Abstract
Cognitive complaint interviews (CCI) have been shown to be useful in the early detection of dementia in elderly people. Surprisingly, CCIs are rarely used in Parkinson’s disease (PD), despite a six-fold higher risk of dementia than in healthy subjects. The present study sought to determine whether a structured CCI could detect cognitive decline in PD. A validated CCI was added to the usual clinical interview for 180 PD patients. Objective cognitive status was assessed by the Mattis dementia rating scale score. The CCIs ability to detect cognitive decline in PD patients was determined using a receiver operating characteristic (ROC) curve. 58 (32.22%) patients had a significant, subjective cognitive complaint (CCI score >3). Of these, 48.27% had objective cognitive decline. Objective cognitive decline was significantly more frequent in the patients with subjective cognitive complaint. However, the ROC curve for discriminating between patients with and without objective cognitive deficits as a function of their subjective cognitive complaint had low sensitivity (0.50, 95% CI: 0.36–0.64) and moderate specificity (0.74, 95% CI: 0.69–0.84). Logistic regression incorporating the main demographical and clinical variables showed that the CCI score’s discriminant power was improved by adding age and the number of years in education to the predictive model. Objective cognitive decline and dementia are more frequent among PD patients reporting a cognitive complaint than among patients not reporting a complaint. However, the CCI does not enable more accurate screening for PD-associated dementia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is a progressive, degenerative, neurological disorder that is characterized most obviously by its motor manifestations (rest tremor, rigidity, akinesia and postural instability). The condition is also associated with change in cognitive functions—sometimes even very early in the course of the disease [1, 2]. Non-demented PD patients exhibit relatively circumscribed executive deficits and secondary disturbances in several other cognitive domains (e.g., memory and visuospatial abilities). Over the natural course of the disease, cognitive function declines and dementia will affect about 40% of PD patients, with a six-fold greater incidence than in healthy subjects [3]. The decline typically includes difficulties in executive and visuospatial functions, as well as memory deficits [4, 5]. Detecting cognitive decline in PD patients is of importance because dementia increases the health care burden and the frequency of institutionalization and reduces quality of life for both patients and carers [6–8]. Moreover, cholinesterase inhibitor drugs with demonstrated efficacy in PD-associated dementia are now available [9]. However, given that performing an extensive cognitive assessment takes time and consumes medical resources, there is a need for brief screening procedures in clinical practice. Several cognitive short tests or batteries have been tested for their discriminant power, with mixed results. It has recently been shown that a number of cognitive bedside assessment procedures can screen for cognitive decline in PD more effectively than the mini mental state examination (MMSE) does, since the latter is not very sensitive to executive and visuospatial dysfunction [10–13]. However, the discriminant power of a cognitive complaint interview (CCI) has never been assessed in PD, despite the fact that several studies in the elderly have suggested that cognitive complaints (when recorded using standardized items) may help to predict dementia [14–18]. Hence, we decided to establish whether the CCI might constitute a rapid, easy-to-perform procedure for screening for PD patients with cognitive decline. Even though the dementia in PD has an insidious onset, the condition is often characterized by a worsening in memory deficits (i.e., greater difficulty encoding new information) and executive and attention impairments (with greater distractibility and unusual errors)—the disorders that are targeted specifically by the CCI.
The main aim of the present study was to determine the ability of a validated French-language CCI to detect cognitive decline (as evidenced by an objective measurement of cognitive status) in PD patients. We also sought to determine whether the cognitive profile of PD patients with a subjective cognitive complaint (perhaps suggesting dementia onset) differed from that of patients without such a complaint.
Methods
Patients
One hundred and eighty consecutive patients with probable PD [80 women; mean (SD) age: 62 (10); 11 (3) years of education; 10 (7) years since disease onset; mean (SD) score on the unified Parkinson’s disease rating scale (UPDRS) part III: 20.65 (10.4)] participated in the study. Parkinson’s disease was defined according to international criteria [19]. All patients were assessed after receiving their usual anti-Parkinsonian medication. None of the patients was suffering from neurological diseases other than PD.
