Abstract
Alemtuzumab is an anti-CD52 monoclonal antibody recently licensed for use in relapsing–remitting multiple sclerosis. Here, we report our experience of its use in neuromyelitis optica (NMO) spectrum disorders. A retrospective case review of patients treated with alemtuzumab in Cambridge, UK, was conducted to identify those who fulfil the criteria for NMO spectrum disorder. Three cases were identified. Case 1, 9-year-old female, presented with transverse myelitis and bilateral optic neuritis, with one lower medullary and several longitudinally extensive cord lesions. Despite immunosuppression including two courses of alemtuzumab, she continued to relapse, was wheelchair bound and registered blind by age 12, and died at age 18. Case 2, 41-year-old female, presented with bilateral optic neuritis and transverse myelitis with longitudinally extensive cervical cord lesions. Despite three courses of alemtuzumab, she had five relapses with visual impairment and new cord lesions. She later developed tumefactive white matter lesions and died aged 51. Case 3, 31-year-old female, presented with transverse myelitis with longitudinally extensive cervical cord lesions and positive aquaporin-4 antibody. After one course of alemtuzumab, she relapsed with 4 episodes of myelitis with new enhancing lesions and accumulating disability. She became relapse free after rituximab and mycophenolate mofetil. From this case series, we conclude that alemtuzumab failed to prevent disabling relapses and poor outcome in NMO. We hypothesise that rituximab is more effective, as in case 3, because it causes much more prolonged B lymphocyte depletion than alemtuzumab. We therefore caution against the use of alemtuzumab in NMO.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alemtuzumab is an anti-CD52 humanised monoclonal antibody recently approved in the European Union and by the US Food and Drug Administration as a therapeutic agent in relapsing–remitting multiple sclerosis (RRMS). Alemtuzumab induces a profound lymphopenia; reconstitution of the various lymphocyte subsets leads to prolonged modulation of the immune repertoire [1–3]. This leads to significant reductions in both relapse frequency and sustained accumulation of disability, compared to interferon beta-1a, in RRMS [4–6].
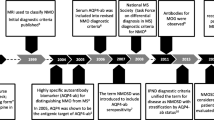
Neuromyelitis optica (NMO) spectrum disorders are a group of syndromes caused by antibodies, discovered in 2004 [7], targeting the aquaporin-4 water channel on astrocytic foot processes [8]. Alemtuzumab has occasionally been used to treat NMO, both before and after NMO was recognised as a distinct clinical entity. Here we report out experience.
Methods
We conducted a retrospective case review, from 1991 to the present day, of patients treated with alemtuzumab at the Department of Neurology in Addenbrooke’s Hospital, Cambridge, UK, to identify those patients who fulfil the criteria for NMO spectrum disorder under the revised Wingerchuk criteria [9] and the consensus criteria drawn up by the International Panel for NMO Diagnosis convened in 2011 [10]. The main outcome measures considered were relapse rate, accumulation of disability and long-term outcome after alemtuzumab treatment.
Results
In retrospect, three cases could be classified as neuromyelitis optica. One case (case 1) was from the 1990s; the remaining two were from the early 2000s.
Case 1
A 9-year-old girl presented in 1998 with protracted vomiting followed by transverse myelitis, two relapses of bilateral optic neuritis and two brainstem episodes (nystagmus, ataxia and facial sensory disturbance) within a year. Imaging showed one lower medullary and several longitudinally extensive cord lesions (images no longer available). Despite high-dose steroids and intensive immunosuppression (Table 1), she remained significantly visually impaired (acuities down to 6/60), as well as having a spastic paraparesis. She received alemtuzumab with no relapses for 12 months. At month 12, she relapsed with myelitis with longitudinally extensive thoracic cord demyelination and was retreated with alemtuzumab; only weeks later, a further relapse resulted in dense paraparesis, rendering her wheelchair bound. Her vision deteriorated further and she was registered blind by age 12. In 2005, her illness was recognised as antibody-mediated NMO [7] and she received plasma exchange (PLEX). She died at age 18, whilst awaiting rituximab treatment. Assays for aquaporin-4 immunoglobulin-G (AQP4-IgG) were not available at the time.
