Abstract
Purpose of review
Neuromyelitis optica spectrum disorders (NMOSDs) are a group of inflammatory and demyelinating disorders of the central nervous system that can occur in children and adults. The classic presentation of NMOSD is characterized by optic neuritis and transverse myelitis, but other presentations are also recognized, expanding the disease as NMO spectrum disorders. The purpose of this review is to discuss the clinical features, along with management and treatment options, including potential future therapeutic options, in pediatric NMOSD.
Recent findings
The aquaporin-4 antibody (AQP4 ab) is specific for NMOSD; however, recently another antibody, the myelin oligodendrocyte glycoprotein (MOG ab) has been found in a subset of AQP4 ab-negative patients including in children. Most treatment studies are reported in adults, but retrospective studies on efficacy and safety of mycophenolate mofetil, azathioprine, and rituximab in pediatric NMOSD are available.
Summary
While some pediatric NMOSD-specific treatment studies are available, more research is needed in the mechanisms of early onset and specific treatment options in children, including whether different treatment considerations are needed for AQP4 ab as opposed to MOG ab-positive disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
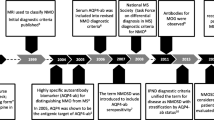
Neuromyelitis optica spectrum disorders (NMOSDs) are a group of inflammatory and demyelinating disorders of the central nervous system and are separate diseases from multiple sclerosis (MS). Initially termed Devic’s disease, NMOSD was first characterized by optic neuritis (ON) and transverse myelitis (TM). However, the antibody targeting aquaporin-4 (AQP4 ab) was discovered as specific for the disease and the more recent guidelines included antibody testing as part of the diagnosis [1••]. Other presentations of NMO are also recognized, broadening the disease as NMOSD. While NMOSD usually occurs in adults, NMOSD can also affect children. This review aims to highlight the characteristics of NMOSD in pediatric patients and most recent insights into the disease.
Epidemiology
While average age of onset in NMOSD is usually in the fourth and fifth decades of life, NMOSD can also occur in children, in up to 3–5% of patients [2]. The age of onset is typically around 10–12 years but has been reported in patients as young as 16 months old [3•]. Girls are more likely to be affected than boys [4] (see Table 1). Incidence and prevalence of pediatric onset NMOSD are not well-characterized, but population studies suggest that the overall incidence of NMOSD in children and adults ranges from 0.05 to 4/100,000 per year and prevalence from 0.52 to 4.4/100,000 [5]. In Japan, the incidence of pediatric NMOSD was 0.06 per 100,000 children [6].
NMOSD is generally a sporadic disease; however, about 3% of cases are familial [7]. While very few genetic risk factors are linked to NMOSD, the HLA-DRB1*03:01 allele was associated with NMOSD in a group of Brazilian patients [8] and several single nucleotide polymorphisms in CD58 were associated with increased risk of NMOSD in Korean patients [9].
Clinical features of pediatric NMOSD
In a large case series of NMOSD from the US Network of Pediatric MS Centers (NPMSC), the most common initial presenting symptoms in pediatric NMOSD patients include motor, visual, and constitutional (including fevers and seizures) symptoms. Vomiting and intractable hiccups are seen in area postrema syndrome, which can be the initial symptoms of NMOSD [10]. Vomiting was more likely to occur in NMOSD (38%) and in acute disseminated encephalomyelitis (ADEM) (46%) than in MS patients (10%; p < 0.01 compared to NMOSD). In this case series, 65% presented with optic nerve involvement, and 55% presented with spinal cord involvement, with 13% having both optic nerve and spinal cord involvement [3•]. Brainstem/cerebellar involvement was observed in 71% of patients. In another series of 20 pediatric onset NMOSD patients, 40% presented with unilateral ON, 20% with bilateral ON, 15% with TM alone, and 15% with simultaneous ON and TM [11].
NMOSD has been linked with other autoimmune diseases including Sjogren’s syndrome [12], lupus [13], celiac, Hashimoto’s disease, childhood onset diabetes, atopic dermatitis [3•], juvenile rheumatoid arthritis, Graves, autoimmune hepatitis, panserositis [14•], and juvenile dermatomyositis [13]. Coexisting autoimmune diseases was found in 9% in a Brazilian study [15], 16% of pediatric NMOSD from the NPMSC study [3•], and 42% in a study from Mayo in AQP4 seropositive children [14•].
Diagnostic criteria for NMOSD
The International Panel for NMO Diagnosis (IPND) published the most recent diagnostic criteria for NMOSD in 2015 [1••]. These diagnostic criteria divide patients into AQP4 ab-positive and AQP4 ab-negative patients. Diagnosis of NMOSD in AQP4 ab-positive patients includes one core clinical characteristic, positive AQP4 ab, and exclusion of alternative diagnoses.
The core clinical characteristics include the following: optic neuritis, acute myelitis, area postrema syndrome of hiccups or nausea, symptomatic narcolepsy or acute diencephalic clinical syndrome with MRI diencephalic lesions typical of NMOSD, acute brainstem syndrome, and symptomatic cerebral syndrome with NMOSD-typical brain lesions.
Diagnostic criteria for NMOSD with either negative or unknown AQP4 status include two core clinical characteristics that meet all of the following requirements: one core clinical characteristic must include optic neuritis, acute myelitis with LETM or area postrema syndrome, dissemination in space of two or more core clinical characteristics, and fulfillment of additional MRI requirements [1••].
Diagnostic criteria from the International Pediatric Multiple Sclerosis Study Group (IPMSSG) for pediatric NMOSD in 2007 were that all three criteria were fulfilled: optic neuritis, acute myelitis, and two of three supportive criteria: Contiguous spinal cord MRI lesion extending over three vertebral segments, brain MRI not meeting diagnostic criteria for MS, and AQP4 IgG seropositive status. However, in 2013, IPMSSG revised diagnostic criteria for pediatric demyelinating disorders, which expanded pediatric NMO into NMOSD. NMOSD includes relapsing ON or relapsing TM with a positive serum AQP4 ab; NMOSD relapses can resemble ADEM, and brain MRI lesions can be located in the supratentorial region, hypothalamus, and brainstem near the fourth ventricle [16••]. LETM can be less specific for NMOSD in children as 15% of pediatric MS patients have LETM [17].
Differential diagnosis in NMOSD
Mimickers of adult NMOSD include multiple sclerosis, ADEM, lupus, sarcoidosis, vasculitis, and malignancy including paraneoplastic disease or chronic infection. Late-onset biotinidase deficiency is a rare but mimicker of NMOSD that occurs in adults [18] and has also been reported in children [19, 20]. NMOSD has also been reported in an adult patient with atypical hemophagocytic lymphohistiocytosis who was found to have a perforin mutation A91V [21]. In children, all of these differentials should be considered, including ADEM, CNS vasculitis, and sarcoidosis.