An additional group of 50 patients (25 with subjective cognitive complaints and 25 without) underwent an extensive neuropsychological assessment. The two subgroups were strictly matched with regard to age, the number of years in education and the severity of motor symptoms. None of the 50 patients was suffering from depression, according to the DSM-IV criteria. Marsh et al.’s recommendations [20] were used to diagnose depression. The subgroups’ demographic and clinical characteristics are shown in Table 1.
All participants gave their informed consent to participation in the study.
Cognitive assessment
Cognitive complaints were assessed using a validated, French-language CCI [17, 21], that consists of 10 questions about changes in cognitive function having occurred over the previous 6 months (see Table 2). CCI is rater-administered and does not involve the caregiver. A score over 3 is considered to reflect a complaint [17, 21]. The CCI was administered in addition to the usual clinical interview. The severity of the depressive symptoms was assessed in terms of the score on the Montgomery and Asberg depression rating scale (MADRS) [22].
Overall cognitive status was assessed on the Mattis dementia rating scale (DRS). A cut-off of 130 was used to judge the presence or absence of objective cognitive decline [23–25]. Moreover, in patients with a Mattis DRS score below 130, we applied the DSM-IV criteria for dementia, according to Emre et al.’s recommendations [26] for PD-associated dementia. Forty-two patients met these criteria.
The extensive neuropsychological assessment encompassed a series of tests for detecting cognitive dysfunction in PD patients: the forward and backward digit span test, the French version of the Grober and Buschke 16-item free/cued word learning and recall test [27], according to the procedure described by Pillon et al. [28]; performance was assessed as the total number of words (out of 48) correctly free-recalled and the total number of words (out of 48) correctly remembered after free and cued recall), the Stroop word color test (described in full elsewhere [29]; performance was evaluated in terms of an interference index), a letter and number sequencing task corresponding to an oral version of the Trail Making Test (described in full elsewhere [29]; performance was evaluated in terms of an alternation cost index), and a word-generation task (performed over 60 s and under phonemic, semantic and alternating conditions).
Data analysis
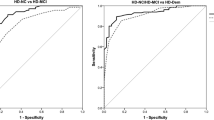
The CCI’s discriminant power in detecting cognitive decline in PD patients was determined using the receiver operating characteristic (ROC) curve and the area under the ROC curve (AUC) with a 95% confidence interval.
Sensitivity (the probability of obtaining a CCI score over 3 if the patient has objective cognitive decline) and specificity (the probability of obtaining a CCI score below 4 if the patient does not have objective cognitive decline) were also calculated, with a 95% confidence interval.
An item-based analysis was performed using a squared, multiple-regression coefficient.
Logistic regression was then performed in order to identify factors capable of enhancing the accuracy of the decision criteria. The multivariate model’s goodness of fit was assessed in terms of the area under the ROC curve and by applying the Hosmer Lemeshow test (also referred to as a calibration test) to determine whether there were differences between the observed and the predicted probabilities of the event.
The multivariate model’s validity was assessed using a cross-validation procedure, as follows: for each patient i, a model M-i is derived from the sample obtained after elimination of the patient i. The cross-validation score (a linear predictor) for i is computed from the coefficients of the model M-i with the characteristics of the patient i. The cross-validation score can be considered as a new covariate. If this covariate is introduced in a logistic regression, the model is considered to be valid if the parameter associated with this new covariate is close to 1 (>0.85).
A multivariate analysis of variance (MANOVA) with “group” (with and without cognitive complaints) as the between-factor was performed on all the parameters in the extensive cognitive assessment. The significance threshold was set at p < 0.05.
