Abstract
Post–mortem computed tomography (PMCT) is a routine tool in many forensic pathology departments as it is fast and non-destructive and allows less gruesome visualization than photographs, and the images are indefinitely storable. Several studies investigated congruence between PMCT and autopsy for skull fracture but registered only the presence or absence of fracture systems. The objective of this study was to determine location-specific sensitivity and specificity of PMCT for individual fracture lines in blunt force head trauma. Accurate 3D models based on PMCT data with all fracture lines visible are important for future studies on fractures, applying finite element analysis (FEA). We retrospectively sampled adult cases from 2013 to 2019 with skull fracture mentioned in the autopsy report. PMCT was on a Siemens 64-slice scanner and autopsy according to international guidelines. The location and direction of all fracture lines at autopsy and at de novo interpretation of scans were registered and compared. Ninety-nine cases with 4809 individual findings were included. Age ranged from 18 to 100 years. The overall sensitivity was 0.58, and specificity was 0.91. For individual locations, sensitivity ranged from 0.24 to 0.85, and specificity ranged from 0.73 to 1.00. Intra-observer agreement was 0.74, and inter-observer agreement ranged from 0.43 to 0.58. In conclusion, PMCT is suited for detection of fracture systems, but not for detection of all individual fracture lines. Our results differed from the existing literature due to the methodological choices of registering individual fracture lines. Future studies utilising FEA must supplement PMCT with autopsy data.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Post-mortem computed tomography (PMCT) is an established supplement to forensic autopsy in both accidental and natural death [1,2,3,4]. PMCT debuted in the forensic realm in 1977 [5] and is the subject of much research [6], and several forensic institutions routinely use non-contrast PMCT prior to autopsy [7,8,9,10].
PMCT is non-destructive and rapid, and data are indefinitely storable. The acquired image data allow for easy-to-understand visual demonstration, 3D printing, crime scene reconstruction, animation of events prior to death [11,12,13], and simulation of different scenarios with advanced techniques such as finite element analysis (FEA) [14, 15].
We aim to perform FEA of blunt force skull trauma in future studies and need to determine if PMCT data are precise enough. FEA is an engineering tool in which a virtual force is applied to a computer model that simulates a fracture pattern, which provides a repeatable, objective, and observer-independent analysis of skull fracture. It is important to identify all fractures to match a FEA of a proposed scenario to the fractures seen at autopsy. In forensic pathology, all fractures are important, as they can be evidence of a specific traumatic force. The location, shape, and extent of fracture systems provide information on the direction of impact, number of impacts, force of impact, and shape of the impacting object. Several papers have compared PMCT to autopsy for skull fracture detection [16,17,18,19,20,21,22] and found sensitivities ranging from 0.67 to 1.00 and specificities ranging from 0.66 to 1.00, with the majority of studies reporting values above 0.90 for both. Methodologically, these studies consider the base and the vault separately, and the presence of any fracture system, no matter the number of fractures or the extent of fracture systems, constitutes a single positive finding, i.e. a fracture is either present or absent. In studies with many cases without and few cases with skull fracture, specificity will appear high as the number of true negatives is included in both the numerator and denominator, with only a small numerical contribution to the denominator from false positives.
The objective of this study was to establish sensitivity and specificity of PMCT for detection of individual fracture lines for each of the bones of the neuro-cranium in blunt force head trauma in adults, in order to facilitate future research with FEA.
Materials and methods
This was a retrospective study of autopsy reports from 2013 to 2019 and de novo interpretation of PMCT images. The Section of Forensic Pathology, Department of Forensic Medicine, University of Copenhagen (UCPH), handled all forensic autopsies requested by the police, the Danish Patient Safety Authority, the Transportation Safety Boards, and the Labour Market Insurance (private institution under governmental oversight) in eastern Denmark. Cases both scanned and autopsied, and with either a certain or a possible skull fracture mentioned in either the “PMCT” section or “internal investigation” section of autopsy reports were included. We excluded cases with non-blunt force skull fracture, neuro-surgery with bone missing at autopsy, age below 18 years, or severely comminuted fractures.
CT scans
The Section of Forensic Pathology scanned all cases on a 64-slice Siemens Somatom Definition scanner (Siemens Medical Solutions, Forchheim, Germany) prior to autopsy. Most deceased were wrapped in hospital sheets with a minor number in body bags. All were in the supine position with arms along the thorax. The tube current varied due to automatic dose modulation. Table 1 summarizes acquisition and reconstruction parameters. Two different scan protocols were used due to a prospective national research project, with parameters differing from routine practice [23].