Case 2
A 41-year-old female presented in 2004 with bilateral optic neuritis and a brainstem deficit (left-sided horizontal nystagmus and ataxia) and two episodes of myelitis within 6 months; imaging showed enhancing brain and longitudinally extensive cervical cord lesions (Fig. 1a–c). She received pulsed high-dose steroids and remained with residual spastic paraparesis. Three cycles of alemtuzumab were administered 12 months apart. At months 3, 4 and 11 after the first cycle, she had discrete relapses attributable to new thoracic cord lesions (Fig. 1d), whilst cerebral lesions improved (not shown). At months 2 and 9 after second cycle, she relapsed with brainstem symptoms (vertigo and incoordination) and bilateral optic neuritis, with residual visual impairment (6/12). After the third cycle, she deteriorated with disabling cognitive deficits. She received rituximab, to no effect, later developing seizures and tumefactive white matter lesions (Fig. 1e, f). A brain biopsy performed to confirm active demyelination showed extensive loss of myelin with numerous CD68+ macrophages throughout, but the specific features of neuromyelitis optica were not sought. She went on to be treated with mitoxantrone with poor response. Late in the course of her illness, as the assay became available, she was tested for AQP4-IgG antibodies, which were absent. She died aged 51.
MRI images. Case 2: a pre-treatment T2-weighted axial views show high signal in posterior part of corpus callosum and left middle cerebellar peduncle. b T2-weighted sagittal view of cervical cord shows expansion with an extensive lesion from medulla to T1 level, and c gadolinium enhancement on T1-weighted image. d Post-treatment T2-weighted sagittal view shows new expansion of thoracic cord between T4 and T7 with increased T2 signal but no gadolinium enhancement. e T2-weighted axial images of brain (left) and FLAIR images (right) at month 20 after third dose of alemtuzumab show a large lesion in right parietal and posterior frontal white matter that extends to posterior corpus callosum and a smaller lesion in left parietal white matter. f Both lesions show an incomplete peripheral rim of enhancement on T1-weighted post-gadolinium axial image (left) and coronal image (right). Case 3: g pre-treatment T2-weighted sagittal MRI sequence (left) shows subtle expansion of cervical cord from C2 to C6 inclusive with diffuse increase in signal, more localised at level of C3/4 as demonstrated on axial view (right). h T1-weighed sagittal and axial sequences with gadolinium contrast show enhancement involving the left side of the cord. Worsening of disease at month 5 after alemtuzumab is shown by i T2-weighted sagittal views of spine showing progression of T2 signal change and swelling in cervical cord (left) and new thoracic hyperintensity extending from T2 to T7 (right); with gadolinium enhancement (j). k T2-weighted sagittal view of cord shows patchy increased intensity and evidence of cord atrophy, 7 years after disease onset
Case 3
A 31-year-old female presented in 2007 with two episodes of transverse myelitis with longitudinally extensive cervical cord lesions (Fig. 1g, h) and tested seropositive for AQP4-IgG antibody. Two years prior, she had a prolonged episode of nausea, vomiting and diplopia that had resolved spontaneously. Response to high-dose steroids and PLEX was moderate, with residual paraesthesia, unsteadiness and tonic spasms. She received a single course of alemtuzumab (12 mg daily for 5 consecutive days) in an attempt to prevent further relapses but at months 3 and 5 after alemtuzumab she represented with spastic paraparesis; cord imaging showed disease progression with new enhancing longitudinally extensive spinal cord lesions (Fig. 1i, j). At months 10 and 18, she had further relapses of myelitis without cord enhancement, losing dominant hand function and ability to walk unassisted despite high-dose steroids and PLEX. She became relapse free for 4 years after two cycles of rituximab in combination with mycophenolate mofetil (MMF), though disability persists with cord atrophy (Fig. 1k). Serum AQP4-IgG antibody remained positive after alemtuzumab treatment.
