Abstract
MRI is the primary screening tool for patients with myelopathy. The decision to obtain additional imaging, notably spinal angiography, is generally based on initial MRI findings. This study retrospectively analyzed the yield of initial MRI in a cohort of patients with angiographically confirmed vascular malformations. MRI obtained at symptom onset was available in 115 patients with either high-flow (29 cases) or low-flow (86 cases) vascular malformations. MRI was classified as “positive” when the report mentioned a vascular malformation or “negative” when considered normal or when another diagnosis was suggested. Initial MRI was positive in 61 patients (53.0%), correctly identifying 28 high-flow (96.6%) but only 33 low-flow (38.4%) lesions. Flow voids were noted in 96.6% of the high-flow lesions and 38.4% of the low-flow ones. T2-signal anomalies (77.4%) and parenchymal enhancement (54.5%) were also common in low-flow anomalies. Patients with negative MRI had an average delay of 111 days before angiography and 239 days before therapy; these intervals were 27 and 76 days for those with positive MRIs. In summary, MRI shows a high yield for high-flow vascular malformations, i.e., characterized by prominent flow voids on T2-weighted images, but misdiagnosed over 60% of low-flow lesions. The percentage of correctly identified anomalies matched the percentage of observed flow voids in both groups, indicating over-reliance on this sign for the diagnosis of slow-flow lesions. MRI findings in slow-flow vascular malformation overlap with other conditions, notably transverse myelitis, which was initially misattributed to 40% of the slow-flow lesions in our cohort.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Spinal vascular malformations (SVMs) represent a heterogeneous and underdiagnosed group of vascular lesions currently estimated to account for up to 9% of all vascular malformations of the central nervous system [1, 2]. SVMs can be divided into two categories based on their flow pattern. Low-flow lesions are the most common (60–80% of all SVMs [3–5]). They include spinal dural arteriovenous fistulas (SDAVF), acquired epidural arteriovenous fistulas (SEAVF) and low-flow perimedullary arteriovenous fistulas (PmAVF, Merland Type I). Patients with low-flow lesions are typically older men presenting with progressive myelopathy secondary to spinal venous hypertension (SVH), with or without superimposed arterial ischemia [6].
High-flow anomalies include spinal arteriovenous malformation (SAVM) as well as high-flow PmAVFs (Merland Type II and III), congenital SEAVFs and paraspinal arteriovenous fistulas (ParAVF). Generally seen in younger patients, these lesions may remain asymptomatic or present with cardiac insufficiency (in small children mostly), hematomyelia, subarachnoid and/or parenchymal hemorrhage, cord compression or, less commonly, SVH. High-flow spinal arteriovenous fistulas can be associated with other vascular anomalies [7], and are not infrequently diagnosed incidentally during the work-up of complex vascular syndromes.
Spinal digital subtraction angiography (SpDSA)—the gold standard imaging modality for the spinal vasculature [8–10]—plays an essential role in the diagnosis and treatment of SVMs [9, 11]. MRI is the primary screening tool for patients with myelopathic symptoms and is heavily relied upon when assessing the need for further investigation with SpDSA. However, findings specific for SVMs on MRI—notably the presence of intra- or perimedullary flow voids—can be absent while intramedullary T2 signal abnormality, cord expansion and parenchymal enhancement can also be seen with conditions such as transverse myelitis (TM), neoplasia or ischemia [12–15]. While favorable SVM treatment outcomes depend for a large part upon early recognition, notably when considering low-flow lesions, accurate diagnosis is often delayed for months or years, even in patients undergoing multiple MRI studies [10, 16]. The purpose of this work was to analyze the yield of conventional MRI as a screening tool in a cohort of 115 patients with SVMs subsequently diagnosed by angiography.
Materials and methods
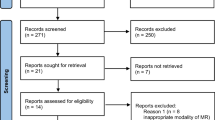
The charts of patients with angiographically confirmed SVMs seen at our institution between March 2006 and November 2016 were reviewed (IRB approved database, additional permission obtained for publication). Patients were included in this study when the imaging data and report of an initial conventional MRI study were available for analysis; 115 of the 123 reviewed patients satisfied this criterion, 83 men (72.2%) and 32 women (27.3%), with an average age of 50.6 years (median: 57 years, range 0.2–88).
