Abstract
Obstructive sleep apnea (OSA) is the most common type of sleep apnea and caused by upper airway obstructions. Clinically, patients with OSA characteristically experience intermittent nocturnal hypoxemia and impaired sleep quality. Cognitive impairments are commonly seen in patients with an OSA diagnosis. A literature search on OSA, cognitive impairments and CPAP was performed with various electronic databases including Medline, EMBASE and Google Scholar. The chosen evidence was limited to human subject studies only, and reports on either central sleep apnea or non-classified sleep apnea were excluded. Available evidence has been systemically reviewed to ascertain what types of cognitive impairments are related to OSA as well as the pathological connections. In addition, effectiveness of continuous positive airway pressure (CPAP) was analyzed as a standard therapy for improving cognitive performance in patients with OSA. The review contributed in: (1) delineating OSA as a risk factor of cognitive impairments; (2) enumerating cognitive impairments seen in patients with OSA; (3) substantiating the relation between OSA and cognitive impairments from the pathological perspective of AD biomarkers; and (4) revealing duration of CPAP is crucial for its therapeutic effects on improving cognitive performance in patients with OSA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is the most common type of sleep apnea, and it prevalence has been shown to be close to 3% in a veteran population [1]. The prevalence of OSA is related to a variety of factors including age [2], gender [3] and body mass index (BMI) [2, 4]. Clinically, OSA is characterized by intermittent hypoxia, hypercapnia, hypoventilation, and sleep disruption due to blocked or reduced airflow in the upper airway. Chronic intermittent nocturnal hypoxemia was suggested to be the cause for cognitive deficits seen in patients with OSA, as the severity of hypoxemia correlates significantly with the observed cognitive deficits [5]. In another study, a modest association was found between nocturnal hypoxemia and global cognitive decline, over a follow-up of more than 3 years [6]. Further, the OSA group was shown to have a significantly lower Mini-Mental State Examination (MMSE) score at baseline, compared to the control group in a cohort study [7]. Non-surprisingly, the severity of OSA was found to be inversely related to the Montreal Cognitive Assessment (MoCA) score [8]. However, the risk of developing mild cognitive impairment (MCI) or dementia was only related to either an elevated oxygen desaturation index or a high percentage of sleep time in apnea/hypopnea [9]. Neither sleep fragmentation nor sleep duration was noted to be related to the risk of developing MCI or dementia [9]. Our goal was to carry out a systemic review for ascertaining what cognitive functions are impaired in patients with OSA and search for pathological evidence between OSA and the associated cognitive impairments. At the same time, we want to analyze if continuous positive airway pressure is effective for improving the impaired cognitive functions seen in patients with OSA.
Methods
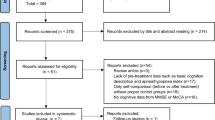
A systemic review was conducted by searching the electronic databases Medline, EMBASE, and Google Scholar with the following keywords: Alzheimer’s disease (AD), dementia, continuous positive airway pressure (CPAP), mild cognitive impairment (MCI), and obstructive sleep apnea syndrome (OSA). A few filters were used for the literature search: (1) language in English; (2) human subject studies; (3) published on or after 01/01/1985; and (4) abstracts are available. The original search returned a total of 493 results. After removing duplicates and review articles, 146 full text articles were left for further analysis. After the abstracts were reviewed, 106 studies were excluded for different reasons by a panel of three reviewers as they were either irrelevant, on central sleep apnea, or non-classified sleep apnea. The current review has focused on the remaining 40 reports (Fig. 1).
Cognitive impairments associated with OSA
People with OSA have an increased risk of developing cognitive impairments compared to those without it [9]. Worse cognitive performance was seen in people with OSA than the controls in the following domains: attention [5, 10, 11], executive function [10, 12], intelligence [12], memory [12], and psychomotor speed [10, 12] (Table 1). In addition, alertness was noted to be impaired in patients with OSA [5]. As expected, attention and memory were impaired in those with severe OSA [13]. Patients with OSA also had a longer reaction time and poorer vigilance than the controls [14]. Moreover, impaired memory [15] and executive function [11, 15, 16] was shown to be associated with the severity of oxygen desaturation or severity of OSA. Nonetheless, no association was observed between OSA and measures of memory function, concentration and attention from a cross-sectional study with an elderly (79–97 years old) cohort [4]. Therefore, the effects of OSA on different cognitive functions need be further investigated, especially utilizing studies with longitudinal designs.