Discussion
We report three cases which demonstrate that alemtuzumab failed to prevent disabling relapses and poor outcome in neuromyelitis optica. This converges from evidence from other drugs effective in multiple sclerosis which also fail to suppress—and indeed may exacerbate—the illness, like interferon beta and natalizumab [11, 12]. We are aware of two other cases of neuromyelitis optica treated using alemtuzumab. In one, there was no effect on the disease which was subsequently effectively treated using an IL-6 antibody [13]. In another, there was a cessation of relapses and reduction in lymphocytes detected in brain lesions pathologically, but the patient deteriorated and died with significant monocyte invasion of her brain lesions [14].
All three cases fulfil the criteria for NMO spectrum disorder under the revised Wingerchuk criteria [9] and the International Panel for NMO Diagnosis consensus [10]. Both cases 1 and 2 presented prior to the clinical availability of an AQP4-IgG antibody test; stored serum samples from case 2 were negative; case 3 was positive in life.
In one of our cases (case 3), the patient subsequently had a good outcome with rituximab and mycophenolate. We hypothesise that the important mechanistic difference between alemtuzumab and rituximab is the latter’s prolonged depletion of B lymphocytes, which are only depleted for 1–2 months after alemtuzumab. The use of alemtuzumab is associated with secondary autoimmunity, directed mainly against the thyroid, but we do not propose this mechanism for continued disease activity of NMO after alemtuzumab.
From this case series, and a review of the literature, we therefore caution against the use of alemtuzumab in cases of neuromyelitis optica.
References
Cox AL, Thompson SA, Jones JL, Robertson VH, Hale G, Waldmann H, Compston DA, Coles AJ (2005) Lymphocyte homeostasis following therapeutic lymphocyte depletion in multiple sclerosis. Eur J Immunol 35(11):3332–3342. doi:10.1002/eji.200535075
Jones JL, Thompson SAJ, Loh P, Davies JL, Tuohy OC, Curry AJ, Azzopardi L, Hill-Cawthorne G, Fahey MT, Compston A, Coles AJ (2013) Human autoimmunity after lymphocyte depletion is caused by homeostatic T-cell proliferation. Proc Natl Acad Sci. doi:10.1073/pnas.1313654110
Hill-Cawthorne GA, Button T, Tuohy O, Jones JL, May K, Somerfield J, Green A, Giovannoni G, Compston DA, Fahey MT, Coles AJ (2012) Long term lymphocyte reconstitution after alemtuzumab treatment of multiple sclerosis. J Neurol Neurosurg Psychiatry 83(3):298–304. doi:10.1136/jnnp-2011-300826
Coles AJ, Fox E, Vladic A, Gazda SK, Brinar V, Selmaj KW, Skoromets A, Stolyarov I, Bass A, Sullivan H, Margolin DH, Lake SL, Moran S, Palmer J, Smith MS, Compston DA (2012) Alemtuzumab more effective than interferon beta-1a at 5-year follow-up of CAMMS223 clinical trial. Neurology 78(14):1069–1078. doi:10.1212/WNL.0b013e31824e8ee7
Cohen JA, Coles AJ, Arnold DL, Confavreux C, Fox EJ, Hartung H-P, Havrdova E, Selmaj KW, Weiner HL, Fisher E, Brinar VV, Giovannoni G, Stojanovic M, Ertik BI, Lake SL, Margolin DH, Panzara MA, Compston DAS (2012) Alemtuzumab versus interferon beta 1a as first-line treatment for patients with relapsing–remitting multiple sclerosis: a randomised controlled phase 3 trial. Lancet 380:1819–1828