Results
The CCI results showed that 58 (32.22%) patients had a significant, subjective cognitive complaint (CCI score >3). Of these patients, 28 (48.27%) had objective cognitive decline (Mattis DRS score <130) of whom 26 (44.83%) met the criteria for dementia. Of the 122 patients free of cognitive complaints, 31 (25.41%) had objective cognitive decline of whom 28 (22.95%) met the criteria for dementia. The frequency of objective cognitive decline was significantly higher in patients with a subjective cognitive complaint (χ 2 = 11.764, p = 0.001).
Discriminant power of the CCI
Despite significantly different mean scores, the probability density function showed a considerable overlap of the CCI score distributions as a function of the presence or absence of an objective cognitive decline (see Fig. 1).
The ROC curve for discriminating between patients with and without objective cognitive deficits as a function of their cognitive complaint status revealed low sensitivity (0.50, 95% CI: 0.36–0.64) and moderate specificity (0.74, 95% CI: 0.69–0.84) for the CCI’s usual cut-off score. As seen in Fig. 2, no other cut-off value was able to yield a better sensitivity/specificity compromise (AUC = 0.69, 95% CI: 0.60–0.77).
An item-based multiple-regression analysis showed that over 90% of the variance was explained by 6 of the 10 questions. However, consideration of these items did not improve the questionnaire’s discriminant power (AUC = 0.72, 95% CI: 0.63–0.80).
The logistic regression analysis incorporating the main demographical and clinical variables (i.e., age, number of years in education, disease duration, severity of motor symptoms and severity of the anxious-depressive symptoms) showed that it was possible to significantly enhance the CCI’s discriminant power by adding in two items of demographic information: age and number of years in education. Thereafter, the AUC was 0.84 (95% CI: 0.78–0.90, see Fig. 3), with a good calibration result (Hosmer Lemeshow test: p = 0.41). The cross-validation covariate was associated with a coefficient value of 0.89 (i.e., close to 1). The composite score calculated from the logistic regression equation enabled determination of the risk of objective cognitive decline according to the patient’s age, number of years in education and severity of the cognitive complaint, as follows: −5.40 + 0.098 × age – 0.27 × number of years in education +0.38 × CCI score. For example, in a 70-year-old subject with 8 years in education and a CCI score of 5, the probability of objective cognitive decline was 0.77.
Comparisons of subgroups with and without cognitive complaints
The mean (SD) results for the cognitive assessment in both patient subgroups are shown in Table 3.
The MANOVA did not reveal any significant group effect (Wilks’ lambda, F (14,36) = 1.91, p = 0.059). The two groups did not differ in terms of any of the cognitive assessment’s parameters.
Discussion
The present results show that objective cognitive decline and dementia are more frequent among PD patients reporting a cognitive complaint than among those not reporting such a complaint. However, use of the CCI score does not facilitate screening for PD-associated dementia. Indeed, for PD patients with a significant cognitive complaint, the proportion of patients with and without objective cognitive decline was quite similar—leading to very low sensitivity in a CCI-based test. Moreover, the CCI’s discriminant power was not improved by varying the cut-off score and an item-based analysis did not enable identification of a selection of items that improved the discrimination. Nevertheless, our results suggest that one way to improve the CCI’s ability to detect PD patients with dementia is to use age and the number of years in education as additional information. Although the validity of this predictive logistic equation has yet to be assessed on an independent series of patients, cross-validation yielded satisfactory results.
A further objective of this study was to investigate any cognitive profile differences between PD patients with and without cognitive complaints. An extensive neuropsychological assessment of two strictly matched patient subgroups revealed that whatever the cognitive domain, PD patients with significant cognitive complaints performed as well as those without complaints. The only difference between the groups was a significantly higher MADRS score for the patients with cognitive complaints, than in patients without complaints (see Table 1). Although none of the study patients met the DSM-IV criteria for depression (since depression was an exclusion criterion), anxious-depressive symptoms were more severe and/or more numerous in patients with complaints. This suggests that patients with complaints had more concerns about their situation in general and their cognitive status in particular and were thus, more likely to complain than the others. This hypothesis is in line with the results reported by Rouch et al. [30] in non-institutionalized, elderly individuals.