Respiratory disturbance during sleep was more often seen in elderly individuals with dementia, when compared to the controls [17]. OSA may aggravate cognitive impairments in people with dementia, and the cognitive dysfunction could be reversed in patients with AD through treatment toward sleep apnea [18]. Although AD and sleep apnea were reported to be two separate conditions [19], a significant positive correlation was also found between apnea index and severity of dementia for AD patients [20].
Other factors for OSA-associated cognitive impairments
OSA is associated with cognitive deficits by interacting with the aging process [21]. For example, respiratory disturbance index of OSA was associated with the severity of cognitive dysfunction, and this association was seen only in patients who were younger than 80 years old [22]. Respiratory events negatively impacted memory function in older adults with an apolipoprotein epsilon 4 carrier status but not in those non-carriers [23]. Therefore, it is unclear on how genetic factors influence the relation between OSA and cognitive impairments. There are other factors that might interact with OSA to increase the risk of cognitive impairments. For example, OSA and short sleep duration were associated with all-cause dementia and AD; however, the associations were attenuated after the associated cardiovascular risk factors were adjusted [24]. Further, the extent of cerebrovascular impairment was shown to correlate with the severity of OSA [25]. The combined evidence suggests the overall cerebrovascular health is an important factor to consider when patients with OSA are evaluated for their cognitive performance.
OSA and AD pathological biomarkers
There are two classical AD pathological markers: amyloid plaques and neurofibrillary tangles. Amyloid plaques accumulate in the extracellular space, which is made up of different forms of β amyloid (Aβ) peptides including Aβ40 and Aβ42. By contrast, neurofibrillary tangles are intracellular accumulations of tau proteins. Patients with OSA had a lower Aβ42 from cerebrospinal fluid (CSF) and a higher Tau/Aβ42 ratio than the controls [12]. Significant correlations were found among CSF tau levels, sleep impairment, and CSF lactate levels in the OSA group [12]. Moreover, CSF Aβ42 levels were found to correlate with either memory impairment or nocturnal oxygen saturation parameters in patients with OSA [12]. Specifically, the OSA group had a higher Pittsburg compound B (Aβ plaque marker) deposition in the right posterior cingulate gyrus and right temporal cortex, when compared to the controls [26]. Similar to CSF Aβ42, CSF Aβ40 was decreased in patients with OSA compared to the controls [27]. Even in cognitively normal elderly people (55–90 years old), the severity of OSA was found to be associated with the annual rate of change of CSF Aβ42, as a measure of amyloid burden [28].
For serum biomarkers, OSA patients had significantly higher Aβ40, Aβ42 and total Aβ levels than the corresponding measures in the controls, and each biomarker positively correlated to the severity of OSA [29]. Compared to the controls, patients with OSA exhibited strikingly higher serum tau (P-181) levels, which positively correlated with serum levels of Aβ40, Aβ42 and total Aβ [29]. In conclusion, the existing evidence on AD pathological biomarkers supports OSA as a risk factor of cognitive impairments.
Cognitive performance improved with the CPAP treatment
Continuous positive airway pressure (CPAP) is the standard and effective treatment for patients with OSA [30]. The CPAP can significantly improve cognitive performance in patients with OSA [2]. For example, elderly patients with severe OSA who presented with cognitive impairments could benefit from CPAP treatment [31]. Improvements in executive functions, intelligence, and memory have been seen in patients with OSA receiving CPAP treatment [12]. In patients with severe OSA, CPAP therapy was beneficial on patients’ occupational well-being and job productivity [32]. Interestingly, CPAP treatment may also delay cognitive deteriorations in patients with OSA [33]. However, there are some limitations with CPAP treatment. For example, CPAP is not indicated in patients with an apnea/hypopnea index (AHI) of ≥ 30 who have no subjective daytime sleepiness [34]. Some cognitive deficits including working memory, attention, executive function, and psychomotor speed were found to be resistant to CPAP treatment in patients with OSA [10]. For instance, immediate memory was the only cognitive function that had been improved with the CPAP therapy [13].