Coles AJ, Twyman CL, Arnold DL, Cohen JA, Confavreux C, Fox EJ, Hartung HP, Havrdova E, Selmaj KW, Weiner HL, Miller T, Fisher E, Sandbrink R, Lake SL, Margolin DH, Oyuela P, Panzara MA, Compston DA (2012) Alemtuzumab for patients with relapsing multiple sclerosis after disease-modifying therapy: a randomised controlled phase 3 trial. Lancet 380(9856):1829–1839. doi:10.1016/s0140-6736(12)61768-1
Lennon VA, Wingerchuk DM, Kryzer TJ, Pittock SJ, Lucchinetti CF, Fujihara K, Nakashima I, Weinshenker BG (2004) A serum autoantibody marker of neuromyelitis optica: distinction from multiple sclerosis. Lancet 364(9451):2106–2112. doi:10.1016/s0140-6736(04)17551-x
Lucchinetti CF, Guo Y, Popescu BF, Fujihara K, Itoyama Y, Misu T (2014) The pathology of an autoimmune astrocytopathy: lessons learned from neuromyelitis optica. Brain Pathol (Zurich, Switzerland) 24(1):83–97. doi:10.1111/bpa.12099
Wingerchuk DM, Lennon VA, Pittock SJ, Lucchinetti CF, Weinshenker BG (2006) Revised diagnostic criteria for neuromyelitis optica. Neurology 66(10):1485–1489. doi:10.1212/01.wnl.0000216139.44259.74
Wingerchuk D, Banwell B, Bennett J, Cabre P, Carroll W, Chitnis T, De Seze J, Fujihara K, Greenberg B, Jacob A, Jarius S, Lana-Peixoto M, Levy M, Simon J, Tenembaum S, Traboulsee A, Waters P, Wellik K, Weinshenker B (2014) Revised diagnostic criteria for neuromyelitis optica spectrum disorders (S63.001). Neurology 82(10 Suppl):S63.001
Wang KC, Lin KH, Lee TC, Lee CL, Chen SY, Chen SJ, Chin LT, Tsai CP (2014) Poor responses to interferon-beta treatment in patients with neuromyelitis optica and multiple sclerosis with long spinal cord lesions. PLoS One 9(6):e98192. doi:10.1371/journal.pone.0098192
Kleiter I, Hellwig K, Berthele A, Kumpfel T, Linker RA, Hartung HP, Paul F, Aktas O (2012) Failure of natalizumab to prevent relapses in neuromyelitis optica. Arch Neurol 69(2):239–245. doi:10.1001/archneurol.2011.216
Kieseier BC, Stuve O, Dehmel T, Goebels N, Leussink VI, Mausberg AK, Ringelstein M, Turowski B, Aktas O, Antoch G, Hartung HP (2013) Disease amelioration with tocilizumab in a treatment-resistant patient with neuromyelitis optica: implication for cellular immune responses. JAMA Neurol 70(3):390–393. doi:10.1001/jamaneurol.2013.668
Gelfand JM, Cotter J, Klingman J, Huang EJ, Cree BA (2014) Massive CNS monocytic infiltration at autopsy in an alemtuzumab-treated patient with NMO. Neurol Neuroimmunol Neuroinflamm 1(3):e34. doi:10.1212/nxi.0000000000000034
Acknowledgments
Clinical work is performed at the Wellcome Clinical Research Facility. JLJ and AJC are supported by the Cambridge Biomedical Research Centre of the National Institute for Health Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
JLJ reports receiving consulting fees and lecture fees from Genzyme Sanofi. AJC reports receiving consulting fees, lecture fees and institutional grant support from Genzyme Sanofi. LA, ALC and CMC declare they have no conflict of interest.
Ethical standards
All patients provided informed consent to alemtuzumab treatment and long-term follow-up at Addenbrooke’s Hospital, Cambridge, UK.
Rights and permissions
About this article
Cite this article
Azzopardi, L., Cox, A.L., McCarthy, C.L. et al. Alemtuzumab use in neuromyelitis optica spectrum disorders: a brief case series. J Neurol 263, 25–29 (2016). https://doi.org/10.1007/s00415-015-7925-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-015-7925-y