Image reconstruction and interpretation
PMCT images were analysed with Myrian Expert 2.2 (Intrasense, Montpellier, France) [24] blinded to autopsy results and circumstances of death. Discontinuation of either the inner or the outer table of the cortical bone defined a fracture. Fractures were identified in the axial, coronal, and sagittal planes, registered in a database and drawn on sketches for documentation, see Fig. 1.
The skull was divided into 39 locations based on anatomy and sidedness, as per Table 2. Sutures were considered anatomical locations, and diastasis was registered as such. It was possible for several fractures to appear in one location. A location with no fracture was registered as a true negative. The facial bones were not considered in this study.
Each individual fracture line was registered as an independent data point. When a fracture line progressed into a new anatomical location, it was considered a new fracture line. When a fracture line abruptly changed direction more than ca. 50°, it was also considered a new fracture line. This angle was chosen for ease of determination. In Fig. 1, the fracture system consists of six individual fracture lines. All fracture lines were equally weighted statistically no matter their size or forensic importance. Fracture lines described as old and/or healed at autopsy were excluded from analysis.
Observers
All scans were interpreted by the first author, a junior doctor with approximately 1.5 years of experience in forensic pathology with more than 100 autopsies including full-body PMCT interpretation. The junior doctor has participated in regular departmental post mortem forensic radiology morning conferences of another approximately 300 cases prior to this study. The forensic pathologist holds a PhD degree in PMCT and has more than 15 years of experience with PMCT interpretation. The forensic anthropologist is an associate professor in forensic anthropology and forensic imaging, has attended the Virtopsy course in Switzerland, has more than 10 years of experience with PMCT, and is responsible for all advanced PMCT 3D visualisation analysis at our department. The clinical radiologist has 10 years of experience in radiology including four years of sub-specialisation in musculoskeletal- and trauma radiology.
Autopsy
A junior doctor supervised by a board-certified forensic pathologist performed the autopsies. Autopsy practice followed guidelines as set forth by Recommendation no. R 3 of the Committee of Ministers to Member States on the harmonization of medico-legal autopsy rules (99) and authoritative textbooks such as The Coroner’s Autopsy by Knight and Autopsy Diagnosis and Technique by Saphir [25,26,27,28]. For examination of the skull, the scalp was incised coronally and reflected to the supraorbital ridge anteriorly, the nuchal line superior-posteriorly and to about the external acoustic meatus laterally. With an electric bone saw, the superior part of the vault was removed, and the brain was removed before inspection of the skull base after removal of the dura. It was not routine to inspect the outside of the skull base.
Autopsy reports are standardized and written as full text. Positive findings, especially traumatic changes, are routinely photo-documented at our institution. Sketches, such as Fig. 1, are drawn on an at-need basis and were only available in a handful of cases in this study. We excluded cases with insufficient autopsy data for reliable analysis; thus, all fractures in this study were analysed based on standardized text and photographs.
Statistical Analysis
Cases for intra- and inter-observer analysis were randomly selected. Four observers participated in the inter-observer analysis: a junior doctor, a forensic anthropologist, and a forensic pathologist; all experienced in post mortem cross-sectional imaging, and a radiologist with no forensic experience. Cohen’s kappa was calculated with 0.41–0.60 considered fair agreement, 0.61–0.80 substantial agreement, and 0.81–1.00 considered almost perfect agreement [29].
Autopsy was the reference test when calculating sensitivity and specificity of the index test, PMCT. Sensitivity was the proportion of fracture lines present at autopsy detected by PMCT. It was calculated as the true positives divided by the sum of true positives and false negatives. Specificity was the proportion of anatomical locations without a fracture line at autopsy and without a fracture line detected by PMCT. Each anatomical location could contribute with more than one true-positive, false-positive, and false negative, but only one true negative. Specificity was calculated as the true negatives divided by the sum of true negatives and false positives [30]. Calculations were performed in Excel 16.0 (Microsoft, Redmond, USA).
Results
Ninety-nine deceased were included in the study. There were 77 accidents, one unknown cause of death, seven homicides, seven suicides, and seven natural deaths. Age ranged from 18 to 100 years, with an average of 50.6 years. The male to female ratio was 3.7:1, and Tables 3 and 4 provide information about cause and mechanism of death. Skull fracture would not be expected in some causes of death and mechanisms of death presented in Tables 3 and 4. This study sampled all cases where the autopsy report and/or original PMCT interpretation mentioned a possible skull fracture. In some cases, the underlying cause of death was non-traumatic, but the deceased had suffered a skull fracture when falling to the ground due to e.g. acute myocardial infarction or poisoning.