Conventional magnetic resonance imaging
Conventional MRI was defined as a set of axial and sagittal T1 and T2-weighted sequences, generally including STIR and post-gadolinium images as well. An MRI study was classified as “positive” when the report mentioned an SVM or when SpDSA was recommended, or “negative” when the study was either considered normal or a diagnosis other than SVM was suggested. The time interval between the initial MRI and either endovascular or surgical treatment—when performed—was recorded.
The following characteristics recorded:
-
(a)
Extent of medullary T2 hyperintensity: absent, focal (less than 3 vertebral segment) or extensive (3 or more vertebral segments),
-
(b)
Spinal cord expansion: present or absent,
-
(c)
Parenchymal enhancement after gadolinium administration: present or absent,
-
(d)
Flow voids (dilated intramedullary or perimedullary vessels): present or absent.
Spinal digital subtraction angiography (SpDSA)
SpDSA was obtained in all patients at our institution. SVMs were classified as “high-flow” or “low-flow” following the scheme discussed in the introduction. In patients with multiple SVMs, the lesion with the highest flow pattern—i.e., the most obvious one on non-invasive imaging—was used for analysis.
Results
Overall MRI analysis
Conventional MRI was obtained in various academic and non-academic settings using different equipment and techniques. Initial reports were positive in 61 patients (53.0%) and negative in 54 (47.0%). The reported diagnoses for these initial studies are listed in Table 1. The most common MRI finding was parenchymal T2 hyperintensity noted in 79/113 (69.9%) patients, including 67 patients with extensive involvement (84.8%) and 12 with focal lesions (15.2%). Spinal cord expansion was present in 27/113 patients (23.9%). Flow voids were noted in 61 cases (53.0%), of which 22 (36.7%) had a normal cord appearance; 8 of these 22 (36.4%) were low-flow lesions. Parenchymal enhancement was noted in 50 of the 103 patients who received gadolinium (48.5%).
Angiographic SVM characterization and treatment
The angiographic diagnoses are listed in Table 2. Sixty SVMs were thoracic in location (52.2%), 35 lumbosacral (30.4%) and 17 cervical (14.8%). Two were at the cervicothoracic junction (1.7%) and one at the thoracolumbar junction (0.9%).
The average interval between initial MRI and SpDSA was 67 days (median 28, range 0–618). A therapeutic intervention (endovascular or surgical) was performed in 89 patients (77.4%) with an average interval of 155 days (median 72, range 0–1197) between initial MRI and treatment.
Patients with an initially negative MRI had an average delay of 111 days before diagnostic angiography (median 70, range 0–618) and—for those treated—239 days before therapy (median 160, range 0–1197); these intervals were, respectively, of 27 days (median 13, range 0–131) and 76 days (median 32, range 0–761) for those with positive MRIs.
MRI in high-flow and low-flow SVMs
Eighty-six patients (74.9%) had low-flow SVMs, including 68 men (79.1%) and 18 women (20.0%) with an average age of 57.9 years (median 60.5, range 6–88). Twenty-nine patients had high-flow SVMs (25.2%), including 15 men (51.7%) and 14 women (48.3%) with an average age of 29 years (median 21, range 0.2–71). The initial MRI for the 86 patients with low-flow SVMs was positive in 33 cases (38.4%); in the high-flow group, 28 patients had a positive initial MRI (96.6%), with only one negative case.
The MRI findings distinguishing the two groups of SVMs are summarized in Table 3. Flow voids were noted in 38.4% of the low-flow lesions and 96.6% of the high-flow ones. T2-signal anomalies were more common with low-flow SVMs (77.4 vs. 48.3.0%), with a tendency to be extensive in that group and focal with high-flow lesions. Parenchymal enhancement was also more common with low-flow lesions (54.5 vs. 30.8%).
Case illustrations
Two cases have been selected to illustrate low-flow and high-flow categories based on the analysis of our cohort.
Case 1—2-year-old girl undergoing investigations for a perirectal and right perineal arteriovenous malformation, with incidental discovery of a perimedullary arteriovenous fistula (Merland Type II). The lesion was identified by MRI (positive MRI), which documented prominent flow voids and a mildly dilated central canal without parenchymal signal anomalies, swelling or enhancement (Fig. 1a). SpDSA was obtained to characterize the lesion and plan management (Fig. 1c).