Laboratory testing in pediatric NMOSD
Initial laboratory testing for a patient with suspected NMOSD usually includes a complete blood count with differential, chemistry panel, and liver function tests. Inflammatory markers including erythrocyte sedimentation rate and c-reactive protein are sometimes elevated. Markers for other autoimmune diseases include screening anti-nuclear antibody (ANA) along with anti-Ro and anti-La. Evaluation for infectious diseases including mycoplasma, Lyme disease, cytomegalovirus, and Epstein-Barr virus can also be sent. Cerebrospinal fluid should be examined when possible for cell count, glucose, protein, gram stain and culture, oligoclonal bands (OCBs), and IgG index.
Cerebrospinal fluid from NMOSD patients generally demonstrates elevated white blood cell counts (average of 105.8) as compared to MS patients (average 19.4) but similar to ADEM patients [3•]. CSF pleocytosis in NMOSD and MS is lymphocytic predominant. Oligoclonal bands are positive in one third of patients, compared to two thirds of MS patients and are generally absent in ADEM patients [3•]. Another study of 20 pediatric NMOSD patients reported that 2/10 AQP4 ab-positive patients whereas 0/7 of the AQP4 ab-negative patients had positive oligoclonal bands [11].
AQP4 antibody testing in NMOSD
Aquaporin-4 antibody (AQP4 ab) was discovered in 2004 and is a specific serum biomarker for NMOSD [22•]. Aquaporin-4 is a water channel localized in the foot processes of astrocytes at the blood-brain barrier [23]. AQP4 ab can be sent from both serum and CSF; however, serum testing is more sensitive than CSF [24]. The sensitivity of the AQP4 ab testing using a cell-based assay is 76.7% [1••]. This proportion was similar among a pediatric NMOSD cohort; however, in children, serial testing revealed that AQP4 ab testing could remain negative even up to 4 years after disease onset [3•]. Thus, repeat testing of AQP4 should be obtained in patients with high suspicion, even if the test is initially negative.
AQP4 ab positivity is associated with early recurrence and visual impairment when compared to AQP4 ab-negative patients [11]. AQP4 positivity portends a lifelong disorder and thus treatment is started as soon as the diagnosis is made and continued indefinitely (see below regarding treatment) [1••].
Imaging characteristics of pediatric NMOSD
MRI of brain and full spine with and without contrast should be obtained in patients who present with suspected NMOSD. If the patient has any visual symptoms then a dedicated orbital MRI can be helpful to evaluate the optic nerve pathway. Brain MRI findings in NMOSD include diencephalic lesions around the third ventricle and aqueduct, dorsal brainstem lesions abutting the fourth ventricle, and periependymal lesions around the lateral ventricles. White matter lesions in the hemispheres can be large and tumefactive or spindle-like following white matter tracts [25]. As mentioned before, LETM is not specific to NMOSD in children and can be seen in MS [17] and non-LETM can be seen in children with NMOSD.
Disease course in pediatric NMOSD
More than 90% of children with NMOSD will have relapses [3•, 11, 17, 26] and can result in disability. As compared to MS or ADEM, pediatric patients have a higher EDSS score within 2 years of disease onset (2.25 versus 1.28 and 0.5, respectively) [3•]. This finding could be attributed to delayed treatment but another study from Brazil reported disability accumulation in pediatric-onset NMOSD despite treatment [27]. A study from France found that pediatric-onset NMOSD has slower long-term disability accrual by EDSS but higher visual disability when compared to adult-onset NMOSD patients [26].
In the study with the longest follow-up in pediatric NMOSD (average 19.3 years), 12 pediatric NMOSD patients were compared with 113 adult NMOSD patients [26]. In pediatric onset patients, the median interval between onset and disability was 20.7 years for EDSS score 4, 26 years for EDSS score 6, and 28.7 years for EDSS score 7. Moreover, median time to severe residual visual loss after the initial episode of optic neuritis was 1.3 years. Compared to adult onset NMOSD, pediatric patients had a longer time to reach EDSS score 4 and 6, which was attributed to the severity of the initial episode of myelitis in adults. Mean annualized relapse rates were 0.6 in children and 1.0 in adult onset NMOSD [26].
Anti-MOG antibody in NMOSD
Antibodies against MOG (myelin oligodendrocyte glycoprotein), a glycoprotein located on the outermost lamella of the CNS myelin sheath [28], have been increasingly recognized in NMOSD. Some NMOSD patients who test negative for the AQP4 ab are found to be seropositive for the MOG ab. In a cohort of adults and children with NMOSD and systematic testing, 73% were seropositive for AQP4, 12% for MOG antibody, and 15% were double-seronegative [29]. MOG ab should also be sent on patients who are AQP4 ab negative and as of October 2017 has become clinically available in the USA. MOG ab seropositivity is also observed in other pediatric demyelinating diseases, including ADEM, clinically isolated syndrome (CIS), and MS [30,31,32,33] that will not be discussed in this article.
Differentiating features of AQP4 versus MOG ab positivity
There are several studies examining differences in NMOSD of comparing AQP4 ab versus MOG ab positivity (see Table 2). In one available pediatric study of NMOSD patients, 3/12 patients tested positive for AQP4 with 7/12 testing positive for MOG [36]. Gender differences are observed between the two antibodies for in NMOSD patients, AQP4 ab patients had a higher female:male ratio as compared to MOG ab patients [34, 37]. Some studies suggest that AQP4 ab is more likely associated with relapsing disease where MOG ab is more likely to be associated with monophasic illness and therefore more benign [32, 37, 38]. However, this may be explained by a shorter follow-up time as other studies with more patients and longer follow-up time reported that MOG ab is associated with relapsing disease, including 55% of one pediatric MOG ab cohort and 80% in an adult MOG ab cohort [39, 40•].
Not only are relapsing rates different but recovery also differ between AQP4 and MOG ab patients. For episodes of myelitis, complete recovery is observed in 19% of AQP4 ab as compared to 35% of MOG ab. For recovery from optic neuritis, 33% of AQP4 ab patients have complete recovery as compared to 53% of MOG ab-positive patients [39]. In this study, the most recent Extended Disability Status Scale (EDSS) was more severe in AQP4 ab patients (median 4.5) as compared to MOG ab-positive patients (median 1.0; however, follow-up time was also different between the two groups (median 7.2 years in AQP4 and 3.7 years in MOG ab).
CSF characteristics are also different. AQP4 ab-positive patients had a lower CSF white blood cell count (mean 13) as compared to MOG ab-positive patients (mean 75) [34]. However, OCBs are found in both AQP4 ab and MOG patients at different rates; one study found OCBs are more likely found in AQP4 ab than in MOG ab CSF (15 and 0%, respectively) [34] whereas another study found that 5/29 AQP4 ab-positive patients had OCBs as compared to 3/3 MOG ab patients [35•].