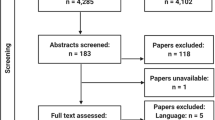
The 99 cases were drawn from 4128 autopsies performed during the study period. Of those, 461 cases were not scanned (technical issues (n = 119), no reason stated in autopsy report (n = 254), did not fit inside scanner (n = 88)). Two hundred fifty cases were initially included, and 151 cases then excluded because of severely comminute fractures (n = 38), gunshot (n = 35), heat burst fractures (n = 20), neurosurgery with bone parts missing (n = 4), sharp trauma (n = 2), chop lesion (n = 1), insufficient reporting (n = 40), wrongful inclusion (n = 5), or age below 18 (n = 6). Neurosurgery with later cranioplasty with the original bone would not result in exclusion. In cases of craniotomy, our department usually receives the surgically removed bone prior to autopsy. This applied to nine cases.
Intra- and inter-observer analysis
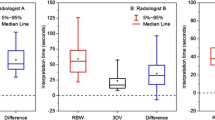
For calculation of intra-observer agreement, we considered the first viewing the reference test. Based on 13 cases, Cohen’s kappa of agreement was 0.76, which is substantial. There were 127 true positive fracture lines, 34 false positive fracture lines, 20 false-negative fracture lines, and 376 locations without fracture, i.e. true negative.
The ten cases for inter-observer analysis yielded a Cohen’s kappa ranging from 0.43 to 0.58. The cases averaged 50 fracture lines and locations without fracture, and the observed inter-observer agreement varied from 0.76 to 0.83. The matrix between all four observers is shown in Table 5. Considering only the presence or absence of fractures in either the vault or base, agreement ranged from 19/20 to 20/20.
Sensitivity and specificity
We found an overall sensitivity of 0.58 and overall specificity of 0.91. For the vault, we found a sensitivity of 0.68 and a specificity of 0.85. The skull base yielded a sensitivity of 0.49 and specificity of 0.84. When grouping the base, we found a sensitivity of 0.40 and specificity of 0.82 for the frontal, ethmoid, and sphenoid bone; sensitivity of 0.55 and specificity 0.91 for the temporal bone and Turkish saddle; and sensitivity of 0.60 and specificity of 0.79 for the occipital bone. For the sutures, i.e. diastasis, we found a sensitivity of 0.60 and specificity of 0.98. Tables 6, 7, and 8 show detail sensitivity and specificity for each anatomical location.
Sensitivity was higher for fractures described as dislocated at autopsy, as demonstrated in Tables 9, 10, 11, and 12.
The sensitivity and specificity of all four individual observers were comparable, as seen in Table 13.
With the methods of prior publications [16,17,18,19,20,21,22], considering the presence or absence of a fracture system, we found a sensitivity of 0.97 for the vault and 0.93 for the base. Specificity would have been 0.58 for the vault and 0.45 for the base. The reasons for the low specificity are explained in the discussion.
Qualitative post hoc analysis
After the quantitative analysis that generated the data, we re-examined the eight poorest performing cases qualitatively. This had no influence on the numbers reported in this paper. Rather, it is an explanatory supplement. In two cases, only some of the several fracture lines constituting a single fracture system in the roof of the orbit were detected, and in another two cases, entire fracture systems comprised of hairline fractures located in the orbital roofs were overlooked. The fractures contributed with a high number of false negatives because they spanned more than one anatomical location or changed direction multiple times. In two cases, only some of the fracture lines radiating from correctly identified hinge fracture systems were identified, possibly due to satisfaction of search [31]. In one case, neurosurgical intervention masked the fracture line, as the surgeon had sawed through it in the lengthwise direction. In one case, artefacts from dental work partly obscured the missed fracture line in the base of the skull, although it was evident upon re-examination. Figure 2 shows examples of “easy” and “difficult” to detect fracture lines as they appear on the macerated skull (not standard practice), the 3D volume rendering (for demonstrative purposes only), and on the axial slice and reformatted coronal slice used for fracture identification in this study.
Examples of a correctly identified fracture line (red arrow) on the macerated skull (A), 3D volume rendering of PMCT data (B), and axial slice (C) and an overlooked fracture (blue arrow) on macerated skull (A), 3D volume rendering (B), and coronal slice (D). The deceased was not scanned in the Frankfurt plane due to rigor
Discussion
In this study, we determined sensitivity and specificity of PMCT for detection of individual fracture lines in each individual bone of the neuro-cranium in adults subjected to blunt force trauma. These anatomical locations are routinely dissected at autopsy and offer a reliable, validated, and generally accepted reference test. We focused this study on blunt force trauma to explore the basis for future studies with FEA of blunt force skull fracture, which is inherently different to sharp and gunshot trauma. This was also the reason for registering individual fracture lines rather than the absence or presence of a fracture system, as we needed to determine whether 3D models generated from PMCT data would provide sufficient data for FEA. The purpose of FEA of skull fractures is to provide an repeatable, objective, and evidence-based analysis of the skull fracture and provide a likelihood of the observed fracture system given the proposed explanation, e.g. an infant falling from a table vs. abuse [15] or an adult slipping in the bath vs. assault [14].
