up study. Am J Ophthalmol 134:317–328
Atkins EJ, Bruce BB, Newman NJ, Biousse V (2010) Treatment of nonarteritic anterior ischemic optic neuropathy. Surv Ophthalmol 55:47–63
Flaharty PM, Sergott RC, Lieb W, Bosley TM, Savino PJ (1993) Optic nerve sheath decompression may improve blood flow in anterior ischemic optic neuropathy. Ophthalmology 100:297–302
Hayreh SS, Joos KM, Podhajsky PA, Long CR (1994) Systemic diseases associated with nonarteritic anterior ischemic optic neuropathy. Am J Ophthalmol 118:766–780
Deanfield JE, Halcox JP, Rabelink TJ (2007) Endothelial function and dysfunction: testing and clinical relevance. Circulation 115:1285–1295
Nadar S, Blann AD, Lip GY (2004) Endothelial dysfunction: methods of assessment and application to hypertension. Curr Pharm Des 10:3591–3605
Celermajer DS, Sorensen KE, Bull C, Robinson J, Deanfield JE (1994) Endothelium dependent dilation in the systemic arteries of asymptomatic subjects relates to coronary risk factors and their interaction. J Am Coll Cardiol 24:1468–1474
Celermajer DS, Sorensen KE, Gooch VM et al (1992) Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet 340:1111–1115
Corretti MC, Anderson TJ, Benjamin EJ et al (2002) Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol 39:257–265
Moens AL, Goovaerts I, Claeys MJ, Vrints CJ (2005) Flow-mediated vasodilation: a diagnostic instrument, or an experimental tool? Chest 127:2254–2263
Benjamin EJ, Larson MG, Keyes MJ et al (2004) Clinical correlates and heritability of flow-mediated dilation in the community: Framingham heart study. Circulation 109:613–619
Juonala M, Viikari JS, Laitinen T et al (2004) Interrelations between brachial endothelial function and carotid intimamedia thickness in young adults: the cardiovascular risk in young Finns study. Circulation 110:2918–2923
Suwaidi JA, Hamasaki S, Higano ST et al (2000) Long-term follow-up of patients with mild coronary artery disease and endothelial dysfunction. Circulation 101:948–954
Heitzer T, Schlinzig T, Krohn K, Meinertz T, Münzel T (2001) Endothelial dysfunction, oxidative stress, and risk of cardiovascular events in patients with coronary artery disease. Circulation 104:2673–2678
Halcox JP, Schenke WH, Zalos G et al (2002) Prognostic value of coronary vascular endothelial dysfunction. Circulation 106:653–658
Santos-García D, Blanco M, Serena J et al (2009) Brachial arterial flow mediated dilation in acute ischemic stroke. Eur J Neurol 16:684–690
Su WW, Cheng ST, Ho WJ et al (2008) Glaucoma is associated with peripheral vascular endothelial dysfunction. Ophthalmology 115:1173–1178
Fadini GP, Pagano C, Baesso I et al (2010) Reduced endothelial progenitor cells and brachial artery flow-mediated dilation as evidence of endothelial dysfunction in ocular hypertension and primary open-angle glaucoma. Acta Ophthalmol 88:135–141
Sogawa K, Nagaoka T, Tanano I et al (2012) Association between diabetic retinopathy and flow-mediated vasodilation in type 2 DM. Curr Eye Res 37:446–451
Tanano I, Nagaoka T, Sogawa K et al (2013) Impaired Systemic Vascular Endothelial Function in Patients with Branch Retinal Vein Occlusion. Curr Eye Res 38:114
Pemp B, Weigert G, Karl K et al (2009) Correlation of flicker-induced and flow-mediated vasodilatation in patients with endothelial dysfunction and healthy volunteers. Diabetes Care 32:1536–1541
Nguyen TT, Islam FM, Farouque HM et al (2010) Retinal vascular caliber and brachial flow-mediated dilation: the Multi-Ethnic Study of Atherosclerosis. Stroke 41:1343–1348
Potarazu SV (1997) Ischemic optic neuropathy: models for mechanism of disease. Clin Neurosci 4:264–269
Sakai T, Shikishima K, Matsushima M, Tsuneoka H (2013) Genetic polymorphisms associated with endothelial function in nonarteritic anterior ischemic optic neuropathy. Mol Vis 19:213–219
Sakai T, Shikishima K, Matsushima M, Kitahara K (2007) Endothelial nitric oxide synthase gene polymorphisms in non-arteritic anterior ischemic optic neuropathy. Graefes Arch Clin Exp Ophthalmol 245:288–292
Miyamoto M, Kotani K, Ishibashi S, Taniguchi N (2012) The effect of antihypertensive drugs on endothelial function as assessed by flow-mediatedvasodilation in hypertensive patients. Int J Vasc Med 2012:453264
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The Department of Science and Technology of Guangdong Province provided financial support in the form of 2014A020212578 funding. The sponsor had no role in the design or conduct of this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Yao, F., Wan, P., Su, Y. et al. Impaired systemic vascular endothelial function in patients with non-arteritic anterior ischaemic optic neuropathy. Graefes Arch Clin Exp Ophthalmol 254, 977–981 (2016). https://doi.org/10.1007/s00417-015-3212-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-3212-y