Variations in imaging characteristics may exist between AQP4 and MOG ab-positive patients. Longitudinally extensive optic involvement and/or chiasmal involvement on imaging can be more suggestive of MOG antibody seropositivity as compared to AQP4 antibody positive optic neuritis [39]. MOG ab positivity was more often associated with anterior optic pathway involvement whereas AQP4 ab is more often associated with posterior optic pathway [41]; see Fig. 1. Whether these imaging findings apply to pediatric patients is a topic of further study.
a, b, c Representative MRI images from an 11-year-old patient presenting with weakness, found to have longitudinally extensive transverse myelitis and serum AQP4 ab positive. T2-weighted images of the cervical (a) and thoracic spine (b) demonstrated LETM and brain MRI showed punctate lesions (c). d, e, f, g Representative MRI images from a 16-year-old pediatric NMOSD patient who is also MOG positive: T2-weighted images of the cervical spine (d) and thoracic spine (e) demonstrate a longitudinal lesion. T2 FLAIR images of the brain show punctate lesions (f), T2-weighted FLAIR images of the orbits demonstrate bilateral optic neuritis (g).
Interestingly, brain lesional biopsy from a MOG ab positive patient demonstrated acute inflammation with demyelination and relative preservation of astrocytes [42]. This is in contrast to biopsy of tissue from AQP4 ab-positive patients in which six different lesion types have been described, one that includes astrocyte apoptosis [43].
How MOG ab seropositivity affects medication options is not entirely established currently and for patients who fit clinical criteria for NMOSD, the same treatment options can be considered as will be discussed below.
Approach to management in patients
Management of NMOSD includes a multidisciplinary approach including a neurologist, neuropsychologist, ophthalmologist/neuro-ophthalmologist, physical therapist, bladder management, and pain management. Monitoring for infectious diseases is also important for patients on immunotherapy. Moreover, interventions for school such as a Section 504 Plan or Individualized Education Program should be considered in patients to provide additional services.
Treatment options for pediatric NMOSD
Treatment for NMOSD includes treatment of acute attacks, preventative therapy, and symptomatic management. Limited Class I evidence is currently published, but we will highlight both pediatric and adult studies on treatment options when available. The following recommendations are off-label use for NMOSD. There is emerging suggestions of differential response to some treatments based on AQP4 or MOG ab serostatus; however, these observations require further validation.
Acute attacks
For acute relapses, methylprednisolone, intravenous immunoglobulin, and plasma exchange are options in pediatric NMOSD. Treating an acute attack targets recovery of neurological deficits and minimizes irreversible CNS injury. Initial treatment is usually IV methylprednisolone, with a dose of 30 mg/kg/day with a maximum of 1000 mg for 5 days. If symptoms are minimally improved or severe, then extending the course to a total of 7 days is considered. However, if minimal response to IV methylprednisolone is observed or if the patient has severe symptoms upon presentation, intravenous immunoglobulin (IVIG) administered at 2 g/kg divided over 2–5 days is generally the next step in treatment. Plasma exchange (PLEX) can also be considered as PLEX been shown to be effective in treating acute relapses in adults with NMOSD [44].
Upon completion of IV methylprednisolone in a first attack, we recommend an oral steroid taper. Different institutions offer different tapers, but we use either prednisone or prednisolone, beginning at 1 mg/kg/day up to 60 mg and cutting the dose in half every 5 days for a total of 4 weeks starting on the first day upon completion of IV steroids.
Preventative therapy
Preventative therapy is utilized to decrease risk of relapses and disability. Disease-modifying treatment options include rituximab, mycophenolate mofetil, azathioprine, and cyclophosphamide [45, 46].
Mycophenolate mofetil
Mycophenolate mofetil has been shown to be effective in adults with NMOSD by reduction of annualized relapse rate (ARR) and improvement in EDSS [47, 48] and even as first-line therapy [49]. In adults, mycophenolate mofetil has been suggested to be more efficacious than azathioprine [50] and another study reported that the efficacy was similar between both medications but that mycophenolate mofetil was better tolerated than azathioprine [51]. One retrospective study including children demonstrated efficacy of mycophenolate mofetil in NMOSD [48]. One study in adults found an association with younger age of disease onset and increased likelihood of failing mycophenolate mofetil or azathioprine and switching to rituximab [52]. Dosing of mycophenolate mofetil is a goal of 600 mg/m2 twice a day for a total of 1200 mg/m2 in a day, with a maximum of 1000 mg twice a day for a total of 2000 mg in a day. Slower uptitration is associated with increased tolerability so we generally start at a quarter dose up to 250 mg twice a day for 14 days, then half dose up to 500 mg twice a day for 14 days and then goal dose after that. Side effects associated with mycophenolate mofetil include gastrointestinal symptoms including nausea, abdominal pain, diarrhea; dizziness, rash, increased risk of infection, and fatigue [47, 51]. A few reports of progressive multifocal leukoencephalopathy (PML) have been associated with mycophenolate mofetil but are rare [53].
Rituximab
Rituximab is an anti-CD20 chimeric monoclonal antibody that depletes B cells and has been used in children with NMOSD [54]. One retrospective study in 16 pediatric patients [55] demonstrated a reduction in ARR with rituximab. Moreover, B cell repopulation was associated with risk of relapse. While on average, the last documented B cell depletion occurred at 4.5 months from the last rituximab dosage and mean time to repopulation was 6.8 months; a wide range of interpatient and intrapatient variability was observed [55]. Rituximab has also been used as first-line preventative agent in pediatric NMOSD with good effect [56]. A randomized clinical trial in adults with NMOSD demonstrated that rituximab was more effective than azathioprine with decreased ARR and improvement in EDSS [57]. Dosing in pediatric patients is generally induction dosing at 375 mg/m2 every week for 4 weeks and then 375 mg/m2 every 6 months after that. For older patients, dosing can be 750 mg/m2 up to 1000 mg maximum every 2 weeks at two doses and then 750 mg/m2 up to 1000 mg maximum every 6 months. Monitoring of B cell counts is recommended every 3–6 months as return of B cells is associated with risk of relapse. Side effects of rituximab include infusion reactions, nausea, vomiting, increased risk for infections, and hepatitis viral reactivation [58]. PML has been linked with many disease-modifying therapies and has been rarely associated with rituximab but has been reported in the setting of treatment for lymphoma [59].
Azathioprine
Azathioprine is a purine analogue that interferes with DNA synthesis in proliferating cells, including T and B cells. Azathioprine has been shown to be effective in decreasing relapse rates along with improving EDSS and visual acuity in adults with NMOSD [60]. In a long-term study in adults, 89% had reduced relapse rate and 61% remained free from relapse at 18 months after treatment initiation [61]. Two retrospective studies on azathioprine included children and demonstrated efficacy and that treatments were discontinued due to tolerability [60, 61]. Dosing in pediatric patients is 2–3 mg/kg/day. Azathioprine has also been used in MOG ab-positive NMOSD [39]. Side effects include nausea, elevated liver function tests, diarrhea, severe leukopenia, rash, and hypersensitivity reactions. A rare side effect also includes lymphoma [60].