Sensitivity, specificity, and intra- and inter-observer agreement are significantly lower in our study than in the majority of previously published studies on the subject, and we argue that two methodological choices, i.e. registering individual fracture lines instead of presence/absence of fracture systems and including only blunt force skull trauma, are responsible for this. Our findings are virtually identical to the findings of others when we employ the commonly used methods for registering fractures.
Scan parameters vary slightly between clinical and post mortem CT, but image evaluation is similar, thus post mortem interpretation is subjective and subject to the same errors as all radiology [32]. In contrast to autopsy, CT images are easy to re-evaluate as the images are permanently storable. In the 1940s, the realization that radiologists did not always agree with neither themselves nor others when interpreting “routine” chest X-rays caused an eerie and spawned investigation into the subject of intra- and inter-observer agreement [33]. Indeed, “mistakes” and therefore intra-observer and inter-observer variation seem to be an inherent a part of radiology [33,34,35]. A problem in considering PMCT a diagnostic test is that the “cut-off value” for fracture is discrete and potentially varying. It is an internal, perceptual, and cognitive process within each interpreter to determine if what one sees is sufficient to cross the “threshold” needed to decide on the presence of a fracture. The three forensically trained observers exemplify the inter-dependency between sensitivity and specificity and different thresholds: observer 1 had the lowest sensitivity but highest specificity, observer 3 had the highest sensitivity but the lowest specificity, and observer 2 was in between.
Observer 4, a clinical radiologist, had no forensic experience and was not accustomed to the level of detail required, and scored a lower sensitivity. Clinically insignificant fractures or the exact shape of a severe comminute fracture system have no consequences for treatment and require neither detailed description nor the patient burdening and time-consuming scanner settings seen in forensic pathology [36, 37]. However, there have been cases of missed, minute fractures that lead to death [38, 39]. For skull fracture detection, the major difference between post mortem radiology and clinical radiology is the lack of secondary signs such as intra-cranial gas, bleeding, or swelling of the surrounding soft tissue when death is instant [40], and differences in imaging parameters. In this study, only discontinuation of the bone constituted a fracture, and only the axial, coronal, and sagittal slices were available for interpretation. In clinical radiology, tools such as maximum intensity projection, secondary signs of fracture, and knowledge of circumstances will presumably result in both higher sensitivity and specificity than presented here.
Post mortem radiology lies between the specialties of pathology and radiology. In studies on forensic PMCT, a radiologist is most commonly the interpreter [2], and it is generally advised that radiologists are trained in forensic pathology [16, 32, 41]. Radiologists trained in forensic pathology and forensic pathologists trained in radiology may be equally proficient [42], though Leth et al. found a kappa of 0.33 for injuries in the skeletal system and of 0.74 for injuries in the head region when comparing Abbreviated Injury Score (AIS) determined at PMCT by a radiologist and a pathologist [41]. A study on 14 cases of simple skull fractures found that a second reading by a radiologist after initial reading by a forensic pathologist provided additional details in nine cases [43].
Cohen’s kappa of agreement is misleading in this study for two reasons. First, the kappa coefficient assumes that the expected agreement depends on the marginal totals of the 2 × 2 table but makes no assumptions regarding the observed values. This means that, even with a high observed agreement, as in our study, the kappa value may be low. The rationale for the chance correction employed in Cohen’s kappa is that observers may agree by chance. This is not a valid assumption when it comes to “trained” observers, as more experience means that chance will play a lesser role in decision-making [44]. Second, the distribution of marginal totals affects the maximum kappa that may be achieved [44], and our population was unbalanced between positive and negative findings.
An overview of some of the larger, more recent studies on PMCT for skull fracture detection are presented in Table 14. In all studies but Jacobsen and Lynnerup [17] and Leth et al. [41], who used pathologists with years of experience in reading PMCT images, scans were interpreted by radiologists.
A reason for the difference between the literature and our study is the fundamental methodical difference of a fracture system versus the individual fracture line. In a study on rib fractures with a more comparable methodology, Schulze et al. found a comparably low sensitivity of 0.63 and specificity of 0.97 [42].
