Abstract
Purpose
This study was conducted to investigate a case of reactive lymphoid hyperplasia following laser assisted in situ keratomileusis (LASIK).
Methods
A 31-year-old man who underwent LASIK presented 1 month later with a fleshy conjunctival (plical) tumor in the left eye. An excision biopsy of the tumor was performed.
Results
Histopathology of the excised tumor revealed reactive lymphoid hyperplasia.
Discussion
Conjunctival lymphomas can masquerade as chronic conjunctivitis and can be preceded by reactive lymphoid hyperplasia. It is important to identify and differentiate these tumors. This report describes the unusual occurrence of a lymphoid conjunctival tumor after LASIK eye surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the most significant areas of development in photorefractive keratectomy is laser-assisted in situ keratomileusis (LASIK) [2], which involves the use of a microkeratome to create a flap of anterior cornea that is raised to facilitate ablation of a portion of the corneal stroma (typically to treat myopia). In this work, we describe a case of lymphoid hyperplasia tumor developing after LASIK surgery.
Case report
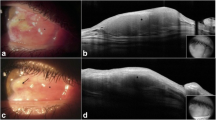
A 31-year-old man underwent LASIK in April 2002 for correction of myopic astigmatism (oculi uterque). After the procedure, he was treated with ocular lubricating drops and topical steroids. One month later, he noticed a small growth forming in the nasal interpalpebral conjunctiva of his left eye (Fig. 1). The tumor did not respond to topical steroid therapy and gradually enlarged. Upon referral to The New York Eye Cancer Center, he was noted to have an uncorrected visual acuity (UCVA) of 20/16 in his left eye. Slit lamp examination revealed a pink hypervascular conjunctival tumor overlying the plica and compressing the caruncle in the left eye (Fig. 1). After obtaining informed consent, a biopsy was performed to include a 1-mm margin of normal-appearing tissue.
Results
Histopathology
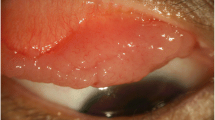
The histopathology of the tan polypoid mucosal tissue (0.5×0.5×0.4 cm) showed irregular follicles in a background of mildly atypical lymphocytes (Fig. 2a). Immunohistochemical stains were performed (CD10, CD20, CD43, CD3, CD5, kappa, lambda). There was marked subepithelial lymphoid hyperplasia with numerous lymphoid follicles surrounded by slightly thickened mantle zones (Fig. 2b). The germinal centers contained CD20 and some CD10 positive centrocytes and centroblasts with rare tangible body macrophages (Fig. 2c). The interfollicular areas were devoid of mitotic activity and showed predominantly T lymphocytes (CD3-, CD5-, and CD43-positive; Fig. 2d) and occasional B cells (CD20-positive). Kappa and lambda stains revealed balanced labeling; there was no evidence of monoclonality. Lymphoepithelial tropism was noted focally, and the germinal center contours were focally moth-eaten, particularly in areas where the mantle zone was expanded. This suggested a diagnosis of reactive lymphoid hyperplasia.
a Histopathology of the excised tumor showing lymphoid follicles (arrow) with germinal centers (hematoxylin–eosin staining; ×10 magnification). b Immunohistochemistry of the excised specimen demonstrating marked subepithelial lymphoid hyperplasia with numerous lymphoid follicles surrounded by slightly thickened mantle zones (CD20-positive; ×10 magnification). c Germinal centers contain CD20 and some CD10-positive centrocytes and centroblasts with rare tangible body macrophages (CD10-positive; ×20 magnification). d Interfolicular areas are devoid of mitotic activity and show predominantly T lymphocytes (CD43-positive) and occasional B cells (CD20-positive; ×10 magnification)
Systemic examination did not reveal systemic lymphoma. The patient is now 2 years postexcision with no evidence of ocular recurrence or systemic lymphoma.
Discussion
Ocular adnexal lymphoproliferative lesions consist of a spectrum of disease entities [1, 4]. This includes reactive lymphoid hyperplasia, atypical lymphoid hyperplasia, and lymphoma. Reactive lymphoid hyperplasia is the benign and reversible enlargement of lymphoid tissue secondary to an antigen stimulus. The causes of reactive lymphoid hyperplasia include idiopathic and chronic conjunctival inflammations, such as infections (infectious mononucleosis, toxoplasmosis, tuberculosis, AIDS) and immunological diseases (rheumatoid arthritis) [6]. Conjunctival lymphomas are usually indolent mucosa-associated lymphoid tissue (MALT) lymphomas and may be preceded by apparent reactive lymphoid hyperplasia [9]. No clinical or radiologic criteria exist to differentiate these lesions, but histopathological evaluation, flow cytometry, gene rearrangement studies, and immunohistochemistry can help in this differentiation [4, 6, 7].