Cyclophosphamide
Cyclophosphamide has been used in treating NMOSD; adult studies generally report that cyclophosphamide is efficacious in NMOSD [62, 63] whereas another retrospective study reported no improvement [64]. Moreover, a study in comparing the effects of azathioprine, mycophenolate mofetil, and cyclophosphamide found that while all three were effective in treating NMOSD, cyclophosphamide did not affect EDSS although both azathioprine and mycophenolate mofetil demonstrated a decrease in EDSS [63]. However, in the few children treated with cyclophosphamide, all had to switch to another medication due to lack of efficacy [17, 26]. With the effectiveness of other options including rituximab and the side effects of cyclophosphamide including hemorrhagic cystitis, infertility, and increased risk of malignancies, we generally use other options.
Medications to avoid in NMOSD
Some of the disease-modifying therapies used in MS are either ineffective or exacerbate NMOSD, demonstrating the need for accurate diagnosis. Interferon-beta has been shown to be ineffective or even exacerbate disease in NMOSD [65, 66]. Glatiramer acetate is ineffective in NMOSD [67]. Severe relapses resulting in significant disability have been associated with the use of dimethyl fumarate [68]. Alemtuzumab also has been reported ineffective in two cases of NMOSD, which included a pediatric patient [69]. Natalizumab has been associated with relapses [70,71,72].
Potential future treatments
Tocilizumab
Tocilizumab is a monoclonal antibody targeting the interleukin-6 (IL-6) receptor. IL-6 is a proinflammatory cytokine and elevated in both serum and cerebrospinal fluid of NMOSD patients [73, 74]. A pilot Class IV study in seven adult NMOSD patients demonstrated efficacy of tocilizumab with reduction in the annualized relapse rate (ARR), along with decreased Expanded Disability Status Scale (EDSS) score, pain, and fatigue [75]. A retrospective observational study with a median follow-up time of 30.9 months also demonstrated reduced ARR and decreased EDSS [76]. While no such study has yet been performed in pediatric NMOSD, one case report of a pediatric patient with both NMOSD and Sjogren’s syndrome had treatment response to tocilizumab, an anti-interleukin-6 monoclonal antibody [77]. Tocilizumab is used in other pediatric diseases including juvenile idiopathic arthritis [78] and juvenile dermatomyositis [79]. Most common adverse events include infections, especially respiratory infections, and laboratory abnormalities reported are liver function abnormalities, neutropenia, and elevated cholesterol [78].
Eculizumab
Part of the pathophysiology of NMOSD has demonstrated that upon binding of the AQP4 ab to astrocytes, the complement cascade is activated that results in lysing of astrocytes [80]. Eculizumab is a humanized monoclonal IgG that targets the complement protein C5, and as a result, inhibits the complement cascade and the endpoint destruction of astrocytes. An open-label pilot study of eculizumab examined 14 adults with NMOSD. Eculizumab demonstrated decrease of attacks and improvement in EDSS. The most common adverse reactions included headache, nausea, and dizziness. Serious adverse events included a transient ischemic attack in a patient who is a smoker and one patient had meningococcal sepsis but recovered and continued on eculizumab [81].
While currently there are no published cases of pediatric NMOSD patients treated with eculizumab, eculizumab is currently used in pediatric patients with other diseases such as paroxysmal nocturnal hemoglobinuria [82] or as first-line therapy in atypical hemolytic uremic syndrome [83]. Side effects of eculizumab reported in children include infusion reactions [84] and increased risk of meningococcal infections [83].
Bevacizumab, a recombinant humanized monoclonal antibody that binds vascular endothelial growth factor (VEGF), was studied in an open-label phase 1b safety and proof of concept study as adjunct therapy to steroids at time of acute relapse in ten adult patients. Bevacizumab was safe in all ten patients, and three patients experienced recovery or improvement as compared to their neurological baseline prior to the attack. None of the patients required PLEX [85].
In adults, currently clinical trials are underway or recently completed without published results investigating the utility of cetirizine, alpha1-antitrypsin, autologous hematopoietic stem cell transplant, C1-esterase inhibitor, MEDI-551, and ublituximab (also known as LFB-R603), a monoclonal antibody that specifically binds to the trans-membrane antigen CD20 [86].
Symptomatic management
Little evidence exists for the symptomatic treatment in NMOSD; consequently, the following recommendations are based on experience and upon symptomatic treatment in other neurological disorders.
Symptomatic management
Urinary retention
When the spine is injured, urinary retention or incontinence can be a lasting symptom. For patients with urinary retention, clean intermittent self-catheterization is the preferred option as an indwelling catheter can easily become infected. Management of urinary incontinence usually includes frequent scheduled trips to the bathroom and pelvic floor exercises. Bladder symptoms are managed with the guidance of urology.
Pain
Even after recovery from an acute attack, many patients experience pain. Pain can be neuropathic including burning or allodynia, or pain due to spasticity. For neuropathic pain, we usually start with gabapentin but amitriptyline or duloxetine can also be considered. For spasticity, baclofen can be helpful as is physical therapy.
Fatigue
Fatigue is a symptom that greatly impacts quality of life in patients with NMOSD. In a survey of pediatric patients with demyelinating diseases including NMOSD, pediatric patients’ reports of fatigue were predictive of decreased quality of life and quality of life was decreased in pediatric demyelinating disease patients as compared to healthy controls [87]. Management of fatigue initially begins with optimizing sleep hygiene and ruling out other medical causes such as hypothyroidism or anemia. First-line interventions for fatigue begin with non-pharmacologic interventions such as routine exercise, cognitive behavioral therapy, mindfulness, and fatigue-management programs [88]. While medications have not been studied specifically for fatigue in NMOSD or in pediatric demyelinating diseases, modafinil has been shown to be effective in adults with MS and can be considered in pediatric patients [89,90,91].
Conclusion
NMOSD can occur in children, and distinguishing the diagnosis of NMOSD from other demyelinating diseases is important in selecting treatment options in these patients. More studies are needed in examining the pathogenesis and management options in NMOSD patients including in patients who are MOG ab positive or AQP4/MOG ab negative. Moreover, studies on long-term effects of these treatments in children are also needed.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance•• Of major importance
•• Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 2015;85(2):177–89. https://doi.org/10.1212/WNL.0000000000001729. This is the most recent diagnostic criteria for NMOSD.
Quek AM, McKeon A, Lennon VA, Mandrekar JN, Iorio R, Jiao Y, et al. Effects of age and sex on aquaporin-4 autoimmunity. Arch Neurol. 2012;69(8):1039–43. https://doi.org/10.1001/archneurol.2012.249.
• Chitnis T, Ness J, Krupp L, Waubant E, Hunt T, Olsen CS, et al. Clinical features of neuromyelitis optica in children: US network of pediatric MS centers report. Neurology. 2016;86(3):245–52. https://doi.org/10.1212/WNL.0000000000002283. This is a retrospective study of a large pediatric NMO cohort from the US Network of Pediatric MS Centers.
Tenembaum S, Chitnis T, Nakashima I, Collongues N, McKeon A, Levy M, et al. Neuromyelitis optica spectrum disorders in children and adolescents. Neurology. 2016;87(9 Suppl 2):S59–66. https://doi.org/10.1212/WNL.0000000000002824.