A 2-year-old girl with a perimedullary arteriovenous fistula (PmAVF Merland Type II) discovered during the work-up of a congenital vascular syndrome. a MRI, T2-weighted image, sagittal plane. The lesion is characterized by dilated perimedullary vessels, notably on the anterior aspect of the cord, appearing as prominent flow voids (arrows). The central canal is slightly enlarged, but there is no parenchymal signal anomaly and no enhancement after gadolinium administration (not shown). Note the presence of a pelvic and perineal vascular malformation (asterisk). b DSA, right injection, posteroanterior projection, early arterial phase, showing a dilated anterior radiculomedullary artery (artery of Adamkiewicz; black arrow) supplying a high-flow perimedullary arteriovenous shunt via the anterior spinal artery (arrowheads); the white arrow points at the early opacification of a small venous aneurysm located on the venous side of the shunt, characteristic of a PmAVF Type II. c DSA, right injection, posteroanterior projection, early venous phase, documenting fast opacification of a diffusely enlarged perimedullary venous system. The venous aneurysm is still visible (white arrow)
Case 2—73-year-old woman with a 10-month history of progressive lower extremity weakness with urinary incontinence and constipation. MRI showed extensive T2 hyperintensity extending from T1 to the conus medullaris, with cord expansion and diffuse enhancement but no flow voids (Fig. 2a–e). She was initially diagnosed with TM (negative MRI), but progression of the leg weakness and incontinence as well as the new onset of bilateral hand numbness and truncal ataxia in spite of medical management led to admission at our institution. At that time, she was unable to stand-up or walk, and her neurological exam only showed minimal anti-gravity strength in both lower extremities (Aminoff–Logue score: 5 + 3+2 = 10). SpDSA revealed a lumbar SEAVF subsequently treated endovascularly (Fig. 2f–g). At the 2-month follow-up visit, the urinary retention and constipation had improved while the truncal ataxia had resolved; her strength also improved, allowing her to stand-up and take a few steps with unaided (Aminoff–Logue score: 4 + 1+1 = 6). Her lower extremity strength continued to get better until she was able to walk with the help of a cane and perform daily activities unaided (Aminoff–Logue score: 3 + 1+1 = 5). She passed away from an unrelated disease 4 years later.
A 73-year-old woman with leg weakness and a lumbar spinal epidural arteriovenous fistula (SEAVF). a Thoracic MRI, T1-weighted image, sagittal plane. Note diffuse central medullary hypointensity consistent with severe spinal cord edema. b Thoracic MRI, T2-weighted image, sagittal plane, confirming the presence of central cord edema extending from the conus to the C7-T1 level, without detectable flow voids. c Thoracic MRI, T1-weighted image after gadolinium injection, sagittal plane, showing diffuse medullary enhancement, more pronounced at the conus medullaris level, but without clear perimedullary vascular enhancement. d Lumbar MRI, T2-weighted image, sagittal plane, documenting edema extension to the tip of the conus medullaris without identifiable perimedullary flow voids. e Lumbar MRI, T2-weighted image, T1-weighted image after gadolinium injection, sagittal plane, confirming the absence of perimedullary or radiculomedullary enhancement. f DSA, bilateral L4 trunk injection, posteroanterior projection, arterial phase; an isolated epidural venous pouch extending over the L3 and L4 levels (arrowheads) is visible during the arterial phase, with retrograde opacification of a left L3 radiculomedullary vein (arrows). This appearance is characteristic of an SEAVF. g DSA, bilateral L4 injection, posteroanterior projection, venous phase; the perimedullary venous system draining the SEAVF is diffusely congested, with the absence of normal lumbar or thoracic radiculomedullary veins, a finding typical of slow-flow arteriovenous fistulas
Discussion
Demographic and angiographic characteristics of the studied cohort
The studied cohort included 86 low-flow and 29 high-flow SVMs. Most low-flow lesions were seen in older men while patients with high-flow lesions were younger and without gender bent. These demographic characteristics and the relative distribution of lesions are consistent with published data [17, 18]; the cohort is, therefore, clinically representative.