In several cases, fractures were detected in both the vault and base of the skull on PMCT, but not to the extent demonstrated at autopsy. Similarly, Wozniak et al. visualized the fracture systems in part in seven of 10 cases and the full extent of fracture in three cases [45]. Registering only the presence or absence of fracture systems, we would have found a sensitivity of 0.97 for the vault and 0.93 for the base.
Due to our inclusion criteria, only 14 skulls had no fractures in the vault, and five skulls had no fractures in the base. Given that presence of fracture was a criterion for inclusion, we consider the stated specificity when using the common method misleading for statistical reasons due to the low number of true negatives in our sample, as specificity = true negatives/(true negatives + false positives), and the false positives contribute disproportionately to the denominator.
A sensitivity of 1.0 is often reported, e.g. by Hoey et al. [46], Sochor et al. [47], Jacobsen et al. [43], and Di Paolo et al. [48]. In these studies, the sample sizes ranged from four to twenty, and the samples consisted of primarily motor vehicle accidents, aircraft mishaps, and high-velocity blunt force trauma or were selected on the basis of fractures detected at autopsy. We assume fracture systems in such cases are clearly visible because of the extent of injury. Le Blanc-Louvry et al. found a sensitivity of 0.97 for the vault and 0.85 for the base at first reading in 236 “routine” cases [20], and Legrand et al. found a sensitivity of 0.97 for the vault and 1.0 for the base in a sample of 73 consecutive deaths [22]. Both studies had a high proportion of gunshot deaths and should projectile trauma have caused skull fracture; it is our experience that they are clearly visible on PMCT. As seen from Table 4, some of our cases have suffered severe trauma, but as we registered all individual fracture lines, severe cases were not “easier”. We excluded cases with severely comminute fractures, as they were too difficult to establish location and direction of individual fracture lines in. Even with these cases excluded, we found a sensitivity comparable to Legrand et al. and Le Blanc-Louvry et al. had we used the common methodology.
For the parietal, occipital, and temporal bones and base part of the frontal and sphenoid bones, the number of false negatives appears high, but these locations contained fracture systems with extensive and intricate patterns. This resulted in a high number of individual fracture lines, and while the fracture system and its major fracture lines were correctly identified, a minute fracture line in the periphery of the fracture system still constituted an individual finding and contributed statistically equal to the larger, and forensically and clinical relevant parts of the fracture system.
The ethmoid bone appears to have a very low sensitivity. It was difficult to detect fractures in the thin, perforated cribriform plate on PMCT, but this finding is probably exaggerated statistically because of the few true positives.
In this study, many of the overlooked fracture lines were non-dislocated, without bleeding, and described as “hairline”, i.e. a minor fracture in which the bones remain aligned. The hairline fracture lines were elusive regardless of anatomical situation. Until the resolution in both acquisition and reconstruction of PMCT images, as well as the ability of the human eye and brain to distinguish such hairline fractures, is sufficient, isolated hairline fractures will remain overlooked for technical and physical reasons.
Sensitivity was higher for the dislocated fractures, but fracture lines of bone fragments that appear dislocated at autopsy may not have been so at PMCT, as the scalp, skin, and other tissues keep the bones in place and to some extent adjacent. Commingled and comminute bone parts made it more difficult to establish the location and direction of individual fracture lines on PMCT compared to autopsy.
Leconte et al. found 29 fractures in the skull base at PMCT and only 20 at autopsy with the differences being in the small (n = 3) and greater (n = 2) wings of the sphenoid, the pyramid of the temporal bone (n = 3), and the occipital bone (n = 1), for a kappa value of 0.68 for the base. In the vault, ten of ten fractures were the same for a kappa of 1.0 [49]. This phenomenon of more fractures at PMCT than at autopsy is the basis for the decision by several authors [18, 41, 50] to calculate agreement rather than sensitivity.
Cattaneo et al. performed a study on five piglets, where four were severely beaten post mortem in order to induce fractures. The piglets were CT-scanned, then autopsied, and finally macerated for osteological analysis. With a slice thickness of 3 mm and interpretation by two radiologists, 26% more fractures were found in the cranium with PMCT than at osteological analysis. The authors speculate that a reason for the excess of fractures at PMCT may be that a single, long fracture line is seen as two, shorter, independent fractures on PMCT, which explain the excess of fractures detected [40]. Considering these findings, we presume osteological analysis of macerated bone the absolute gold standard for fracture identification, and thus the additional fractures “seen” at PMCT as false positives of PMCT rather than false negatives of osteological analysis.
In our study, the neuro-cranium was visualized at autopsy, yet fractures just above the nasal-frontal suture, in the frontal sinuses, and of the occipital condyles were missed. All fractures registered at PMCT not found at autopsy were considered false positives, even when presumably “true”, which increased the number of false positives. Fracture lines, which were beyond doubt the same at PMCT and autopsy, but had been registered differently, e.g. diastatic vs. close to the suture line resulted in both a false and a false negative.