Pandit L, Asgari N, Apiwattanakul M, Palace J, Paul F, Leite MI, et al. Demographic and clinical features of neuromyelitis optica: a review. Mult Scler. 2015;21(7):845–53. https://doi.org/10.1177/1352458515572406.
Yamaguchi Y, Torisu H, Kira R, Ishizaki Y, Sakai Y, Sanefuji M, et al. A nationwide survey of pediatric acquired demyelinating syndromes in Japan. Neurology. 2016;87(19):2006–15. https://doi.org/10.1212/WNL.0000000000003318.
Matiello M, Kim HJ, Kim W, Brum DG, Barreira AA, Kingsbury DJ, et al. Familial neuromyelitis optica. Neurology. 2010;75(4):310–5. https://doi.org/10.1212/WNL.0b013e3181ea9f15.
Alvarenga MP, Fernandez O, Leyva L, Campanella L, Vasconcelos CF, Alvarenga M, et al. The HLA DRB1*03:01 allele is associated with NMO regardless of the NMO-IgG status in Brazilian patients from Rio de Janeiro. J Neuroimmunol. 2017;310:1–7. https://doi.org/10.1016/j.jneuroim.2017.05.018.
Kim JY, Bae JS, Kim HJ, Shin HD. CD58 polymorphisms associated with the risk of neuromyelitis optica in a Korean population. BMC Neurol. 2014;14:57. https://doi.org/10.1186/1471-2377-14-57.
Popescu BF, Lennon VA, Parisi JE, Howe CL, Weigand SD, Cabrera-Gomez JA, et al. Neuromyelitis optica unique area postrema lesions: nausea, vomiting, and pathogenic implications. Neurology. 2011;76(14):1229–37. https://doi.org/10.1212/WNL.0b013e318214332c.
Absoud M, Lim MJ, Appleton R, Jacob A, Kitley J, Leite MI, et al. Paediatric neuromyelitis optica: clinical, MRI of the brain and prognostic features. J Neurol Neurosurg Psychiatry. 2015;86(4):470–2. https://doi.org/10.1136/jnnp-2014-308550.
Gmuca S, Lieberman SM, Mehta J. Pediatric neuromyelitis optica spectrum disorder and Sjogren syndrome: more common than previously thought? J Rheumatol. 2017;44(6):959–60. https://doi.org/10.3899/jrheum.160978.
Amorim ALM, Cabral NC, Osaku FM, Len CA, Oliveira EML, Terreri MT. Association between demyelinating disease and autoimmune rheumatic disease in a pediatric population. Rev Bras Reumatol Engl Ed. 2017;57(3):224–8. https://doi.org/10.1016/j.rbre.2016.09.016.
• McKeon A, Lennon VA, Lotze T, Tenenbaum S, Ness JM, Rensel M, et al. CNS aquaporin-4 autoimmunity in children. Neurology. 2008;71(2):93–100. https://doi.org/10.1212/01.wnl.0000314832.24682.c6. This is a retrospective study of the largest number of pediatric NMOSD patients to date.
Amorim AL, Cabral NC, Osaku FM, Len CA, Oliveira EM, Terreri MT. Association between demyelinating disease and autoimmune rheumatic disease in a pediatric population. Rev Bras Reumatol. 2016;57:224–8. https://doi.org/10.1016/j.rbr.2016.08.004.
•• Krupp LB, Tardieu M, Amato MP, Banwell B, Chitnis T, Dale RC, et al. International pediatric multiple sclerosis study group criteria for pediatric multiple sclerosis and immune-mediated central nervous system demyelinating disorders: revisions to the 2007 definitions. Mult Scler. 2013;19(10):1261–7. https://doi.org/10.1177/1352458513484547. This is the most recent consensus statement of diagnostic criteria in pediatric demyelinating diseases.
Banwell B, Tenembaum S, Lennon VA, Ursell E, Kennedy J, Bar-Or A, et al. Neuromyelitis optica-IgG in childhood inflammatory demyelinating CNS disorders. Neurology. 2008;70(5):344–52. https://doi.org/10.1212/01.wnl.0000284600.80782.d5.
Bottin L, Prud'hon S, Guey S, Giannesini C, Wolf B, Pindolia K, et al. Biotinidase deficiency mimicking neuromyelitis optica: initially exhibiting symptoms in adulthood. Mult Scler. 2015;21(12):1604–7. https://doi.org/10.1177/1352458515596457.
Yilmaz S, Serin M, Canda E, Eraslan C, Tekin H, Ucar SK, et al. A treatable cause of myelopathy and vision loss mimicking neuromyelitis optica spectrum disorder: late-onset biotinidase deficiency. Metab Brain Dis. 2017;32(3):675–8. https://doi.org/10.1007/s11011-017-9984-5.
Girard B, Bonnemains C, Schmitt E, Raffo E, Bilbault C. Biotinidase deficiency mimicking neuromyelitis optica beginning at the age of 4: a treatable disease. Mult Scler. 2017;23(1):119–22. https://doi.org/10.1177/1352458516646087.
Palterer B, Brugnolo F, Sieni E, Barilaro A, Parronchi P. Neuromyelitis optica, atypical hemophagocytic lymphohistiocytosis and heterozygous perforin A91V mutation. J Neuroimmunol. 2017;311:10–3. https://doi.org/10.1016/j.jneuroim.2017.08.003.
• Lennon VA, Wingerchuk DM, Kryzer TJ, Pittock SJ, Lucchinetti CF, Fujihara K, et al. A serum autoantibody marker of neuromyelitis optica: distinction from multiple sclerosis. Lancet. 2004;364(9451):2106–12. This paper reports on the discovery of aquaporin-4, the first serum antibody biomarker in demyelinating disease.
He D, Zhang A, Li Y, Cai G, Li Y, Guo S. Autoimmune aquaporin-4 induced damage beyond the central nervous system. Mult Scler Relat Disord. 2017;18:41–6. https://doi.org/10.1016/j.msard.2017.09.013.
Majed M, Fryer JP, McKeon A, Lennon VA, Pittock SJ. Clinical utility of testing AQP4-IgG in CSF: guidance for physicians. Neurol Neuroimmunol Neuroinflamm. 2016;3(3):e231. https://doi.org/10.1212/NXI.0000000000000231.
Kim HJ, Paul F, Lana-Peixoto MA, Tenembaum S, Asgari N, Palace J, et al. MRI characteristics of neuromyelitis optica spectrum disorder: an international update. Neurology. 2015;84(11):1165–73. https://doi.org/10.1212/WNL.0000000000001367.
Collongues N, Marignier R, Zephir H, Papeix C, Fontaine B, Blanc F, et al. Long-term follow-up of neuromyelitis optica with a pediatric onset. Neurology. 2010;75(12):1084–8. https://doi.org/10.1212/WNL.0b013e3181f39a66.