Overall, our present results do not support the use of a CCI as a rapid, easy-to-use instrument for helping detect cognitive decline in PD patients. However, a number of study limitations must be considered. Firstly, the CCI we used was initially designed for elderly subjects in general and has mainly been used for the detection of mild cognitive impairment and Alzheimer’s disease (AD) in memory clinic outpatients. It was initially designed to detect the cognitive difficulties typically associated with AD (forgetting whole events, anomia, orientation difficulties, lack of interest, etc.). Consequently, the CCI does not feature items that are specific for PD-associated cognitive difficulties, such as executive dysfunction. It is possible that the addition of more PD-specific items could increase the CCI’s discriminant power. This also highlights the specificity of PD-associated dementia which is mainly characterized by impaired attention and executive and visuospatial functions [3]. Secondly, the cognitive complaints dealt with here were only patient-rated and an informant’s opinion was not incorporated in the evaluation. Hence, it is possible that some of the patients with objective cognitive decline were not aware of their difficulties and, as a result, did not complain. This eventuality may have reduced the CCI’s sensitivity. Comparing the patient’s opinion with a reliable opinion from a caregiver could also help enhance the procedure’s discriminant power. Thirdly, all the study patients had suffered from PD for several years (10 years, on average). It is thus, very likely that they had already been experiencing cognitive symptoms for a long while and were thus, perhaps less sensitive to recent changes in their cognitive status. This possibility may also explain the low rate of complaints among those with objective cognitive decline. Lastly, the present study’s cross-sectional design may also induce bias. Indeed, some of the patients with objective cognitive decline and/or dementia had suffered from these conditions for more than 6 months; however, the CCI only deals with changes having occurred over the previous 6 months. It is thus, possible that some patients reported no change but were well aware of their difficulties. A longitudinal design would provide more information on changes over time and could help determine more precisely the CCI’s ability to detect cognitive changes heralding dementia in PD.
Overall, our results suggest that due to its specificity, PD-associated dementia has effects on the reporting of cognitive complaints that differ clearly from those usually associated with AD and thus, needs to be detected by using specific signs of cognitive and behavioral change.
In conclusion, although subjective cognitive complaints are related to objective cognitive decline in PD patients, the CCI does not have adequate clinimetric properties for detecting dementia in PD patients. Our present results underline the difficulty of rapid screening for cognitive decline in PD and highlight the need to develop new instruments which take account of the condition’s specific features, incorporate a caregiver opinion and assess recent changes in the patient’s activities of daily living.