In the existing literature, specificity is not always reported [16, 51] or becomes 1.0 as inclusion criteria are presence of fracture [17]. In studies with a few false positives, they are masked statistically by a large number of true negatives from cases with no head trauma at all [19]. For these reasons, the specificity was lower in our study than reported elsewhere.
Conclusion
We investigated the sensitivity and specificity of PMCT for individual fracture lines in individual bones of the neuro-cranium because reliable PMCT data may be used for 3D models and FEA. Considering the aim of using 3D models based on PMCT data for FEA to assist the forensic pathologist in interpreting blunt force skull fracture, we suggest supplementing PMCT data with information gathered at autopsy in order to compare the results of finite element analysis and the actual fractures of the deceased’s skull.
PMCT with the parameters employed in this study is suited to detect the presence of a fracture system, but not suited to detect each individual fracture line. If a case warrants full elucidation of fractures, then autopsy supplemented by PMCT is better than PMCT alone.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Jalalzadeh H, Giannakopoulos GF, Berger FH et al (2015) Post-mortem imaging compared with autopsy in trauma victims–a systematic review. Forensic Sci Int 257:29–48. https://doi.org/10.1016/j.forsciint.2015.07.026
Ampanozi G, Halbheer D, Ebert LC, Thali MJ, Held U (2019) Postmortem imaging findings and cause of death determination compared with autopsy: a systematic review of diagnostic test accuracy and meta-analysis. Int J Legal Med 321–37.https://doi.org/10.1007/s00414-019-02140-y
Blokker BM, Wagensveld IM, Weustink AC, Oosterhuis JW, Hunink MG (2016) Non-invasive or minimally invasive autopsy compared to conventional autopsy of suspected natural deaths in adults: a systematic review. Eur Radiol 26:1159–1179. https://doi.org/10.1007/s00330-015-3908-8
Thali MJ, Viner MD, Brogdon BG (2010) Brogdon’s forensic radiology, 2nd edn. Taylor & Francis
Wullenweber R, Schneider V, Grumme T (1977) A computer-tomographical examination of cranial bullet wounds. Z Rechtsmed J Legal Med 80:227–246. https://doi.org/10.1007/bf02114619
Baglivo M, Winklhofer S, Hatch GM, Ampanozi G, Thali MJ, Ruder TD (2013) The rise of forensic and post-mortem radiology—analysis of the literature between the year 2000 and 2011. J Forensic Radiol Imaging 1:3–9. https://doi.org/10.1016/j.jofri.2012.10.003
Poulsen K, Simonsen J (2007) Computed tomography as routine in connection with medico-legal autopsies. Forensic Sci Int 171:190–197. https://doi.org/10.1016/j.forsciint.2006.05.041
Leth PM (2009) Computerized tomography used as a routine procedure at postmortem investigations. Am J Forensic Med Pathol 30:219–222. https://doi.org/10.1097/PAF.0b013e318187e0af
O’Donnell C, Rotman A, Collett S, Woodford N (2007) Current status of routine post-mortem CT in Melbourne, Australia. Forensic Sci Med Pathol 3:226–232. https://doi.org/10.1007/s12024-007-9006-8
Delbreil A, Gambier A, Lebeau M, Voyer M, Houpert T, Sapanet M (2015) Le scanner post-mortem : état des lieux des pratiques en France en 2013. Rev de Méd Lég 6:47–52. https://doi.org/10.1016/j.medleg.2015.06.002
Ebert LC, Schweitzer W, Gascho D et al (2017) Forensic 3D visualization of CT data using cinematic volume rendering: a preliminary study. AJR Am J Roentgenol 208:233–240. https://doi.org/10.2214/ajr.16.16499
Villa C, Olsen KB, Hansen SH (2017) Virtual animation of victim-specific 3D models obtained from CT scans for forensic reconstructions: living and dead subjects. Forensic Sci Int 278:27–33. https://doi.org/10.1016/j.forsciint.2017.06.033
Buck U, Naether S, Räss B, Jackowski C, Thali MJ (2013) Accident or homicide–virtual crime scene reconstruction using 3D methods. Forensic Sci Int 225:75–84. https://doi.org/10.1016/j.forsciint.2012.05.015
Kleiven S (2006) Biomechanics as a forensic science tool: reconstruction of a traumatic head injury using the finite element method. Scand J Forens Sci 2:73–78