Fragoso YD, Ferreira ML, Oliveira EM, Domingues RB, Ribeiro TA, Brooks JB, et al. Neuromyelitis optica with onset in childhood and adolescence. Pediatr Neurol. 2014;50(1):66–8. https://doi.org/10.1016/j.pediatrneurol.2013.07.003.
Brunner C, Lassmann H, Waehneldt TV, Matthieu JM, Linington C. Differential ultrastructural localization of myelin basic protein, myelin/oligodendroglial glycoprotein, and 2′,3′-cyclic nucleotide 3′-phosphodiesterase in the CNS of adult rats. J Neurochem. 1989;52(1):296–304.
Sepulveda M, Aldea M, Escudero D, Llufriu S, Arrambide G, Otero-Romero S, et al. Epidemiology of NMOSD in Catalonia: influence of the new 2015 criteria in incidence and prevalence estimates. Mult Scler. 2017:1352458517735191. https://doi.org/10.1177/1352458517735191.
Fernandez-Carbonell C, Vargas-Lowy D, Musallam A, Healy B, McLaughlin K, Wucherpfennig KW, et al. Clinical and MRI phenotype of children with MOG antibodies. Mult Scler. 2016;22(2):174–84. https://doi.org/10.1177/1352458515587751.
Jarius S, Ruprecht K, Kleiter I, Borisow N, Asgari N, Pitarokoili K, et al. MOG-IgG in NMO and related disorders: a multicenter study of 50 patients. Part 1: frequency, syndrome specificity, influence of disease activity, long-term course, association with AQP4-IgG, and origin. J Neuroinflammation. 2016;13(1):279. https://doi.org/10.1186/s12974-016-0717-1.
Sato DK, Callegaro D, Lana-Peixoto MA, Waters PJ, de Haidar Jorge FM, Takahashi T, et al. Distinction between MOG antibody-positive and AQP4 antibody-positive NMO spectrum disorders. Neurology. 2014;82(6):474–81. https://doi.org/10.1212/WNL.0000000000000101.
Reindl M, Di Pauli F, Rostasy K, Berger T. The spectrum of MOG autoantibody-associated demyelinating diseases. Nat Rev Neurol. 2013;9(8):455–61. https://doi.org/10.1038/nrneurol.2013.118.
Sepulveda M, Armangue T, Sola-Valls N, Arrambide G, Meca-Lallana JE, Oreja-Guevara C, et al. Neuromyelitis optica spectrum disorders: comparison according to the phenotype and serostatus. Neurol Neuroimmunol Neuroinflamm. 2016;3(3):e225. https://doi.org/10.1212/NXI.0000000000000225.
• Probstel AK, Rudolf G, Dornmair K, Collongues N, Chanson JB, Sanderson NS, et al. Anti-MOG antibodies are present in a subgroup of patients with a neuromyelitis optica phenotype. J Neuroinflammation. 2015;12:46. https://doi.org/10.1186/s12974-015-0256-1. This article includes pediatric NMOSD patients who are also MOG antibody positive.
Lechner C, Baumann M, Hennes EM, Schanda K, Marquard K, Karenfort M, et al. Antibodies to MOG and AQP4 in children with neuromyelitis optica and limited forms of the disease. J Neurol Neurosurg Psychiatry. 2016;87(8):897–905. https://doi.org/10.1136/jnnp-2015-311743.
van Pelt ED, Wong YY, Ketelslegers IA, Hamann D, Hintzen RQ. Neuromyelitis optica spectrum disorders: comparison of clinical and magnetic resonance imaging characteristics of AQP4-IgG versus MOG-IgG seropositive cases in the Netherlands. Eur J Neurol. 2016;23(3):580–7. https://doi.org/10.1111/ene.12898.
Kitley J, Waters P, Woodhall M, Leite MI, Murchison A, George J, et al. Neuromyelitis optica spectrum disorders with aquaporin-4 and myelin-oligodendrocyte glycoprotein antibodies: a comparative study. JAMA Neurol. 2014;71(3):276–83. https://doi.org/10.1001/jamaneurol.2013.5857.
Jarius S, Ruprecht K, Kleiter I, Borisow N, Asgari N, Pitarokoili K, et al. MOG-IgG in NMO and related disorders: a multicenter study of 50 patients. Part 2: epidemiology, clinical presentation, radiological and laboratory features, treatment responses, and long-term outcome. J Neuroinflammation. 2016;13(1):280. https://doi.org/10.1186/s12974-016-0718-0.
• Hennes EM, Baumann M, Schanda K, Anlar B, Bajer-Kornek B, Blaschek A, et al. Prognostic relevance of MOG antibodies in children with an acquired demyelinating syndrome. Neurology. 2017;89(9):900–8. https://doi.org/10.1212/WNL.0000000000004312. This article includes the longest follow up time on pediatric NMOSD.
Ramanathan S, Prelog K, Barnes EH, Tantsis EM, Reddel SW, Henderson AP, et al. Radiological differentiation of optic neuritis with myelin oligodendrocyte glycoprotein antibodies, aquaporin-4 antibodies, and multiple sclerosis. Mult Scler. 2016;22(4):470–82. https://doi.org/10.1177/1352458515593406.
Wang JJ, Jaunmuktane Z, Mummery C, Brandner S, Leary S, Trip SA. Inflammatory demyelination without astrocyte loss in MOG antibody-positive NMOSD. Neurology. 2016;87(2):229–31. https://doi.org/10.1212/WNL.0000000000002844.
Misu T, Hoftberger R, Fujihara K, Wimmer I, Takai Y, Nishiyama S, et al. Presence of six different lesion types suggests diverse mechanisms of tissue injury in neuromyelitis optica. Acta Neuropathol. 2013;125(6):815–27. https://doi.org/10.1007/s00401-013-1116-7.
Abboud H, Petrak A, Mealy M, Sasidharan S, Siddique L, Levy M. Treatment of acute relapses in neuromyelitis optica: steroids alone versus steroids plus plasma exchange. Mult Scler. 2016;22(2):185–92. https://doi.org/10.1177/1352458515581438.
Kimbrough DJ, Fujihara K, Jacob A, Lana-Peixoto MA, Leite MI, Levy M, et al. Treatment of neuromyelitis optica: review and recommendations. Mult Scler Relat Disord. 2012;1(4):180–7. https://doi.org/10.1016/j.msard.2012.06.002.
Trebst C, Jarius S, Berthele A, Paul F, Schippling S, Wildemann B, et al. Update on the diagnosis and treatment of neuromyelitis optica: recommendations of the neuromyelitis optica study group (NEMOS). J Neurol. 2014;261(1):1–16. https://doi.org/10.1007/s00415-013-7169-7.
Huh SY, Kim SH, Hyun JW, Joung AR, Park MS, Kim BJ, et al. Mycophenolate mofetil in the treatment of neuromyelitis optica spectrum disorder. JAMA Neurol. 2014;71(11):1372–8. https://doi.org/10.1001/jamaneurol.2014.2057.