Duration of CPAP treatment is crucial
After patients with OSA received CPAP treatment for 12 months, executive function, memory and reactive time were significantly improved [2] (Table 2). Cognitive dysfunction in patients with OSA could be at least partially reversed using 6-month-long CPAP therapy [35]. For example, alertness and continuous attention were noted to be significantly improved after a 6-month course of CPAP treatment [5]. OSA patients were found to have most of their executive and learning disabilities normalized after using CPAP treatments for 4–6 months [16]. For those with OSA, even a 3-month course of CPAP treatment showed a significant improvement on MMSE scores [7], episodic and short-term memory, as well as executive function [31]. In patients with severe OSA, CPAP treatment for 3 months resulted in a significant improvement in cognitive functions related to concentration and memory [36]. For AD patients with severe OSA (an AHI ≥ 30), CPAP treatment for 3 months was associated with a significantly slower cognitive decline than the control group (no CPAP treatment) during a follow-up of 3 years [37]. Although 1 month of CPAP treatment can lead to improved verbal episodic memory in patients with OSA [38], the therapeutic effects of CPAP could not be observed anymore when an even shorter duration (< 4 weeks) is used. For example, 2 weeks of CPAP or oxygen-supplementation treatment was insufficient to show beneficial cognitive effects [39]. A comparison of subjects randomized to 3 weeks of therapeutic versus placebo CPAP had no significant improvements in cognition for patients with AD and OSA [18]. Therefore, the duration of CPAP therapy is a crucial factor for improving the cognitive performance/functions in patients with OSA. It is also worthy to note that some domains of cognitive function might not be as sensitive to CPAP treatment as others [14].
By directly addressing the possible underlying causes for the pathological changes seen in patients with OSA including hypoxia, hypercapnia, and poor sleep quality, CPAP has proven to be effective in improving the associated impaired cognitive functions. CPAP treatment has been shown to increase the connectivity of the default mode network and attenuate cortical thinning [31]. More specifically, an increase in the connectivity was seen in the right middle frontal gyrus after 3 months of CPAP treatment [31]. Further, 12 months of CPAP treatment almost completely reversed white matter abnormalities [40]. More interestingly, significant improvements involving attention, executive function, and memory actually paralleled white matter changes for the therapeutic effects of CPAP [40].
In conclusion, patients with OSA are more likely to develop cognitive impairments. A minimal therapeutic duration of 4 weeks is needed if CPAP was used to treat patients with OSA for associated cognitive impairments or deficits. The underlying mechanism for cognitive impairments seen in patients with OSA need be investigated further for making more specific therapeutic treatments. It is also important for practitioners to properly educate their patients about CPAP therapy and emphasize its potential benefits on preventive measures against cognitive deterioration processes. Lastly, patients that initially present with signs of cognitive deficits would likely benefit from a screening sleep test, possibly more from an instrumental study though it might not be available in a lot of countries.
References
Sharafkhaneh A, Giray N, Richardson P, Young T, Hirshkowitz M (2005) Association of psychiatric disorders and sleep apnea in a large cohort. Sleep 28:1405–1411
Ng SS, Chan TO, To KW, Chan KK, Ngai J, Tung A, Ko FW, Hui DS (2015) Prevalence of obstructive sleep apnea syndrome and CPAP adherence in the elderly Chinese population. PLoS ONE 10:e0119829
Heinzer R, Vat S, Marques-Vidal P, Marti-Soler H, Andries D, Tobback N, Mooser V, Preisig M, Malhotra A, Waeber G, Vollenweider P, Tafti M, Haba-Rubio J (2015) Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med 3:310–318
Foley DJ, Masaki K, White L, Larkin EK, Monjan A, Redline S (2003) Sleep-disordered breathing and cognitive impairment in elderly Japanese-American men. Sleep 26:596–599