Yield of initial MRI in patients with spinal vascular malformations
An analysis of initial conventional MRI in 115 patients with subsequently documented SVMs showed an overall accuracy rate of 53.0%. The yield of MRI for high-flow lesions—which are associated with prominent intra- and/or perimedullary vessels responsible for conspicuous flow voids on T2-weighted images—was predictably high (96.6%). The single negative report in that group was also the only one not mentioning flow voids: the patient presented with a subarachnoid hemorrhage, which might have obscured the presence of flow voids on the initial MRI study.
On the other hand, initial MRIs in patients with low-flow lesions—by far the most common SVMs—were only positive in 38.4%. This figure likely represents a considerable underestimation of the actual number of patients with low-flow lesions and negative MRIs, since a negative MRI is generally believed to obviate the need for further evaluation with angiography, therefore decreasing the prospect of accurate diagnosis for these patients.
The fact that the accuracy rates for both types of SVMs matched exactly the rates of detection of flow voids (96.6 and 38.4% for high-flow and low-flow lesions, respectively) emphasizes the importance attached to this finding during image interpretation. However, our review shows that, contrary to a relatively common assumption, the lack of flow voids has a low negative predictive value for patients with low-flow SVMs.
Falsely negative MRIs in patients with SVMs led to delayed angiographic diagnosis and treatment. The median time to angiography was 13 days for patients with a positive MRI and 70 days for those investigated by angiography in spite of a negative initial report. The median time interval before endovascular or surgical treatment was 32 and 160 days, respectively. The extensive period of time elapsed between angiography and treatment in some patients was caused by the additional interference of falsely negative initial spinal angiograms.
This study is based on a cohort of patients with diagnosis confirmed by angiography. It, therefore, provides no information with regard to the number of patients with undiagnosed SVMs. This population includes patients with negative MRI and no angiographic evaluation as well as patients misdiagnosed after a falsely negative spinal angiogram.
Thirty-four of the 54 patients (63%) with SVMs and negative initial MRI were initially diagnosed with TM. Patients with low-flow lesions are particularly at risk to be misdiagnosed since, based on our findings, their typical MRI presentation includes a longitudinally extensive myelopathy (72.1%) with parenchymal enhancement (54.5%) and no flow voids (61.6%), a set of characteristics overlapping the diagnostic criteria for TM [19]. Other MRI findings reported in TM, such as centrally located T2 hyperintensity and cord expansion [13, 20], were also noted in our patients with low-flow lesions.
Role of advanced non-invasive imaging and SpDSA in evaluation of SVMs
This study only looked at the yield of conventional MRI studies, which currently constitutes the principal screening tool for patients presenting with myelopathy. Advanced MRI techniques, such as time-resolved contrast enhanced MRA (CE-MRA), have shown significant promises for the detection of SVMs [21–23], with reported sensitivity rates ranging between 81% [23] and 100% [22]. However, most studies involve small samples and do not clearly separate SVMs into low- and high-flow categories, which present—as shown in our review—different diagnostic challenges. A study specifically addressing the role of CE-MRA for the localization of SDAVFs showed a detection rate of 81% [23]. That study also reported flow voids as the most constant anomaly on conventional MRI (seen in all 50 patients with retrievable information, out of a total of 53), a finding probably indicating that patients who underwent CE-MRA were selected based on the presence of flow voids (a group accounting for <40% of the low-flow lesions in our cohort). The efficacy of CE-MRA for the detection of low-flow lesions without flow voids on conventional MRI has, to our knowledge, not been addressed.
The impact of advanced MRI techniques such as CE-MRA for the screening of patients with myelopathy remains unclear. A study of 154 patients with SDAVFs divided into early (1986–1999) and recent (2000–2008) cohorts showed no difference in the time interval between symptom onset and diagnosis in spite of the recent introduction of modern imaging [10]. Yet, a wider use of advanced MRI techniques in patients with suspected vascular myelopathies should increase our ability to detect low-flow lesions and allow earlier diagnoses if those patients are not misrouted based on the lack of specificity of their initial MRI findings.