Conjunctival lymphoma may not present with the classic salmon-patch subepithelial nodular infiltration but may rather occur diffusely, causing persistent conjunctival inflammation and cicatrizing conjunctivitis, masquerading as chronic conjunctivitis or even scleritis unresponsive to steroid or immunosuppressive therapy [3, 10]. Yeung et al. [10] have reported an 18-year-old male with a 3-month history of intractable follicular conjunctivitis unsuccessfully treated for Chlamydial conjunctivitis. In their case, a conjunctival biopsy revealed MALT lymphoma. In addition, two reported cases of persistent allergic conjunctivitis were biopsied after 2 months of ineffective treatment and were found to be low-grade MALT lymphomas [3]. Clearly, when confronted with tumor formation or chronic conjunctivitis, the clinician should suspect malignancy. Although squamous and sebaceous carcinomas are typically suspected, these cases demonstrate that the differential diagnosis should include lymphoid tumors.
There have been no previous reports describing the development of conjunctival lymphoid tumors following LASIK eye surgery. Postoperative complications after LASIK eye surgery that have been described include: dry eyes (mainly due to reduced corneal sensitivity), diffuse lamellar keratitis, infectious keratitis, flap striae, haze, and visual aberrations [2]. There have also been reports of retinal breaks and visual field loss after LASIK [5, 8].
Our patient developed reactive lymphoid hyperplasia within a short period (1 month) of his LASIK surgery. This tumor is probably only temporally related to the LASIK procedure with no cause–effect relationship. The lesion may have been present but unnoticed before the LASIK and the use of eye drops or constant irritation may have aggravated the condition and made the tumor prominent. However, it is important to be aware of this condition in patients with a history of a chronic conjunctivitis or of LASIK.
References
Coupland SE, Krause L, Delecluse HJ et al (1998) Lymphoproliferative lesions of the ocular adnexa. Analysis of 112 cases. Ophthalmology 105:1430–1441
Davis E, Hardten D, Lindstrom R (2000) LASIK complications. Int Ophthalmol Clin 40:67–75
Lee D, Sohn H, Park S, Kang Y (2001) Bilateral conjunctival mucosa-associated lymphoid tissue lymphoma misdiagnosed as allergic conjunctivitis. Cornea 20:427–429
Mannami T, Yoshino T, Oshima K et al (2001) Clinical, histopathological and immunogenetic analysis of ocular adnexal lymphoproliferative disorders: characterization of malt lymphoma and reactive lymphoid hyperplasia. Mod Pathol 14:641–649
Ruiz-Morino JM, Alio JL (2003) Incidence of retinal disease following refractive surgery in 9,239 eyes. J Refract Surg 19:534–547
Sharara N, Holden JT, Wojno TH, Feinberg AS, Grossniklaus HE (2003) Adnexal lymphoid proliferations: clinical, histologic, flow cytometric, and molecular analysis of forty-three cases. Ophthalmology 110:1245–1254
Takada S, Yoshino T, Taniwaki M et al (2000) Involvement of the chromosomal translocation t (11:18) in some mucosa-associated lymphoid tissue lymphomas and diffuse large B-cell lymphomas of the ocular adnexa. Mod Pathol 16:445–452
Weiss H, Rubinfeld R, Anderschat J (2001) LASIK-associated visual field loss in a glaucoma suspect. Arch Ophthalmol 119:774–775
Wotherspoon AC, Diss TC, Pan LX et al (1993) Primary low grade B-cell lymphoma of the conjunctiva: a mucosa-associated lymphoid type lymphoma. Histopathology 23:417–424
Yeung L, Tsao Y, Chen P, Kuo T, Lin K, Lai L (2004) Combination of adult inclusion conjunctivitis and mucosa-associated lymphoid tissue (MALT) lymphoma in a young adult. Cornea 23:7
Acknowledgements
This research was supported by The EyeCare Foundation, Inc. and Research to Prevent Blindness, New York, USA. We thank Drs. Steven A. McCormick and Madhavi Kurli for their help with histopathologic analysis, data acquisition, drafting, and revision of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reddy, S., Finger, P.T., Chynn, E.W. et al. Reactive lymphoid hyperplasia 1 month after LASIK surgery. Graefe's Arch Clin Exp Ophthalmo 244, 262–264 (2006). https://doi.org/10.1007/s00417-005-0007-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-005-0007-6