Li X, Sandler H, Kleiven S (2019) Infant skull fractures: accident or abuse?: Evidences from biomechanical analysis using finite element head models. Forensic Sci Int 294:173–182. https://doi.org/10.1016/j.forsciint.2018.11.008
Yen K, Lövblad KO, Scheurer E et al (2007) Post-mortem forensic neuroimaging: correlation of MSCT and MRI findings with autopsy results. Forensic Sci Int 173:21–35. https://doi.org/10.1016/j.forsciint.2007.01.027
Jacobsen C, Lynnerup N (2010) Craniocerebral trauma–congruence between post-mortem computed tomography diagnoses and autopsy results: a 2-year retrospective study. Forensic Sci Int 194:9–14. https://doi.org/10.1016/j.forsciint.2009.10.001
Daly B, Abboud S, Ali Z, Sliker C, Fowler D (2013) Comparison of whole-body post mortem 3D CT and autopsy evaluation in accidental blunt force traumatic death using the abbreviated injury scale classification. Forensic Sci Int 225:20–26. https://doi.org/10.1016/j.forsciint.2012.08.006
Leth P, Thomsen J (2013) Experience with post-mortem computed tomography in Southern Denmark 2006–11. J Forensic Radiol Imaging 1:161–166. https://doi.org/10.1016/j.jofri.2013.07.006
Le Blanc-Louvry I, Thureau S, Duval C et al (2013) Post-mortem computed tomography compared to forensic autopsy findings: a French experience. Eur Radiol 23:1829–1835. https://doi.org/10.1007/s00330-013-2779-0
Graziani G, Tal S, Adelman A, Kugel C, Bdolah-Abram T, Krispin A (2018) Usefulness of unenhanced post mortem computed tomography - findings in postmortem non-contrast computed tomography of the head, neck and spine compared to traditional medicolegal autopsy. J Forensic Leg Med 55:105–111. https://doi.org/10.1016/j.jflm.2018.02.022
Legrand L, Delabarde T, Souillard-Scemama R et al (2019) Comparison between postmortem computed tomography and autopsy in the detection of traumatic head injuries. J Neuroradiol 47:5–12. https://doi.org/10.1016/j.neurad.2019.03.008
Banner JH, Høyer C, Christensen M, Gheorghe A, Bugge A, Ottesen G, Boel L, Thomsen J, Kruckow L, Jacobsen C (2019) SURVIVE: Let the dead help the living - an autopsy-based cohort study for mapping risk markers of death among those withs evere mental illnesses. Scand J Forens Sci 24:7–17. https://doi.org/10.2478/sjfs-2018-0002
Intrasense (2017) Myrian Expert. 2.2 ed
Connolly AJ, Finkbeiner WE, Ursell PC, Davis RL (2015) Autopsy pathology: a manual and atlas. Elsevier Health Sciences
Rutty GN (2001) Post-mortem changes and artefacts. In: Rutty GN (ed) Essentials of autopsy practice, vol 1. Springer, London, pp 63–95
Knight B (1983) The coroner’s autopsy: a guide to non-criminal autopsies for the general pathologist. Churchill Livingstone
Saphir O (1958) Autopsy diagnosis and technic. P.B. Hoeber
Viera AJ, Garrett JM (2005) Understanding interobserver agreement: the kappa statistic. Fam Med 37:360–363
Akobeng AK (2007) Understanding diagnostic tests 1: sensitivity, specificity and predictive values. Acta Paediatr 96:338–341. https://doi.org/10.1111/j.1651-2227.2006.00180.x
Ashman CJ, Yu JS, Wolfman D (2000) Satisfaction of search in osteoradiology. AJR Am J Roentgenol 175:541–544. https://doi.org/10.2214/ajr.175.2.1750541
Filograna L, Tartaglione T, Filograna E, Cittadini F, Oliva A, Pascali VL (2010) Computed tomography (CT) virtual autopsy and classical autopsy discrepancies: radiologist’s error or a demonstration of post-mortem multi-detector computed tomography (MDCT) limitation? Forensic Sci Int 195:13–17. https://doi.org/10.1016/j.forsciint.2009.11.001
Garland LH (1949) On the scientific evaluation of diagnostic procedures. Radiology 52:309–328. https://doi.org/10.1148/52.3.309
Pescarini L, Inches I (2006) Systematic approach to human error in radiology. Radiol Med (Torino) 111:252–267
Wood BP (1999) Decision making in radiology. Radiology 211:601–603. https://doi.org/10.1148/radiology.211.3.r99jn35601
Gascho D, Thali MJ, Niemann T (2018) Post-mortem computed tomography: Technical principles and recommended parameter settings for high-resolution imaging. Med Sci Law 58:70–82. https://doi.org/10.1177/0025802417747167