A weakness of our study, besides the fact that it specifically analyzed patients with angiographically proven lesions, lies in the lack of technical homogeneity of the reviewed MRI data. Studies were performed in various academic and non-academic settings using different machines and techniques. This heterogeneity should, however, have little impact on our findings as conventional MRI was a well standardized and routinely obtained study during the time period covered by our review, as opposed for example to less-standardized complex MRA methods or to operator-dependent angiography techniques. In addition, our review analyzed MRI reports rather than actual MRI studies. However, we believe that, precisely for these reasons, our cohort is representative of the heterogeneous imaging data available to neurologists who screen patients with myelopathy and, therefore, clinically relevant. By suggesting that initial MRI reports should be considered with caution, our study re-emphasizes the critical role played by the clinical presentation in the management of patients with myelopathies.
Conclusion
The separation of SVMs into high- and low-flow lesions has important diagnostic implications. In our review, conventional MRI successfully identified 96.6% of the high-flow SVMs but less than 40% of the low-flow ones. These observations are based on a cohort of patients with angiographically proven SVMs. Since patients with a negative MRI are less likely to undergo angiography, our statistics likely underestimate the number of patients with SVMs and negative MRIs who remain misdiagnosed, notably in the low-flow group.
The rate of SVM identification matched exactly the rate of observed flow voids on T2-weighted images in both groups. Over-reliance on this finding for the screening of patients who would benefit from further imaging (e.g., CE-MRA or SpDSA) seems to represent a major hurdle for the diagnosis of low-flow SVMs.
Neurologists and other clinicians evaluating patients with myelopathies should be aware that a negative MRI report and/or the absence of flow voids on MRI do not rule out a vascular etiology, notably the presence of a low-flow SVM such as a dural or epidural arteriovenous fistula. Considering the extremely low risk of complication of modern SpDSA [24] and the potential for positive treatment outcomes even in paraplegic patients, we agree with Cosnard’s recommendation that “medullary arteriography and treatment should be widely indicated, even in elderly patients with many problems” [15].
References
Rangel-Castilla L, Russin JJ, Zaidi HA, Martinez-Del-Campo E, Park MS, Albuquerque FC, McDougall CG, Nakaji P, Spetzler RF (2014) Contemporary management of spinal AVFs and AVMs: lessons learned from 110 cases. Neurosurg Focus 37(3):E14. doi:10.3171/2014.7.FOCUS14236
Flores BC, Klinger DR, White JA, Batjer HH (2016) Spinal vascular malformations: treatment strategies and outcome. Neurosurg Rev. doi:10.1007/s10143-016-0713-z
Gilbertson JR, Miller GM, Goldman MS, Marsh WR (1995) Spinal dural arteriovenous fistulas: MR and myelographic findings. AJNR Am J Neuroradiol 16(10):2049–2057
Özkan N, Kreitschmann-Andermahr I, Goerike SL, Wrede KH, Kleist B, Stein KP, Gembruch O, Sandalcioglu IE, Wanke I, Sure U (2015) Single center experience with treatment of spinal dural arteriovenous fistulas. Neurosurg Rev 38(4):683–692. doi:10.1007/s10143-015-0645-z
Lanzino G, D’Urso PI, Kallmes DF, Cloft HJ (2012) Onyx embolization of extradural spinal arteriovenous malformations with intradural venous drainage. Neurosurgery 70(2):329–333. doi:10.1227/NEU.0b013e318230929e
Merland JJ, Riche MC, Chiras J (1980) Intraspinal extramedullary arteriovenous fistulae draining into the medullary veins. J Neuroradiol 7(4):271–320
Thiex R, Mulliken JB, Revencu N, Boon LM, Burrows PE, Cordisco M, Dwight Y, Smith ER, Vikkula M, Orbach DB (2010) A novel association between RASA1 mutations and spinal arteriovenous anomalies. AJNR Am J Neuroradiol 31(4):775–779. doi:10.3174/ajnr.A1907