Jacob A, Matiello M, Weinshenker BG, Wingerchuk DM, Lucchinetti C, Shuster E, et al. Treatment of neuromyelitis optica with mycophenolate mofetil: retrospective analysis of 24 patients. Arch Neurol. 2009;66(9):1128–33. https://doi.org/10.1001/archneurol.2009.175.
Montcuquet A, Collongues N, Papeix C, Zephir H, Audoin B, Laplaud D, et al. Effectiveness of mycophenolate mofetil as first-line therapy in AQP4-IgG, MOG-IgG, and seronegative neuromyelitis optica spectrum disorders. Mult Scler. 2017;23(10):1377–84. https://doi.org/10.1177/1352458516678474.
Mealy MA, Wingerchuk DM, Palace J, Greenberg BM, Levy M. Comparison of relapse and treatment failure rates among patients with neuromyelitis optica: multicenter study of treatment efficacy. JAMA Neurol. 2014;71(3):324–30. https://doi.org/10.1001/jamaneurol.2013.5699.
Chen H, Qiu W, Zhang Q, Wang J, Shi Z, Liu J, et al. Comparisons of the efficacy and tolerability of mycophenolate mofetil and azathioprine as treatments for neuromyelitis optica and neuromyelitis optica spectrum disorder. Eur J Neurol. 2017;24(1):219–26. https://doi.org/10.1111/ene.13186.
• Kim SH, Hyun JW, Joung A, Park EY, Joo J, Kim HJ. Predictors of response to first-line immunosuppressive therapy in neuromyelitis optica spectrum disorders. Mult Scler. 2017;1352458516687403:1902–8. https://doi.org/10.1177/1352458516687403. This paper discusses the use of rituximab, including monitoring, B cell repopulation correlating with relapses and redosing in pediatric NMOSD.
Henegar CE, Eudy AM, Kharat V, Hill DD, Bennett D, Haight B. Progressive multifocal leukoencephalopathy in patients with systemic lupus erythematosus: a systematic literature review. Lupus. 2016;25(6):617–26. https://doi.org/10.1177/0961203315622819.
Mahmood NA, Silver K, Onel K, Ko M, Javed A. Efficacy and safety of rituximab in pediatric neuromyelitis optica. J Child Neurol. 2011;26(2):244–7. https://doi.org/10.1177/0883073810381445.
Nosadini M, Alper G, Riney CJ, Benson LA, Mohammad SS, Ramanathan S, et al. Rituximab monitoring and redosing in pediatric neuromyelitis optica spectrum disorder. Neurol Neuroimmunol Neuroinflamm. 2016;3(1):e188. https://doi.org/10.1212/NXI.0000000000000188.
Longoni G, Banwell B, Filippi M, Yeh EA. Rituximab as a first-line preventive treatment in pediatric NMOSDs: preliminary results in 5 children. Neurol Neuroimmunol Neuroinflamm. 2014;1(4):e46. https://doi.org/10.1212/NXI.0000000000000046.
Nikoo Z, Badihian S, Shaygannejad V, Asgari N, Ashtari F. Comparison of the efficacy of azathioprine and rituximab in neuromyelitis optica spectrum disorder: a randomized clinical trial. J Neurol. 2017;264:2003–9. https://doi.org/10.1007/s00415-017-8590-0.
Tien YC, Yen HH, Chiu YM. Incidence and clinical characteristics of hepatitis B virus reactivation in HBsAg-negative/HBcAb-positive patients receiving rituximab for rheumatoid arthritis. Clin Exp Rheumatol. 2017;35(5):831–6.
Kelly D, Monaghan B, McMahon E, Watson G, Kavanagh E, O'Rourke K, et al. Progressive multifocal leukoencephalopathy secondary to rituximab-induced immunosuppression and the presence of John Cunningham virus: a case report and literature review. Radiol Case Rep. 2016;11(3):251–4. https://doi.org/10.1016/j.radcr.2016.06.003.
Costanzi C, Matiello M, Lucchinetti CF, Weinshenker BG, Pittock SJ, Mandrekar J, et al. Azathioprine: tolerability, efficacy, and predictors of benefit in neuromyelitis optica. Neurology. 2011;77(7):659–66. https://doi.org/10.1212/WNL.0b013e31822a2780.
Elsone L, Kitley J, Luppe S, Lythgoe D, Mutch K, Jacob S, et al. Long-term efficacy, tolerability and retention rate of azathioprine in 103 aquaporin-4 antibody-positive neuromyelitis optica spectrum disorder patients: a multicentre retrospective observational study from the UK. Mult Scler. 2014;20(11):1533–40. https://doi.org/10.1177/1352458514525870.
Yaguchi H, Sakushima K, Takahashi I, Nishimura H, Yashima-Yamada M, Nakamura M, et al. Efficacy of intravenous cyclophosphamide therapy for neuromyelitis optica spectrum disorder. Intern Med. 2013;52(9):969–72.
Xu Y, Wang Q, Ren HT, Qiao L, Zhang Y, Fei YY, et al. Comparison of efficacy and tolerability of azathioprine, mycophenolate mofetil, and cyclophosphamide among patients with neuromyelitis optica spectrum disorder: a prospective cohort study. J Neurol Sci. 2016;370:224–8. https://doi.org/10.1016/j.jns.2016.09.035.
Bichuetti DB, Oliveira EM, Boulos Fde C, Gabbai AA. Lack of response to pulse cyclophosphamide in neuromyelitis optica: evaluation of 7 patients. Arch Neurol. 2012;69(7):938–9. https://doi.org/10.1001/archneurol.2012.545.
Kim SH, Kim W, Li XF, Jung IJ, Kim HJ. Does interferon beta treatment exacerbate neuromyelitis optica spectrum disorder? Mult Scler. 2012;18(10):1480–3. https://doi.org/10.1177/1352458512439439.
Wang KC, Lin KH, Lee TC, Lee CL, Chen SY, Chen SJ, et al. Poor responses to interferon-beta treatment in patients with neuromyelitis optica and multiple sclerosis with long spinal cord lesions. PLoS One. 2014;9(6):e98192. https://doi.org/10.1371/journal.pone.0098192.
Ayzenberg I, Schollhammer J, Hoepner R, Hellwig K, Ringelstein M, Aktas O, et al. Efficacy of glatiramer acetate in neuromyelitis optica spectrum disorder: a multicenter retrospective study. J Neurol. 2016;263(3):575–82. https://doi.org/10.1007/s00415-015-7991-1.
Yamout BI, Beaini S, Zeineddine MM, Akkawi N. Catastrophic relapses following initiation of dimethyl fumarate in two patients with neuromyelitis optica spectrum disorder. Mult Scler. 2017;23(9):1297–300. https://doi.org/10.1177/1352458517694086.
Azzopardi L, Cox AL, McCarthy CL, Jones JL, Coles AJ. Alemtuzumab use in neuromyelitis optica spectrum disorders: a brief case series. J Neurol. 2016;263(1):25–9. https://doi.org/10.1007/s00415-015-7925-y.