Christe A, Flach P, Ross S et al (2010) Clinical radiology and postmortem imaging (Virtopsy) are not the same: specific and unspecific postmortem signs. Leg Med (Tokyo) 12:215–222. https://doi.org/10.1016/j.legalmed.2010.05.005
Carson HJ (2010) Unexpected death following single blow to the orbit. Am J Forensic Med Pathol 31:370–372. https://doi.org/10.1097/PAF.0b013e3181d3dbd7
Brahams D (1991) Hairline fracture and undiagnosed meningitis. Lancet 337:605–606. https://doi.org/10.1016/0140-6736(91)91659-i
Cattaneo C, Marinelli E, Di Giancamillo A et al (2006) Sensitivity of autopsy and radiological examination in detecting bone fractures in an animal model: implications for the assessment of fatal child physical abuse. Forensic Sci Int 164:131–137. https://doi.org/10.1016/j.forsciint.2005.12.016
Leth PM, Struckmann H, Lauritsen J (2013) Interobserver agreement of the injury diagnoses obtained by postmortem computed tomography of traffic fatality victims and a comparison with autopsy results. Forensic Sci Int 225:15–19. https://doi.org/10.1016/j.forsciint.2012.03.028
Schulze C, Hoppe H, Schweitzer W, Schwendener N, Grabherr S, Jackowski C (2013) Rib fractures at postmortem computed tomography (PMCT) validated against the autopsy. Forensic Sci Int 233:90–98. https://doi.org/10.1016/j.forsciint.2013.08.025
Jacobsen C, Bech BH, Lynnerup N (2009) A comparative study of cranial, blunt trauma fractures as seen at medicolegal autopsy and by computed tomography. BMC Med Imaging 9.https://doi.org/10.1186/1471-2342-9-18
Feinstein AR, Cicchetti DV (1990) High agreement but low kappa: I. The problems of two paradoxes. J Clin Epidemiol 43:543–549. https://doi.org/10.1016/0895-4356(90)90158-l
Woźniak K, Urbanik A, Moskała A, Chrzan R, Kamieniecka B (2008) Skull fractures–a comparison of clinical CT and autopsy findings. Arch Med Sadowej Kryminol 58:188–193
Hoey BA, Cipolla J, Grossman MD et al (2007) Postmortem computed tomography, “CATopsy”, predicts cause of death in trauma patients. J Trauma 63:979–85. https://doi.org/10.1097/TA.0b013e318154011f discussion 85-6
Sochor MR, Trowbridge MJ, Boscak A, Maino JC, Maio RF (2008) Postmortem computed tomography as an adjunct to autopsy for analyzing fatal motor vehicle crash injuries: results of a pilot study. J Trauma 65:659–665. https://doi.org/10.1097/TA.0b013e3181238d66
Di Paolo M, Maiese A, dell’Aquila M et al (2020) Role of post mortem CT (PMCT) in high energy traumatic deaths. Clin Ter 171:490–500. https://doi.org/10.7417/ct.2020.2263
Leconte C, Peyron PA, Meusy A, Lossois M, Baccino E (2016) Confrontation of the efficiency of post-mortem computed tomography and classical autopsy in the detection of osteoarticular traumatic injuries: About 28 cases. Rev de Méd Lég 7:51–59. https://doi.org/10.1016/j.medleg.2016.02.002
Wijetunga C, O’Donnell C, So TY et al (2020) Injury detection in traumatic death: postmortem computed tomography vs. open autopsy. Forensic Imaging 20:100349. https://doi.org/10.1016/j.jofri.2019.100349
Cha JG, Kim DH, Kim DH et al (2010) Utility of postmortem autopsy via whole-body imaging: initial observations comparing MDCT and 3.0 T MRI findings with autopsy findings. Korean J Radiol 11:395–406. https://doi.org/10.3348/kjr.2010.11.4.395
Author information
Authors and Affiliations
Contributions
MJH, CJ, and CV conceived the study. MJH, CJ, and CV contributed to the protocol. MJH registered findings and interpreted PMCT images. All authors contributed to inter-observer analysis. MJH wrote the first draft. All authors contributed to the writing and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Per Danish legislation, no ethical approval is needed for studies based on registry data.
Data approval
The University of Copenhagen approved the data-handling plan on behalf of the Danish Data Protection Agency (514–0437/19–3000).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Henningsen, M.J., Harving, M.L., Jacobsen, C. et al. Fractures of the neuro-cranium: sensitivity and specificity of post-mortem computed tomography compared with autopsy. Int J Legal Med 136, 1379–1389 (2022). https://doi.org/10.1007/s00414-022-02779-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-022-02779-0