Saraf-Lavi E, Bowen BC, Quencer RM, Sklar EM, Holz A, Falcone S, Latchaw RE, Duncan R, Wakhloo A (2002) Detection of spinal dural arteriovenous fistulae with MR imaging and contrast-enhanced MR angiography: sensitivity, specificity, and prediction of vertebral level. AJNR Am J Neuroradiol 23(5):858–867
Koch C (2006) Spinal dural arteriovenous fistula. Curr Opin Neurol 19(1):69–75
Saladino A, Atkinson JL, Rabinstein AA, Piepgras DG, Marsh WR, Krauss WE, Kaufmann TJ, Lanzino G (2010) Surgical treatment of spinal dural arteriovenous fistulae: a consecutive series of 154 patients. Neurosurgery 67(5):1350–1357. doi:10.1227/NEU.0b013e3181ef2821 (discussion 1357–1358)
Eckart Sorte D, Obrzut M, Wyse E, Gailloud P (2016) Normal venous phase documented during angiography in patients with spinal vascular malformations: incidence and clinical implications. AJNR Am J Neuroradiol 37(3):565–571. doi:10.3174/ajnr.A4601
Mirbagheri S, Eckart Sorte D, Zamora CA, Mossa-Basha M, Newsome SD, Izbudak I (2016) Evaluation and management of longitudinally extensive transverse myelitis: a guide for radiologists. Clin Radiol 71(10):960–971. doi:10.1016/j.crad.2016.05.020
Choi KH, Lee KS, Chung SO, Park JM, Kim YJ, Kim HS, Shinn KS (1996) Idiopathic transverse myelitis: MR characteristics. AJNR Am J Neuroradiol 17(6):1151–1160
Kumral E, Polat F, Güllüoglu H, Uzunköprü C, Tuncel R, Alpaydin S (2011) Spinal ischaemic stroke: clinical and radiological findings and short-term outcome. Eur J Neurol 18(2):232–239. doi:10.1111/j.1468-1331.2010.02994.x
Cosnard G (2012) Tips and traps in spinal cord pathology. Diagn Interv Imaging 93(12):975–984. doi:10.1016/j.diii.2012.08.003
Jellema K, Canta LR, Tijssen CC, van Rooij WJ, Koudstaal PJ, van Gijn J (2003) Spinal dural arteriovenous fistulas: clinical features in 80 patients. J Neurol Neurosurg Psychiatry 74(10):1438–1440
Rosenblum B, Oldfield EH, Doppman JL, Di Chiro G (1987) Spinal arteriovenous malformations: a comparison of dural arteriovenous fistulas and intradural AVM’s in 81 patients. J Neurosurg 67(6):795–802. doi:10.3171/jns.1987.67.6.0795
Symon L, Kuyama H, Kendall B (1984) Dural arteriovenous malformations of the spine. Clinical features and surgical results in 55 cases. J Neurosurg 60(2):238–247. doi:10.3171/jns.1984.60.2.0238
Transverse Myelitis Consortium Working G (2002) Proposed diagnostic criteria and nosology of acute transverse myelitis. Neurology 59(4):499–505
Harzheim M, Schlegel U, Urbach H, Klockgether T, Schmidt S (2004) Discriminatory features of acute transverse myelitis: a retrospective analysis of 45 patients. J Neurol Sci 217(2):217–223
Amarouche M, Hart JL, Siddiqui A, Hampton T, Walsh DC (2015) Time-resolved contrast-enhanced MR angiography of spinal vascular malformations. AJNR Am J Neuroradiol 36(2):417–422. doi:10.3174/ajnr.A4164
Unsrisong K, Taphey S, Oranratanachai K (2016) Spinal arteriovenous shunts: accuracy of shunt detection, localization, and subtype discrimination using spinal magnetic resonance angiography and manual contrast injection using a syringe. J Neurosurg Spine 24(4):664–670. doi:10.3171/2015.7.SPINE15319
Lindenholz A, TerBrugge KG, van Dijk JM, Farb RI (2014) The accuracy and utility of contrast-enhanced MR angiography for localization of spinal dural arteriovenous fistulas: the Toronto experience. Eur Radiol 24(11):2885–2894. doi:10.1007/s00330-014-3307-6
Chen J, Gailloud P (2011) Safety of spinal angiography: Complication rate analysis in 302 diagnostic angiograms. Neurology 77(13):1235–1240. doi:10.1212/WNL.0b013e3182302068
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
El Mekabaty, A., Pardo, C.A. & Gailloud, P. The yield of initial conventional MRI in 115 cases of angiographically confirmed spinal vascular malformations. J Neurol 264, 733–739 (2017). https://doi.org/10.1007/s00415-017-8419-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-017-8419-x