Lee DH, Laemmer AB, Waschbisch A, Struffert T, Maihofner C, Schwab S, et al. Neuromyelitis optica presenting with relapses under treatment with natalizumab: a case report. J Med Case Rep. 2014;8:155. https://doi.org/10.1186/1752-1947-8-155.
Kitley J, Evangelou N, Kuker W, Jacob A, Leite MI, Palace J. Catastrophic brain relapse in seronegative NMO after a single dose of natalizumab. J Neurol Sci. 2014;339(1–2):223–5. https://doi.org/10.1016/j.jns.2014.01.035.
Jacob A, Hutchinson M, Elsone L, Kelly S, Ali R, Saukans I, et al. Does natalizumab therapy worsen neuromyelitis optica? Neurology. 2012;79(10):1065–6. https://doi.org/10.1212/WNL.0b013e31826845fe.
Icoz S, Tuzun E, Kurtuncu M, Durmus H, Mutlu M, Eraksoy M, et al. Enhanced IL-6 production in aquaporin-4 antibody positive neuromyelitis optica patients. Int J Neurosci. 2010;120(1):71–5. https://doi.org/10.3109/00207450903428970.
Uzawa A, Mori M, Ito M, Uchida T, Hayakawa S, Masuda S, et al. Markedly increased CSF interleukin-6 levels in neuromyelitis optica, but not in multiple sclerosis. J Neurol. 2009;256(12):2082–4. https://doi.org/10.1007/s00415-009-5274-4.
Araki M, Matsuoka T, Miyamoto K, Kusunoki S, Okamoto T, Murata M, et al. Efficacy of the anti-IL-6 receptor antibody tocilizumab in neuromyelitis optica: a pilot study. Neurology. 2014;82(15):1302–6. https://doi.org/10.1212/WNL.0000000000000317.
Ringelstein M, Ayzenberg I, Harmel J, Lauenstein AS, Lensch E, Stogbauer F, et al. Long-term therapy with interleukin 6 receptor blockade in highly active neuromyelitis optica spectrum disorder. JAMA Neurol. 2015;72(7):756–63. https://doi.org/10.1001/jamaneurol.2015.0533.
Marino A, Narula S, Lerman MA. First pediatric patient with neuromyelitis optica and Sjogren syndrome successfully treated with tocilizumab. Pediatr Neurol. 2017;73:e5–6. https://doi.org/10.1016/j.pediatrneurol.2017.05.015.
Machado SH, Xavier RM. Safety of tocilizumab in the treatment of juvenile idiopathic arthritis. Expert Opin Drug Saf. 2017;16(4):493–500. https://doi.org/10.1080/14740338.2017.1303479.
Spencer CH, Rouster-Stevens K, Gewanter H, Syverson G, Modica R, Schmidt K, et al. Biologic therapies for refractory juvenile dermatomyositis: five years of experience of the childhood arthritis and rheumatology research alliance in North America. Pediatr Rheumatol Online J. 2017;15(1):50. https://doi.org/10.1186/s12969-017-0174-0.
Saadoun S, Waters P, Bell BA, Vincent A, Verkman AS, Papadopoulos MC. Intra-cerebral injection of neuromyelitis optica immunoglobulin G and human complement produces neuromyelitis optica lesions in mice. Brain. 2010;133(Pt 2):349–61. https://doi.org/10.1093/brain/awp309.
Pittock SJ, Lennon VA, McKeon A, Mandrekar J, Weinshenker BG, Lucchinetti CF, et al. Eculizumab in AQP4-IgG-positive relapsing neuromyelitis optica spectrum disorders: an open-label pilot study. Lancet Neurol. 2013;12(6):554–62. https://doi.org/10.1016/S1474-4422(13)70076-0.
Mercuri A, Farruggia P, Timeus F, Lombardi L, Onofrillo D, Putti MC, et al. A retrospective study of paroxysmal nocturnal hemoglobinuria in pediatric and adolescent patients. Blood Cells Mol Dis. 2017;64:45–50. https://doi.org/10.1016/j.bcmd.2017.03.006.
Loirat C, Fakhouri F, Ariceta G, Besbas N, Bitzan M, Bjerre A, et al. An international consensus approach to the management of atypical hemolytic uremic syndrome in children. Pediatr Nephrol. 2016;31(1):15–39. https://doi.org/10.1007/s00467-015-3076-8.
Terano C, Ishikura K, Hamada R, Yoshida Y, Kubota W, Okuda Y, et al. Practical issues in using eculizumab for children with atypical hemolytic uremic syndrome in the acute phase: a review of 4 patients. Nephrology (Carlton). 2017; https://doi.org/10.1111/nep.13054.
Mealy MA, Shin K, John G, Levy M. Bevacizumab is safe in acute relapses of neuromyelitis optica. Clin Exp Neuroimmunol. 2015;6(4):413–8. https://doi.org/10.1111/cen3.12239.
Neuromyelitis optica. http://www.clinicaltrials.gov. Accessed October 20 2017.
Self MM, Fobian A, Cutitta K, Wallace A, Lotze TE. Health-related quality of life in pediatric patients with demyelinating diseases: relevance of disability, relapsing presentation, and fatigue. J Pediatr Psychol. 2017;43:133–42. https://doi.org/10.1093/jpepsy/jsx093.
Tur C. Fatigue management in multiple sclerosis. Curr Treat Options Neurol. 2016;18(6):26. https://doi.org/10.1007/s11940-016-0411-8.
Stankoff B, Waubant E, Confavreux C, Edan G, Debouverie M, Rumbach L, et al. Modafinil for fatigue in MS: a randomized placebo-controlled double-blind study. Neurology. 2005;64(7):1139–43. https://doi.org/10.1212/01.WNL.0000158272.27070.6A.
Zifko UA, Rupp M, Schwarz S, Zipko HT, Maida EM. Modafinil in treatment of fatigue in multiple sclerosis. Results of an open-label study J Neurol. 2002;249(8):983–7. https://doi.org/10.1007/s00415-002-0765-6.
Rammohan KW, Rosenberg JH, Lynn DJ, Blumenfeld AM, Pollak CP, Nagaraja HN. Efficacy and safety of modafinil (Provigil) for the treatment of fatigue in multiple sclerosis: a two centre phase 2 study. J Neurol Neurosurg Psychiatry. 2002;72(2):179–83.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Grace Gombolay declares no conflict of interest.
Tanuja Chitnis is a member of the Steering committee for pediatric clinical trials for Novartis and Sanofi-Genzyme. She has provided one-time consultation for Genzyme-Sanofi, Biogen-Idec, Novartis, Genentech-Roche, and Bayer Pharmaceuticals. She receives grant support from Biogen-Idec, Serono, and Verily.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Multiple Sclerosis and Related Disorders
Rights and permissions
About this article
Cite this article
Gombolay, G.Y., Chitnis, T. Pediatric Neuromyelitis Optica Spectrum Disorders. Curr Treat Options Neurol 20, 19 (2018). https://doi.org/10.1007/s11940-018-0502-9
Published:
DOI: https://doi.org/10.1007/s11940-018-0502-9