Kotterba S, Rasche K, Widdig W, Duscha C, Blombach S, Schultze-Werninghaus G, Malin JP (1998) Neuropsychological investigations and event-related potentials in obstructive sleep apnea syndrome before and during CPAP-therapy. J Neurol Sci 159:45–50
Blackwell T, Yaffe K, Laffan A, Redline S, Ancoli-Israel S, Ensrud KE, Song Y, Stone KL (2015) Associations between sleep-disordered breathing, nocturnal hypoxemia, and subsequent cognitive decline in older community-dwelling men: the Osteoporotic Fractures in Men Sleep Study. J Am Geriatr Soc 63:453–461
Kanbay A, Demir NC, Tutar N, Köstek O, Özer Şimşek Z, Buyukoglan H, Demir R, Parrino L (2017) The effect of CPAP therapy on insulin-like growth factor and cognitive functions in obstructive sleep apnea patients. Clin Respir J 11:506–513
Chen R, Xiong KP, Huang JY, Lian YX, Jin F, Li ZH, Zhao MY, Liu CF (2011) Neurocognitive impairment in Chinese patients with obstructive sleep apnoea hypopnoea syndrome. Respirology 16:842–848
Yaffe K, Laffan AM, Harrison SL, Redline S, Spira AP, Ensrud KE, Ancoli-Israel S, Stone KL (2011) Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA 306:613–619
Lau EY, Eskes GA, Morrison DL, Rajda M, Spurr KF (2010) Executive function in patients with obstructive sleep apnea treated with continuous positive airway pressure. J Int Neuropsychol Soc 16:1077–1088
Yamout K, Goldstein FC, Lah JJ, Levey AI, Bliwise DL (2012) Neurocognitive correlates of nocturnal oxygen desaturation in a memory clinic population. J Clin Exp Neuropsychol 34:325–332
Liguori C, Mercuri NB, Izzi F, Romigi A, Cordella A, Sancesario G, Placidi F (2017) Obstructive sleep apnea is associated with early but possibly modifiable Alzheimer's disease changes. Sleep 40:1–10
Jurádo-Gámez B, Guglielmi O, Gude F, Buela-Casal G (2016) Effects of continuous positive airway pressure treatment on cognitive functions in patients with severe obstructive sleep apnoea. Neurologia 31:311–318
Muñoz A, Mayoralas LR, Barbé F, Pericás J, Agusti AG (2000) Long-term effects of CPAP on daytime functioning in patients with sleep apnoea syndrome. Eur Respir J 15:676–681
Torelli F, Moscufo N, Garreffa G, Placidi F, Romigi A, Zannino S, Bozzali M, Fasano F, Giulietti G, Djonlagic I, Malhotra A, Marciani MG, Guttmann CR (2011) Cognitive profile and brain morphological changes in obstructive sleep apnea. Neuroimage 54:787–793
Naegele B, Pepin JL, Levy P, Bonnet C, Pellat J, Feuerstein C (1998) Cognitive executive dysfunction in patients with obstructive sleep apnea syndrome (OSAS) after CPAP treatment. Sleep 21:392–397
Mant A, Saunders NA, Eyland AE, Pond CD, Chancellor AH, Webster IW (1988) Sleep-related respiratory disturbance and dementia in elderly females. J Gerontol 43:M140–144
Ancoli-Israel S, Palmer BW, Cooke JR, Corey-Bloom J, Fiorentino L, Natarajan L, Liu L, Ayalon L, He F, Loredo JS (2008) Cognitive effects of treating obstructive sleep apnea in Alzheimer's disease: a randomized controlled study. J Am Geriatr Soc 56:2076–2081
Bliwise DL, Yesavage JA, Tinklenberg JR, Dement WC (1989) Sleep apnea in Alzheimer's disease. Neurobiol Aging 10:343–346
Hoch CC, Reynolds CF, Kupfer DJ, Houck PR, Berman SR, Stack JA (1986) Sleep-disordered breathing in normal and pathologic aging. J Clin Psychiatry 47:499–503
Djonlagic I, Guo M, Matteis P, Carusona A, Stickgold R, Malhotra A (2014) Untreated sleep-disordered breathing: links to aging-related decline in sleep-dependent memory consolidation. PLoS ONE 9:e85918
Aoki K, Matsuo M, Takahashi M, Murakami J, Aoki Y, Aoki N, Mizumoto H, Namikawa A, Hara H, Miyagawa M, Kadotani H, Yamada N (2014) Association of sleep-disordered breathing with decreased cognitive function among patients with dementia. J Sleep Res 23:517–523
O'Hara R, Schröder CM, Kraemer HC, Kryla N, Cao C, Miller E, Schatzberg AF, Yesavage JA, Murphy GM (2005) Nocturnal sleep apnea/hypopnea is associated with lower memory performance in APOE epsilon4 carriers. Neurology 65:642–644
Lutsey PL, Misialek JR, Mosley TH, Gottesman RF, Punjabi NM, Shahar E, MacLehose R, Ogilvie RP, Knopman D, Alonso A (2018) Sleep characteristics and risk of dementia and Alzheimer's disease: the atherosclerosis risk in communities study. Alzheimers Dement 14:157–166
Buratti L, Viticchi G, Falsetti L, Cagnetti C, Luzzi S, Bartolini M, Provinciali L, Silvestrini M (2014) Vascular impairment in Alzheimer's disease: the role of obstructive sleep apnea. J Alzheimers Dis 38:445–453