References
Dujardin K et al (1999) Neuropsychological abnormalities in first degree relatives of patients with familial Parkinson’s disease. J Neurol Neurosurg Psychiatry 67(3):323–328
Muslimovic D et al (2005) Cognitive profile of patients with newly diagnosed Parkinson disease. Neurology 65(8):1239–1245
Emre M (2003) Dementia associated with Parkinson’s disease. Lancet Neurol 2(4):229–237
Emre M (2004) Dementia in Parkinson’s disease: cause and treatment. Curr Opin Neurol 17(4):399–404
Bosboom JL, Stoffers D, Wolters E (2004) Cognitive dysfunction and dementia in Parkinson’s disease. J Neural Transm 111(10–11):1303–1315
Martinez-Martin P et al (2005) Quality of life of caregivers in Parkinson’s disease. Qual Life Res 14(2):463–472
Buter TC et al (2008) Dementia and survival in Parkinson disease: a 12-year population study. Neurology 70(13):1017–1022
Parashos SA et al (2002) Medical services utilization and prognosis in Parkinson disease: a population-based study. Mayo Clin Proc 77(9):918–925
Emre M et al (2004) Rivastigmine for dementia associated with Parkinson’s disease. N Engl J Med 351(24):2509–2518
Bak TH et al (2005) Cognitive bedside assessment in atypical Parkinsonian syndromes. J Neurol Neurosurg Psychiatry 76(3):420–422
Athey RJ, Walker RW (2006) Demonstration of cognitive decline in Parkinson’s disease using the Cambridge cognitive assessment (Revised CAMCOG-R). Int J Geriatr Psychiatry 21(10):977–982
Zadikoff C et al (2008) A comparison of the mini mental state exam to the montreal cognitive assessment in identifying cognitive deficits in Parkinson’s disease. Mov Disord 23(2):297–299
Marinus J et al (2003) Assessment of cognition in Parkinson’s disease. Neurology 61(9):1222–1228
Schmand B et al (1996) Subjective memory complaints may announce dementia. Neurology 46(1):121–125
Schofield PW et al (1997) The validity of new memory complaints in the elderly. Arch Neurol 54(6):756–759
Gagnon M et al (1994) Self-reported memory complaints and memory performance in elderly French community residents: results of the PAQUID Research Program. Neuroepidemiology 13(4):145–154
Thomas-Anterion C. et al. (2003) Le questionnaire de plainte cognitive: un outil de recherche de plainte suspecte d’évoquer une maladie d’Alzheimer? L’année gérontologique 56–65
Miranda B et al (2008) Self-perceived memory impairment and cognitive performance in an elderly independent population with age-related white matter changes. J Neurol Neurosurg Psychiatry 79(8):869–873
Gelb DJ, Oliver E, Gilman S (1999) Diagnostic criteria for Parkinson disease. Arch Neurol 56(1):33–39
Marsh L et al (2006) Provisional diagnostic criteria for depression in Parkinson’s disease: report of an NINDS/NIMH work group. Mov Disord 21(2):148–158
Thomas-Anterion C, Honore-Masson S, Laurent B (2006) The cognitive complaint interview. Psychogeriatrics 6(1):18–22
Montgomery SA, Asberg M (1979) A new depression scale designed to be sensitive to change. Br J Psychiatry 134:382–389
Monsch AU et al (1995) Clinical validity of the Mattis dementia rating scale in detecting dementia of the Alzheimer type. A double cross-validation and application to a community-dwelling sample. Arch Neurol 52(9):899–904
Brown GG et al (1999) Validity of the dementia rating scale in assessing cognitive function in Parkinson’s disease. J Geriatr Psychiatry Neurol 12(4):180–188
Green RC, Woodard JL, Green J (1995) Validity of the Mattis dementia rating scale for detection of cognitive impairment in the elderly. J Neuropsychiatry Clin Neurosci 7(3):357–360
Emre M et al (2007) Clinical diagnostic criteria for dementia associated with Parkinson’s disease. Mov Disord 22(12):1689–1707 quiz 1837
Van der Linden M (2004) L’épreuve de rappel libre/rappel indicé à 16 items (RL/RI-16). In: Van der Linden M, Gremem et al (eds) L’évaluation des troubles de la mémoire. Solal, Marseille, pp 25–47
Pillon B et al (1993) Explicit memory in Alzheimer’s, Huntington’s, and Parkinson’s diseases. Arch Neurol 50(4):374–379
Dujardin K et al (2001) Memory and executive function in sporadic and familial Parkinson’s disease. Brain 124(Pt 2):389–398
Rouch I et al (2008) Cognitive complaints, neuropsychological performance and affective disorders in elderly community residents. Disabil Rehabil 30(23):1794–1802
Conflicts of interest statement
The authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dujardin, K., Duhamel, A., Delliaux, M. et al. Cognitive complaints in Parkinson’s disease: its relationship with objective cognitive decline. J Neurol 257, 79–84 (2010). https://doi.org/10.1007/s00415-009-5268-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-009-5268-2