Yun CH, Lee HY, Lee SK, Kim H, Seo HS, Bang SA, Kim SE, Greve DN, Au R, Shin C, Thomas RJ (2017) Amyloid burden in obstructive sleep apnea. J Alzheimers Dis 59:21–29
Ju YE, Finn MB, Sutphen CL, Herries EM, Jerome GM, Ladenson JH, Crimmins DL, Fagan AM, Holtzman DM (2016) Obstructive sleep apnea decreases central nervous system-derived proteins in the cerebrospinal fluid. Ann Neurol 80:154–159
Sharma RA, Varga AW, Bubu OM, Pirraglia E, Kam K, Parekh A, Wohlleber M, Miller MD, Andrade A, Lewis C, Tweardy S, Buj M, Yau PL, Sadda R, Mosconi L, Li Y, Butler T, Glodzik L, Fieremans E, Babb JS, Blennow K, Zetterberg H, Lu SE, Badia SG, Romero S, Rosenzweig I, Gosselin N, Jean-Louis G, Rapoport DM, de Leon MJ, Ayappa I, Osorio RS (2018) Obstructive sleep apnea severity affects amyloid burden in cognitively normal elderly. a longitudinal study. Am J Respir Crit Care Med 197:933–943
Bu XL, Liu YH, Wang QH, Jiao SS, Zeng F, Yao XQ, Gao D, Chen JC, Wang YJ (2015) Serum amyloid-beta levels are increased in patients with obstructive sleep apnea syndrome. Sci Rep 5:1–8
Engleman HM, McDonald JP, Graham D, Lello GE, Kingshott RN, Coleman EL, Mackay TW, Douglas NJ (2002) Randomized crossover trial of two treatments for sleep apnea/hypopnea syndrome: continuous positive airway pressure and mandibular repositioning splint. Am J Respir Crit Care Med 166:855–859
Dalmases M, Solé-Padullés C, Torres M, Embid C, Nuñez MD, Martínez-Garcia MÁ, Farré R, Bargalló N, Bartrés-Faz D, Montserrat JM (2015) Effect of CPAP on cognition, brain function, and structure among elderly patients with OSA: a randomized pilot study. Chest 148:1214–1223
Jurádo-Gámez B, Guglielmi O, Gude-Sampedro F, Buela-Casal G (2015) Effect of CPAP therapy on job productivity and psychosocial occupational health in patients with moderate to severe sleep apnea. Sleep Breath 19:1293–1299
Osorio RS, Gumb T, Pirraglia E, Varga AW, Lu SE, Lim J, Wohlleber ME, Ducca EL, Koushyk V, Glodzik L, Mosconi L, Ayappa I, Rapoport DM, de Leon MJ (2015) Sleep-disordered breathing advances cognitive decline in the elderly. Neurology 84:1964–1971
Barbé F, Mayoralas LR, Duran J, Masa JF, Maimó A, Montserrat JM, Monasterio C, Bosch M, Ladaria A, Rubio M, Rubio R, Medinas M, Hernandez L, Vidal S, Douglas NJ, Agustí AG (2001) Treatment with continuous positive airway pressure is not effective in patients with sleep apnea but no daytime sleepiness. a randomized, controlled trial. Ann Intern Med 134:1015–1023
Wu SQ, Liao QC, Xu XX, Sun L, Wang J, Chen R (2016) Effect of CPAP therapy on C-reactive protein and cognitive impairment in patients with obstructive sleep apnea hypopnea syndrome. Sleep Breath 20:1185–1192
Borak J, Cieślicki JK, Koziej M, Matuszewski A, Zieliński J (1996) Effects of CPAP treatment on psychological status in patients with severe obstructive sleep apnoea. J Sleep Res 5:123–127
Troussière AC, Charley CM, Salleron J, Richard F, Delbeuck X, Derambure P, Pasquier F, Bombois S (2014) Treatment of sleep apnoea syndrome decreases cognitive decline in patients with Alzheimer's disease. J Neurol Neurosurg Psychiatry 85:1405–1408
Rosenzweig I, Glasser M, Crum WR, Kempton MJ, Milosevic M, McMillan A, Leschziner GD, Kumari V, Goadsby P, Simonds AK, Williams SC, Morrell MJ (2016) Changes in neurocognitive architecture in patients with obstructive sleep apnea treated with continuous positive airway pressure. EBioMedicine 7:221–229
Lim W, Bardwell WA, Loredo JS, Kim EJ, Ancoli-Israel S, Morgan EE, Heaton RK, Dimsdale JE (2007) Neuropsychological effects of 2-week continuous positive airway pressure treatment and supplemental oxygen in patients with obstructive sleep apnea: a randomized placebo-controlled study. J Clin Sleep Med 3:380–386
Castronovo V, Scifo P, Castellano A, Aloia MS, Iadanza A, Marelli S, Cappa SF, Strambi LF, Falini A (2014) White matter integrity in obstructive sleep apnea before and after treatment. Sleep 37:1465–1475
Author information
Authors and Affiliations
Contributions
All the authors contributed to data analysis and interpretation, draft and critical revision of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Wang, G., Goebel, J.R., Li, C. et al. Therapeutic effects of CPAP on cognitive impairments associated with OSA. J Neurol 267, 2823–2828 (2020). https://doi.org/10.1007/s00415-019-09381-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09381-2